Abstract
Purpose
To assess whether combination therapy (CT) reduces retreatments when compared to ranibizumab monotherapy (RM), while safely maintaining similar vision outcomes.
Methods
In this 24-month trial, patients with age-related macular degeneration (AMD) were randomized to 1) quarter-fluence or 2) half-fluence triple therapy (verteporfin photodynamic therapy [vPDT] + ranibizumab + dexamethasone), 3) half-fluence double therapy (vPDT + ranibizumab), or 4) RM. The primary outcomes were number of retreatment visits and change from baseline in visual acuity (VA) at 12 months.
Results
One hundred sixty-two subjects enrolled. There were 4.0 (P=0.02), 3.2 (P<0.001), 4.1 (P=0.03), and 5.7 retreatment visits through month 12, and 5.9 (P=0.03), 4.3 (P<0.001), 5.9 (P=0.02) and 8.7 through month 24, in groups 1, 2, 3, and 4, respectively (P-value comparing with RM). Month 12 VA score change from baseline (95% confidence interval) was +3.6 (−0.9 to +8.1), +6.8 (+2.4 to +11.1), +5.0 (+0.6 to +9.3), and +6.5 (+1.7 to +11.4), respectively.
Conclusion
CT resulted in significantly fewer retreatment visits than a RM regimen at months 12 and 24. VA results appeared similar although wide confidence intervals preclude conclusions regarding vision outcomes.
Keywords: age-related macular degeneration (AMD), combination therapy, ranibizumab, photodynamic therapy (PDT), verteporfin
Introduction
Intravitreal ranibizumab (IVR; Lucentis®; Genentech, South San Francisco, CA USA) monotherapy is a proven effective treatment for choroidal neovascularization (CNV) due to age-related macular degeneration (AMD),1–2 limitations include the need for continued monthly injections for 1 year or longer to achieve the best outcomes, cost, risk of infection, and the potential inability of patients to attend monthly treatment visits.1–4
Combination therapy (CT) with verteporfin photodynamic therapy (vPDT) and IVR with or without intravitreal dexamethasone (IVD) for neovascular AMD may reduce the number and frequency of treatments while preserving vision gains associated with antivascular endothelial growth factor (VEGF) alone.5–15 Multiple retrospective case series of patients with CNV treated with double therapy (vPDT and intravitreal anti-VEGF) have demonstrated fewer retreatments than would be expected with monotherapy with stabilized or improved visual acuity (VA).5,8,12 Williams et al and Hatz et al both compared double therapy with IVR monotherapy in randomized, prospective 1-year studies and demonstrated similar VA results with fewer retreatments in the CT cohorts.13,14 Triple therapy (vPDT, intravitreal anti-VEGF, and steroid) has similarly demonstrated benefit in retrospective and prospective studies.9,15 Neovascular AMD has a multifactorial etiology and CT targets different aspects of the disease, including abnormal VEGF production, inflammation, and increased vascular permeability.16,17
The objective of Reduced Fluence Visudyne-Anti-VEGF-Dexamethasone In Combination for AMD Lesions (RADICAL) was to determine if CT (double and triple therapy) reduces retreatment visits compared with ranibizumab monotherapy (RM) while maintaining similar vision outcomes and an acceptable safety profile.
Materials and methods
RADICAL was a phase II, exploratory, multicenter, randomized, single-masked clinical study that included subjects with CNV due to AMD. The study design was reviewed by an advisory group (comprising selected study investigators), the Institutional Review Board (IRB) of the participating clinical centers, and an independent data and safety monitoring committee (DSMC). Approving IRBs included Western IRB, Scott & White IRB, IRB of Wills Eye Hospital, The Research Ethic Board, Capital District Health Authority – Research Ethics Board, Clinical Research Ethics Board, Research Ethics Review Committee of the College of Physicians and Surgeons of Alberta, and Health Sciences Research Ethics Board. The DSMC reviewed the data approximately every 6 months. No prospectively defined stopping rules were employed. The study was registered on ClinicalTrials.gov as NCT00492284. Support for this trial was provided by QLT Inc.
Study conduct
Twenty-six clinical centers enrolled subjects from July 2007 to May 2008. After informed consent was obtained, vision testing, color photographs, fluorescein angiograms (FA), optical coherence tomography (OCT), intraocular pressure (IOP), and clinical examination were performed. Key inclusion criteria were ≥50 years of age; active subfoveal CNV due to AMD ≥50% of the total lesion; treatment-naive in the study eye, best-corrected VA letter score 73–25 (approximate Snellen equivalent of 20/40–20/320); and lesion greatest linear dimension ≤5,400 µm.
Subjects who satisfied eligibility criteria were randomly assigned to one of four treatment groups (1:1:1:1 ratio): 1) quarter-fluence vPDT (15 J/cm2; 180 mW/cm2 for 83 seconds) + IVR (0.5 mg) + IVD (0.5 mg) (quarter-fluence triple therapy); 2) half-fluence vPDT (25 J/cm2; 300 mW/cm2 for 83 seconds) + IVR + IVD (half-fluence triple therapy); 3) half-fluence vPDT + IVR (half-fluence double therapy); and 4) RM. Subjects in the CT groups received one initial treatment at day 0. Subjects assigned to RM received three initial IVR treatments (day 0, months 1 and 2). Random treatment assignments were stored in sealed opaque envelopes. Randomization was stratified by study center and baseline VA letter score (upper strata of 73–51 [approximate Snellen equivalent of 20/40–20/100] and lower strata of 50–25 [approximate Snellen equivalent of 20/100–20/320]).
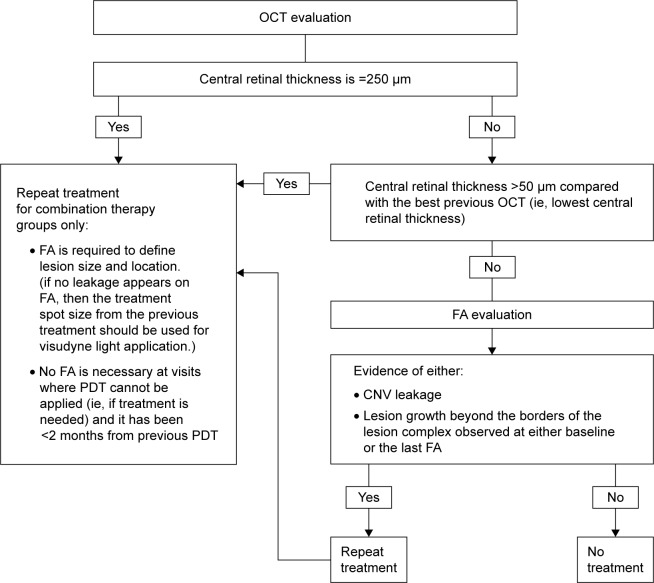
Vision examiners and evaluating physicians were masked to treatment assignment. Evaluating physicians assessed OCT and FA to determine the need for retreatment after the mandatory treatment(s), according to specified criteria (Figure 1). Treating investigators and study coordinators were unmasked and responsible for randomization, treatment administration, and study assessments other than VA and retreatment.
Figure 1.
Results of a phase II randomized trial retreatment criteria.
Abbreviations: CNV, choroidal neovascularization; FA, fluorescein angiography; OCT, optical coherence tomography; PDT, photodynamic therapy.
Subjects had study visits every month for 12 months, and then at least every 3–24 months. Subjects underwent follow-up procedures and assessment for retreatment according to a standard protocol. CT subjects were assessed for retreatment at every monthly visit. If retreatment was necessary, the assigned CT was administered, provided that the last CT was given >55 days before. If not, IVR was administered. RM subjects were assessed for retreatment beginning at the month 3 visit. If retreatment was necessary, the subject was treated with RM. For analyses of retreatment, any day that any study treatment was administered after day 0 was considered to be a retreatment visit.
Statistical methods
The primary outcomes were mean number of retreatment visits and mean change from baseline in VA letter score at month 12 study visit using an intent to treat (ITT) analysis. The sample size of 40 subjects per treatment group in this exploratory study was estimated to be adequate (>80% power) to detect a mean difference of >1.5 in number of retreatment visits between groups which is considered clinically significant. An appropriately powered noninferiority comparison of VA change from baseline would only be feasible in a larger study due to the large variation and small acceptable noninferiority margin in VA change from baseline.
Comparison analysis was performed between each CT group separately and RM at month 12 (primary analyses) and month 24. A two-sided t-test was utilized with alpha-level of 0.05. No alpha adjustment was made for multiple comparisons because the comparisons were intended for reference only in the context of an exploratory study. A 95% confidence interval (CI) between treatment groups was provided.
Exploratory analyses were done for the mean number of retreatment procedures (number of vPDT, IVR, and IVD), companion to the mean number of retreatment visits.
ITT analyses were done and included all subjects randomly assigned to therapy; missing VA letter scores were imputed using last observation carried forward (LOCF). To confirm results, analysis was performed with observed values without imputation of missing values and observed values excluding subjects with predefined protocol deviations. Results were similar to the ITT analyses.
Results
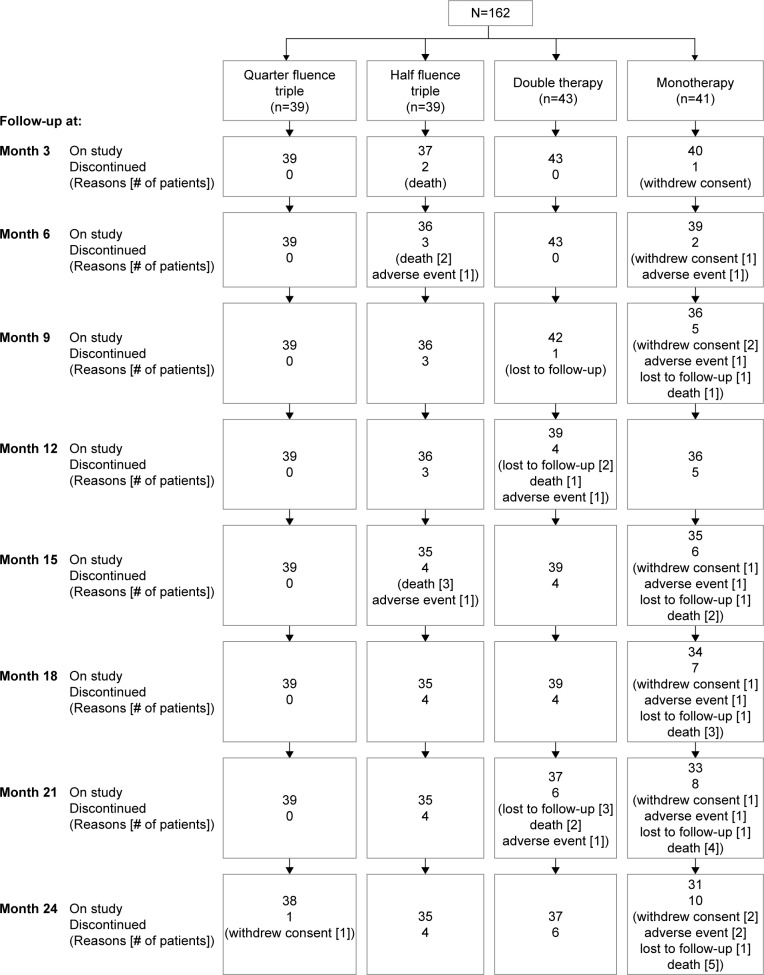
One hundred sixty-two eyes (162 subjects) were enrolled: 1) 39 subjects, quarter-fluence triple therapy group; 2) 39 subjects, half-fluence triple therapy group; 3) 43 subjects, half-fluence double therapy group; and 4) 41 subjects, RM. Baseline characteristics for these subjects appeared balanced except that the triple therapy groups had more predominantly classic lesions than the other groups (59%, 49%, 33%, and 37% in groups 1, 2, 3, and 4, respectively). In the CT groups, 92%–100% of subjects completed to month 12, compared with 88% in the RM group (Figure 2).
Figure 2.
Subject disposition through 24 months.
Retreatment
Table 1 summarizes treatment through months 12 and 24. The number of retreatment visits in all CT groups was lower than in the RM group at both months 12 and 24 (P<0.03 and P<0.001 for the half-fluence triple therapy group; Figure 3). The mean number of individual retreatment procedures received through months 12 and 24 was higher in the CT groups than in the RM group.
Table 1.
Summary of treatmenta
| Month 12
|
Month 24
|
|||||||
|---|---|---|---|---|---|---|---|---|
| Quarter-fluence triple (N=39) | Half-fluence triple (N=39) | Half-fluence double (N=43) | Ranibizumab (N=41) | Quarter-fluence triple (N=39) | Half-fluence triple (N=39) | Half-fluence double (N=43) | Ranibizumab (N=41) | |
| Number of treatment visitsb | 4.97 | 4.22 | 5.13 | 6.74 | 6.92 | 5.34 | 6.92 | 9.68 |
| 95% CI | 3.96–5.98 | 3.37–5.08 | 4.16–6.10 | 5.65–7.82 | 5.35–8.49 | 4.09–6.60 | 5.46–8.38 | 7.74–11.62 |
| P-valuec | 0.02 | <0.001 | 0.03 | – | 0.03 | <0.001 | 0.02 | – |
| Number of proceduresb | 12.62 | 10.75 | 8.97 | 6.74 | 17.55 | 14.00 | 12.16 | 9.68 |
| 95% CI | 10.36–14.87 | 8.94–12.56 | 7.48–10.47 | 5.65–7.82 | 14.00–21.11 | 11.09–16.91 | 9.88–14.45 | 7.74–11.62 |
| P-valueb | <0.001 | <0.001 | 0.02 | – | <0.001 | 0.01 | 0.10 | – |
| Number of retreatment visits (excludes day 0) | 3.97 | 3.22 | 4.13 | 5.74 | 5.92 | 4.34 | 5.92 | 8.68 |
| 95% CI | 2.96–4.98 | 2.37–4.08 | 3.16–5.10 | 4.65–6.82 | 4.35–7.49 | 3.09–5.60 | 4.46–7.38 | 6.74–10.62 |
| P-valuec | 0.02 | <0.001 | 0.03 | – | 0.03 | <0.001 | 0.02 | – |
| Number of procedures (excludes day 0) | 9.62 | 7.75 | 6.97 | 5.74 | 14.55 | 11.00 | 10.16 | 8.68 |
| 95% CI | 7.36–11.87 | 5.94–9.56 | 5.48–8.47 | 4.65–6.82 | 11.00–18.11 | 8.09–13.91 | 7.88–12.45 | 6.74–10.62 |
| P-valueb | 0.003 | 0.06 | 0.18 | – | 0.01 | 0.18 | 0.33 | – |
| Number of retreatment visits (excludes all mandatoryd) | 3.97 | 3.22 | 4.13 | 3.79 | 5.92 | 4.34 | 5.92 | 6.81 |
| 95% CI | 2.96–4.98 | 2.37–4.08 | 3.16–5.10 | 2.72–4.87 | 4.36–7.49 | 3.09–5.60 | 4.46–7.38 | 4.89–8.72 |
| P-valueb | 0.80 | 0.40 | 0.64 | – | 0.46 | 0.33 | 0.45 | – |
| Number of procedures (excludes all mandatoryd) | 9.62 | 7.75 | 6.97 | 3.79 | 14.55 | 11.00 | 10.16 | 6.81 |
| 95% CI | 7.36–11.87 | 5.94–9.56 | 5.48–8.47 | 2.72–4.87 | 11.00–18.11 | 8.09–13.91 | 7.88–12.48 | 4.89–8.72 |
| P-valueb | <0.001 | <0.001 | <0.001 | – | <0.001 | 0.02 | 0.03 | – |
Notes: In the combination therapy groups, a ranibizumab injection alone resulted in the visit being considered a treatment/retreatment visit.
The primary variable is highlighted. All other analyses were exploratory.
All treatments (including day 0) through month 12.
Compared with RM.
Excludes day 0 treatment in all groups and months 1 and 2 treatments in the RM group.
Abbreviations: CI, confidence interval; RM, ranibizumab monotherapy.
Figure 3.
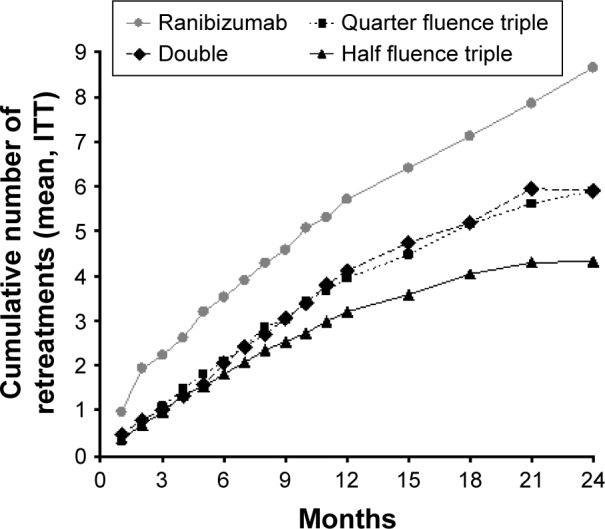
Cumulative mean number of visits at which retreatment was applied (excluding day 0).
Abbreviation: ITT, intent to treat.
Vision outcomes
At month 12, mean VA change from baseline (95% CI), was +3.6 (−0.9 to +8.1), +6.8 (+2.4 to +11.1), +5.0 (+0.6 to +9.3), and +6.5 (+1.7 to +11.4) in groups 1, 2, 3, and 4, respectively (Figure 4). Outcomes compared with the RM group were not statistically significant (P≥0.38). The difference in mean VA letter score change from baseline to 12 months between groups 1, 2, or 3, respectively, and the RM group (and 95% CI) was −2.9 (−9.5 to 3.6), 0.3 (−6.2 to 6.7), and −1.6 (−8.0 to 4.9), with the lower bounds of the 95% CI, to evaluate for noninferiority outcomes, lying below −5.0 in all three groups.
Figure 4.
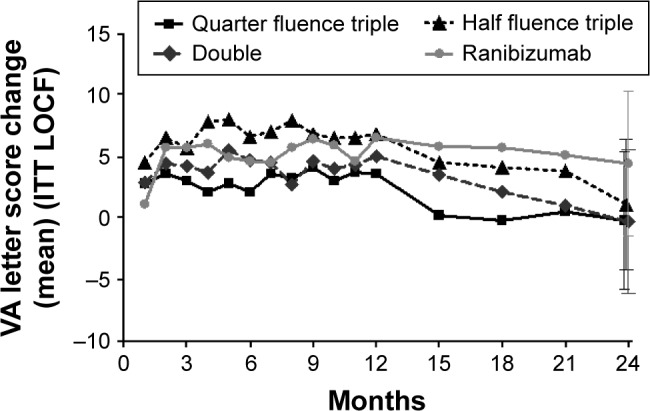
Mean visual acuity letter score change from baseline through 12 months (1 line equals 5 letters; ITT LOCF).
Abbreviations: ITT, intent to treat; LOCF, last observation carried forward.
At the month 24 examination, mean VA letter score change from baseline (95% CI), was −0.2 (−5.7 to +5.4), +1.1 (−4.3 to +6.4), −0.3 (−6.2 to +5.6), and +4.4 (−1.5 to +10.2) in groups 1–4, respectively (Figure 4).
Safety
The overall incidence of adverse events (AE) was similar among treatment groups (Table 2). However, the incidence of treatment-associated AE was higher in the CT groups (44%–49%) than in the RM group (27%). This higher incidence of treatment-associated AE with CT was due to systemic events of infusion-related pain (such as back pain), intravenous injection site events and ocular AE. Despite the protocol requiring protection from direct sunlight for 5 days (corresponding to the vPDT label), two photosensitivity reactions were reported. No subject discontinued the study because of infusion-related, injection-site, or photosensitivity events.
Table 2.
Summary of AE
| AE category | Number of subjects (%)
|
|||
|---|---|---|---|---|
| Quarter-fluence triple (N=39) | Half-fluence triple (N=39) | Half-fluence double (N=43) | Ranibizumab (N=41) | |
| All AE | 38 (97) | 36 (92) | 37 (86) | 40 (98) |
| All ocular AE | 26 (67) | 25 (64) | 26 (61) | 25 (61) |
| SAE (not treatment associated) | 10 (26) | 13 (33) | 15 (35) | 19 (46) |
| Deaths | 0 | 3 (8) | 2 (5) | 5 (12) |
| Withdrawal due to SAE | 0 | 1 (3)a | 0 | 0 |
| Treatment-associated AEb | 19 (49) | 17 (44) | 20 (47) | 11 (27) |
| Infusion-related back pain | 1 (3) | 2 (5) | 4 (9) | 0 |
| Intravenous injection site | ||||
| Extravasation | 1 (3) | 1 (3) | 3 (7) | 0 |
| Pain | 1 (3) | 1 (3) | 3 (7) | 0 |
| Photosensitivity reaction | 1 (3)c | 0 | 1 (2)d | 0 |
| Ocular AE | 15 (38) | 14 (36) | 13 (30) | 11 (27) |
| Choroidal hypoperfusion | 0 | 0 | 2 (5)e | 0 |
| Conjunctivitis | 0 | 2 (5) | 1 (2) | 1 (2) |
| Corneal lesion | 0 | 2 (5) | 0 | 0 |
| Eye pain | 5 (13) | 7 (18) | 7 (16) | 8 (20) |
| Increased IOPf | 1 (3) | 4 (10) | 3 (7) | 0 |
| Vision abnormal | 4 (10) | 1 (3) | 2 (5) | 0 |
| Vision decreased | 3 (8) | 3 (8) | 2 (5) | 0 |
| Visual field defect | 4 (10) | 0 | 2 (5) | 2 (5) |
| Withdrawal due to treatment-associated AE | 0 | 1 (3)g | 0 | 0 |
| Treatment-associated SAE | 2 (5) | 2 (5) | 1 (2) | 0 |
| Increased IOP | 0 | 1 (3) | 0 | 0 |
| Retinal detachment | 0 | 0 | 1 (2) | 0 |
| Retinal tear | 1 (3) | 0 | 0 | 0 |
| Vision decreased | 0 | 1 (3) | 1 (2) | 0 |
| Visual field defect | 0 | 0 | 1 (2) | 0 |
| Vitreous hemorrhage | 1 (3) | 0 | 1 (2) | 0 |
| Withdrawal due to SAE | 0 | 1 (3) | 0 | 0 |
| Deaths | 0 | 0 | 0 | 0 |
Notes:
Due to anxiety.
As assessed by the Investigator. Difference is statistically significant (P=0.045) between the quarter-fluence triple group (49%) and ranibizumab monotherapy group (27%).
Reported 2 days after the subject’s second treatment.
Reported on the day of initial treatment.
Moderate in intensity and associated with verteporfin photodynamic therapy; not associated with visual symptoms and not serious.
Defined as an increase of ≥10 mmHg from the previous visit or measurement of ≥25 mmHg. IOP elevations were considered mild except in one subject. Of the seven subjects with treatment-associated increased IOP, two received treatment (paracentesis and topical eye drops).
Due to the SAE of increased IOP.
Abbreviations: AE, adverse events; IOP, intraocular pressure; SAE, serious adverse events.
Treatment-associated ocular AE incidence was higher with CT (30%–38%) than with RM (27%), primarily from abnormal vision, decreased vision, visual field defect events (“vision disturbances”), and increased IOP. Most vision disturbances in the CT groups (82%) were transient (duration ≤1 month), with only one mild visual field defect (quarter-fluence triple therapy group) considered ongoing at study conclusion.
The overall incidence of increased IOP was similar across treatment groups (5%, 13%, 12%, and 12% in groups 1–4, respectively). Most (9 of 14 events) were postinjection IOP elevations that resolved the same day.
Five subjects had treatment-associated serious AE (SAE); all were in the CT groups (Table 2). One subject in the half-fluence double therapy group had four SAE and another subject in the half-fluence triple therapy group was withdrawn from the study due to the SAE of increased IOP. In addition, one patient each developed retinal tear, vitreous hemorrhage, and decreased vision. In the RM group, one patient withdrew from the study due to anxiety. A total of 10 deaths occurred in the study, none related to therapy.
Discussion
The RADICAL study demonstrated that significantly fewer retreatment visits are required with each CT arm versus RM. While the VA results appear similar the wide CIs preclude conclusions regarding whether the vision outcomes are superior, similar, or inferior with CT compared with RM. The decrease in retreatment visits observed in this large randomized trial supports data from previously published case series utilizing combination triple therapy9,15 and those randomized studies utilizing combination double therapy.13,14 The half-fluence triple therapy group had the fewest retreatment visits, but the difference was not statistically significant among the CT groups, so we cannot conclude that any specific CT resulted in fewer visits.
Although fewer retreatment visits were needed with CT, these groups also had more treatment procedures than the RM group. Only the quarter-fluence triple therapy result was significant when compared with RM. However, this result can mitigate the advantage of the fewer retreatment visits seen with CT. With triple therapy, three separate procedures were performed at each visit compared with one procedure in the RM group. The concern with multiple procedures is patient tolerance and potential complications. In the triple therapy group, there was one iatrogenic tear associated with the dexamethasone injection. This additional intravitreal injection is a risk factor for this SAE. Overall, however, the safety profile for intravitreal injections was excellent, confirming other reports.3,4 There were a number of patients with IOP elevations following treatment, but this was seen equally in all treatment groups and has been a well-documented complication from ranibizumab injections.1,2 The additional treatment with vPDT was similarly well-tolerated with the predominant additional complications nonserious and previously well-documented (infusion-related pain and intravenous injection events).18 In the clinical setting these results are especially important when considering CT because this treatment protocol may eliminate return visits for patients, but still result in equivalent or more procedures. Under certain circumstances this may be appropriate for a patient unable to routinely attend monthly visits.
The trial did not include a treatment group that received continuous monthly RM nor the regimen followed in PIER.19 Subjects in all treatment groups were assessed monthly, after the initial mandatory treatment(s), to determine if retreatment was needed. Such need-based therapy is consistent with standard clinical practice and has been demonstrated effective in multiple clinical trials.20–24 The authors recognize that the standard of care for RM is continuing to evolve and that continued monthly injections for the first year of treatment may be more effective than need-based therapy.22,24 This should be considered when interpreting the study results. Another limitation of the RADICAL study is that vPDT is approved for use only in predominantly classic subfoveal CNV due to AMD, with standard fluence, and every 3 months.18
CT in the RADICAL trial resulted in fewer retreatment visits compared with a RM regimen at 1 and 2 years. Vision outcomes appeared similar among treatment groups, but the wide CIs did not permit determining whether the outcomes with CT were superior, the same, or inferior to the monotherapy regimen given in this study. No acute severe vision loss was observed. Further studies would be needed to determine if vision outcomes are similar between CT and RM.
Acknowledgments
RADICAL trial group
Clinical centers
Matthew Ziemianski, MD, Carol Iverson: Associated Retina Consultants, Phoenix, AZ; Miguel Busquets, MD, Michelle Colwell: Associates in Ophthalmology, West Mifflin, PA; Geoff Williams, MD, Mark Hannah: Calgary Retina Consultants, Calgary, AB, Canada; John Dickinson, MD, Andrea Dean: Capital Health Ophthalmology, Halifax, NS; Richard Chace, MD, Sunny Kallay: Eyesight Ophthalmic Services, PA, Portsmouth, NH; Thomas Sheidow, MD, Teresa Jantzi: Ivvey Eye Institute – Lawson Health Research Institute, London, ON; Mark Emig, MD, Virginia Keenan: Midwest Eye Care, Omaha, NE; Thomas Ciulla, MD, Tonya Adkins: Midwest Eye Institute, Indianapolis, IN; Kent W Small, MD, Rosemary Silva-Garcia: Molecular Insight, Los Angeles, CA; Thomas, A Ghuman, Cheryl Kiesel: National Ophthalmic Research Institute, Fort Myers, FL; Leonardo Antaris, MD, Debby Curran: Quad Cities Retina Consultants, Davenport, IA; Henry L Hudson, MD, FACS, Patricia Wilkins: Retina Centers, PC, Tucson, AZ; Paul Tornambe, MD, Ruth Baer: Retina Consultants of San Diego, Poway, CA; Allen Ho, MD, Rose Soto: Retina Diagnostic & Treatment Assoc., LLC, Retina Research, Wills Eye Hospital, Philadelphia, PA; Ron P Gallemore, MD, PhD, Lillian Chen: Retina Macula Institute, Torrance, CA; Colin Ma, MD, Marcia Kopfer: Retina NorthWest, Portland, OR; Alan Franklin, MD, Willie Ross: Retina Specialists – Vision America of Mobile, Mobile, AL; David Boyer, MD, Janet Kurokouchi: Retina Vitreous Associates Medical Group, Beverly Hills, CA; Joel Pearlman, MD, Nyla Secor: Retinal Consultants Medical Group, Inc., Sacramento, CA; Amr Dessouki, MD, Tweetie Nguy: Retinal Diagnostic Center, Campbell, CA; Brian Sippy, MD, Rita Lennon: Rocky Mountain Eye Center, P.C., Missoula, MT; Robert Rosa, MD, Vanessa Hoelscher: Scott and White Memorial Hospital and Clinic, Temple, TX; David Callanan, MD, Patricia Bradley: Texas Retina Associates, Arlington, TX; Andrew Merkur MD, Dawne Gillies: University of British Columbia/Vancouver Hospital – Eye Care Centre, Vancouver, BC; Michael Brent, MD, Nicole McLaren: University Health Network – Toronto Western Hospital, Toronto, ON; Craig Wells, MD, Melita Williams: Vitreoretinal Associates, Seattle, WA. Clinic Monitors: Melissa Broemeling, Sue-Anne Crocker, Mary Beth McClain, Michelle Shivers, Wendy Wilson. QLT Inc., Vancouver, BC, Canada: Sue-Anne Crocker, AHT, CCRP, Oscar Cuzzani, MD, Yong Hao, MD, PhD, Laurie Haynes, Edward Ronyecz, H Andrew Strong, PhD, Xiang Yao Su, PhD. Committees: Data and Safety Monitoring Committee: Neil M Bressler, MD, and Michael Ip, MD. RADICAL Trial Advisory Group: Allen C Ho, MD, Henry L Hudson, MD, FACS. Xiang Yao Su, PhD, QLT Inc, provided statistical analyses. Laurie Haynes, ELS, QLT Inc, prepared the initial draft and edited drafts. Sherry Stinn, QLT Inc, created graphs and figures.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Brown DM, Kaiser PK, Michels M, et al. for the ANCHOR Study Group Ranibizumab versus verteporfin for neovascular age-related macular degeneration. N Engl J Med. 2006;355(14):1432–1444. doi: 10.1056/NEJMoa062655. [DOI] [PubMed] [Google Scholar]
- 2.Rosenfeld PJ, Brown DM, Heier JS, et al. for the MARINA Study Group Ranibizumab for neovascular age-related macular degeneration. N Engl J Med. 2006;355(14):1419–1431. doi: 10.1056/NEJMoa054481. [DOI] [PubMed] [Google Scholar]
- 3.Schmidt-Erfurth U. Clinical safety of ranibizumab in age-related macular degeneration. Expert Opin Drug Saf. 2010;9(1):149–165. doi: 10.1517/14740330903418422. [DOI] [PubMed] [Google Scholar]
- 4.Klein KS, Walsh MK, Hassan TS, et al. Endophthalmitis after anti-VEGF injections. Ophthalmology. 2009;116(6):1225. doi: 10.1016/j.ophtha.2009.02.031. [DOI] [PubMed] [Google Scholar]
- 5.Dhalla MS, Shah GK, Blinder KJ, Ryan EH, Jr, Mittra RA, Tewari A. Combined photodynamic therapy with verteporfin and intravitreal bevacizumab for choroidal neovascularization in age-related macular degeneration. Retina. 2006;26(9):988–993. doi: 10.1097/01.iae.0000247164.70376.91. [DOI] [PubMed] [Google Scholar]
- 6.Lazic R, Gabric N. Verteporfin therapy and intravitreal bevacizumab combined and alone in choroidal neovascularization due to age-related macular degeneration. Ophthalmology. 2007;114(6):1179–1185. doi: 10.1016/j.ophtha.2007.03.006. [DOI] [PubMed] [Google Scholar]
- 7.Potter MJ, Claudio CC, Szabo SM. A randomised trial of bevacizumab and reduced light dose photodynamic therapy in age-related macular degeneration: the VIA study. Br J Ophthalmol. 2010;94(2):174–179. doi: 10.1136/bjo.2008.155531. [DOI] [PubMed] [Google Scholar]
- 8.Kaiser PK, Boyer DS, Garcia R, et al. Registry of Visudyne AMD Therapy Writing Committee. Verteporfin photodynamic therapy combined with intravitreal bevacizumab for neovascular age-related macular degeneration. Ophthalmology. 2009;116(4):747–755. doi: 10.1016/j.ophtha.2008.12.057. [DOI] [PubMed] [Google Scholar]
- 9.Augustin AJ, Puls S, Offermann I. Triple therapy for choroidal neovascularization due to age-related macular degeneration: verteporfin PDT, bevacizumab, and dexamethasone. Retina. 2007;27(2):133–140. doi: 10.1097/IAE.0b013e3180323de7. [DOI] [PubMed] [Google Scholar]
- 10.Antoszyk AN, Tuomi L, Chung CY, Singh A, FOCUS Study Group Ranibizumab combined with verteporfin photodynamic therapy in neovascular age-related macular degeneration (FOCUS): year 2 results. Am J Ophthalmol. 2008;145(5):862–874. doi: 10.1016/j.ajo.2007.12.029. [DOI] [PubMed] [Google Scholar]
- 11.Schmidt-Erfurth U, Wolf S, PROTECT Study Group Same-day administration of verteporfin and ranibizumab 0.5 mg in patients with choroidal neovascularisation due to age-related macular degeneration. Br J Ophthalmol. 2008;92(12):1620–1627. doi: 10.1136/bjo.2007.135277. [DOI] [PubMed] [Google Scholar]
- 12.Smith BT, Dhalla MS, Shah GK, Blinder KJ, Ryan EH, Jr, Mittra RA. Intravitreal injection of bevacizumab combined with verteporfin photodynamic therapy for choroidal neovascularization in age-related macular degeneration. Retina. 2008;28(5):675–681. doi: 10.1097/IAE.0b013e31816b316e. [DOI] [PubMed] [Google Scholar]
- 13.Williams PD, Callanan D, Solley W, Avery RL, Pieramici DJ, Aaberg T. A prospective pilot study comparing combined intravitreal ranibizumab and half-fluence photodynamic therapy with ranibizumab monotherapy in the treatment of neovascular age-related macular degeneration. Clin Ophthalmol. 2012;6:1519–1525. doi: 10.2147/OPTH.S31010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hatz K, Schneider U, Henrich PB, Braun B, Sacu S, Prünte C. Ranibizumab plus verteporfin photodynamic therapy in neovascular age-related macular degeneration: 12 months of retreatment and vision outcomes from a randomized study. Ophthalmologica. 2015;233(2):66–73. doi: 10.1159/000367603. [DOI] [PubMed] [Google Scholar]
- 15.Yip PP, Woo CF, Tang HH, Ho CK. Triple therapy for neovascular age-related macular degeneration using single-session photodynamic therapy combined with intravitreal bevacizumab and triamcinolone. Br J Ophthalmol. 2009;93(6):754–758. doi: 10.1136/bjo.2008.150987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gallemore RP, Nguyen D. When anti-VEGF treatment fails. Rev Opthalmol. 2008;15:03. [Google Scholar]
- 17.Shah GK, Sang DN, Hughes MS. Verteporfin combination regimens in the treatment of neovascular age-related macular degeneration. Retina. 2009;29(2):133–148. doi: 10.1097/IAE.0b013e3181960a28. [DOI] [PubMed] [Google Scholar]
- 18.VISUDYNE® Verteporfin for Injection) Full Prescribing Information. Bridgewater, NJ, USA: Valeant Ophthalmics; 2013. [Accessed June 2, 2016]. Available from: http://www.bausch.com/Portals/77/-/m/BL/United%20States/Files/Package%20Inserts/Pharma/visudyne-package-insert.pdf. [Google Scholar]
- 19.Regillo CD, Brown DM, Abraham P, et al. for the PIER Study Group Randomized, double-masked, sham-controlled trial of ranibizumab for neovascular age-related macular degeneration: PIER study year 1. Am J Ophthalmol. 2008;145(2):239–248. doi: 10.1016/j.ajo.2007.10.004. [DOI] [PubMed] [Google Scholar]
- 20.Fung AE, Lalwani GA, Rosenfeld PJ, et al. An optical coherence tomography-guided, variable dosing regimen with intravitreal ranibizumab (Lucentis) for neovascular age-related degeneration (AMD) Am J Ophthalmol. 2007;143(4):566–583. doi: 10.1016/j.ajo.2007.01.028. [DOI] [PubMed] [Google Scholar]
- 21.Lalwani GA, Rosenfeld PJ, Fung AE, et al. A variable-dosing regimen with intravitreal ranibizumab for neovascular age-related macular degeneration: year 2 of the PrONTO study. Am J Ophthalmol. 2009;148(1):43.e1–58.e1. doi: 10.1016/j.ajo.2009.01.024. [DOI] [PubMed] [Google Scholar]
- 22.Busbee BG, Ho AC, Brown DM, et al. HARBOR Study Group Twelve-month efficacy and safety of 0.5 mg or 2.0 mg ranibizumab in patients with subfoveal neovascular age-related macular degeneration. Ophthalmology. 2013;120(5):1046–1056. doi: 10.1016/j.ophtha.2012.10.014. [DOI] [PubMed] [Google Scholar]
- 23.Martin DF, Maguire MG, Ying GS, Grunwald JE, Fine SL, Jaffe GJ, CATT Research Group Ranibizumab and bevacizumab for neovascular age-related macular degeneration. N Engl J Med. 2011;364(20):1897–1908. doi: 10.1056/NEJMoa1102673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Martin DF, Maguire MG, Fine SL, et al. Comparison of Age-related Macular Degeneration Treatments Trials (CATT) Research Group Ranibizumab and bevacizumab for treatment of neovascular age-related macular degeneration: two year results. Ophthalmology. 2012;119(7):1388–1398. doi: 10.1016/j.ophtha.2012.03.053. [DOI] [PMC free article] [PubMed] [Google Scholar]