Abstract:
Evidence suggests that providers are not adhering to current testosterone replacement therapy guidelines when treating male hypogonadism. Understanding the diagnosis and management of this condition is further complicated by conflicting recommendations among available guidelines. NPs must select and follow the best guideline recommendations available to optimally treat male hypogonadism.
Keywords: male hypogonadism, testosterone, testosterone deficiency, testosterone replacement therapy
Evidence suggests that providers are not adhering to current testosterone replacement therapy guidelines when treating male hypogonadism. Understanding diagnosis and management is further complicated by conflicting recommendations among available guidelines. NPs must select and follow the best guideline recommendations available to optimally treat this condition.
Figure.

No caption available.
Male hypogonadism (testosterone deficiency in men) is an increasingly common condition seen in primary care, with a prevalence rate as high as 38.7% in men age 45 and older.1 Despite many providers feeling less than confident in how to approach this issue, the rate of testosterone use in men over age 40 has increased from 0.81% in 2001 to 2.91% in 2011.2
NPs need to be aware of the indications and concerns regarding diagnosis, treatment, and management of male hypogonadism to provide the best care for their patients. Typically, these men present to the office setting seeking treatment for signs and symptoms such as depression, fatigue, loss of muscle mass or strength, decreased libido, and loss of nocturnal erections, which can make the diagnosis of male hypogonadism challenging because these symptoms commonly occur in a variety of other conditions (obesity, diabetes mellitus, metabolic syndrome).3
Male hypogonadism results when the testes produce inadequate amounts of testosterone (primary hypogonadism), when there is pituitary or hypothalamic deficiency (secondary hypogonadism), or with failure of biologic action (androgen resistance, hormone bioavailability, alterations in receptor sensitivity).4 Testosterone is responsible for the maintenance of secondary male characteristics; plays an important role in sexual desire and function; and impacts the brain, bones, muscles, and kidneys.3
Declines in testosterone may result in mood changes, depression, insomnia, fatigue, changes in cognition, osteopenia or osteoporosis, increased body fat, and decreased lean muscle mass.4 Because there is a natural, gradual decline in testosterone beginning at age 30, NPs need to be able to discern from a variety of underlying causes to effectively manage and treat male hypogonadism.
The Endocrine Society's clinical practice guideline is the most widely recognized guideline on treating male hypogonadism, although it has not been updated since it was published in 2010.5 Evidence exists that a significant number of providers, particularly those in primary care settings, are not following established guidelines.6-9 This leads to considerable inconsistencies in clinical practices for screening, diagnosing, treating, and managing testosterone replacement therapy (TRT) in adult males among specialists and primary care providers.
Between 2001 and 2011, Baillargeon and colleagues identified 74.72% of males prescribed TRT who had a documented testosterone level in the previous 12 months; men treated by endocrinology or urology practices were more likely to receive treatment according to clinical guideline recommendations than those treated in primary care and other specialties.6 Muram and colleagues reported similar findings between 2010 and 2012, determining that men were not having guideline-recommended follow-up measurements of testosterone following TRT.9
In the 6 months after the initiation of TRT, 54% of men did not have a testosterone level checked at all, 18% had only one level checked, and 27% had two or more testosterone measurements.9 A 2015 review of testosterone prescribing practices within the Department of Veterans Affairs (VA) concluded that only 3.1% of men treated for hypogonadism in the VA healthcare system had a proper diagnostic evaluation; 16.5% did not have any testosterone level testing, and some received therapy despite contraindications.7
A number of guidelines and publications related to the diagnosis and management of male hypogonadism were reviewed to determine consensus in directing a clinician's approach for this issue. The works reviewed included the International Society for Sexual Medicine's Process of Care for the Assessment and Management of Testosterone Deficiency in Adult Men, the Endocrine Society's clinical practice guideline on male hypogonadism, and additional works by Afiadata and Ellsworth and Lunenfeld and colleagues.5,10-12
This article provides a summary and comparison of available works to support practice decisions regarding screening, lab testing, considerations for prostate cancer and cardiovascular risks, and pharmacologic versus nonpharmacologic treatments related to TRT.
Guideline comparison of screening and presenting symptoms
None of the guidelines endorse universal screening of adult males for hypogonadism; there is also a lack of agreement regarding which patients warrant screening. Several of the guidelines suggest screening men with chronic diseases, though there are subtle differences.5,10,11 One guideline endorses screening for men presenting with hypogonadism symptoms, and another includes screening in opioid or glucocorticoid use, chronic disease, obesity, metabolic syndrome, and type 2 diabetes mellitus (T2DM).5,12
Vitamin D deficiency was endorsed as an additional screening indication for male hypogonadism.11 Although the other guidelines endorse screening in chronic disease, the International Society for Sexual Medicine (ISSM) guideline does not recommended systematic screening in men with increased fracture risk, reduced muscle strength, anxiety, depression, asthma, chronic obstructive pulmonary disease, or prostate disease.10
An observational cohort study noted that low testosterone levels are common in men who have diabetes mellitus or who are obese, suggesting a correlation between the conditions.13 A meta-analysis of cross-sectional studies determined a significant association between male hypogonadism and metabolic syndrome.14 Metabolic syndrome components (with the exception of hypertension) increase the risk of male hypogonadism, the most predictive of these being increased waist circumference.4 The ISSM guideline recommendation of systematic screening of all men with obesity, metabolic syndrome, and T2DM is supported by the results of these studies.10
Evaluating patients is a challenge, as symptoms of normal physiologic aging and male hypogonadism are not clearly differentiated. Further complicating the issue, the signs and symptoms of male hypogonadism are not exclusive and can result from many other existing conditions.4 Carruthers and colleagues found no relationship between diagnostic symptoms and initial testosterone levels.15
Most guidelines state that in order to accurately diagnose male hypogonadism, at least one subjective symptom (which may include changes in sleep, energy, mood, or affect; disturbances in physical, cognitive, and sexual function; and supporting lab values) must be present.5,10,11 Afiadata and Ellsworth describe presenting symptoms, which are not explicitly required for diagnosis, and endorse treatment only for symptomatic men.12
Sexual manifestations are prevalent and continue to be the main reported symptom, but there has been a significant increase in reported obesity, depression, anxiety, insomnia, and memory loss or impairment in hypogonadal men.16 The European Male Ageing Study (EMAS) reported only three symptoms associated with testosterone levels: erectile function, morning erections, and sexual thoughts.17 Corona and colleagues acknowledge that although signs and symptoms may vary, sexual symptoms must always be present for diagnosis, but none of the other guidelines reviewed specify this requirement.4
Testosterone measurements
It was evident in the literature reviewed that there has yet to be a clearly defined normal range for testosterone levels and at what point treatment is appropriate. Several works recommend TRT in symptomatic men with total testosterone (TT) under 8 nmol/L, and there is a common agreement among professional societies to treat men at this result as long as there are no contraindications.10,12,18,19
The Endocrine Society guideline recommends treatment when TT is less than the lower limit of the normal range as defined by the individual lab reporting the results (usually less than 9.0 to 9.8 nmol/L).5 Lunenfeld and colleagues recommend TRT consideration when TT is less than 12.1 nmol/L, and the EMAS recommends it when TT is less than 11 nmol/L.11,17 Afiadata and Ellsworth and the ISSM guideline endorse further investigation and evaluation when the TT level is more than 8 nmol/L, but Lunenfeld and colleagues report levels of less than 15 nmol/L as appropriate for TRT.10-12
Circadian rhythms impact testosterone levels, and the guidelines recommended testing in the morning, but the recommended times seem to vary between 7:00 a.m. and 11:00 a.m., 8:00 a.m. and 12:00 p.m., and 10:00 a.m. and 11:00 a.m.10-12 The Endocrine Society guideline vaguely specifies “morning” testosterone levels.5 The need for repeat measurements are agreed upon, but the timeline is not consistent. Most guidelines do not identify a specific time period for a repeat measurement, but a few recommend it be obtained 1 week after the initial level.5,9
Additional testing and screening
If low TT is confirmed, clinicians need to distinguish between primary (testicular) or secondary (pituitary-hypothalamic) male hypogonadism.5,9,10 Low TT levels with elevated follicle-stimulating hormone (FSH) and luteinizing hormone (LH) levels are seen in primary hypogonadism, whereas low TT levels with low normal LH levels are found in secondary hypogonadism.5 Elevated levels of LH and FSH have been associated with primary testicular failure and should be further explored to rule out related conditions such as Klinefelter syndrome (also known as XXY male); once these conditions are excluded, TRT should be considered.9,10,22,23
Identification of secondary hypogonadism necessitates further evaluation and testing to identify possible causes of hypothalamic or pituitary dysfunction, which include destructive or infiltrative disease, medication use, nutritional deficiency, hyperprolactinemia, hemochromatosis, and pituitary lesions.5,9,10 Identified causes should be managed as per recommendations; if there are no identifiable causes, initiation of TRT should be considered.5,10,20,21
A subtle but notable difference between guidelines is the variation of other lab screenings suggested in the diagnostic workup. The ISSM guideline recommends that when low TT levels are identified, primary and secondary hypogonadism should be evaluated by obtaining LH and prolactin levels at the same time as the second TT level, also including sex hormone binding globulin (SHBG) for older or obese men.10 Two guidelines recommend obtaining LH and FSH levels, then considering a prolactin level if the second TT level is below normal.5,12 Lunenfeld and colleagues recommend LH and prolactin levels if TT is less than 5.2 nmol/L or when a primary tumor is suspected.11 Afiadata and Ellsworth also suggest considering pituitary function testing.12
A portion of TT is bound to SHBG and not biologically active. As SHBG levels increase, free or bioavailable testosterone decreases. When TT levels are in the low-normal range and altered SHBG levels are suspected (in thyroid disease, diabetes, obesity, chronic illness, or older age), several guidelines recommend free or bioavailable testosterone measurements to discern what portion of TT is biologically active.5,11,12 The ISSM guideline recommends directly checking SHBG levels for older or obese men after the first decreased testosterone measurement.10 If the testosterone level is more than 8 nmol/L but less than 12 nmol/L, and the patient has bothersome symptoms and/or an elevated SHBG, the ISSM guideline recommends further evaluation.10
Prostate health considerations
Digital rectal exam (DRE) and prostate-specific antigen (PSA) screening prior to initiation of TRT is addressed in all of the guidelines, but a consistent recommendation does not exist. The ISSM guideline recommends DRE only in men over age 40; the Endocrine Society guideline and Afiadata and Ellsworth recommend DRE in men age 40 and over with a baseline PSA greater than 0.6 ng/mL; Lunenfeld and colleagues recommend DRE and PSA in all men before starting TRT.5,10-12
A 2013 systematic review and meta-analysis analyzing the effect of TRT on prostate growth found no significant change in the four determinants of prostate growth (prostate volume, PSA levels, maximum flow rate, and International Prostate Symptom Score [IPSS]) in the 16 studies comparing TRT and placebo.22
A 2015 systematic review and meta-analysis of 15 studies examining the effect of TRT on PSA levels of currently treated hypogonadal men determined that increases in PSA levels were not associated with TRT, and elevated PSA levels posttreatment were comparable between control and treatment groups.23 According to this study, normal testosterone levels may actually provide protection from prostate cancer, and low testosterone levels may place patients at higher risk for developing prostate cancer. The authors concluded that existing evidence, albeit insufficient, does not demonstrate that prostate cancer risk is influenced by TRT.23
Cardiovascular health considerations
The ISSM guideline states there is no change in TRT treatment approach in men with stable cardiovascular disease.10 Other guidelines do not specifically address cardiovascular risk or TRT in men with cardiovascular disease, although they do agree that poorly controlled or uncontrolled heart failure and an elevated hematocrit level are contraindications to TRT.5,11 Two guidelines do not address cardiovascular risk factors, suggesting insufficient literature available.5,11
Table.
Some studies suggest that cardiovascular risk increases with TRT, though each of these has largely been deemed invalid.10,24-29 Current evidence does not support a concern regarding increased cardiovascular risk with TRT.10,15,28,29 The FDA requires labeling related to the possible increased risk of myocardial infarction and stroke with the use of testosterone products and advises providers to use TRT only in cases of pathologic loss of testosterone, not that which occurs as part of the normal aging process.30
The ISSM guideline addresses each of the studies suggesting cardiovascular risk with TRT, adverse cardiovascular risk and outcomes associated with male hypogonadism, and literature that identifies cardiovascular benefits with TRT in hypogonadal men.10 Miner and colleagues found that middle-aged hypogonadal men had higher cardiometabolic risk factors, suggesting that untreated hypogonadism increases cardiovascular risks.31
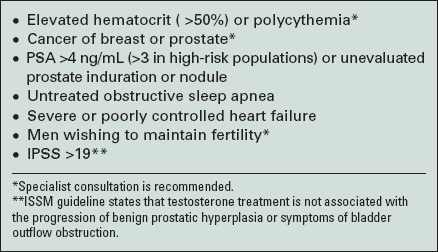
The ISSM guideline is careful to state there are not enough available trials to draw definitive conclusions. Both the ISSM guideline and Afiadata and Ellsworth conclude that available literature suggests TRT does not impose increased cardiovascular risk and may actually provide protective cardiovascular benefits (see Contraindications to TRT).10,12
Nonpharmacologic treatment
Nonpharmacologic treatment of male hypogonadism is recommended by the ISSM guideline.10 Several guidelines do not identify or endorse any nonpharmacologic interventions.5,11,12
Testosterone synthesis can be improved with lifestyle modifications, weight loss, treatment of sleep apnea, and discontinuation of medications such as carbamazepine and opioids.10 Corona and colleagues surmised that weight loss can improve testosterone levels and even recommend that this be the primary approach in treating male hypgonadism.4 The ISSM guideline acknowledges that adherence with lifestyle modifications is generally low, and unless providers are confident in their patients' commitment to diet and activity changes, drug treatment for testosterone therapy should be initiated.10
Discussion
Of the guidelines reviewed, the ISSM guideline appears to be the most current, with over half of its 133 referenced works published in 2010 or later. This represents newer literature that was not available when the Endocrine Society published their guidelines in 2010. In nearly all areas compared, the ISSM guideline is more comprehensive regarding the evaluation of potential contraindications when initiating or continuing TRT.
NPs need to be able to discern between the symptoms of male hypogonadism and those of normal physiologic aging. The guidelines vary, as some require presenting symptoms for diagnosis and treatment and some do not. Only one study specifically requires at least one sexual symptom be present for diagnosis.17
There is no agreement among the reviewed guidelines on a serum TT level that is diagnostic for male hypogonadism; new research has not provided enough data to support one guideline over another. Generally, guidelines advise that TT levels less than 8 nmol/L warrant treatment; levels over 8 and less than 12 nmol/L should be considered, especially in symptomatic men; and levels over 12 nmol/L are not appropriate for TRT.5,10-12,18,19
The variance between suggested timing of performing lab tests for testosterone levels is recognized, but a morning lab draw is clearly indicated. Due to the natural variances in testosterone levels, each guideline recommends a repeat confirmatory measurement be obtained prior to initiation of treatment; some do not specify a time period for this second TT measurement, and some recommend it 1 week after the initial level.
There is variance between the guidelines as to which tests (FSH, LH, prolactin, or SHBG) are indicated in differentiating primary and secondary hypogonadism causes. NPs must balance the need for lab information with cost and patient convenience. The approach endorsed by the ISSM guideline includes a greater number of lab assessments earlier in the process, but it also simplifies the process because fewer lab assessments are optional and subject to consideration by the clinician.
In regards to PSA and DRE, NPs should consider the current guidelines from the American College of Physicians, American Urological Association (AUA), and U.S. Preventive Services Task Force that address prostate cancer screening in average-risk men.32-34 DRE and PSA screening prior to initiation of TRT is addressed in all of the guidelines (although a consistent recommendation does not exist). The lack of evidence regarding prostate cancer risk with TRT leaves the NP to consider obtaining a PSA for men over age 40 before treatment, at each follow-up visit, and to perform a DRE based on individual risks and preferences. The Endocrine Society has additional recommendations for men with elevated PSA and indications for urologic consultation for elevated measurement within 12 months of testosterone treatment, detection of prostate abnormality on DRE, and AUA/International Prostate Symptom Score (IPSS) over 19.5
Generally stated, the guidelines do not support TRT in men with poorly or uncontrolled heart failure. The guidelines that further address cardiovascular risk state that existing evidence suggests there is no increased risk with TRT and TRT may actually provide cardioprotective benefits. However, it is recognized that these findings need to be confirmed through additional research.
The two hallmark studies most responsible for raising concern in the media and hesitation among clinicians about the cardiovascular risk with TRT have been widely dispelled in recently published high-quality systematic reviews.35 As with any treatment, clinicians must monitor and evaluate the effects of TRT. Adverse reactions (specifically elevated hematocrit) are closely tied to overtreatment and must be observed for and responded to appropriately, which may require discontinuation of TRT.
NPs should acknowledge and consider other ways to improve testosterone synthesis in their care for patients with male hypogonadism. Lifestyle modifications resulting in weight loss, discontinuation of certain medications, and treatment of sleep apnea should be considered prior to initiation of TRT (particularly in motivated patients) and as adjunctive treatment in those receiving TRT.
Conclusions and recommendations
In order to safely diagnose and manage male hypogonadism in the primary care setting, clinicians must be aware of the guidelines, the differences between them, and the implications behind the variety of approaches. The lack of congruency between the guidelines highlights the need for consistent and optimal diagnosis and management of male hypogonadism in primary care settings. The variety of approaches may contribute to the lack of clinician alignment with current recommendations.
Further research may help identify additional reasons behind this low level of guideline adherence. There is simply not enough published evidence available at this time focused on practice outcomes for the variety of approaches to definitively determine which specific recommendations are superior. Further investigation and research is needed to either support or dispute the existing guidelines.
REFERENCES
- 1.Mulligan T, Frick MF, Zuraw QC, Stemhagen A, Mcwhirter C. Prevalence of hypogonadism in males aged at least 45 years: the HIM study. Int J Clin Pract. 2006;60(7):762–769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Baillargeon J, Urban RJ, Ottenbacher KJ, Pierson KS, Goodwin JS. Trends in androgen prescribing in the United States, 2001 to 2011. JAMA Intern Med. 2013;173(15):1465–1466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kirby M. Testosterone deficiency. Pract Nurse. 2015;45(11):32–36. [Google Scholar]
- 4.Corona G, Rastrelli G, Maggi M. Diagnosis and treatment of late-onset hypogonadism: systematic review and meta-analysis of TRT outcomes. Best Pract Res Clin Endocrinol Metab. 2013;27(4):557–579. [DOI] [PubMed] [Google Scholar]
- 5.Bhasin S, Cunningham GR, Hayes FJ, et al. Testosterone therapy in men with androgen deficiency syndromes: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2010;95(6):2536–2559. [DOI] [PubMed] [Google Scholar]
- 6.Baillargeon J, Urban RJ, Kuo YF, et al. Screening and monitoring in men prescribed testosterone therapy in the U.S., 2001-2010. Public Health Rep. 2015;130(2):143–152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jasuja GK, Bhasin S, Reisman JI, Berlowitz DR, Rose AJ. Ascertainment of testosterone prescribing practices in the VA. Med Care. 2015;53(9):746–752. [DOI] [PubMed] [Google Scholar]
- 8.Malik RD, Lapin B, Wang CE, Lakeman JC, Helfand BT. Are we testing appropriately for low testosterone? Characterization of tested men and compliance with current guidelines. J Sex Med. 2015;12(1):66–75. [DOI] [PubMed] [Google Scholar]
- 9.Muram D, Zhang X, Cui Z, Matsumoto AM. Use of hormone testing for the diagnosis and evaluation of male hypogonadism and monitoring of testosterone therapy: application of hormone testing guideline recommendations in clinical practice. J Sex Med. 2015;12(9):1886–1894. [DOI] [PubMed] [Google Scholar]
- 10.Dean JD, McMahon CG, Guay AT, et al. The International Society for Sexual Medicine's process of care for the assessment and management of testosterone deficiency in adult men. J Sex Med. 2015;12(8):1660–1686. [DOI] [PubMed] [Google Scholar]
- 11.Lunenfeld B, Mskhalaya G, Kalinchenko S, Tishova Y. Recommendations on the diagnosis, treatment and monitoring of late-onset hypogonadism in men: a suggested update. Aging Male. 2013;16(4):143–150. [DOI] [PubMed] [Google Scholar]
- 12.Afiadata A, Ellsworth P. Testosterone replacement therapy: who to evaluate, what to use, how to follow, and who is at risk. Hosp Pract (1995). 2014;42(5):69–82. [DOI] [PubMed] [Google Scholar]
- 13.Saad F, Haider A, Doros G, Traish A. Long-term treatment of hypogonadal men with testosterone produces substantial and sustained weight loss. Obesity (Silver Spring). 2013;21(10):1975–1981. [DOI] [PubMed] [Google Scholar]
- 14.Corona G, Monami M, Rastrelli G, et al. Testosterone and metabolic syndrome: a meta-analysis study. J Sex Med. 2011;8(1):272–283. [DOI] [PubMed] [Google Scholar]
- 15.Carruthers M, Cathcart P, Feneley MR. Evolution of testosterone treatment over 25 years: symptom responses, endocrine profiles and cardiovascular changes. Aging Male. 2015;18(4):217–227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gooren LJ, Behre HM. Diagnosing and treating testosterone deficiency in different parts of the world: changes between 2006 and 2010. Aging Male. 2012;15(1):22–27. [DOI] [PubMed] [Google Scholar]
- 17.Huhtaniemi IT. Andropause: lessons from the European Male Ageing Study. Ann Endocrinol (Paris). 2014;75(2):128–131. [DOI] [PubMed] [Google Scholar]
- 18.Buvat J, Maggi M, Guay A, Torres LO. Testosterone deficiency in men: systematic review and standard operating procedures for diagnosis and treatment. J Sex Med. 2013;10(1):245–284. [DOI] [PubMed] [Google Scholar]
- 19.Wu FC, Tajar A, Beynon JM, et al. Identification of late-onset hypogonadism in middle-aged and elderly men. N Engl J Med. 2010;363(2):123–135. [DOI] [PubMed] [Google Scholar]
- 20.Dandona P, Rosenberg MT. A practical guide to male hypogonadism in the primary care setting. Int J Clin Pract. 2010;64(6):682–696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lunenfeld B, Arver S, Moncada I, Rees DA, Schulte HM. How to help the aging male? Current approaches to hypogonadism in primary care. Aging Male. 2012;15(4):187–197. [DOI] [PubMed] [Google Scholar]
- 22.Cui Y, Zhang Y. The effect of androgen-replacement therapy on prostate growth: a systematic review and meta-analysis. Eur Urol. 2013;64(5):811–822. [DOI] [PubMed] [Google Scholar]
- 23.Kang DY, Li HJ. The effect of testosterone replacement therapy on prostate-specific antigen (PSA) levels in men being treated for hypogonadism: a systematic review and meta-analysis. Medicine (Baltimore). 2015;94(3):e410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Basaria S, Coviello AD, Travison TG, et al. Adverse events associated with testosterone administration. N Engl J Med. 2010;363(2):109–122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Finkle WD, Greenland S, Ridgeway GK, et al. Increased risk of non-fatal myocardial infarction following testosterone therapy prescription in men. PLoS One. 2014;9(1):e85805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Vigen R, O'Donnell CI, Barón AE, et al. Association of testosterone therapy with mortality, myocardial infarction, and stroke in men with low testosterone levels. JAMA. 2013;310(17):1829–1836. [DOI] [PubMed] [Google Scholar]
- 27.Xu L, Freeman G, Cowling BJ, Schooling CM. Testosterone therapy and cardiovascular events among men: a systematic review and meta-analysis of placebo-controlled randomized trials. BMC Med. 2013;11(1):108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Maganty A, Osterberg EC, Ramasamy R. Hypogonadism and testosterone therapy: associations with cardiovascular risk. Am J Mens Health. 2015;9(4):340–344. [DOI] [PubMed] [Google Scholar]
- 29.Morgentaler A, Miner MM, Caliber M, Guay AT, Khera M, Traish AM. Testosterone therapy and cardiovascular risk: advances and controversies. Mayo Clin Proc. 2015;90(2):224–251. [DOI] [PubMed] [Google Scholar]
- 30.U. S. Food and Drug Administration. FDA Drug Safety Communication: FDA cautions about using testosterone products for low testosterone due to aging; requires labeling change to inform of possible increased risk of heart attack and stroke with use. 2014. www.fda.gov/downloads/Drugs/DrugSafety/UCM436270.pdf. [DOI] [PubMed]
- 31.Miner MM, Khera M, Bhattacharya RK, Blick G, Kushner H. Baseline data from the TRiUS Registry: symptoms and comorbidities of testosterone deficiency. Postgrad Med. 2011;123(3):17–27. [DOI] [PubMed] [Google Scholar]
- 32.Qaseem A, Barry MJ, Denberg TD, Owens DK, Shekelle P, Clinical Guidelines Committee of the American College of Physicians Screening for prostate cancer: a guidance statement from the Clinical Guidelines Committee of the American College of Physicians. Ann Intern Med. 2013;158(10):761–769. [DOI] [PubMed] [Google Scholar]
- 33.Carter HB, Albertsen PC, Barry MJ, et al. Early detection of prostate cancer: AUA guideline. J Urol. 2013;190(2):419–426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Moyer VA; U.S. Preventive Services Task Force. Screening for prostate cancer: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2012;157(2):120–134. [DOI] [PubMed] [Google Scholar]
- 35.Corona GG, Rastrelli G, Maseroli E, Sforza A, Maggi M. Testosterone replacement therapy and cardiovascular risk: a review. World J Mens Health. 2015;33(3):130–142. [DOI] [PMC free article] [PubMed] [Google Scholar]


