Abstract
We describe a patient with Burkitt lymphoma who developed carotidynia. MRI showed thickening of the walls of both common carotid arteries and PET CT showed increased radiotracer uptake in the same regions. MRI was essential in establishing the diagnosis of this rare clinical presentation.
Keywords: Burkitt lymphoma, carotidynia, MRI, carotid artery, carotid sheath
Introduction
Burkitt lymphoma (BL) is a highly aggressive B-cell non-Hodgkin lymphoma that generally responds to chemotherapy. It may be endemic or sporadic, or immunodeficiency-associated 1,2. The endemic form occurs in Africa and is related to Epstein-Barr virus infection. It usually affects children and its most common location is the mandible. The sporadic form occurs in the United States and other Western countries and most commonly affects the abdomen including mesenteric and retroperitoneal lymph nodes1,2. The neck is less frequently involved than in other lymphomas but some reports describe it in the sinonasal and orbit regions and also in more unusual locations such as the nasopharynx, parapharyngeal space, mastoid, and oral cavity3,4. Here, we describe a case of Burkitt lymphoma affecting the carotid arteries.
Case Report
A 62-year-old man presented with diffuse adenopathy and biopsy revealed typical findings for Burkitt lymphoma (starry sky pattern, CD20, CD10, BCL-6, Ki-67 positive, and FISH c-myc gene rearrangement). A lumbar puncture showed the CSF to be normal. He presented to our hospital with left neck pain of three days duration and on physical examination was noticed to have tenderness to palpation of the neck along the anterior border of the left sternocleidomastoid muscle. Neck CT, MRI and MRA revealed diffuse circumferential thickening and enhancement surrounding the left common carotid artery from the level of the cricoid cartilage to the carotid bulb without reduction of vessel lumen. The abnormal pericarotid tissue demonstrated hypoattenuation on CT and low signal intensity on T1 and T2-weighted images on MRI with intense and homogenous contrast enhancement. No cervical lymphadenopathy was identified and his chemotherapy, including steroids, was continued. The patient continued to have neck pain extending to the contralateral side and a PET CT obtained three weeks later showed increased FDG uptake in the carotid regions (left greater than right). Repeat neck MRI and MRA showed development of new enhancing soft tissue, with similar signal characteristics to the one initially present on the left side, surrounding the right common carotid artery. Again no arterial luminal narrowing was seen. Chemotherapy was continued and at the time of this writing, the patient continues to be stable but without significant change in neck findings.
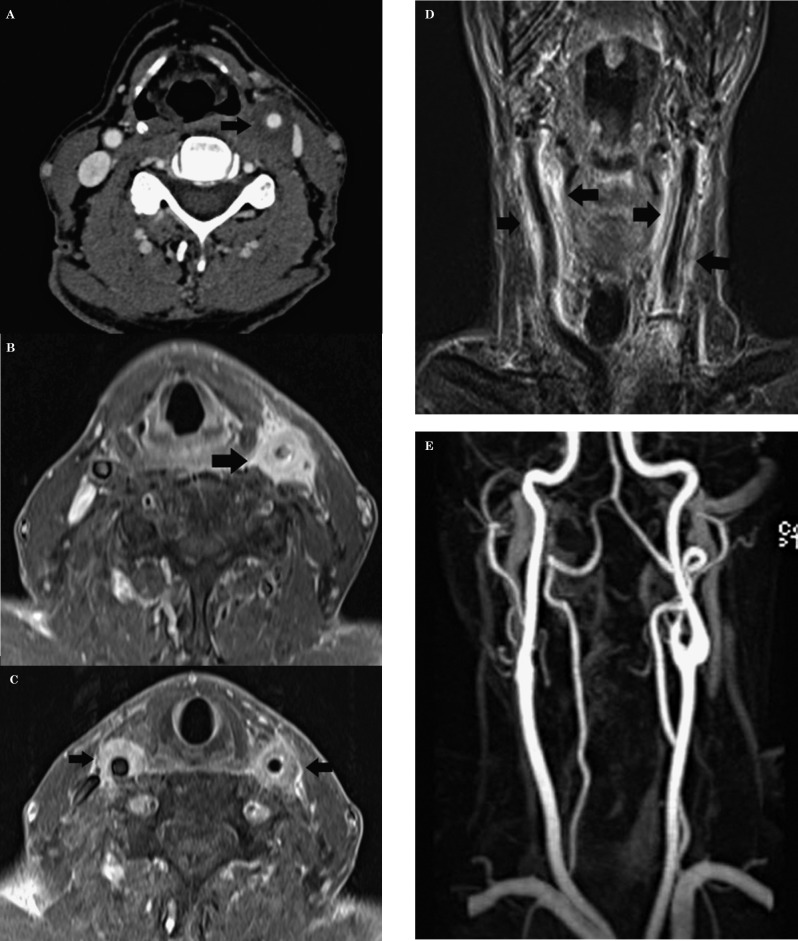
Figure 1.
Burkitt lymphoma presenting as carotidynia. A) Axial post contrast CT shows low density soft tissues encircling (arrow) the left common carotid artery (CCA) without narrowing of its enhancing lumen. B) Corresponding fat-suppressed axial post contrast T1 image shows marked enhancement of the pericarotid tissues (arrow) on the left. C) Axial post contrast fat-suppressed image during the second presentation shows that now there are significant enhancing tissues (arrow) surrounding both CCAs. D) Coronal post contrast T1 image shows the abnormalities following the CCAs throughout their extent. E) Coronal view from a contrast-enhanced MR angiogram shows the lumen of the CCAs to be normal.
Discussion
The sporadic form of BL is characterized by rapidly growing masses, usually in the abdomen and predominantly occurring in men. An increase in tumor size may cause obstruction or compression of vital structures4. The occurrence of BL in the head and neck is rare and predominantly seems to affect lymph nodes 4,5. To the best of our knowledge, Burkitt lymphoma presenting as carotidynia and affecting both carotid arteries has not been reported.
Imaging findings in our patient, in both CT and MRI, are similar to those described in patients with idiopathic inflammatory pseudotumor of the carotid sheath, previously equated with the term “carotidynia” 5,6. Carotidynia is now considered to refer to only neck pain in the area corresponding to the carotid arteries and is not a distinct pathologic entity. The differential diagnosis of carotidynia includes giant cell arteritis, atherosclerosis, thrombosis, intraluminal hemorrhage, fibromuscular dysplasia, aneurysm, dissection, and inflammatory pseudotumor 7. Malignant tumors of the head and neck, such as squamous cell carcinoma, may also infiltrate the tissues surrounding the neck blood vessels and usually result in reduction of the arterial lumina suggesting a more infiltrative and/or invasive process8.
Pericarotid thickening and intense contrast enhancement about the carotid sheath, associated with absence of reduction in the arterial lumen and rapid response to corticosteroids or non-steroidal anti-inflammatory drugs with symptom regression, are criteria supporting the diagnosis of idiopathic inflammatory pseudotumor. Our patient did not have a significant response to corticosteroids (as part of his chemotherapy). Thus, in rare instances, unresponsive carotidynia may be due to Burkitt's lymphoma and this entity should be included in the clinical differential diagnosis.
Anatomopathological studies focusing on the composition of the carotid sheath have found a predominance of fibrofatty tissue and scattered neutrophils. Khafif-Hefetz et al., however, found lymphoid aggregates almost exclusively composed of B cells in some cases9. Thus, lymphoma such as Burkitt's may originate in or involve the carotid arteries.
Conclusion
Burkitt lymphoma (BL) may rarely affect the carotid arteries and present as carotidynia. The key to the diagnosis on imaging studies is the absence of luminal narrowing despite pericarotid enhancing tissues similar to that seen with inflammatory conditions occurring in the same region. Inflammatory conditions respond rapidly to steroids, but BL will not. When pericarotid inflammation without luminal narrowing is found, we propose that although rare, BL be included in the differential diagnosis.
References
- 1.Ziegler JL. Burkitt's lymphoma. CA Cancer J Clin. 1982; 32 (3): 144–161. [Google Scholar]
- 2.Upile T Jerjes W Abiola J et al. A patient with primary Burkitt's lymphoma of the postnasal space: case report. Head Neck Oncol. 2012; 4: 33. doi: 10.1186/1758-3284-4-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Meuwly JY Lepori D Theumann N et al. Multimodality imaging evaluation of the pediatric neck: techniques and spectrum of findings. Radiographics. 2005; 25 (4): 931–948. [DOI] [PubMed] [Google Scholar]
- 4.Arakapis I Fradis M Schipper J et al. Recurrent syncope as presenting symptom of Burkitt's lymphoma at the carotid bifurcation. Ann Otol Rhinol Laryngol; 2004: 113 (5): 373–377. [DOI] [PubMed] [Google Scholar]
- 5.Farage L Motta AC Goldenberg D et al. Idiopathic inflammatory pseudotumor of the carotid sheath. Arq Neuropsiquiatr. 2007; 65 (4B): 1241–1244. [DOI] [PubMed] [Google Scholar]
- 6.Headache Classification Subcommittee of the International Headache Society. The International Classification of Headache Disorders: 2nd edition. Cephalalgia. 2004; 24 (Suppl 1): 9–160. [DOI] [PubMed] [Google Scholar]
- 7.Burton BS Syms MJ Petermann GW et al. MR imaging of patients with carotidynia. Am J Neuroradiol. 2000; 21 (4): 766–769. [PMC free article] [PubMed] [Google Scholar]
- 8.Nakahira M Nakatani H Takeda T. Syncope as a sign of occult malignant recurrence in the retropharyngeal and parapharyngeal space: CT and MR imaging findings in four cases. Am J Neuroradiol. 2002; 23 (7): 1257–1260. [PMC free article] [PubMed] [Google Scholar]
- 9.Khafif-Hefetz A Leider-Trejo L Medina JE et al. The carotid sheath: an anatomicopathologic study. Head Neck. 2004; 26 (7): 594–597. [DOI] [PubMed] [Google Scholar]