Abstract
Whether the lower risk of mortality associated with arteriovenous fistula use in hemodialysis patients is due to the avoidance of catheters or if healthier patients are simply more likely to have fistulas placed is unknown. To provide clarification, we determined the proportion of access-related deaths in a retrospective cohort study of patients aged ≥18 years who initiated hemodialysis between 2004 and 2012 at five Canadian dialysis programs. A total of 3168 patients initiated dialysis at the participating centers; 2300 met our inclusion criteria. Two investigators independently adjudicated cause of death using explicit criteria and determined whether a death was access-related. We observed significantly lower mortality in individuals who underwent a predialysis fistula attempt than in those without a predialysis fistula attempt in patients aged <65 years (hazard ratio [HR], 0.49; 95% confidence interval [95% CI], 0.29 to 0.82) and in the first 2 years of follow-up in those aged ≥65 years (HR0–24 months, 0.60; 95% CI, 0.43 to 0.84; HR24+ months, 1.83; 95% CI, 1.25 to 2.67). Sudden deaths that occurred out of hospital accounted for most of the deaths, followed by deaths due to cardiovascular disease and infectious complications. We found only 2.3% of deaths to be access-related. In conclusion, predialysis fistula attempt may associate with a lower risk of mortality. However, the excess mortality observed in patients treated with catheters does not appear to be due to direct, access-related complications but is likely the result of residual confounding, unmeasured comorbidity, or treatment selection bias.
Keywords: hemodialysis access, hemodialysis, arteriovenous fistula
Arteriovenous fistulas (“fistulas”) are considered the preferred form of vascular access for hemodialysis (HD) and are actively promoted. Canadian, American, and European guidelines cite evidence from observational studies that fistulas are associated with better patient survival, the lowest risk of complications, and are the least expensive form of creating and maintaining access.1–6 These guidelines recommend that all suitable candidates undergo an attempt at fistula creation prior to starting HD.7–9
However, a systematic review of this observational literature demonstrated a high risk of bias in studies comparing outcomes of patients treated with different forms of vascular access.10 Specifically, although access-related complications might explain the increased risk of death in patients treated with central venous catheters, it may also be due to the fact that sicker patients are more likely to be treated with them. One way to address this potential bias is to determine if the excess mortality observed in patients treated with catheters is attributable to access-related complications. Unfortunately, the majority of prior studies have not reported detailed information about cause of death.2–6
We compared mortality in incident HD patients who underwent a fistula attempt prior to starting dialysis to those who did not have an attempt. We then examined causes of death and determined the proportion of deaths adjudicated to be access-related. This allowed us to determine how much of the excess mortality in patients who did not have a fistula creation prior to dialysis initiation was directly attributable to their vascular access.
Results
A total of 3168 patients initiated dialysis at the five participating centers during the study period. Six hundred and sixty-six patients were excluded because they were treated with peritoneal dialysis (PD) initially (n=524), or within 6 months of starting dialysis (n=142). A further 130 patients were treated with grafts during follow-up and were excluded. Seventy patients had a limited life expectancy due to one, or a combination of terminal malignancy at baseline (n=56), end-stage liver disease (n=9), end-stage cardiac disease (n=4), and end-stage lung disease (n=2). Two patients were missing information about date of birth. A total of 2300 patients met our inclusion criteria.
Four hundred and eighty-seven patients (21%) underwent a predialysis fistula attempt and 1813 (79%) patients did not. Baseline characteristics are presented in Table 1, according to age category and whether they underwent a predialysis fistula attempt. Patients who had undergone a predialysis fistula attempt were more likely to have received at least 4 months of predialysis care, had higher body mass indexes (BMIs), serum albumin, calcium, and hemoglobin levels at baseline, regardless of age. Patients who had undergone a predialysis fistula attempt had lower eGFR at dialysis initiation and were less likely to have started in hospital or the intensive care unit, and to have a history of congestive heart failure, regardless of age. Median follow-up time was longer in the attempt group compared with the no attempt group (18 versus 11 months in those <65 years [P value <0.01]; 23 versus 9 months in those ≥65 years [P value <0.01]). Patients in the attempt group were more likely to receive a transplant and were less likely to recover kidney function (see Table 2).
Table 1.
Characteristics of the study cohort, by age and whether patient received a predialysis fistula attempt
| Baseline characteristics | <65 yr | ≥65 yr | ||||
|---|---|---|---|---|---|---|
| No Attempt | Attempt | P Value | No Attempt | Attempt | P Value | |
| n=795 | n=212 | n=1018 | n=275 | |||
| Age, median (IQR) | 54 (44, 60) | 56 (47, 61) | 0.07 | 75.3 (70, 81) | 76 (71, 80.1) | 0.81 |
| Male, n (%) | 493 (62) | 141 (67) | 0.23 | 613 (60) | 169 (62) | 0.71 |
| Initiation of dialysis | ||||||
| Predialysis care, n (%) | ||||||
| Any | 531 (67) | 212 (100) | <0.01 | 733 (72) | 275 (100) | <0.01 |
| ≥4 mo | 406 (51) | 199 (94) | <0.01 | 584 (57) | 268 (98) | <0.01 |
| ≥12 mo | 301 (38) | 165 (78) | <0.01 | 468 (46) | 234 (85) | <0.01 |
| Inpatient start | 535 (67) | 37 (18) | <0.01 | 720 (71) | 83 (30) | <0.01 |
| ICU start | 166 (21) | 3 (1) | <0.01 | 210 (21) | 7 (3) | <0.01 |
| eGFR, median (IQR) | 8.4 (6, 12.2) | 7.3 (5.6, 9.2) | <0.01 | 9.3 (6.6, 12.7) | 8.8 (7.3, 10.8) | 0.11 |
| eGFR category, n (%) | <0.01 | <0.01 | ||||
| <10 | 473 (60) | 167 (79) | 569 (56) | 181 (66) | ||
| 10–15 | 181 (23) | 34 (16) | 285 (28) | 81 (30) | ||
| >15 | 125 (16) | 8 (4) | 143 (14) | 11 (4) | ||
| Comorbidities, n (%) | ||||||
| Diabetes | 467 (59) | 132 (62) | 0.35 | 527 (52) | 158 (58) | 0.09 |
| Coronary artery disease | 203 (26) | 55 (26) | 0.90 | 475 (47) | 110 (40) | 0.05 |
| Congestive heart failure | 181 (23) | 31 (15) | 0.01 | 398 (39) | 69 (25) | <0.01 |
| Cerebrovascular disease | 78 (10) | 25 (12) | 0.40 | 215 (21) | 50 (18) | 0.28 |
| Peripheral vascular disease | 107 (14) | 27 (13) | 0.78 | 245 (24) | 42 (15) | <0.01 |
| Cancer | 73 (9) | 16 (8) | 0.46 | 274 (27) | 61 (22) | 0.11 |
| BMI, median (IQR) | 27.3 (23.6, 32) | 29.7 (25.9, 35) | <0.01 | 26.2 (23, 30.4) | 27.2 (23.9, 31) | 0.03 |
| Laboratory measurements | ||||||
| Albumin, g/L, mean (SD) | 28.9 (7.5) | 32.4 (6.5) | <0.01 | 29.9 (6.9) | 33.1 (6) | <0.01 |
| Bicarbonate, mmol/L, median (IQR) | 19 (16, 23) | 19 (16, 22) | 0.17 | 20 (17, 24) | 20 (17, 23) | 0.41 |
| Calcium, mmol/L, mean (SD) | 2 (0.2) | 2.1 (0.2) | <0.01 | 2.1 (0.2) | 2.2 (0.2) | <0.01 |
| Creatinine, µmol/L, median (IQR) | 576 (423, 797) | 676 (557, 824) | <0.01 | 505 (380, 668) | 528 (436, 638) | 0.09 |
| Hemoglobin, g/L, mean (SD) | 92.9 (16.7) | 99.2 (16.7) | <0.01 | 95.5 (15.4) | 101.7 (15.7) | <0.01 |
| Parathyroid hormone, pmol/L, median (IQR) | 268 (138, 474) | 282 (138, 418) | 0.59 | 256 (141, 421) | 182 (110, 307) | <0.01 |
| Phosphate, mmol/L, mean (SD) | 2 (0.7) | 2 (0.5) | 0.60 | 1.9 (0.6) | 1.7 (0.4) | <0.01 |
| Urea, mmol/L, mean (SD) | 31.7 (12.1) | 32.9 (9.9) | 0.18 | 33.3 (12) | 32.5 (9.9) | 0.37 |
IQR, interquartile range; ICU, intensive care unit.
Table 2.
Participant follow-up and outcomes
| <65 yr | ≥65 yr | |||||
|---|---|---|---|---|---|---|
| No Attempt | Attempt | P Value | No Attempt | Attempt | P Value | |
| n=795 | n=212 | n=1018 | n=275 | |||
| Follow-up time, mo, median (IQR) | 10.7 (3.6, 23.9) | 18 (9.1, 34.2) | <0.01 | 9.2 (3.5, 23.7) | 22.5 (9.8, 34.6) | <0.01 |
| Reason for termination of follow-up, n (%) | <0.01 | <0.01 | ||||
| End of study | 381 (48) | 139 (66) | 427 (42) | 147 (54) | ||
| Dead | 141 (18) | 20 (9) | 355 (35) | 101 (37) | ||
| Transplant | 65 (8) | 39 (18) | 8 (<1) | 3 (1) | ||
| Recovery | 119 (15) | 0 | 115 (11) | 3 (1) | ||
| Transfer | 54 (67) | 6 (3) | 82 (8) | 18 (7) | ||
| Lost | 1 (<1) | 0 | 1 (<1) | 1 (<1) | ||
| Switched to PD | 34 (4) | 8 (4) | 30 (3) | 2 (<1) | ||
IQR, interquartile range.
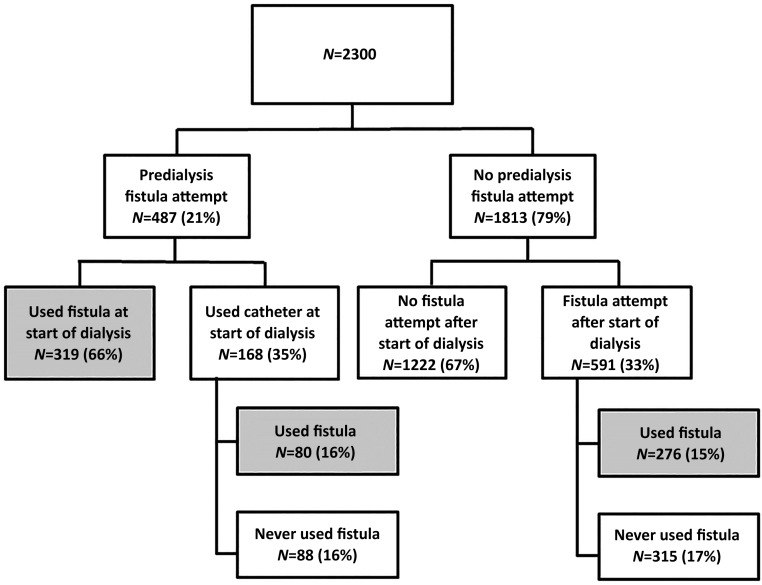
Fistula Attempts and Independent Fistula Use
A total of 389 (80%) of the patients who underwent a fistula attempt prior to the start of dialysis went on to independent fistula use at some point during follow-up (319 [66%] started dialysis using a fistula; an additional 80 [16%] went on to independent fistula use after the start of dialysis). Of the patients who did not undergo a predialysis fistula attempt, 591 (33%) underwent a fistula attempt after the start of dialysis and 276 (15%) used the fistula independently during follow-up (see Figure 1).
Figure 1.
Fistula attempts and independent fistula use in cohort of incident HD patients. A total of 2300 patients met our inclusion criteria and 21% received a predialysis fistula attempt. The majority started dialysis with an independently functioning fistula and 82% used the fistula independently throughout follow-up. In those who did not attempt a fistula prior to the start of dialysis, 33% attempted fistula creation during follow-up and 15% used them independently. Independent fistula use was defined as catheter-free fistula use.
The Association between Predialysis Fistula Attempt and Mortality
We tested for an interaction between age at the initiation of dialysis and predialysis fistula attempt (P value for interaction term = 0.01), and analyses were stratified by age. In those aged >65 years, there was a violation of proportional hazards, such that the impact of predialysis fistula attempt changed over time. We therefore reported results for the first 24 months following dialysis initiation and the period after 24 months separately. Forest plots showing the impact of predialysis fistula attempt on all-cause mortality are presented in Figure 2.
Figure 2.
Forest plot for all-cause mortality according to whether patient received a predialysis fistula attempt, by age group and time from dialysis initiation. We identified a significant interaction between age and fistula attempt when modeling the outcome of mortality. Accordingly, Cox models were stratified by age (<65 years and ≥65 years) and adjusted for important baseline variables. Predialysis fistula attempt was associated with lower mortality in younger patients and in the first 24 months of therapy among those ≥65 years. After 24 months, the risk of mortality was significantly higher in those who had attempted a fistula prior to the start of dialysis. *Adjusted for sex, BMI, at least 4 months or predialysis care, inpatient start, cancer, cerebrovascular disease, congestive heart failure, coronary artery disease, diabetes, gastrointestinal bleeding, peripheral vascular disease, polycystic kidney disease, albumin, hemoglobin, and eGFR.
In patients aged <65 years, we observed significantly lower mortality in individuals who underwent a predialysis fistula attempt, compared with those without a predialysis fistula attempt (hazard ratio [HR], 0.49; 95% confidence interval [95% CI], 0.29 to 0.82). In patients aged ≥65 years, there was a similar lower mortality in the first 24 months of therapy (HR, 0.60; 95% CI, 0.43 to 0.84] associated with a predialysis fistula attempt. However, there was a significantly higher mortality observed after 24 months of follow-up (HR, 1.83; 95% CI, 1.25 to 2.67).
The Association between Fistula Use and Mortality in Those Undergoing a Predialysis Fistula Attempt
The interaction between age at the initiation of dialysis and use of a fistula as the initial form of access for HD was again significant (P value for interaction term = 0.02), and analyses were stratified by age. In patients aged <65 years, we observed a significantly lower mortality in those who attempted a fistula and used it to start dialysis (HR, 0.26; 95% CI, 0.08 to 0.90). In patients aged ≥65 years, there was no significant difference in outcomes among those patients who used a fistula and those who used a catheter as the first form of vascular access for HD (HR, 0.92; 95% CI, 0.57 to 1.47).
Access-Related Complications as a Cause of Death
A total of 617 deaths occurred in our cohort during follow-up. The majority were sudden deaths that occurred out of hospital (n=230; 37%), followed by deaths due to cardiovascular disease (n=127; 21%) and infectious complications (n=93, 15%). Inter-rater reliability was substantial for cause of death (Cohen κ =0.65).11,12 For the classification of death as either access-related or not, there was 98% agreement between observers, but because access-related deaths were rare and expected agreement was high, inter-rater reliability was moderate (Cohen κ =0.58).11,12 Crude rates of death according to cause are presented in Figure 3. Of note, only 14 of 617 (2%) deaths were considered access-related; results cannot be reported by group given cell sizes, per local privacy standards. Overall, ten of 14 (71%) access-related deaths were due to complications of catheters; the remainder were due to complications of fistulas (three of 14; 21%) and PD catheters (one of 14; 7%).
Figure 3.
Death rates, per 1000 person-years, by cause of death and according to whether patient received a predialysis fistula attempt. The rate of death was higher in those who underwent a predialysis fistula attempt, for all categories of cause of death examined. Patients with a limited life expectancy due to malignancy or other chronic diseases were excluded from the analysis. Total follow-up time in the no attempt group was 2515 person-years and 1029 person-years in the attempt group.
Excess Mortality Attributable to Access-Related Complications
The excess mortality observed in patients who did not undergo a predialysis fistula attempt was equivalent to 79.7 deaths per 1000 patient-years of follow-up. However, the excess mortality attributable to access-related complications was only 0.1 deaths per 1000 patient-years in those who did not undergo a fistula attempt prior to starting dialysis. Figure 4 shows the crude rate of death in both groups, according to age group. Similar trends are observed in that the crude rate of death is lower in those who received a fistula attempt predialysis, and the fraction of the death rate attributable to access-related complications is quite small, regardless of age. The crude rate of access-related death was higher in patients aged ≥65 years who attempted a fistula prior to the start of dialysis.
Figure 4.
Rates of access-related and nonaccess related death per 1000 person-years of follow-up, by age, and according to whether patient received a predialysis fistula attempt. Although the rates of death were highest in older patients and in those who had not undergone a predialysis fistula attempt, the rates of access-related death were low in all groups, regardless of age. In patients aged <65 years, the rates of death per 1000 person-years of follow-up were 4.4 (95% CI, 1.8 to 10.7; total 1126 person-years follow-up) in those who did not attempt a fistula predialysis compared with 2.3 (95% CI, 0.3 to 16.0; 443 person-years follow-up) in those who did. In patients aged ≥65 years, rates of death per 1000 person-years of follow-up were 3.6 (95% CI, 1.5 to 8.6; 1389 person-years follow-up) in those who did not attempt a fistula predialysis compared with 5.1 (95% CI, 1.7 to 15.9; 586 person-years follow-up) in those who did. AVF, arteriovenous fistula.
Discussion
We found that incident HD patients who had undergone a predialysis fistula attempt had a lower risk of death. We also found that, in those who attempted a fistula predialysis, use of the fistula was associated with a lower risk of death in patients aged <65 years, but not in patients aged ≥65 years. The vast majority of deaths were not related to complications of vascular access, suggesting that predialysis fistula attempt could be a surrogate marker for a healthy patient who has had predialysis care, or the benefit observed is due to an indirect mechanism. Much of the excess mortality observed in patients treated with catheters may be due to residual confounding, unmeasured comorbidity, or treatment selection bias, rather than directly due to access-related complications. Catheters are used preferentially in patients with AKI, short life expectancy, and in those with poor vessels, making the risk of bias in observational studies very high. This finding has important implications for clinical care, research, and current guideline and policy recommendations.
In reports from North American institutions, approximately half of elderly patients who undergo a fistula creation attempt prior to the start of HD will use it as their first form of vascular access.13,14 In our study, 66% of patients who underwent a fistula creation attempt prior to starting HD used it as their first form of vascular access and 80% went on to use it at some time during follow-up. Those who underwent a fistula attempt prior to the start of dialysis had a significantly lower risk of death—a finding consistent with other studies. A report from the Canadian Organ Replacement Register showed a 61% increase in the relative hazard of death in incident HD patients in Canada who used a catheter for vascular access.2 DeSilva et al. showed that patients aged >67 years who received a catheter as the first predialysis access placed had a 77% higher relative hazard of death compared with those who had a fistula as the first predialysis access.15 Prior studies from the United States have shown a 40%–70% increase in mortality in those treated with a catheter compared with those treated with a fistula3,4,6 and a systematic review of the literature suggested a 53% higher risk of death.10
Constructing a fair comparison of catheters to fistulas is challenging due to the fact that relatively healthy patients are selected for fistula attempts and the sickest patients will be treated almost exclusively with catheters. First, individuals who start dialysis urgently are typically included in these studies, are at a high risk of death, and are treated preferentially with catheters.16 Second, in clinical practice, the only patients faced with a choice between fistulas and catheters are those who are eligible for both. Those who are not eligible for a fistula have traditionally been included in the catheter cohort in these types of analyses, as information about eligibility is not available, and have a higher risk of mortality.17 Finally, in order to inform clinical decision-making, patients should be compared based on the intended form of access, rather than the access that is ultimately achieved. Most prior analyses have instead compared those who had a successful fistula attempt to all patients using a catheter. This indication bias is difficult to overcome in the absence of randomization and may not be addressed through the use of simple risk adjustment.
One potential way to distinguish between outcomes that occur because a patient has a poor prognosis and those that are a direct consequence of their access is to focus on access-related outcomes. We had detailed clinical data available to us and this study provides important insights into the possible reasons for the excess mortality observed in patients treated with catheters. We elected to review all patient deaths and classify them according to cause of death and whether they were deemed to be access-related. We hypothesized that, if catheters were causally related to the increased risk of death, a substantial proportion of deaths would be due to complications of vascular access. Alternatively, if patients treated with catheters are simply sicker, the majority of deaths would be due to comorbidities and unrelated to complications of vascular access. We studied a large, multicenter prospective cohort with detailed clinical data, collected with rigorous oversight, to ensure accurate measurement and consistent coding of information. This provided a unique opportunity to explore this relationship and our findings suggest that access-related complications are a relatively rare cause of death among incident HD patients, regardless of vascular access type. In addition, nearly all causes of death were more common in the group that did not attempt a fistula, even those causes of death that would not be expected to increase with exposure to a catheter. This suggests that the excess mortality observed in patients treated with catheters is not associated with the presence of the catheter, but instead reflects differences in the health of patients selected for an attempt at fistula creation.
A second way to address the inherent treatment selection bias in comparisons of fistulas and catheters is to restrict the population studied. In a secondary analysis, we isolated individuals who had an attempt at fistula creation prior to the start of dialysis, and were therefore deemed eligible for a fistula attempt. We then compared the outcomes of those who had a functioning fistula at the time of dialysis initiation to those whose fistulas were not functioning and were forced to use a catheter. In younger patients, we observed a significantly lower risk of mortality among those whose fistulas were usable at the time they started dialysis. This may relate to the fact that fistula use is protective and spares patients from the complications of catheters, or it may reflect the fact that young patients who cannot mature a fistula or who start dialysis urgently are at a higher risk of mortality. Given that very few deaths were access-related, it seems that the latter explanation is more likely. Interestingly, we observed no difference in mortality among patients aged ≥65 years who used a fistula compared with those who had a nonfunctioning fistula. This finding reinforces the fact that the important predictor of outcomes in older patients is being identified as healthy enough for a fistula attempt, not whether that fistula attempt is successful.
Prior studies have shown a higher risk of infectious3–5 and cardiovascular complications3 in those treated with catheters. While some have suggested that chronic inflammation leads to a higher risk of cardiovascular events,18 the majority of the excess mortality observed in patients who use catheters is felt to be attributable to infections. The rate of catheter-related bacteremia in Canadian programs is <0.5 events per 1000 catheter-days, or an average of one catheter-related bacteremia every 5.5 years.19 Given that only a small percentage of these events are fatal, it has been difficult to reconcile the significant absolute increase in mortality historically observed in patients treated with catheters.10 We found that patients who did not receive a fistula creation attempt had an excess of infection-related mortality, consistent with prior studies, but only 2% of deaths were classified as access-related. This suggests that the higher infection-related mortality observed previously may be due to the fact that patients with a greater comorbid burden, who are likely more susceptible to infectious complications, are treated preferentially with catheters.
Our study also has several limitations. Ultimately, a randomized controlled trial is the ideal way to test the efficacy and safety of fistula attempts in an unbiased fashion. Despite our attempts to reduce the impact of confounding in our results, there is likely residual bias given that patients in whom fistulas are attempted are almost certainly different than patients who do not undergo a fistula attempt. In addition, classifying outcomes as access-related may include a subjective component. However, we had good inter-rater reliability, made every attempt to blind adjudicators to exposure status, and used clear definitions for defining cause of death and what was considered access-related. We used a conservative approach in situations where deaths were possibly, but not certainly access-related, and classified them as access-related. It is also possible that catheters lead to increased mortality by other, less direct mechanisms, such as chronic inflammation. This would not be captured as an access-related death in our analysis. There were also a number of sudden deaths that occurred outside the hospital where it is very difficult to determine the exact cause of death with certainty. Finally, our data are from Canadian dialysis programs where catheter use is high and rates of catheter-related bloodstream infections are generally low. As a consequence, the proportion of deaths related to access-related complications may be different in other jurisdictions and our results may not be generalizable to these settings.
Our results have important implications for vascular access research, clinical practice, and guideline recommendations. Our findings call into question the belief that the higher risk of death among patients treated with catheters is, in fact, due to complications of their access. Instead, our findings suggest that prior comparisons may be confounded by underlying differences in the health of patients who receive different access types—an issue that we may be able to address only through randomization. Current guidelines recommend fistulas as the preferred form of access,7–9 but they are based on low-quality evidence at high risk of bias.10 Despite this, many jurisdictions around the world are actively promoting fistulas and dedicating significant resources to increasing the proportion of patients treated with fistulas. There is a clear evidence gap that should be addressed to ensure that efforts to promote fistulas are appropriate and do not have unintended consequences for patients in the form of adverse events that could ultimately lead to diminished quality of life for patients, the potential for harm, and increased resource use and costs. As support for these initiatives increases and pressure to hit fistula utilization targets intensifies, it will become much more difficult to study this question in a clinical trial. To that end, we are planning a pilot randomized controlled trial to determine the feasibility of conducting a larger study comparing all-cause mortality, by access type (Clinicaltrials.gov identifier: NCT02675569).
In summary, we found that incident HD patients who underwent a predialysis fistula attempt had a lower risk of death than those who did not. However, much of the excess mortality observed in patients treated with catheters may be due to residual confounding, unmeasured comorbidity, and treatment selection bias, rather than from the direct effects from access-related complications. This finding has important implications for clinical care, research, and current guideline and policy recommendations.
Concise Methods
Data Sources
We used data from the Dialysis Measurement Analysis and Reporting (DMAR) system, supplemented by chart review. DMAR prospectively collects high-quality data for the purposes of quality improvement using a web-based data collection platform. Data are entered by trained, front-line staff, based on a standardized coding scheme. Data elements include detailed information on comorbidities, laboratory values, demographic characteristics, predialysis care history, and acuity of dialysis start. In addition, all vascular access procedures and the indication for the procedures are captured, as are dialysis modality changes, hospitalizations, transplants, loss to follow-up, transfers out of the program, and deaths. To ensure data quality, all data elements collected at the participating sites are double-reviewed by the same two investigators (R.Q. and M.O.). Queries are communicated in real-time to end users and must be rectified prior to analysis.
Patient Population
We identified adult patients aged >18 years initiating HD between January 1, 2004 and May 31, 2012 at the five Canadian sites participating in DMAR (London Health Sciences Centre, the Ottawa Hospital, Sunnybrook Health Sciences Centre, the Manitoba Renal Program, and the Southern Alberta Renal Program, Calgary Region). Individuals who had ESRD in the opinion of their attending nephrologist, those who received outpatient dialysis, and those with AKI requiring dialysis for a period of ≥28 days were included in the study. Patients were excluded from the study if they initiated therapy following a failed kidney transplant, were treated with PD within 6 months of starting dialysis, or had a limited life expectancy at baseline due to metastatic cancer or other terminal illness. Patients treated with arteriovenous grafts for HD access were also excluded due to the small numbers of patients treated with them.
Predialysis Fistula Attempt and Fistula Use
Individuals were classified based on whether they had undergone a predialysis fistula attempt of any type (e.g., radiocephalic, brachiocephalic, brachiobasilic, or variants). Individuals who had received at least one fistula attempt prior to the initiation of HD were assigned to the “attempt” group and those who had no predialysis attempt at a fistula creation were assigned to the “no attempt” group. We also determined what proportion of patients had an attempt at any point during follow-up, as well as the proportion that used a fistula independently for the first dialysis treatment and what proportion went on to independent fistula use. Independent fistula use was defined as the point at which the fistula alone was used for HD access and the catheter was removed, if one was in place.
Outcomes of Interest
Patients were followed from the time of initiation of dialysis until kidney transplantation, change in dialysis treatment modality (e.g., switch to PD, patients who switched to PD after >6 months of dialysis), move to another program, recovery of kidney function, death, or end of the study period (August 31, 2012). Our primary outcome of interest was all-cause mortality. All deaths were reviewed by the same two investigators (R.Q. and K.P.) independently, and classified into one of six categories of cause of death: cardiovascular, infectious, malignancy-related, elective withdrawal from dialysis, sudden death at home, or other (see Supplemental Appendix). For patients who died in hospital, cause of death was classified based on the condition that led to the admission. For patients who died as an outpatient, all recent interventions and hospitalizations were reviewed along with notes regarding the cause of death. In situations where patients died suddenly at home, cause of death was classified as “sudden death”. Once deaths were classified into one of the six categories for cause of death, they were also classified according to whether they were access-related or not. Deaths were considered access-related if they resulted from a direct complication of the access or any access-related procedures (e.g., complications of catheter-related bacteremia leading to death). An inclusive definition of access-related death was employed. If a patient was admitted to hospital with an access-related complication and died during that hospitalization, the death was considered access-related. If a patient had undergone an access-related procedure or experienced an access-related complication within 1 month of the date of death, the death was reviewed in detail to determine if it could possibly be access-related. Access-related deaths in both groups were further subclassified as catheter-related deaths, fistula-related deaths, or PD catheter-related deaths. The classification of causes of death was done in a blinded fashion, with no prior knowledge of exposure status, to the extent that this was possible. In other words, adjudication was done without knowledge of whether the patient had a fistula attempt prior to the start of dialysis. In cases where there was disagreement, consensus was reached after discussion and review of the individual cases without the need to involve a third reviewer.
Statistical Analyses
After assessing distributional assumptions, we compared baseline characteristics between groups using unpaired, two-sided t tests or Wilcoxon rank-sum tests for continuous variables, and chi-squared tests for categorical variables. We used Cohen κ statistic to measure reliability between two investigators who categorized deaths as access-related or nonaccess-related. We compared survival by exposure group using a Cox proportional hazards model. In cases where the proportional hazards assumption was not met, we split time into bands of equal duration. We identified a significant interaction between age and fistula attempt when modeling the outcome of mortality. Accordingly, Cox models were stratified by age (<65 years and ≥65 years) and adjusted for sex, predialysis care of at least 4 month’s duration, inpatient dialysis start, eGFR at initiation, diabetes, coronary artery disease, congestive heart failure, peripheral vascular disease, cancer, cerebrovascular disease, polycystic kidney disease, gastrointestinal bleeding, albumin, hemoglobin, and BMI. We used multivariate normal multiple imputation for missing values of adjustment covariates (BMI, albumin, hemoglobin, and creatinine were missing in 7.4%, 4.6%, 2.0%, and 1.8% of cases, respectively) prior to running the Cox model, and conducted a sensitivity analysis using case-wise deletion for missing values. Analyses were repeated using robust variance and stratification to account for clustering within programs. This did not materially change our results. We evaluated the proportional hazards assumption graphically using log-log plots, mathematically by examining Schoenfeld residuals, and assessed model fit using Cox–Snell residuals. We performed a secondary analysis to look at the impact of starting HD with a functioning fistula at the time of dialysis initiation. This analysis was restricted to those with a predialysis fistula attempt in order to minimize the impact of patient selection on outcomes. We calculated unadjusted death rates per 1000 person-years of follow-up overall, and by individual causes of death. A level of significance of 0.05 was used. All analyses were conducted in SAS Version 9.2 (SAS Institute Inc., Cary, NC) and Stata Version 11 (www.stata.com; StataCorp., College Station, TX). Ethics approval was obtained separately at all participating sites.
Disclosures
R.Q. and M.O. coinvented the Dialysis Measurement Analysis and Reporting system.
Supplementary Material
Acknowledgments
This study was supported by the Institute for Clinical Evaluative Sciences (ICES), which is funded by an annual grant from the Ontario Ministry of Health and Long-Term Care (MOHLTC). This work was supported by the Canadian Institutes of Health Research (CIHR) (funding reference numbers 130514 and 119366). R.Q. and P.R. were supported by CIHR, Ashford foundation, and Medical Services Incorporated.
The opinions, results, and conclusions reported in this paper are those of the authors and are independent from the funding sources. No endorsement by ICES or the Ontario MOHLTC is intended or should be inferred.
Footnotes
Published online ahead of print. Publication date available at www.jasn.org.
See related editorial, “Vascular Access for Hemodialysis and Value-Based Purchasing for ESRD,” on pages 395–397.
This article contains supplemental material online at http://jasn.asnjournals.org/lookup/suppl/doi:10.1681/ASN.2016020151/-/DCSupplemental.
References
- 1.Lee H, Manns B, Taub K, Ghali WA, Dean S, Johnson D, Donaldson C: Cost analysis of ongoing care of patients with end-stage renal disease: the impact of dialysis modality and dialysis access. Am J Kidney Dis 40: 611–622, 2002 [DOI] [PubMed] [Google Scholar]
- 2.Moist LM, Trpeski L, Na Y, Lok CE: Increased hemodialysis catheter use in Canada and associated mortality risk: data from the Canadian Organ Replacement Registry 2001-2004. Clin J Am Soc Nephrol 3: 1726–1732, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dhingra RK, Young EW, Hulbert-Shearon TE, Leavey SF, Port FK: Type of vascular access and mortality in U.S. hemodialysis patients. Kidney Int 60: 1443–1451, 2001 [DOI] [PubMed] [Google Scholar]
- 4.Pastan S, Soucie JM, McClellan WM: Vascular access and increased risk of death among hemodialysis patients. Kidney Int 62: 620–626, 2002 [DOI] [PubMed] [Google Scholar]
- 5.Polkinghorne KR, McDonald SP, Atkins RC, Kerr PG: Vascular access and all-cause mortality: a propensity score analysis. J Am Soc Nephrol 15: 477–486, 2004 [DOI] [PubMed] [Google Scholar]
- 6.Astor BC, Eustace JA, Powe NR, Klag MJ, Fink NE, Coresh J; CHOICE Study : Type of vascular access and survival among incident hemodialysis patients: the Choices for Healthy Outcomes in Caring for ESRD (CHOICE) Study. J Am Soc Nephrol 16: 1449–1455, 2005 [DOI] [PubMed] [Google Scholar]
- 7.Jindal K, Chan CT, Deziel C, Hirsch D, Soroka SD, Tonelli M, Culleton BF; Canadian Society of Nephrology Committee for Clinical Practice Guidelines : Hemodialysis clinical practice guidelines for the Canadian Society of Nephrology. J Am Soc Nephrol 17[Suppl 1]: S1–S27, 2006 [DOI] [PubMed] [Google Scholar]
- 8.Tordoir J, Canaud B, Haage P, Konner K, Basci A, Fouque D, Kooman J, Martin-Malo A, Pedrini L, Pizzarelli F, Tattersall J, Vennegoor M, Wanner C, ter Wee P, Vanholder R: EBPG on Vascular Access. Nephrol Dial Transplant 22[Suppl 2]: ii88–ii117, 2007 [DOI] [PubMed] [Google Scholar]
- 9.Vascular Access Work Group : Clinical practice guidelines for vascular access. Am J Kidney Dis 48[Suppl 1]: S248–S273, 2006 [DOI] [PubMed] [Google Scholar]
- 10.Ravani P, Palmer SC, Oliver MJ, Quinn RR, MacRae JM, Tai DJ, Pannu NI, Thomas C, Hemmelgarn BR, Craig JC, Manns B, Tonelli M, Strippoli GF, James MT: Associations between hemodialysis access type and clinical outcomes: a systematic review. J Am Soc Nephrol 24: 465–473, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Landis JR, Koch GG: The measurement of observer agreement for categorical data. Biometrics 33: 159–174, 1977 [PubMed] [Google Scholar]
- 12.Cohen J: A coefficient of agreement for nominal scales. Educ Psychol Meas 20: 37–46, 1960 [Google Scholar]
- 13.Hod T, Patibandla BK, Vin Y, Brown RS, Goldfarb-Rumyantzev AS: Arteriovenous fistula placement in the elderly: when is the optimal time? J Am Soc Nephrol 26: 448–456, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lee T, Thamer M, Zhang Y, Zhang Q, Allon M: Outcomes of Elderly Patients after Predialysis Vascular Access Creation. J Am Soc Nephrol 26: 3133–3140, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.DeSilva RN, Patibandla BK, Vin Y, Narra A, Chawla V, Brown RS, Goldfarb-Rumyantzev AS: Fistula first is not always the best strategy for the elderly. J Am Soc Nephrol 24: 1297–1304, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tennankore KK, Soroka SD, Kiberd BA. The impact of an “acute dialysis start” on the mortality attributed to the use of central venous catheters: A retrospective cohort study. BMC Nephrol 13: 72, 2012. [DOI] [PMC free article] [PubMed]
- 17.Mazonakis E, Stirling C, Booth KL, McClenahan J, Heron N, Geddes CC: The influence of comorbidity on the risk of access-related bacteremia in chronic hemodialysis patients. Hemodial Int 13: 6–10, 2009 [DOI] [PubMed] [Google Scholar]
- 18.van Leuven SI, Franssen R, Kastelein JJ, Levi M, Stroes ES, Tak PP: Systemic inflammation as a risk factor for atherothrombosis. Rheumatology (Oxford) 47: 3–7, 2008 [DOI] [PubMed] [Google Scholar]
- 19.Battistella M, Bhola C, Lok CE: Long-term follow-up of the Hemodialysis Infection Prevention with Polysporin Ointment (HIPPO) Study: a quality improvement report. Am J Kidney Dis 57: 432–441, 2011 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.