Abstract
Objectives:
This study evaluated the effectiveness of a structured multidisciplinary risk assessment and management programme for patients with hypertension (RAMP-HT) who were managed in public primary care clinics but had suboptimal blood pressure (BP) control in improving BP, LDL-cholesterol (LDL-C) and predicted 10-year cardiovascular disease (CVD) risk after 12 months of intervention.
Methods:
A total of 10 262 hypertension patients with suboptimal BP despite treatment, aged less than 80 years and without existing CVD were enrolled in RAMP-HT between October 2011 and March 2012 from public general out-patient clinics in Hong Kong. Their clinical outcomes and predicted 10-year CVD risk were compared with a matched cohort of hypertension patients who were receiving usual care in general out-patient clinics without any RAMP-HT intervention by propensity score matching. Multivariable linear and logistic regressions were used to determine the independent effectiveness of RAMP-HT after adjusting for potential confounding variables.
Results:
Compared with the usual care group after 12 months, significantly greater proportions of RAMP-HT participants achieved target BP (i.e. BP < 140/90 mmHg) (OR = 1.18, P < 0.01) and LDL-C levels (i.e. <3.4 mmol/l for patients with CVD risk ≤20% or <2.6 mmol/l for CVD risk >20%) (OR = 1.13, P < 0.01). RAMP-HT participants also had significantly greater reduction in predicted 10-year CVD risk by 0.44% (coefficient = −0.44, P < 0.01).
Conclusion:
The structured multidisciplinary RAMP-HT was more effective than usual care in achieving target BP, LDL-C and reducing predicted 10-year CVD risk in public primary care patients with suboptimal hypertension control after 12 months of intervention. A long-term follow-up should be conducted to confirm whether the improvement in clinical outcomes can be translated into actual reductions in CVD complications and mortalities and whether such approach is cost-effective.
Keywords: cardiovascular disease risk, hypertension, primary care, risk assessment, risk management, risk stratification
INTRODUCTION
Hypertension is a global public health issue of the 21st century [1], affecting more than one-third of the world's population [2]. Blood pressure (BP) optimization has been an important management goal for healthcare providers to prevent hypertension-related complications and mortality. An array of treatment options, including pharmacological agents and lifestyle modification such as dietary approaches to stop hypertension, exercise, weight reduction, smoking cessation and moderation of alcohol consumption, had proven efficacy in lowering BP and reducing long-term hypertension complications [3–5]. However, successful implementation of these multifaceted interventions in the real-world clinical setting can be challenged by many factors, such as difficult accesses to healthcare, financial constraints of patients and the healthcare system, insufficient consultation time, patients’ poor adherence to interventions and follow-ups, doctors’ inertia to adjust medication or make referral to allied health services, and confounding or even contrasting recommendations from international guidelines regarding ‘optimal’ treatment threshold of BP and other comorbid cardiovascular disease (CVD) risk factors [6,7]. Various interventions had been explored to address these barriers, including educational intervention directed to the patients or the physicians, health profession–led (nurse or pharmacist) care, organization interventions and appointment reminder system [8]. Among these different interventions, structured algorithm-driven health profession–led care involving prescription adjustment and multidisciplinary care were shown to favour BP control [8–10]. However, evidence on the effects of multidisciplinary care for patients with hypertension was still sparse and lacked generalizability.
In addition to BP control, assessment and management of total CVD risk of hypertension patients has been advocated internationally as a holistic and cost-effective way to achieve maximal prevention or reduction in CVD and resultant mortalities [4,11–13]. A prospective trial on CVD-risk stratification and risk-guided intervention involving 7090 hypertension patients managed in primary care in the United States demonstrated that the implementation of CVD-risk stratification and intervention was associated with a 12-mmHg reduction in SBP over 10 years [14]. In Canada, the Cardiovascular Health Awareness Program confirmed that comprehensive screening and management via stratification of risk factors for hypertension patients reduced CVD mortality compared with usual care [15]. Mendis also reported that CVD risk management led to greater decrease in SBP, DBP and some behavioural changes even in low-resource settings [16]. However, these studies focused on CVD-risk stratification and risk-guided management by physicians; multidisciplinary team care was not employed nor evaluated.
Up to date, evidence is lacking in the effectiveness of structured protocol-driven intervention programme for hypertension patients in the primary care setting that encompasses both multidisciplinary care and CVD-risk stratification and management. This study aimed at evaluating the effectiveness of the risk assessment and management programme for patients with hypertension (RAMP-HT), a structured CVD-risk assessment and coordinated multidisciplinary management programme using readily available resources among public primary care clinics in Hong Kong, for hypertension patients with suboptimal BP control despite pharmacological treatment or lifestyle intervention in terms of clinical outcomes and predicted long-term CVD risks after 12 months of intervention. This was the first study to provide imperative translational evidence of CVD-risk stratification and risk-specific management delivered by a multidisciplinary team as an additional but integrated service to usual care for Chinese hypertension patients in the real-world primary care setting.
METHODS
We conducted a longitudinal cohort study to compare the changes in clinical outcomes and predicted long-term CVD risks at a 12-month follow-up between the RAMP-HT and the usual care group.
The RAMP-HT is a territory-wide quality improvement programme initiated by the Hospital Authority of Hong Kong, which manages over 200 000 people with hypertension without diabetes mellitus in Hong Kong, to enhance care of hypertension patients in the public primary care setting. Patients with hypertension who are aged less than 80 years, without existing CVD or diabetes mellitus, currently receiving usual care treatment (either pharmacotherapy or lifestyle interventions) from a public primary care clinic [i.e. general out-patient clinic (GOPC)] but still have suboptimal BP control (i.e. BP ≥ 140/90 mmHg) are targeted, although all hypertension patients managed under GOPC are served. From October 2011 to March 2012, the RAMP-HT was piloted in five of the seven clusters in Hong Kong. Details of the RAMP-HT programme have been reported elsewhere [17].
In summary, the enrolled patients underwent standardized CVD-risk assessment, hypertensive complication screening and assessment on adherence to medications and lifestyle by registered nurses during the RAMP-HT intake assessment, who acted as the care-managers. The standardized CVD-risk assessment comprised smoking habit assessment, anthropometric measurement (clinic BP, body height, body weight and waist circumference) and blood tests for full lipid profile and fasting plasma glucose level. To screen for hypertensive complications, an ECG was performed on each patient and reviewed by doctors to look for presence of left ventricular hypertrophy or evidence of cardiac ischaemia; vascular Doppler was performed by registered nurses to assess for weak or absent foot pulses signifying peripheral vascular disease; blood test for creatinine level was used to assess renal function based on the estimated glomerular filtration rate (eGFR) calculated by the MDRD formula, whereas spot urine for protein-to-creatinine ratio (PCR) was collected to look for significant proteinuria (i.e. urine PCR ≥ 10 mg/mmol). The registered nurses also assessed the participants’ self-management and lifestyle (e.g. diet, exercise, alcohol and self-monitoring of BP) and drug adherence by pill-counting and reviewing with each patient whether he or she could correctly recall the medication regime. Patients were then stratified into low, medium or high risk groups according to the 10-year CVD risk calculated from their relevant risk factors by the Joint British Society 2005 Equation. A multidisciplinary team comprising doctors, nurses, dieticians, physiotherapists and/or occupational therapists would then deliver individualized management targeted to the patient's risk factors, lifestyle and compliance according to standardized risk-stratified guidelines. Each team member had a well defined role: the care-manager nurse provided patient education on hypertension knowledge, self-BP monitoring, adherence to drug and lifestyle advices on diet, exercise and alcohol consumption, informed other team members on individual patient's risk profile via electronic reminder system and referred the patients to respective services by other team members according to protocol; special smoking cessation counselling sessions were also offered by nurses to smokers who were motivated to quit smoking; frontline doctors were responsible for drug therapy titration and overseeing the process of care; dietitians and physiotherapists dealt with obesity and impaired glucose homeostasis, whereas occupational therapists managed clinically significant psychological distress resulting from or contributing to poor BP control (Fig. 1).
FIGURE 1.
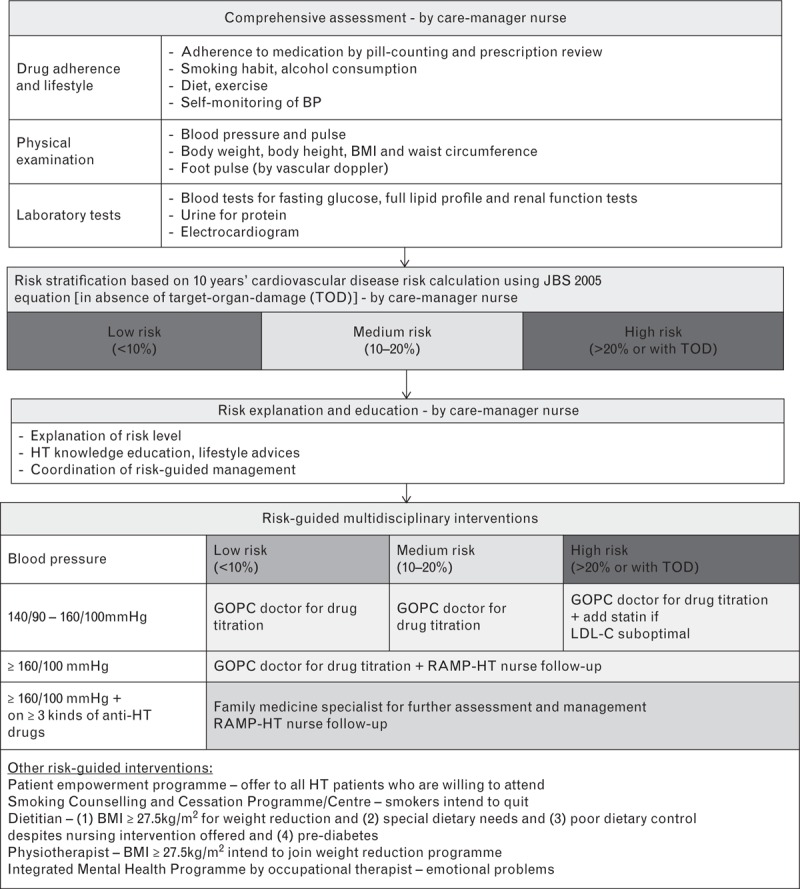
Risk assessment and management programme for hypertension workflow.
On the other hand, patients under usual care would be continuously managed by GOPCs doctors without the nurse-led structured risk assessment and risk-guided management. These patients had access to the same drug formulary and could still be referred to for physical examination, laboratory testing and ECG assessment, or to various allied health professionals services at their doctors’ discretion.
A total of 12 234 hypertension patients aged less than 80 years, without existing CVD or diabetes mellitus, with suboptimal BP control (i.e. average SBP ≥ 140 mmHg or average DBP ≥90 mmHg) despite lifestyle or pharmacological intervention, who were enrolled in the RAMP-HT between October 2011 and March 2012 and had clinical outcomes records collected at 12 months from baseline were identified from the Hospital Authority Clinical Management System (CMS). A total of 10 262 out of the 12 234 RAMP-HT participants were matched to the same number of patients receiving usual care at GOPC who never enrolled in RAMP-HT on or before 30 Jun 2013 using propensity score matching based on social demographics, drug history, biometric data and predicted 10-year CVD risk and the stage of hypertension [18]. The propensity score mapping was made by using the ‘psmatch2’ command with one-to-one matching without replacement and a caliper of 0.001 approach in the STATA. Figure 2 shows the flow of patient selection and matching in this study. These two matched cohorts were included in the evaluation of the effectiveness of RAMP-HT. The dates of baseline for RAMP-HT participants and usual care group were defined as the date of enrolment and 31 Oct 2011, respectively, and the follow-up period for both groups was defined as 12-month after baseline.
FIGURE 2.
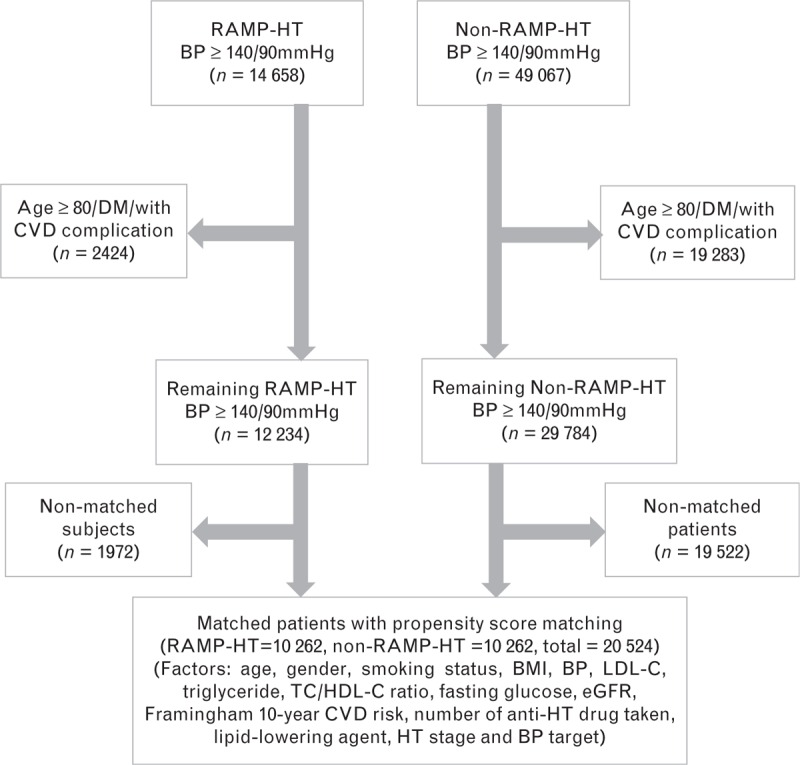
Flow chart of patients matching.
The primary outcomes of this study were the proportion of patients achieving satisfactory BP (SBP < 140 mmHg and/or DBP < 90 mmHg), LDL-C (<3.4 mmol/l for patients with predicted CVD risk ≤20% or <2.6 mmol/l for CVD risk >20%) as recommended by the Hong Kong framework [19], and the mean changes in predicted 10-year CVD risk after 12 months of intervention. The secondary outcomes were the mean changes in the clinical outcomes (SBP, DBP, LDL-C), the likelihood to improve (post–pre <0) in clinical outcomes and predicted 10-year CVD risks at a 12-month follow-up, and the number needed to treat (NNT) to achieve satisfactory BP and to prevent a predicted CVD event.
All information including sociodemographics and biomedical outcomes data at baseline and 12 months were extracted from the Hospital Authority CMS. Sociodemographics included age, sex and smoking habit. Drug history included the number of antihypertensive drugs prescribed and the use of lipid lowering agent. Biometric data were BP, BMI, lipid profile [LDL-cholesterol (LDL-C), total cholesterol-to-HDL-cholesterol ratio (TC/HDL-C ratio) and triglyceride], fasting glucose and eGFR. The stage of hypertension was defined according to the Joint National Committee – Stage I: BP between 140–159/90–99 mmHg; Stage II: BP at least 160/100 mmHg [4]. The 10-year predicted CVD risk was estimated by the total CVD risk of the Framingham risk prediction function [12]. To avoid the impact of ageing on CVD risks, we applied the age at baseline to calculate the CVD risks at both baseline and 12 months. The BP at baseline was defined as the averages of all available BP readings within 6 months before baseline, whereas the BP at 12 months was defined as the averages of all BP measurements between 6 and 18 months after baseline. All other biometric data at baseline and 12 months were defined as the latest available reading until 3 months and between 6 and 18 months after baseline, respectively.
Descriptive statistics were used to report the characteristics of sociodemographics, drug history, biomedical data, predicted 10-year CVD risk and the stage of hypertension of each patient in RAMP-HT group and usual care groups at baseline and after 12 months. Differences in baseline and 12-month characteristics between groups were tested using independent t tests for continuous variables or chi-square tests for categorical variables.
To assess the effectiveness of RAMP-HT compared with usual care after 12 months of intervention, the mean changes, the proportion of target achievement and improvements in clinical outcomes (SBP, DBP and LDL-C) and predicted 10-year CVD risk were evaluated. Paired t tests were used to evaluate the mean within-patients changes in the outcomes of interest at 12 months compared with baseline. Unadjusted difference-in-difference estimation in the outcomes between groups was performed by independent t tests. The NNT to achieve satisfactory BP and to prevent a predicted CVD event were calculated. Adjusted difference-in-difference estimations between groups were assessed using multiple linear regressions by the adjustment of confounding factors (sociodemographics, drug history, biomedical data, predicted 10-year CVD risk and the stage of hypertension). Similarly, for the evaluation of the rate of target achievement and improvement in the outcomes, chi-square test was used to test the unadjusted difference-in-difference in the proportion of target achievement rate and improvement between groups. Adjusted difference-in-difference estimations between groups were assessed using multiple logistic regressions by the adjustment of confounding factors mentioned above.
All statistical analyses were performed using STATA version 13.0 (StataCorp LP. College Station, Texas, USA). All significance tests were two-tailed and findings with a P value less than 0.05 were considered statistically significant.
Ethics approvals
The current study has received ethics approval from the Institutional Review Board of the University of Hong Kong/Hospital Authority Hong Kong West Cluster (UW 13-227), Hong Kong East Cluster (HKEC-2013-029), Kowloon East and Kowloon Central Cluster (KC/KE-13-0069/ER-3), Kowloon West Cluster [KW/EX-13-082 (64-10)], New Territories East Cluster (CRE-2013.423) and New Territories West Cluster (NTWC/CREC/1193/13). The clinical trial number and registry is NCT02219958, ClinicalTrials.gov.
RESULTS
A total of 20 524 patients, 10 262 from each of the RAMP-HT group and usual care group, were included in the final data analysis (Fig. 2). The baseline and 12-month characteristics of the RAMP-HT participants and usual care hypertension patients are shown in Table 1. Due to propensity score matching, the sociodemographics, drug history, biomedical data, predicted 10-year CVD risk and the stage of hypertension between the two groups were similar at baseline. All patients had suboptimal BP at least 140/90 mmHg at enrolment, whereas 10% of patients had BP at least 160/100 mmHg. Among these patients, over 98% were taking at least one antihypertensive medication, whereas the remaining 2% were receiving lifestyle interventions. Approximately 60% of patients had suboptimal LDL-C control (i.e. ≥2.6 mmol/l for patients with predicted 10-year CVD risk >20% and ≥3.4 mmol/l for patients with predicted 10-year CVD risk ≤20%) at enrolment, but only 10% were prescribed a lipid-lowering-agent.
TABLE 1.
Sociodemographic and clinical characteristics of the patients at baseline and 12 months
| Clinical outcomes | Baseline | At 12 months | ||||
| RAMP-HT (n = 10 262) | Usual care (n = 10 262) | P value | RAMP-HT (n = 10 262) | Usual care (n = 10 262) | P value | |
| Age (mean ± SD) | 63.78 ± 9.60 (10 262) | 63.71 ± 10.03 (10 262) | 0.615 | 64.78 ± 9.60 (10 262) | 64.71 ± 10.03 (10 262) | 0.615 |
| Sex (%, n) | 0.910 | 0.910 | ||||
| Female | 56.4% (5789) | 56.3% (5781) | 56.4% (5789) | 56.3% (5781) | ||
| Male | 43.6% (4473) | 43.7% (4481) | 43.6% (4473) | 43.7% (4481) | ||
| Smoking status (%, n) | 0.880 | 0.007* | ||||
| Nonsmoker/ex-smoker | 91.7% (9406) | 91.6% (9400) | 92.8% (9527) | 91.8% (9424) | ||
| Current smoker | 8.3% (856) | 8.4% (862) | 7.2% (735) | 8.2% (838) | ||
| Baseline clinical characteristics (mean ± SD) | ||||||
| SBP (mmHg) | 148.70 ± 8.18 (10 262) | 148.68 ± 8.34 (10 262) | 0.890 | 136.85 ± 9.64 (10 262) | 137.68 ± 10.48 (10 262) | <0.001* |
| <140 mmHg (%, n) | 3.41% (350) | 3.46% (355) | 0.848 | 65.60% (6732) | 62.00% (6362) | <0.001* |
| DBP (mmHg) | 81.70 ± 9.34 (10 262) | 81.74 ± 9.09 (10 262) | 0.717 | 77.58 ± 8.37 (10 262) | 77.60 ± 8.56 (10 262) | 0.885 |
| <90 mmHg (%, n) | 79.43% (8151) | 79.38% (8146) | 0.931 | 93.70% (9615) | 92.81% (9524) | 0.011* |
| LDL-C (mmol/l) | 3.27 ± 0.83 (10 262) | 3.27 ± 0.81 (10 262) | 0.739 | 3.17 ± 0.80 (7949) | 3.24 ± 0.82 (6110) | <0.001* |
| <3.4 mmol/l (CVD risk ≤20%a); <2.6 mmol/l (CVD risk >20%b) (%, n) | 41.14% (4222) | 40.78% (4185) | 0.599 | 44.77% (3559) | 42.05% (2569) | 0.001* |
| TC (mmol/l) | 5.34 ± 0.92 (10 262) | 5.34 ± 0.91 (10 262) | 0.859 | 5.23 ± 0.91 (7998) | 5.32 ± 0.92 (6154) | <0.001* |
| Triglyceride (mmol/l) | 1.44 ± 0.77 (10 262) | 1.44 ± 0.82 (10 262) | 0.786 | 1.42 ± 0.84 (7997) | 1.43 ± 0.85 (6150) | 0.604 |
| HDL-C (mmol/l) | 1.42 ± 0.39 (10 262) | 1.42 ± 0.38 (10 262) | 0.258 | 1.42 ± 0.39 (7995) | 1.44 ± 0.37 (6148) | 0.052 |
| Fasting glucose (mmol/l) | 5.34 ± 0.56 (10 262) | 5.35 ± 0.58 (10 262) | 0.625 | 5.35 ± 0.62 (7734) | 5.41 ± 0.66 (6013) | <0.001* |
| eGFR (ml/min per 1.73 m2) | 84.30 ± 18.29 (10 262) | 84.26 ± 19.89 (10 262) | 0.879 | 84.51 ± 18.47 (8357) | 84.22 ± 20.29 (6900) | 0.353 |
| ≥60 ml/min per 1.73 m2 (%, n) | 93.36% (9581) | 92.55% (9497) | 92.66% (7744) | 91.36% (6304) | ||
| <60 ml/min per 1.73 m2 (%, n) | 6.64% (681) | 7.45% (765) | 7.34% (613) | 8.64% (596) | ||
| BMI (kg/m2) | 25.92 ± 3.85 (10 262) | 25.91 ± 3.97 (10 262) | 0.828 | 25.92 ± 3.97 (6417) | 26.16 ± 4.05 (4636) | 0.003* |
| Framingham 10-year CVD risk (%) | 23.25 ± 13.35 (10 262) | 23.25 ± 13.35 (10 262) | 0.983 | 19.52 ± 11.48 (7995) | 20.01 ± 11.93 (6148) | 0.013* |
| ≤20% (%, n) | 50.30% (5162) | 50.34% (5166) | 0.955 | 62.38% (4987) | 60.44% (3716) | 0.019* |
| HT stage (%, n) | 0.650 | <0.001* | ||||
| Stage I (SBP/DBP: 140–159/90–99 mmHg) | 89.5% (9184) | 89.3% (9164) | 94.6% (3503) | 92.3% (3777) | ||
| Stage II (SBP/DBP ≥ 160/100 mmHg) | 10.5% (1078) | 10.7% (1098) | 5.4% (200) | 7.7% (313) | ||
| Number of antihypertensive drugs taken (%, n) | 0.981 | 0.001* | ||||
| 0 | 1.9% (194) | 1.9% (194) | 2.5% (260) | 3.1% (318) | ||
| 1 | 54.0% (5545) | 54.3% (5573) | 45.6% (4675) | 47.3% (4854) | ||
| 2 | 35.8% (3671) | 35.5% (3643) | 40.4% (4148) | 38.1% (3914) | ||
| ≥3 | 8.3% (852) | 8.3% (852) | 11.5% (1179) | 11.5% (1176) | ||
| Lipid lowering agent (%, n) | 0.850 | <0.001* | ||||
| Yes | 9.6% (990) | 9.7% (998) | 19.1% (1956) | 15.3% (1573) | ||
| No | 90.4% (9272) | 90.3% (9264) | 80.9% (8306) | 84.7% (8689) | ||
CVD, cadiovascular disease; eGFR, estimated glomerular filtration rate; HDL-C, HDL-cholesterol; LDL-C, LDL-cholesterol; OGTT, oral glucose tolerance test; RAMP-HT, risk assessment and management programme for hypertension; TC, total cholesterol.
aFramingham 10-year CVD risk ≤ 20%.
bFramingham 10-year CVD risk >20%.
*Significant differences (P < 0.05) between RAMP-HT and usual care participants by independent t test or by chi-square test, as appropriate.
After 12 months, significant improvement in SBP (RAMP-HT: −11.85 mmHg; usual care: −11.01 mmHg), DBP (RAMP-HT: −4.12 mmHg; usual care: −4.15 mmHg), LDL-C level (RAMP-HT: −0.09 mmol/l; usual care: −0.04 mmol/l) and predicted 10-year CVD risks (RAMP-HT: −3.34%; usual care: −2.96%), were observed in both the RAMP-HT and usual care group. The observed differences between the two groups in BP control, LDL-C level and predicted 10-year CVD risks (SBP: −0.84 mmHg, P < 0.01; LDL-C: −0.05 mmol/l, P < 0.01; CVD risk: −0.39%, P < 0.01) were modest yet statistically significant. Significant differences were observed in the use of antihypertensive drugs and lipid-lowering agent between RAMP-HT participants and usual care patients. There were also significantly less current smoker and patients with BP more than 160/100 mmHg in the RAMP-HT group.
Table 2 and Fig. 3 show the target achievement rates, within-patient changes and improvement rates on clinical outcomes and predicted 10-year CVD risk from baseline to after 12 months of both RAMP-HT participants and usual care patients. Compared with the usual care group, a significantly greater proportion of RAMP-HT participants achieved the target BP, SBP, DBP and LDL-C after 12 months (BP: 3.77%, P < 0.01; SBP: 3.61%, P < 0.01; DBP: 0.89%, P = 0.011; LDL-C: 2.73%, P < 0.01). The NNT for patients reaching satisfactory BP control and for reduction of 1 predicted CVD event were 27 and 204, respectively. After adjusting for confounding factors, RAMP-HT was associated with an increased likelihood of target achievement in BP (OR = 1.18, P < 0.01), SBP (OR = 1.18, P < 0.01), DBP (OR = 1.21, P < 0.01), LDL-C (OR = 1.13, P < 0.01) and a greater reduction in the predicted 10-year CVD risk (coefficient = −0.44, P < 0.01).
TABLE 2.
Comparisons of the target achievement rates, within-patient changes and improvement rates on clinical outcomes and predicted 10-year cardiovascular disease risk from baseline to after 12 months of both risk assessment and management programme for hypertension participants and usual care patients
| Clinical outcomes | RAMP-HT (n = 10 262) | Usual care (n = 10 262) | Unadjusted difference-in-difference* | Adjusted difference-in-difference** | ||
| Paired difference***/after 12 months | Paired difference***/after 12 months | Estimate (95% CI) | P value | Coefficient/odds ratio (95% CI) | P value | |
| Target achievement rates (%, n) | ||||||
| SBP < 140 mmHg | 62.19% | 58.54% | 3.61% (2.291, 4.920) | <0.001**** | 1.18 (1.115, 1.254) | <0.001**** |
| DBP < 90 mmHg | 14.27% | 13.43% | 0.89% (0.200, 1.573) | 0.011**** | 1.21 (1.077, 1.366) | 0.001**** |
| SBP/DBP < 140/90 mmHg | 63.92% | 60.14% | 3.77% (2.444, 5.098) | <0.001**** | 1.18 (1.117, 1.253) | <0.001**** |
| LDL-C < 3.4 mmol/l (CVD risk ≤20%a); <2.6 mmol/l (CVD risk >20%b) | 3.63% | 1.27% | 2.73% (1.076, 4.378) | 0.001**** | 1.13 (1.039, 1.223) | 0.004**** |
| Mean changes | ||||||
| SBP (mmHg) | −11.85**** | −11.01**** | −0.84 (−1.147, −0.538) | <0.001**** | −0.84 (−1.099, −0.574) | <0.001**** |
| DBP (mmHg) | −4.12**** | −4.15**** | 0.03 (−0.164, 0.224) | 0.764 | 0.02 (−0.146, 0.182) | 0.828 |
| LDL-C (mmol/l) | −0.09**** | −0.04**** | −0.05 (−0.073, −0.025) | <0.001**** | −0.06 (−0.081, −0.039) | <0.001**** |
| Framingham 10-year CVD risk (%) | −3.34**** | −2.96**** | −0.39 (−0.578, −0.197) | <0.001**** | −0.44 (−0.606, −0.280) | <0.001**** |
| Improvements (%)c | ||||||
| SBP | 87.58% | 84.85% | 2.73% (1.786, 3.671) | <0.001**** | 1.27 (1.166, 1.373) | <0.001**** |
| DBP | 71.89% | 72.60% | −0.71% (−1.937, 0.514) | 0.255 | 0.97 (0.909, 1.038) | 0.389 |
| LDL-C < 3.4 mmol/l (CVD risk ≤20%a); <2.6 mmol/l (CVD risk >20%b) | 49.68% | 47.55% | 2.13% (0.468, 3.800) | 0.012**** | 1.13 (1.052, 1.213) | 0.001**** |
| Framingham 10-year CVD risk | 75.72% | 74.69% | 1.03% (−0.405, 2.468) | 0.159 | 1.07 (0.991, 1.160) | 0.081 |
CI, confidence interval; CVD, cardiovascular disease; RAMP-HT, risk assessment and management programme for hypertension.
aFramingham 10-year CVD risk ≤20%.
bFramingham 10-year CVD risk >20%.
cPre–post >0.
*P value of testing significance using independent t test.
**P value of testing significance in adjusted difference-in-difference estimate using multiple linear or logistic regressions, as appropriate.
***P value of testing significance using paired t test or chi-square test, as appropriate.
****Significant differences of P value <0.05.
FIGURE 3.
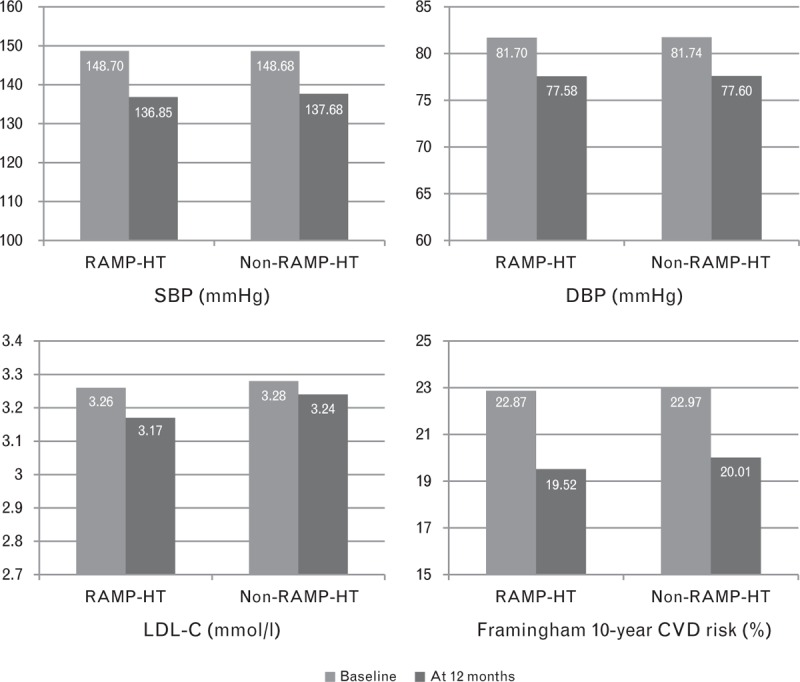
Changes between baseline and 12 months on clinical outcomes in risk assessment and management programme for hypertension and non-risk assessment and management programme for hypertension groups. All differences between baseline and 12 months for risk assessment and management programme for hypertension/non–risk assessment and management programme for hypertension are significant with P values <0.0001.
DISCUSSION
To the best of our knowledge, this is the first study to evaluate the effectiveness of a structured CVD-risk stratification and risk-guided management programme building on existing clinical resources and available multidisciplinary interventions, as an added-on service to usual care for patients with hypertension in the real-world primary care setting. Our results demonstrated that RAMP-HT led to greater proportion of patients achieving target BP and LDL-C and greater reduction in predicted 10-year CVD risk after 12 months of intervention among primary care patients with suboptimal BP control compared with the usual care; the difference reached statistical significance.
The RAMP-HT interventions are evidence based [17] and multifaceted, aiming to address four inter-related components of the chronic care model [20] using a multidisciplinary team approach. In contrast to traditional doctor-led idiosyncratic clinical care, the RAMP-HT nurse acts as the care manager for each RAMP-HT participant and is responsible for providing patient assessment and education, and coordinating frontline doctors care and allied health professionals services according to protocol. In addition to ensuring the delivery of appropriate treatment tailored to individual patient's needs and risks, these organizational changes allow focused yet coordinated interventions according to the expertise of each team members and are time-saving. Moreover, an electronic clinical data entry platform is available to enhance relay of information among the different team members. This feedback system prompts frontline doctors of the assessment results, enables them to review the process of care delivered to the respective patients and to adjust drug prescription as indicated. From the patient's perspective, multiple contacts with different team members help to reinforce knowledge, adherence and self-management. These strategies were postulated to contribute to the observed beneficial effect of RAMP-HT on BP, LDL-C and CVD risk in addition to the effects of various interventions provided.
Compared with previous studies, the mean BP reduction achieved in the RAMP-HT group after 12 months (SBP: −11.9 mmHg, DBP: −4.12 mmHg) was similar to those found in another cardiovascular risk management programme [16] and a nurse-led drug titration and education intervention [21], but greater than those of a nurse-led drug titration intervention or multidisciplinary intervention focusing on lifestyle alone [10,22]. Mendis found that implementation of the WHO CVD risk management package, which was a clinical decision support intervention consisting of risk stratification based on age, clinical history of CVD, diabetes, smoking and SBP and risk-guided drug therapy and lifestyle advices by primary care doctors according to standardized protocol, led to greater BP reduction (SBP: −11.0 to −13.3 mmHg; DBP: −5.4 to −6.1 mmHg) compared with control [16]. Both Rudd et al.[21] and Hill et al.[22] evaluated the effect of hypertension drug titration by nurses or community health workers according to standardized algorithms and demonstrated that this approach led to greater reduction in BP in a period of 6–36 months (Rudd: SBP: −14.2 mmHg, DBP: −6.5 mmHg; Hill: SBP: −8.2 mmHg; DBP: −4.0 mmHg); the greater BP reduction observed in Rudd's study could be explained by the additional nurse education on correct use of self-BP monitoring and drug compliance through telephone consultation [21]. On the other hand, the multidisciplinary lifestyle intervention in Mattila's study led to only a small but significant reduction in BP compared with control (SBP: −2.1 mmHg, DBP: −1.5 mmHg) [10]. Our findings further supported that algorithm-driven, multidisciplinary CVD risk assessment and risk-guided management involving patient education and drug titration was an effective way to improve BP control and was superior to lifestyle intervention or drug titration alone.
Significantly, although the RAMP-HT encompassed more interventions compared with these previous studies, an additive effect on BP reduction was not apparent. Moreover, the net difference in BP improvement between the intervention (RAMP-HT) and control group (usual care) found in our study (SBP: −0.84 mmHg, DBP: 0.03 mmHg) was much smaller than these studies (SBP: −3.74 to −8.50 mmHg, DBP: −1.53 mmHg to −6.4 mmHg), although the magnitude of improvement remained statistically significantly greater in the RAMP-HT group. This could be explained by the study design and the absence of an algorithm for hypertension drug titration by frontline doctors. Our study was an observational cohort study on the implementation of RAMP-HT as an additional but integrated component to usual GOPC care in the real-world primary care setting, as opposed to a randomized controlled trial [17]. First, adherence to RAMP-HT protocol would not be ideal in the presence of patient's and doctor's barriers. Second, as RAMP-HT was not a stand-alone programme, the allied health professional services, patient education via Patient Empowerment Programme and laboratory assessment were also accessible to usual care patients at their doctors’ discretion [23]. Furthermore, except from the very high-risk group with BP more than 160/100 mmHg despite on three or more antihypertensive medications or features suggestive of secondary hypertension who would be managed by specialists in family medicine, all the RAMP-HT participants and usual care hypertension patients were managed by the same group of primary care doctors working in the different GOPCs across Hong Kong using the same drug formulary. The only difference affecting the doctor's management would be the availability of feedback from RAMP-HT nurses and allied health professionals on CVD risks of RAMP-HT participants but not the usual care group. Because of this arrangement, a specific algorithm for antihypertensive drug titration only for RAMP-HT participants would neither be practical nor feasible. It was also highly probable that participation of these primary care doctors in the RAMP-HT improved their awareness on the needs for CVD-risk assessment, drug titration and referral to allied health services even when they were providing ‘usual care’ to hypertension patients not enrolled in RAMP-HT. These factors might bias the effects of RAMP-HT towards null as nearly comparable BP improvement was also observed in the usual care group (SBP: −11.0 mmHg; DBP: −4.2 mmHg). Nevertheless, considering that a significantly greater proportion of RAMP-HT patient achieved target BP than usual care group, which was a more meaningful outcome than mean BP reduction for healthcare providers, the clinical benefit of having the additional RAMP-HT services in addition to usual care and the use of feedback loop was still evident and important.
In addition to BP control, we demonstrated that RAMP-HT was also effective in improving LDL-C and CVD risks. Although hyperlipidaemia often coexists with hypertension and assessment of total CVD risk has been strongly advocated, very few hypertension intervention studies evaluated LDL-C or predicted 10-year CVD risk as outcomes of their interventions [14,15]. In the RAMP-HT, one important component of CVD risk management was the prescription of lipid-lowering agents to participants with highly predicted 10-year CVD risk more than 20% in addition to lifestyle advices. A significantly higher proportion of RAMP-HT participants were prescribed lipid-lowering agents after 12 months, possibly prompted by the feedback reminders on the CMS about the CVD risk of RAMP-HT participants. As a result, a significantly greater proportion of patients had achieved target LDL-C or improved LDL-C in the RAMP-HT group compared with the usual care group. Together with improved BP, the improved lipid profile contributed to a significantly greater reduction in the predicted 10-year CVD risks in the RAMP-HT group compared with usual care after 12 months of intervention.
The RAMP-HT is an organizational investment from the Hospital Authority to improve the quality of hypertension care in Hong Kong. Our findings confirmed that RAMP-HT, a protocol-driven multidisciplinary CVD-risk stratification based management, was effective in improving BP control, LDL-C and predicted 10-year CVD risk of patients with suboptimal BP control after 12 months when compared with usual care. Nevertheless, it was not yet certain if the observed benefits could be extrapolated to patients with stable control hypertension. Also, BP and LDL-C were only surrogate CVD markers. Therefore, a longer term follow-up is required to evaluate whether the intervention can lead to actual reduction in CVD events and to validate the effectiveness of RAMP-HT among different risk groups over a longer time span. The long-term impact of RAMP-HT on noncardiovascular complications such as renal failure and on healthcare resources and service utilization is yet to be evaluated. To attain the desired health benefits of the RAMP-HT in the real-world clinical setting, one must also ensure that the intended care has been provided; annual evaluation of quality of care and feedback on possible areas of improvement are essential.
Our study had several limitations. First, evaluation of the RAMP-HT was designed as a population-based matched cohort study as opposed to an experimental randomized control study. The aim of RAMP-HT is to improve population BP control through an optimized, coordinated use of existing resources in the public primary care setting; such set-up requires concerted efforts from various stakeholders including health policy-makers, frontline healthcare providers and patients with continual feedback from the research team to ensure its implementation in the real-world clinical setting. Therefore, conducting a participatory-action research instead of randomized control trial is the most appropriate, although it is well aware that unobserved potential confounders may affect the results, and blinding of healthcare providers and patients is not possible. Moreover, literatures had shown that similar results could be obtained from observational studies and RCTs. Second, not all the RAMP-HT participants nor usual care hypertension patients were included in the analysis. Patients with missing clinical or demographic data were excluded, and it was most possible that hypertension patients receiving suboptimal ‘usual care’ would not even have clinical or laboratory data to be included in the data analysis. Some RAMP-HT participants who could not be matched to control pairs were excluded at the matching phase. These may have biased the potential benefits of RAMP-HT. In addition, some patients with satisfactory BP control were enrolled into RAMP-HT during the studied period; we did not include them in our analysis because we hypothesized that these RAMP-HT participants would not be receiving additional RAMP-HT interventions to usual care in view of their good BP. Conversely, patients older than 80 years were excluded because BP and LDL-C targets for the elderly group remain controversial. Lastly, the predicted 10-year CVD risk, but not the incidence of CVD events, was evaluated in this study because a 12-month follow-up period was too short to observe CVD events. The predicted 10-year CVD risk was estimated by the Framingham function, which was derived from the US population. Yet, there is currently no CVD-risk prediction function available for Chinese hypertension patients. Thus, the estimated benefit in CVD-risk reduction may not be accurate. Further study with a longer follow-up period (e.g. 5 years) is needed to confirm the effectiveness of RAMP-HT by observed clinical events and whether such intervention is cost-effective.
In conclusion, among patients with suboptimal hypertension control, such structured, protocol-driven multidisciplinary RAMP-HT was more effective than usual care in achieving satisfactory control of BP and LDL-C, and reducing predicted 10-year CVD risk after 12 months of intervention. Long-term evaluation should be conducted to assess whether improvement in the clinical outcomes can be translated into actual reduction in CVD complications and mortalities in the real-world clinical setting, and whether the intervention is cost-effective.
ACKNOWLEDGEMENTS
The authors wish to acknowledge the contributions of the multidisciplinary risk-stratification based hypertension management programme teams at the Hospital Authority head office, chief of service in primary care and programme coordinator in each cluster and Statistics and Statistics and Workforce Planning Department at the Hong Kong Hospital Authority.
The current study has been funded by the Health and Health Services Research Fund, Food and Health Bureau, HKSAR Commissioned Research on Enhanced Primary Care Study (Ref. no: EPC-HKU-2). The funders had no role in study design, data collection and analysis, decision to publish or preparation of the manuscript.
Conflicts of interest
There are no conflicts of interest.
Reviewers’ Summary Evaluations
Reviewer 1
The Risk-Assessment-and-Management-Programme for patients with Hypertension (RAMP-HT) study tested the potential effects of a protocol-driven multidisciplinary risk assessment and management program in a large cohort of hypertensive patients at low-moderate risk (without diabetes or other comorbidities), who did not achieve optimal control of blood pressure and low-density lipoprotein cholesterol levels. The study demonstrated that this approach was more effective than usual care in achieving satisfactory control of BP and LDL-C levels, and reducing predicted 10-years cardiovascular risk at 12-month follow-up observation. Such educational and therapeutic strategy can be effectively applied in a setting of real practice, although in some selected Countries several economic limitations and regulatory rules may at least, in part, limit the clinical effectiveness of this approach.
Reviewer 2
The authors successfully implemented a nonrandomized multidisciplinary assessment-and-management program (RAMP-HT) for treated but uncomplicated hypertension with suboptimal BP control in primary care. RAMP-HT significantly improved the proportion of patients achieving target levels of SBP and LDL-cholesterol and reduced predicted 10-y Framingham CVD risk versus usual care after 12 months follow-up. However, the absolute difference between SBP, LDL-C and risk reductions comparing both strategies is very small. It remains to be proven whether implementation of such a nurse-led multidisciplinary program as an additional but integrated component of usual care in drug-treated hypertension with suboptimal BP will translate into considerable less CV events at a reasonable cost–benefits ratio.
Footnotes
Abbreviations: BP, blood pressure; CMS, Clinical Management System; CVD, cardiovascular disease; GOPCs, general out-patient clinics; HA, Hospital Authority; HT, hypertension; LDL-C, LDL-cholesterol; NNT, number needed to treat; RAMP-HT, risk assessment and management programme for hypertension; TC/HDL-C ratio, total cholesterol-to-HDL-cholesterol ratio; TG, triglyceride
REFERENCES
- 1.World Health Organization. A global brief on hypertension: silent killer, global public health crisis. World Health Day 2013. 2013. [Google Scholar]
- 2.World Health Organization. Causes of death 2008 summary tables. Geneva, Switzerland: World Health Organization; 2011. [Google Scholar]
- 3.Glynn LG, Murphy AW, Smith SM, Schroeder K, Fahey T. Interventions used to improve control of blood pressure in patients with hypertension. Cochrane Database Syst Rev 2010; 3:CD005182. [DOI] [PubMed] [Google Scholar]
- 4.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr, et al. The seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA 2003; 289:2560–2571. [DOI] [PubMed] [Google Scholar]
- 5.Wood D, Wray R, Poulter N, Williams B, Kirby M, Patel V, et al. JBS 2: Joint British Societies’ guidelines on prevention of cardiovascular disease in clinical practice. Heart 2005; 91:1–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hill MN, Miller NH. Compliance enhancement. A call for multidisciplinary team approaches. Circulation 1996; 93:4–6. [DOI] [PubMed] [Google Scholar]
- 7.Walsh JM, Sundaram V, McDonald K, Owens DK, Goldstein MK. Implementing effective hypertension quality improvement strategies: barriers and potential solutions. J Clin Hypertens 2008; 10:311–316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Glynn LG, Murphy AW, Smith SM, Schroeder K, Fahey T. Interventions used to improve control of blood pressure in patients with hypertension. London: The Cochrane Library; 2010. [DOI] [PubMed] [Google Scholar]
- 9.Clark CE, Smith LF, Taylor RS, Campbell JL. Nurse led interventions to improve control of blood pressure in people with hypertension: systematic review and meta-analysis. BMJ 2010; 341:c3995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mattila R, Malmivaara A, Kastarinen M, Kivelä S, Nissinen A. Effectiveness of multidisciplinary lifestyle intervention for hypertension: a randomised controlled trial. J Hum Hypertens 2003; 17:199–205. [DOI] [PubMed] [Google Scholar]
- 11.British Cardiac Society, British Hypertension Society, Diabetes UK, HEART UK, Primary Care Cardiovascular Society, Stroke Association. JBS 2: Joint British Societies’ guidelines on prevention of cardiovascular disease in clinical practice. Heart 2005; 91 Suppl 5:v1–v52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.D’Agostino RB, Vasan RS, Pencina MJ, Wolf PA, Cobain M, Massaro JM, et al. General cardiovascular risk profile for use in primary care: the Framingham Heart Study. Circulation 2008; 117:743–753. [DOI] [PubMed] [Google Scholar]
- 13.Padwal RS, Hemmelgarn BR, Khan NA, Grover S, McKay DW, Wilson T, et al. The 2009 Canadian Hypertension Education Program recommendations for the management of hypertension: Part 1 – Blood pressure measurement, diagnosis and assessment of risk. Can J Cardiol 2009; 25:279–286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ogden LG, He J, Lydick E, Whelton PK. Long-term absolute benefit of lowering blood pressure in hypertensive patients according to the JNC VI risk stratification. Hypertension 2000; 35:539–543. [DOI] [PubMed] [Google Scholar]
- 15.Kaczorowski J, Chambers LW, Dolovich L, Paterson JM, Karwalajtys T, Gierman T, et al. Improving cardiovascular health at population level: 39 community cluster randomised trial of Cardiovascular Health Awareness Program (CHAP). BMJ 2011; 342:d442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mendis S, Johnston SC, Fan W, Oladapo O, Cameron A, Faramawi MF. Cardiovascular risk management and its impact on hypertension control in primary care in low-resource settings: a cluster-randomized trial. Bull World Health Organ 2010; 88:412–419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yu EYT, Wan EYF, Chan KHY, Wong CKH, Kwok RLP, Fong DYT, et al. Evaluation of the quality of care of a multidisciplinary Risk Factor Assessment and Management Programme for Hypertension (RAMP-HT). BMC Fam Prac 2015; 16:71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rosenbaum PR, Rubin DB. The central role of the propensity score in observational studies for causal effects. Biometrika 1983; 70:41–55. [Google Scholar]
- 19.Food, Health Bureau HKSAR. Hong Kong reference framework for hypertension care for adults in primary care settings. 2013. [Google Scholar]
- 20.Wagner EH, Austin BT, Davis C, Hindmarsh M, Schaefer J, Bonomi A. Improving chronic illness care: translating evidence into action. Health Aff 2001; 20:64–78. [DOI] [PubMed] [Google Scholar]
- 21.Rudd P, Miller NH, Kaufman J, Kraemer HC, Bandura A, Greenwald G, et al. Nurse management for hypertension. A systems approach. Am J Hypertens 2004; 17:921–927. [DOI] [PubMed] [Google Scholar]
- 22.Hill MN, Han H-R, Dennison CR, Kim MT, Roary MC, Blumenthal RS, et al. Hypertension care and control in underserved urban African American men: behavioral and physiologic outcomes at 36 months. Am J Hypertens 2003; 16:906–913. [DOI] [PubMed] [Google Scholar]
- 23.Wong CKH, Wong WCW, Lam CLK, Wan YF, Wong WHT, Chung KL, et al. Effects of Patient Empowerment Programme (PEP) on clinical outcomes and health service utilization in type 2 diabetes mellitus in primary care: an observational matched cohort Study. PLoS One 2014; 9:e95328. [DOI] [PMC free article] [PubMed] [Google Scholar]


