Abstract
Objective
Investigators conducting Alzheimer’s disease (AD) research need to consider participants’ capacity to consent. Cognitive functioning is a significant predictor of decisional capacity, but there is a dearth of information on the influence of neuropsychiatric symptoms in AD on decisional capacity. We examined the rates of decisional capacity associated with two types of research protocols, and the association of capacity with neuropsychiatric symptoms and other participant characteristics.
Methods
We comprehensively evaluated decisional capacity among 64 patients with mild-to-moderate AD and 70 healthy comparison (HC) subjects randomized to consider either a medium risk or higher risk hypothetical research protocol. Additional measures included sociodemographics, cognitive deficits, and neuropsychiatric symptoms.
Results
Twenty AD patients (31.3%) and 67 HCs (95.7%) were deemed capable; 44 AD patients (68.8%) and 3 HCs (4.3%) incapable of consent. Age, education, and severity of cognitive deficits were associated with incapable status; there were no significant associations with severity of neuropsychiatric symptoms or protocol risk level.
Conclusions
Findings highlight the importance of understanding of capacity and its assessment among people with AD, rather than treating AD diagnosis as synonymous with impaired capacity. As novel treatments move from bench to bedside, methods of assessing and addressing capacity impairment must similarly advance.
Clinical Implications
In assessing research consent capacity, use structured assessments with population specific cut scores interpreted in the context of the person’s background including education, culture, and language. Individuals should be encouraged to execute research proxy documents when able.
Introduction
Alzheimer’s disease (AD) affected 5.3 million people in the United States in 2015, and is associated with more than $200 billion in annual health care costs (Alzheimer's Association, 2015; Hoyert & Xu, 2012). With no foreseeable cure, present hopes are tied to novel approaches to better manage AD and/or slow disease progression. Treatment advances will require increased clinical research, in turn increasing the need to enroll participants with AD. However, as is the case when testing any novel intervention, unanticipated risks are likely and benefits uncertain.
A key problem in AD clinical research is determining whether participants have capacity to consent. AD is a risk factor for impaired decisional capacity, but some patients retain consent capacity in some research contexts. Kim et al. (2001), Karlawish et al. (2008), and Warner et al. (2008) found, respectively, that 55.6%, 52.5%, and 23.9% of patients with mild-to moderate AD were capable to consent to a placebo-controlled clinical trial. Although the variation between the two former studies and the latter may be due to methodological differences in the studies of consent, another possibility is variation in the clinical trials that participants were being asked to consider. Risks of false-positive versus false-negative determinations vary based on the nature of specific clinical trials, as well as the inherent complexity of a particular trial. Using the majority opinion of expert raters, Kim et al. (2011) found that 61.7% of participants with AD were capable of appointing a proxy for research decision making, whereas 41.4% were capable of consenting to a randomized drug trial, and only 15.6% were capable of consenting to neurosurgical trial. Further work is needed to develop a deeper understanding of the participant characteristics, as well as protocol-level variables that may be associated with impaired capacity among people with AD.
Severity of cognitive deficits is a significant predictor of impaired decisional capacity (Palmer & Savla, 2007; Palmer, Savla, & Harmell, 2012). However, in addition to the cognitive deficits that typify AD, this disorder is frequently associated with neuropsychiatric symptoms such as mood disturbances, delusions, hallucinations, and agitation (Burke, Hall, & Tariot, 2013; Cantillon, De La Puente, & Palmer, 1998; Cummings & Zhong, 2015). Such neuropsychiatric symptoms exert a profound adverse impact, including increased caregiver burden and early institutionalization of patients. To our knowledge, however, no prior published studies have examined the influence of neuropsychiatric symptoms in AD on decisional capacity.
The goals of the present study were to: 1) obtain further empirical evidence regarding rates of impaired capacity to consent to clinical trials among people with mild-to-moderate AD relative to healthy comparison (HC) subjects; and 2) identify factors associated with capable versus incapable research consent status. Potential predictive factors included diagnosis, sociodemographics, neuropsychiatric symptoms, cognitive functioning, and clinical trial type. Each participant was randomized to consider one of two hypothetical but realistic protocols: a phase III clinical trial of an investigational cholinomimetic medication (hereafter referred to as “medium risk” protocol) vs. a phase II trial of a novel immunotherapeutic agent targeting beta-amyloid deposits (“higher risk” protocol).
We hypothesized that: 1) AD would be a significant risk factor for impaired decisional capacity; and 2) age, education, severity of neuropsychiatric symptoms, severity of cognitive deficits, and clinical trial type would differ between capable versus incapable participants. We also examined the degree to which a 5-item questionnaire was associated with capacity determinations made through a more comprehensive process. This comparison was included to determine whether a brief set of questions that can be incorporated into virtually any consent process with minimal participant or protocol burden could help identify those participants warranting a more extensive/comprehensive capacity evaluation.
Methods
Participants
Participants included 64 people with possible or probable AD of mild-to-moderate severity, and 70 age-comparable healthy comparison (HC) subjects. The data were collected as part of a larger study on the effectiveness of multimedia consent procedures, but the focus of the present report is on predicting decisional capacity under routine consent conditions (none of the participants in the current report received consent via an enhanced or multimedia presentation). Participants with AD were recruited through the University of California, San Diego (UC San Diego) Shiley-Marcos Alzheimer’s Disease Research Center (ADRC), AD caregiver support groups, UC San Diego Advanced Center for Innovation in Services and Intervention Research (ACISIR), memory care centers, physician referrals, community events, and word of mouth. Recruitment of HC subjects included the Stein Institute for Research on Aging, ACISIR, and ADRC, word of mouth, local retirement homes and senior centers, postings on craigslist.com, and flyers posted in the community. Inclusion criteria included: (a) possible or probable AD (patients only), (b) MMSE total score ≥ 15, (c) age ≥ 50 years, (d) fluency in English, and (e) written informed consent from the participant, or written assent from the participant with consent from a legally authorized representative. Exclusion criteria included: (a) other neurologic conditions potentially affecting cognition and (b) physical/medical conditions precluding the participant from completing the study procedures or assessments. Potential HC subjects were also excluded if they had a known history of any significant mental health condition that could impair neurocognitive functioning.
Diagnosis of AD was generally pre-established by the recruitment site and is the type of diagnostic information that recruiters for AD research generally access when first approaching and consenting people for possible participation. For HCs, the absence of current or past neuropsychiatric disorders was established with the Mini International Neuropsychiatric Interview (Sheehan, Lecrubier, & Sheehan, 1998). This study was reviewed and approved by the UC San Diego Human Research Protections Program.
Measures and procedures
To minimize participant burden, the study procedures and assessments were provided over two study visits (usually over two consecutive days). All measures administered during those two days, with the exception of the simulated consent and 5-item questionnaire, were administered by the same research associate (RA-1). A second research associated (RA-2) was responsible for completing the simulated consent process and the 5-item questionnaire. Training of study personnel was overseen by the first author (BWP) in conjunction with a trained and experienced study coordinator.
Day 1
In addition to completing screening and consent for this study itself, the following assessments were conducted on the first day with each participant:
Demographic information
Age, education, gender, and ethnic background (dichotomized as non-Latino Caucasian or other ethnic background) were collected through interview and/or review of available records.
Cognitive measures
Cognitive impairment was evaluated by RA-1 with the Mini Mental State Examination (MMSE; Folstein, Folstein, & McHugh, 1975), the Montreal Cognitive Assessment (MoCA; Nasreddine et al., 2005) and the Mattis Dementia Rating Scale – Second Edition (DRS-II; Jurica, Leitten, & Mattis, 1991). Although the DRS-II yields several subscale scores, prior research provides little evidence of differential associations of specific cognitive domains with decisional capacity independent of the effects of differential psychometric properties of the measures of those domains (Palmer & Savla, 2007). Therefore, for the present analyses our focus was on the DRS-II total scores.
Day 2
Neuropsychiatric symptoms
Caregivers of participants in the AD group completed the Caregiver-Administered Neuropsychiatric Inventory (CGA-NPI; Kang et al., 2004). Although the CGA-NPI is designed to permit caregivers to self-complete the questionnaire, many caregivers expressed a preference, and were given the option, to complete the questionnaire with the assistance of RA-1. The CGA-NPI assesses prevalence, severity, and frequency of twelve neuropsychiatric symptom domains, yielding a score for each domain (ranging from 0 to 12) and a total score ranging from 0 to 144 (higher scores indicate more severe symptoms). [The CGA-NPI was not administered to HC participants. CGA-NPI scores were unavailable for nine of the AD participants, and a total score could not be calculated for 18 AD participants due to ≥ one missing domain.]
Hypothetical protocols
Participants were randomly assigned to one of two hypothetical protocols: (a) a phase III clinical trial of an investigational cholinomimetic drug (medium risk protocol), or (b) a phase II trial of an AD (anti-amyloid) immunotherapy (higher risk protocol). For each hypothetical protocol, subjects were presented with a printed consent form designed to have the same structure and content as an IRB-approved study. Details of the hypothetical protocols are summarized in Table 1.
Table 1.
Summary of hypothetical protocols (to be made supplemental).
| Phase III Trial (Lower Risk) | Phase II Trial (Higher Risk) |
|---|---|
|
|
Simulated consent procedures
RA-2 explained that she was going to read and discuss the consent form with the participant, and encouraged the participant to read along. Participants were encouraged to stop the RA at any point for clarification or questions. The RA paused after each major conceptual unit, such as after the first paragraph in which the study purpose was described, and asked the participant if he or she had any questions about that information. The RA answered any questions, and proceeded to review the remainder of the consent form in the same manner.
Comprehension and decision making capacity
Immediately after presenting hypothetical consent information, RA-2 proceeded to administer the 5-item questionnaire to evaluate the participant’s short-term memory related to understanding of the purpose, procedures, risks, benefits, and voluntary nature of the described protocol. Following the scoring procedures for other consent scales (Appelbaum & Grisso, 2001), each response was scored as 0 (incorrect), 1 (partially correct), or 2 (fully correct). The purpose of the 5-item questionnaire was to determine the amount of information subjects retained in short-term memory at the point they would most typically be asked to sign the consent form if recruited to an actual protocol, and whether this quickly assessable information would be strongly associated with decisional capacity status determined through a more comprehensive evaluation process.
After completing the above procedures and measures, each subject met with RA-1 to conduct a comprehensive capacity assessment using a modified MacArthur Competence Assessment Tool for Clinical Research (MacCAT-CR; Appelbaum & Grisso, 2001). The MacCAT-CR is a 15-20 minute semi-structured interview providing subscale scores for four dimensions of decision-making capacity: Understanding (range=0-26), Appreciation (range=0-6), Reasoning (range=0-8), and Expression of a Choice (range=0-2). Higher scores indicate better performance. In standard MacCAT-CR procedures, information relevant to answering the items is embedded as part of the semi-structured interview; the questions are interlaced with presentation of information. For example, the purpose and general procedures of the protocol are described, and then participants are asked to describe their understanding of the information just presented, followed by specific probes, i.e. questions about information that was not provided in the participant’s initial response. If necessary, corrective feedback is provided at that point. However, because one goal of the larger study was to determine the effects of the consent procedure on comprehension, we omitted the initial embedded disclosures from the MacCAT-CR interview. Such MacCAT-CR modification has been successfully employed in prior consent studies (Mittal et al., 2007; Rubright et al., 2010). The subjects’ understanding score under these conditions is referred to as Trial 1. However, in accord with standard MacCAT-CR administration procedures, any misunderstood information was subsequently re-explained and the subject’s understanding re-assessed. The scores obtained after such re-explanation are hereafter referred to as Trial 2. Trial 2 scores were employed in the final capacity determinations, described below.
The MacCAT-CR, as originally developed and published, did not establish pre-determined cut-off scores indicating lack of capacity. Thus, we used procedures developed and validated by one of our co-authors (SYHK) to determine appropriate cut-scores (Kim, et al., 2001, 2007). Specifically, MacCAT-CR interviews for the larger study of enhanced consent were video recorded (the larger study included 114 people with AD, 64 of whom, included in the present report, received routine/non-multimedia consent procedures). A subset of the recorded AD patient interviews (n=40) were then independently reviewed by three geriatric psychiatrists experienced in making capacity determinations and trained by SYHK in the task for this study.
Of the 40 videos selected for review, all were participants with AD; 19 had received the high risk hypothetical protocol and 21 the medium risk protocol. When we initially designed the study we had planned to have equal numbers within three MMSE groups (MMSE totals: 15-19, 20-24, and ≥ 25). However, we soon revised this plan as we realized that the most complicated decisions would be in the middle group. That is, it was more likely that there would be disagreement regarding decisional capacity in the middle range group. Thus, the final sample included 11 videotapes where the interviewee had MMSE scores of 15-19, 11 where the interviewee had obtained a score ≥ 25, and 18 with MMSE total scores between 20-24 points. (These were randomly selected from among the video tapes within those MMSE ranges.) After viewing the video, each psychiatrist responded to the following question “Based on the interview on the tape you just saw, do you believe that this person has sufficient capacity to give his or her own informed consent to the research study?” The psychiatrists’ responded on a four point scale: 1 = definitely has sufficient capacity, 2 = probably has sufficient capacity, 3= probably does not have sufficient capacity, 4 = definitely does not have sufficient capacity. For present analyses, scores of 1 or 2 were deemed “capable” and those of 3 or 4 were deemed “incapable.” The capacity status endorsed by at least 2 of the 3 psychiatrists was used as the determination of capacity status for each subject. These dichotomized capacity ratings were used as the “gold standard” for determining the most appropriate MacCAT-CR cut-points using Receiver Operating Characteristic (ROC) curve analyses.
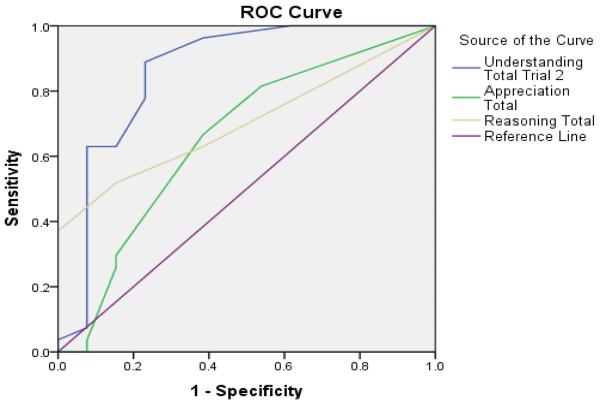
Statistical analyses
The ROC curve analyses were conducted in SPSS 21.0 using the dichotomized capacity ratings for the 40 subjects whose videotapes were rated by the three geriatric psychiatrists. We examined the area under the curve (AUC) with 95% confidence intervals for the MacCAT-CR Understanding (Trial 2), Appreciation, and Reasoning subscales. We then selected the subscale and cut-score with the optimal balance of sensitivity and specificity, and applied that cut-score to the entire sample to categorize each participant as capable or incapable of consent.
Capable and incapable AD patients were compared in terms of sociodemographics (age, education, gender, ethnicity), severity of neuropsychiatric symptoms (CGA-NPI total and domain scores), cognitive deficits (MMSE, MoCA, and DRS total scores), MacCAT-CR subscale scores, and protocol type (medium versus higher risk), using independent t-test for continuous variables and Pearson’s Chi-square for categorical variables. Similar analyses were conducted to compare the sociodemographic characteristics and cognitive functioning of the 70 HC versus 64 AD participants. Significance for all analyses was defined as p < 0.05 (two-tailed).
Results
Sociodemographic and cognitive comparison of HC and AD participants
There were no significant differences in age, education, or race/ethnicity (data not shown). Relative to the HC group, the AD group had fewer women (58.6% versus 39.1%), χ2[1] = 5.09, p = 0.204, and had worse performance on all three cognitive measures [mean (SD) MMSE = 27.7 (2.0) versus 21.7 (3.4), MoCA = 23.1 (3.6) versus 15.0 (4.8), DRS total = 134 (7.9) versus 114.2 (13.3) respectively], t(101.6) = 12.41, t(90.39) = 9.64, and t(90.34)=10.34, respectively, all p-values <.001.
Predicting and Categorizing Capacity Status
Of the 40 AD patients whose capacity status was rated through video review, 13 were deemed capable and 27 incapable. Interrater reliability for capacity determination was good (ICC = 0.779). The Understanding subscale (using Trial 2, as it corresponds to the standard MacCAT-CR scoring) was found to be the best at discriminating capacity status, AUC = .860, p <.001; 95% CI= .712 to 1.00. The values for the Appreciation subscale were AUC = .655, p= .116; 95% CI = .463 to .848, and for Reasoning AUC = .702, p = .040; 95% CI = .544 to .861. A cut- score of 20.5 on the Understanding subscale provided a good balance of sensitivity (0.889) and specificity (0.769), with an overall correct classification rate of 85.0%.
Applying the Understanding Trial 2 cut-score of 20.5 to the entire sample, 20 AD patients (31.3%) were deemed capable and 44 patients (68.8%) were deemed incapable of consenting to research. Among HCs, 67 participants (95.7%) were deemed capable and 3 participants (4.3%) were deemed incapable of consent. As almost all the HCs were classified as capable of consent, our analysis of differences among capable versus incapable subjects was limited to the AD group.
Comparison of decisionally capable versus incapable participants with AD
Among the AD patients, people in the incapable group were older, had fewer years of education, had worse cognitive deficits (MMSE, MoCA, and DRS total scores), and performed worse on the 5-item questionnaire, compared to the capable group (Table 2). Those people with AD who were incapable of consent also had lower Appreciation and Reasoning scores. There were no significant differences between the capable and incapable groups in terms of gender, ethnicity, severity of overall or subdomain neuropsychiatric symptoms, ability to express a choice, or protocol type. Although all participants were fluent in English, 6 of the 64 AD participants reported that English was their second language; five of these six participants (83.3%) were decisionally incapable as defined by the Understanding cut-score.
Table 2.
Comparison of decisionally capable and incapable subjects with Alzheimer’s disease.
| Capable AD (n=20) |
Incapable AD (n=44) |
Statistical test with df |
p | |
|---|---|---|---|---|
| Age (years) | 76.9 (6.2) | 80.6 (6.9) | t(62.0) = 2.09 | .041 |
| Education (years) | 15.6 (2.7) | 13.1 (3.1) | t(61.0) = 3.01 | .004 |
| Gender (% female) | 46.5% | 43.2% | χ2(1) = 0.09 | .767 |
| Ethnicity (% Caucasian) | 90.7% | 79.5% | χ2(1) = 1.06 | .304 |
| NPI-CGA total | 10.86 (12.39) | 16.28 (15.34) | t(44) = 1.16 | .250 |
| Delusions | 0.31 (1.01) | 0.74 (1.90) | t(44.0) = 1.16 | .250 |
| Hallucinations | 0.31 (1.01) | 0.13 (0.41) | t(53.0) = 0.97 | .337 |
| Agitation/Aggression | 1.44 (3.10) | 1.44 (2.36) | t(22.5) = 0.01 | .999 |
| Depression/Dysphoria | 1.13 (1.09) | 1.05 (2.37) | t(53) = 0.12 | .906 |
| Anxiety | 1.06 (2.14) | 0.90 (2.40) | t(53) = 0.24 | .813 |
| Elation/Euphoria | 0.50 (1.55) | 0.28 (1.02) | t(53) = 0.61 | .542 |
| Apathy/Indifference | 2.63 (3.72) | 3.65 (4.04) | t(48) = 0.85 | .397 |
| Disinhibition | 0.69 (1.66) | 0.95 (2.11) | t(53) = 0.44 | .661 |
| Irritability/Lability | 1.56 (2.48) | 1.26 (2.69) | t(53) = 0.39 | .697 |
| Motor | 1.60 (3.58) | 0.95 (1.93) | t(52) = 0.86 | .393 |
| Sleep/Nighttime | 1.07 (2.22) | 1.30 (3.26) | t(50) = 0.25 | .803 |
| Appetite/Eating | 1.63 (3.52) | 2.51 (3.99) | t(53) = 0.77 | .442 |
| MMSE total | 23.3 (3.4) | 21.0 (3.1) | t(62.0) = 2.64 | .010 |
| MoCA total | 17.5 (4.6) | 13.9 (4.6) | t(48.0) = 2.47 | .017 |
| DRS total | 120.8 (8.2) | 111.4 (14.1) | t(55.4) = 3.30 | .002 |
| 5-item total | 7.6 (2.1) | 4.7 (2.3) | t(62) = 4.85 | <.001 |
| MacCAT-CR | ||||
| Understanding | 23.4 (1.6) | 11.7 (5.6) | a | a |
| Appreciation | 5.1 (0.9) | 3.7 (1.4) | t(61) = 4.04 | <.001 |
| Reasoning | 7.1 (1.9) | 5.4 (2.5) | t(45.4) = 2.94 | .005 |
| Expression of Choice | 1.7 (0.7) | 1.6 (0.7) | t(61) = 0.75 | .454 |
| Protocol type (% higher risk) |
50.0% | 47.7% | χ2(1) = 0.03 | .866 |
t-test not calculated since grouping was based on MacCAT-CR Understanding cut-score, null hypothesis false by definition.
Note: Values represent group means (and SDs) or proportions; AD = Alzheimer’s disease; CGA-NPI = Caregiver Administered Neuropsychiatric Inventory; MMSE = Mini Mental State Examination; MoCA= Montreal Cognitive Assessment; DRS = Mattis Dementia Rating Scale; MacCAT-CR = MacArthur Competence Assessment Tool – Clinical Research.
Discussion
This study evaluated capacity to consent to research among people with mild to moderate AD and HC subjects. Consistent with our hypotheses, AD diagnosis was a significant predictor of impaired capacity. However, 31% of people with AD retained capacity to consent. Also consistent with our hypotheses, we found older age, lower education, and more severe cognitive deficits among decisionally incapable relative to capable AD patients. AD patients classified as decisionally capable through a comprehensive assessment had significantly better scores than incapable subjects on a 5-item questionnaire. Contrary to our hypotheses, we found no association between capacity status and severity of neuropsychiatric symptoms or protocol type.
While the absence of an association of neuropsychiatric symptoms with decisional capacity was contrary to our hypotheses, it parallels findings in schizophrenia where psychotic symptoms appear to be less predictive of capacity to consent to research or treatment than cognitive deficits (Palmer & Savla, 2007; Palmer et al., 2012). Note that mean levels of neuropsychiatric symptoms in our AD sample were low relative to the potential range of the CGA-NPI. It is plausible that more severe neuropsychiatric symptoms might interfere with the consent process. Thus, further research on the impact of neuropsychiatric symptoms is warranted in research contexts involving AD patients with more severe neuropsychiatric disturbances.
Protocol risk level did not have a strong influence on decisional capacity, possibly due to the relative complexity of both protocols. However, given that many AD trials involve procedures and complexity similar to those described in our hypothetical protocols, investigators may need to consider capacity “at risk” for most AD clinical trials. The question of whether protocol complexity affects decisional capacity was not directly addressed by the present study, but it seems very likely that a procedurally simple protocol would require less cognitive skills than consenting to a complex protocol (Kim et al., 2011).
As decisional capacity is a “context-specific” construct, our results may not generalize to other study populations or research protocols. The protocols we employed involved hypothetical scenarios. This method permitted us to maximize enrollment across a broad spectrum of people with AD and to randomly assign participants to protocol type. It is possible that the context of a real protocol would somehow affect level of attention and therefore ultimate capacity levels, but this seems unlikely to be a major source of variance in the key outcomes of the study. Another potential limitation is that the MacCAT-CR was modified from its standard procedures, in that the initial disclosures were not embedded in the MacCAT-CR interview. This may have reduced participants’ ability to immediately describe the essential information. On the other hand, information that was missed by participants was eventually re-disclosed, and their responses after re-disclosure was among the material available to the psychiatrists rating participants for decisional capacity.
Despite the dominant focus on surrogate decision making for AD research, the present and prior empirical studies document that some people with AD retain capacity for some research decisions (Karlawish et al., 2008; Kim, et al., 2001; Palmer et al., 2005). For those individuals, making those specific decisions, surrogate consent might be unwarranted. Investigators need to consider the likelihood of impaired decision making capacity so that they can identify individuals warranting comprehensive capacity assessment. In this regard, it is notable that a simple set of 5-questions administered immediately after review of the consent document significantly differed among decisionally capable versus incapable AD patients. We previously reported on a 10-item questionnaire, the UCSD Brief Assessment of Consent Capacity (UBACC) that showed a strong association with the MacCAT-CR (Jeste et al., 2007). Although the UBACC was designed in reference to schizophrenia research, this or similar brief questionnaires may have a role in routine consent for AD research and other “at risk” populations, adding minimal time and burden to the consent process. We have also previously shown the value of incorporating a short set of questions within the process of consent as an aid to identify problems and enhance understanding in a range of psychiatric and medical research populations (Palmer, Cassidy, Dunn, Spira, & Sheikh, 2008). The value of an iterative process with corrective feedback was also shown in work by Taub and colleagues (e.g., Taub & Baker, 1983), and appears to remain a viable recommendation as a standard consent procedure across biomedical research.
In order to uphold the ethical principle of “respect for persons,” there remains a need for greater understanding of the predictors of impaired capacity in this population, as well as rigorous data regarding what tools are most appropriate to use for capacity assessment in the context of AD clinical research (Dunn, Nowrangi, Palmer, Jeste, & Saks, 2006; American Bar Association / American Psychological Association, 2005; Simpson, 2010). For example, it is noted that education levels were significantly lower among incapable versus capable persons with AD. Education may itself be confounded with a range of other factors such as reading skill, health literacy, research literacy, and preferred learning style. Part of the needed research is to determine how combinations of factors, such as performance on screening questionnaires (such as the 5-item questionnaire employed in the present study), sociodemographics (such as age, education, and health or research literacy), as well clinical factors (such as severity of cognitive impairment or more severe neuropsychiatric symptoms) may be useful in developing methods with good sensitivity and specificity that can be routinely employed to rapidly identify those potential participants at risk for impaired capacity. Also, although all participants were fluent in English, five of six participants for whom English was a second language were categorized as decisionally incapable. Research consent procedures for multilingual participants have received little empirical attention.
Investigators also need empirical guidance on ways to enhance the consent capacity of those with AD who show impaired capacity, or in certain subgroups such as those with lower education or more severe cognitive impairment. For example, Rubright et al. (2010) reported that AD patients receiving a memory and organizational aid during the research consent process had a higher likelihood of being judged capable of consent and higher MacCAT-CR Understanding subscale scores than those who received routine consent procedures. In a systematic review of the efficacy of multimedia aids for the research consent process (Palmer, Lanouette, & Jeste, 2012), only 1 of 20 studies identified was focused on AD patients (Mittal, et al., 2007). However, the latter study yielded equivocal results due to a small sample size (n=32) and lack of a non-enhanced control consent procedure. (The effectiveness of multimedia aided consent is a question we will be further evaluating in a future report with the larger study from which the present sample was drawn.)
Clinical Implications
What would an appropriate capacity assessment consist of? Based on our findings and those of others (Karlawish et al., 2002; Kim, et al., 2001; Rubright, et al., 2010), we would argue that, at minimum, a structured assessment of the ability to describe, in the participant’s own words, the purpose, procedures, and potential risks of the research, should be conducted for each trial. The MacCAT-CR, which is the most widely used research instrument of this type, can be administered in approximately 15-20 minutes, but as noted above, our group also developed and validated a briefer measure, the UBACC that can be administered in less than 5-minutes (Jeste, et al., 2007). The choice among these and other available instruments in terms of trade-off between time of administration and comprehensiveness may be dictated by the complexity of the study procedures and risk:benefit ratio (see Dunn, et al., 2006).
The ROC analyses indicated a MacCAT-CR cut-score of 20.5 on the Understanding subscale as providing a good balance of sensitivity and specificity. This was useful in the context of the present study as it provided a basis for categorizing capacity status of each participant in the full sample, without the burden of having experts review and rate every interview. But we would not necessarily recommend this or any specific cut-score for every applied setting. In a large scale study of schizophrenia in which the MacCAT-CR was used to determine eligibility, the investigators employed an Understanding cut-score ≥ 16 as defining capacity to consent (Stroup et al., 2005), which may have been appropriate given the low rates of incapacity (determined by expert ratings similar to those employed in the present study) in that population (Kim, et al., 2007). Due to the contextual nature of the construct of decision making capacity, the authors of the MacCAT-CR intentionally did not provide specific cut-offs (Appelbaum & Grisso, 2001). However, consideration of the sensitivity and specificity associated with specific cut-scores, such as those depicted in Figure 1 of the present report for AD, and those reported by Kim et al. (2007) for schizophrenia, together with a consideration of the base-rates of incapacity which affect the positive and negative predictive value of test results, and the potential harm of false-positive and false-negative errors in a given context, may be helpful to investigators in selecting at least preliminary cut-scores for identifying those participants warranting more careful scrutiny in regard to decisional capacity.
Figure 1.
Receiver Operating Characteristic (ROC) curve analyses examining the utility of the MacCAT-CR subscales (Understanding, Appreciation, and Reasoning) in detecting “incapable” status
Given the heterogeneity in consent capacity of patients with AD, one might ask whether it makes sense for investigators to routinely seek surrogate consent for dementia research. To respect patient autonomy to the extent possible, while protecting those with diminished autonomy, a balanced approach is reasonable. For patients deemed decisionally capable at the initiation of a study, it makes sense to involve a knowledgeable family member, or “study partner,” from the outset. This is because even if the person meets the capacity threshold, there is some degree of impairment, making the person more vulnerable than a fully cognitively intact person. Also, the patient may lose capacity over the course of the study, so the study partner’s consent may be needed. For patients who lack capacity, surrogate consent as well as patient assent is a prudent and ethically appropriate approach. However, further research is needed regarding the optimal approaches for involving caregivers or surrogate decision makers in the research process. One option to keep in mind is that most persons at early stages of AD will be able to appoint a research proxy, even if he or she is not able to consent to a protocol independently (Kim, et al., 2011).
Despite some limitations, the present findings underscore the importance of increasing our understanding of capacity and its assessment among people with AD, and not treating AD diagnosis as synonymous with an absence of capacity. In addition, it points toward future research that is needed, such as study of capacity assessment and enhancement among people with other cognitive disorders, such as MCI, stroke, and TBI. As novel treatments move from bench to bedside for these potentially vulnerable patients, our methods of assessing and addressing capacity impairment must similarly advance.
In summary, the clinical implications are:
AD is not synonymous with incapacity
Use structured assessment of research capacity
Employ population specific cut scores
Encourage execution of research proxy document when participants are still able
Acknowledgments
Source(s) of Support: This project was supported, in part, by National Institutes of Health Grants R01AG028827 and T32MH019934, and by the Department of Veterans Affairs.
Footnotes
Please note: The opinions expressed in this article are the authors’ and do not represent the views or policies of the National Institutes of Health, Department of Health and Human Services, or the US government
References
- Alzheimer's Association 2015 Alzheimer's disease facts and figures. Alzheimer's & Dementia. 2015;11(3):332. doi: 10.1016/j.jalz.2015.02.003. + from http://www.alz.org/facts/downloads/facts_figures_2015.pdf. [DOI] [PubMed] [Google Scholar]
- American Bar Association and American Psychological Association Assessment of Capacity in Older Adults Project Working Group . Assessment of older adults with diminished capacity: A handbook for lawyers. American Bar Association Commission on Law and Aging/American Psychological Association; Washington, D.C.: 2005. [Google Scholar]
- Appelbaum PS, Grisso T. MacCAT-CR: MacArthur Competence Assessment Tool for Clinical Research. Professional Resource Press; Sarasota, FL: 2001. [Google Scholar]
- Burke A, Hall G, Tariot PN. The clinical problem of neuropsychiatric signs and symptoms in dementia. Continuum (Minneap Minn) 2013;19(2 Dementia):382–396. doi: 10.1212/01.CON.0000429177.14354.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cantillon M, De La Puente AM, Palmer BW. Psychosis in Alzheimer's Disease. Seminars in Clinical Neuropsychiatry. 1998;3(1):34–40. [PubMed] [Google Scholar]
- Cummings J, Zhong K. Trial design innovations: Clinical trials for treatment of neuropsychiatric symptoms in Alzheimer's Disease. Clinical Pharmacology and Therapeutics. 2015;98(5):483–485. doi: 10.1002/cpt.190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunn LB, Nowrangi M, Palmer BW, Jeste DV, Saks E. Assessing capacity to consent to treatment and research: a review of instruments. American Journal of Psychiatry. 2006;163:1323–1334. doi: 10.1176/ajp.2006.163.8.1323. [DOI] [PubMed] [Google Scholar]
- Folstein MF, Folstein SE, McHugh PR. Mini-mental state": A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- Hoyert DL, Xu J. Deaths: Preliminary data for 2011. National Vital Statistics Reports. 2012;61(6) Retrieved from http://www.cdc.gov/nchs/data/nvsr/nvsr61/nvsr61_06.pdf. [PubMed] [Google Scholar]
- Jeste DV, Palmer BW, Appelbaum PS, Golshan S, Glorioso D, Dunn LB, Kraemer HC. A new brief instrument for assessing decisional capacity for clinical research. Archives of General Psychiatry. 2007;64:966–974. doi: 10.1001/archpsyc.64.8.966. [DOI] [PubMed] [Google Scholar]
- Jurica PL, Leitten CL, Mattis S. Professional Manual. Psychological Assessment Resources, Inc; Odessa, FL: 1991. Dementia Rating Scale-2. [Google Scholar]
- Kang SJ, Choi SH, Lee BH, Jeong Y, Hahm DS, Han IW, Na DL. Caregiver-Administered Neuropsychiatric Inventory (CGA-NPI) Journal of Geriatric Psychiatry and Neurology. 2004;17(1):32–35. doi: 10.1177/089198873258818. [DOI] [PubMed] [Google Scholar]
- Karlawish J, Kim SY, Knopman D, van Dyck CH, James BD, Marson D. Interpreting the clinical significance of capacity scores for informed consent in Alzheimer disease clinical trials. American Journal of Geriatric Psychiatry. 2008;16(7):568–574. doi: 10.1097/JGP.0b013e318172b406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karlawish JH, Casarett DJ, James BD. Alzheimer's disease patients' and caregivers' capacity, competency, and reasons to enroll in an early-phase Alzheimer's disease clinical trial. Journal of the American Geriatrics Society. 2002;50(12):2019–2024. doi: 10.1046/j.1532-5415.2002.50615.x. [DOI] [PubMed] [Google Scholar]
- Kim SY, Appelbaum PS, Swan J, Stroup TS, McEvoy JP, Goff DC, Caine ED. Determining when impairment constitutes incapacity for informed consent in schizophrenia research. British Journal of Psychiatry. 2007;191:38–43. doi: 10.1192/bjp.bp.106.033324. [DOI] [PubMed] [Google Scholar]
- Kim SY, Caine ED, Currier GW, Leibovici A, Ryan JM. Assessing the competence of persons with Alzheimer's disease in providing informed consent for participation in research. American Journal of Psychiatry. 2001;158(5):712–717. doi: 10.1176/appi.ajp.158.5.712. [DOI] [PubMed] [Google Scholar]
- Kim SY, Karlawish JH, Kim HM, Wall IF, Bozoki AC, Appelbaum PS. Preservation of the capacity to appoint a proxy decision maker: implications for dementia research. Archives of General Psychiatry. 2011;68(2):214–220. doi: 10.1001/archgenpsychiatry.2010.191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mittal D, Palmer BW, Dunn LB, Landes R, Ghormley C, Beck C, Jeste DV. Comparison of two enhanced consent procedures for patients with mild Alzheimer disease or mild cognitive impairment. American Journal of Geriatric Psychiatry. 2007;15(2):163–167. doi: 10.1097/JGP.0b013e31802dd379. [DOI] [PubMed] [Google Scholar]
- Nasreddine ZS, Phillips NA, Bedirian V, Charbonneau S, Whitehead V, Collin I, Chertkow H. The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. Journal of the American Geriatrics Society. 2005;53(4):695–699. doi: 10.1111/j.1532-5415.2005.53221.x. [DOI] [PubMed] [Google Scholar]
- Palmer BW, Cassidy EL, Dunn LB, Spira AP, Sheikh JI. Effective use of consent forms and interactive questions in the consent process. IRB: Ethics & Human Research. 2008;30(2):8–12. [PubMed] [Google Scholar]
- Palmer BW, Dunn LB, Appelbaum PS, Mudaliar S, Thal L, Henry R, Jeste DV. Assessment of capacity to consent to research among older persons with schizophrenia, Alzheimer disease, or diabetes mellitus: comparison of a 3-item questionnaire with a comprehensive standardized capacity instrument. Archives of General Psychiatry. 2005;62(7):726–733. doi: 10.1001/archpsyc.62.7.726. [DOI] [PubMed] [Google Scholar]
- Palmer BW, Lanouette NM, Jeste DV. Effectiveness of multimedia aids to enhance comprehension during research consent: A systematic review. IRB: Ethics & Human Research. 2012;34(6):1–15. [PMC free article] [PubMed] [Google Scholar]
- Palmer BW, Savla GN. The association of specific neuropsychological deficits with capacity to consent to research or treatment. Journal of the International Neuropsychological Society. 2007;13:1047–1059. doi: 10.1017/S1355617707071299. [DOI] [PubMed] [Google Scholar]
- Palmer BW, Savla GN, Harmell AL. Healthcare decision-making capacity. In: Demakis GJ, editor. Civil capacities in clinical neuropsychology: Research findings and practical applications. Oxford University Press; New York: 2012. pp. 69–94. [Google Scholar]
- Rubright J, Sankar P, Casarett DJ, Gur R, Xie SX, Karlawish J. A memory and organizational aid improves Alzheimer disease research consent capacity: results of a randomized, controlled trial. American Journal of Geriatric Psychiatry. 2010;18(12):1124–1132. doi: 10.1097/JGP.0b013e3181dd1c3b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheehan DV, Lecrubier Y, Sheehan KH. The Mini-International Neuropsychiatric Interview (M.I.N.I.): The development of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. Journal of Clinical Psychiatry. 1998;59:22–33. [PubMed] [Google Scholar]
- Simpson C. Decision-making capacity and informed consent to participate in research by cognitively impaired individuals. Applied Nursing Research. 2010;23(4):221–226. doi: 10.1016/j.apnr.2008.09.002. [DOI] [PubMed] [Google Scholar]
- Stroup S, Appelbaum P, Swartz M, Patel M, Davis S, Jeste D, Lieberman J. Decision-making capacity for research participation among individuals in the CATIE schizophrenia trial. Schizophrenia Research. 2005;80(1):1–8. doi: 10.1016/j.schres.2005.08.007. [DOI] [PubMed] [Google Scholar]
- Taub HA, Baker MT. The effect of repeated testing upon comprehension of informed consent materials by elderly volunteers. Experimental Aging Research. 1983;9(3):135–138. doi: 10.1080/03610738308258441. [DOI] [PubMed] [Google Scholar]
- Warner J, McCarney R, Griffin M, Hill K, Fisher P. Participation in dementia research: rates and correlates of capacity to give informed consent. Journal of Medical Ethics. 2008;34(3):167–170. doi: 10.1136/jme.2006.019786. [DOI] [PubMed] [Google Scholar]