Abstract
Globally, adult intensive care units routinely use the International Society on Thrombosis and Haemostasis (ISTH) scoring system for identifying overt disseminated intravascular coagulation (DIC). However, in our pediatric intensive care unit, a modified diagnostic criterion (Texas Children’s Hospital [TCH] criteria) that requires serial monitoring of the coagulation variables is employed. A retrospective analysis of 2,136 DIC panels from 130 patients who had at least 4 DIC panels during 1 admission to a pediatric intensive care unit was done to compare the diagnostic utility of the TCH criteria with the ISTH scoring method in children. Both scoring systems were evaluated against the gold standard diagnostic method of autopsy confirmation of DIC in the subset of children who died. Receiver operating characteristic analysis indicates that TCH diagnostic criteria are comparable to the ISTH scoring method (area under the curve of 0.878 for TCH and 0.950 for ISTH). On the contrary, TCH diagnostic criteria perform better, with a sensitivity significantly higher than the ISTH scoring method when tested against the gold standard (P < .05). Fibrinogen is not a significant predictor of overt DIC in both models. Sequential testing of coagulation parameters is recommended for improved sensitivity when applying ISTH criteria to pediatric populations.
Keywords: Disseminated intravascular coagulation, Children, International Society on Thrombosis and Haemostasis (ISTH), Autopsy, DIC score
Overt disseminated intravascular coagulation (DIC) in children is a spectrum of manifestations of severe systemic activation of coagulation. Diagnosis of DIC is complicated because it includes a wide range of clinical presentation, including mild to excessive bleeding and systemic thromboembolic phenomenon, and is associated with multiorgan failure.1 The lack of a gold standard for laboratory diagnosis of overt DIC has added to the difficulty in identifying and clinically managing this disorder.
The International Society on Thrombosis and Haemostasis (ISTH) diagnostic scoring system for overt DIC has been widely used in intensive care units, and many outcome studies validating the ISTH diagnostic score against morbidity scores have been published (eg, logistic organ dysfunction, Acute Physiology and Chronic Health Evaluation, and Pediatric Risk of Mortality III).2–4 Although the common predisposing conditions for DIC are not the same in adults and children, the pathophysiology remains the same, with an overwhelmed hemostatic system that is unable to cope with continuous thrombin activation and the consumption of coagulation factors and platelets.
In pediatrics, however, there are still controversies regarding the varying manifestations of DIC in subsets of critically ill children, wide ranges of coagulation parameters in different age groups, and the choice of confirmatory laboratory tests for overt DIC.5 In our pediatric intensive care unit (PICU), the standard method of diagnosis is expert opinion based on criteria that include sequential testing of the components of the ISTH scoring system (ie, prothrombin time [PT], platelet count, fibrinogen, and D-dimer). Despite the fact that many PICUs in the United States routinely use the ISTH scoring system, there is a paucity of clinical research studies examining its utility in children.
In this article, we examine the predictive ability of the global coagulation tests to identify patients with overt DIC and also compare our Texas Children’s Hospital (TCH) criteria with the ISTH diagnostic algorithm. Furthermore, a small subset of patients (n = 24) provided a gold standard (ie, autopsy results) against which we compared the performance of the ISTH score and our hospital’s modified criteria.
Materials and Methods
Patients
Patients with 4 or more consecutive DIC panels during a single hospital visit from November 2005 to September 2008 were included in the study. Data were collected on pediatric patients of all ages with DIC-related conditions from the electronic laboratory and medical records after obtaining institutional review board approval from Baylor College of Medicine (Houston, TX) for the research study. Independent variables included age, sex, predisposing condition, and global coagulation assays such as PT, fibrinogen, platelet count, and D-dimer. DIC scores were calculated using the ISTH scoring system Table 1 for diagnosis of overt DIC. A score of 5 or greater was concluded to have a positive result. Similarly, TCH conclusion of DIC was attained using the criteria in Table 1. Autopsy results of patients who died of DIC (manifested by disseminated intravascular coagulation, DIC, or disseminated intravascular coagulopathy in the final anatomic diagnosis [FAD] and with micro-thrombi described in 1 or more organs) were extracted by retrospective review of the anatomic pathology database. In our hospital, DIC is included in the FAD if there are findings of coagulopathy (clinical or laboratory evidence of coagulopathy or hemorrhages/petechiae appreciated at autopsy) and micro-thrombi identified within routinely sampled organ systems. The cases were re-reviewed to confirm the presence of fibrin thrombi in the microvasculature of organs, most often the liver sinusoids, adrenal glands, or kidneys. Their last set of coagulation tests right before death was retrospectively collected from the clinical pathology database used for routine reporting of test results.
Table 1.
Comparing ISTH and TCH Criteria for DIC
| Coagulation Test and ISTH Criteria | Score | TCH Valuesa |
|---|---|---|
| Platelet count,/μL | ||
| >100,000 | 0 | Sequential measurement |
| 50,000–100,000 | 1 | |
| <50,000 | 2 | |
| Prolongation of PT, s | ||
| <3 | 0 | <2.6 |
| 3–6 | 1 | 2.6–5.6 |
| >6 | 2 | >5.6 |
| Fibrinogen, mg/dL | ||
| ≥100 | 0 | Sequential measurement |
| <100 | 1 | |
| D-dimer, μg/mL FEU | ||
| No increase | 0 | <1.5 |
| Moderate increase | 2 | 1.5–3.9 |
| Strong increase | 3 | ≥4 |
| Interpretation | ||
| Overt DIC | ≥5 | Overt DICb |
DIC, disseminated intravascular coagulation; FEU, fibrinogen equivalent unit; ISTH, International Society on Thrombosis and Haemostasis; PT, prothrombin time; TCH, Texas Children’s Hospital.
Normal values of PT at TCH are less than 15.2 seconds.
TCH does not have a scoring system, but coagulation assays (PT, platelet count, fibrinogen, and D-dimer) are sequentially evaluated by the transfusion medicine specialists along with the patient’s clinical condition before determining overt DIC.
Laboratory Methods
The laboratory coagulation assays for PT, fibrinogen, and D-dimer were performed on a STA-R analyzer (Diagnostica Stago, Parsippany, NJ) using commercially available reagents, and platelet count was measured on a Sysmex XE-2100 analyzer (Sysmex America, Lincolnshire, IL).
Statistical Analysis
Continuous variables that were normally distributed are expressed as mean ± SD. Two logistic regression models were built by including independent variables—namely, fibrinogen, PT, platelet, and D-dimer—to compare the TCH method of diagnosis with the ISTH scoring method. The binary outcome variable measured was the presence or absence of DIC, as defined by 2 different sets of criteria (ISTH and TCH). The predicted probabilities of each model were evaluated against the ISTH diagnosis of overt DIC or no DIC by using receiver operating characteristic (ROC) analysis. In this analysis, the power of the model’s predicted values to discriminate between positive and negative cases was derived by calculating the area under the curve (AUC). Next, stepwise logistic regression analysis was done to assess the ability of the independent variables, such as PT, D-dimer, platelet count, and fibrinogen, to predict overt DIC according to the ISTH and TCH criteria and also to identify the best set of predictors of DIC in both systems. In addition, sensitivity and specificity, which are statistical measurements of a binary classification test (presence or absence of DIC), were calculated according to their specific criteria and compared with the autopsy diagnosis of DIC, which is the global gold standard of diagnosis. All statistical tests were performed using SPSS version 19 (SPSS, Chicago, IL).
Results
A total of 2,136 DIC panels from 130 patients (57.7% male and 42.3% female), with a mean age of 6.9 years (range, 1 day to 18 years in males and females), were collected and evaluated. Analysis of these panels showed that TCH suspected 65% (1,399) of the panels to be positive for DIC, whereas the ISTH system suspected only 37% (794) of the same panels to be positive for DIC. The mean values of the coagulation parameters measured for patients classified as overt DIC and non-DIC by the 2 different ISTH and TCH criteria are listed in Table 2. There was a significant difference in the coagulation parameters between patients with and without a diagnosis of DIC.
Table 2.
Descriptive Characteristics of Patients With Overt DIC and Non-DIC Categorized by the TCH and ISTH Scoring System
| TCH, Mean ± SD
|
ISTH, Mean ± SD
|
|||
|---|---|---|---|---|
| Coagulation Test | Non-DIC (n = 724) | DIC (n = 1,316) | Non-DIC (n = 1,298) | DIC (n = 742) |
| PT, s | 15.2 ± 2.3 | 19.7 ± 6.2a | 16.2 ± 2.6 | 21.5 ± 7.5b |
| Fibrinogen, mg/dL | 446.8 ± 211.5 | 373.0 ± 208.9a | 434.4 ± 210.7 | 337.6 ± 202.1b |
| Platelet count, ×103/μL | 140 ± 130 | 96 ± 98a | 142 ± 124 | 57 ± 54b |
| D-dimer, μg/mL FEU | 4.29 ± 5.12 | 10.64 ± 7.05a | 5.85 ± 6.07 | 12.81 ± 6.62b |
DIC, disseminated intravascular coagulation; FEU, fibrinogen equivalent unit; ISTH, International Society on Thrombosis and Haemostasis; PT, prothrombin time; TCH, Texas Children’s Hospital.
P < .001 when compared with non-DIC (TCH).
P < .001 when compared with non-DIC (ISTH).
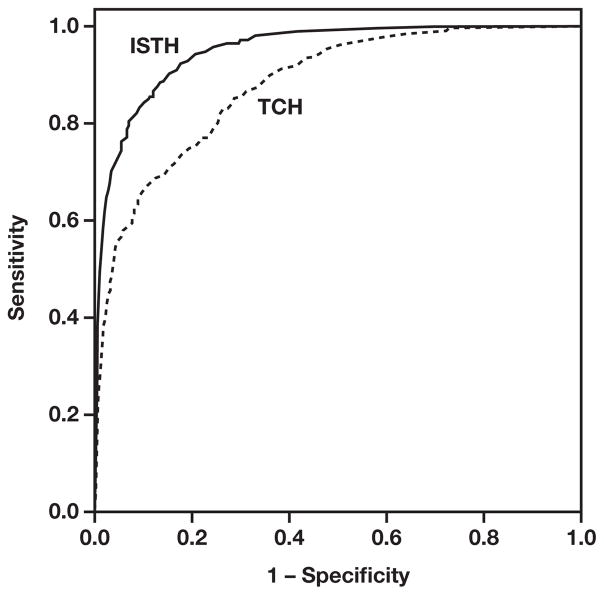
The ROC analysis evaluates the quality of both the ISTH and TCH algorithms to discriminate between positive and negative diagnosis of DIC, and the ROC curves Figure 1 are a plot of their predicted probabilities. Generally, the AUC for ROC plots greater than 0.8 is considered excellent. The numerical values of the AUC with the 95% confidence interval (CI) and standard error are given in Table 3. The multivariate TCH and ISTH models had an AUC of 0.88 and 0.95, respectively, which determines their ability to correctly classify DIC.
Figure 1.
Receiver operating characteristic plot of the sensitivity against 1 – specificity values associated with the International Society on Thrombosis and Haemostasis (ISTH) and Texas Children’s Hospital (TCH) predicted event probabilities.
Table 3.
Area Under the Curve as a Measure of Model Fit for the ISTH and TCH Regression Models Based on Independent Predictors (PT, Platelet Count, and D-Dimer)
| Predicted Probability | Area Under Curve | SE | P Value | 95% CI |
|---|---|---|---|---|
| ISTH | 0.950 | 0.005 | <.001 | 0.941–0.959 |
| TCH | 0.878 | 0.008 | <.001 | 0.863–0.893 |
CI, confidence interval; ISTH, International Society on Thrombosis and Haemostasis; PT, prothrombin time; SE, standard error; TCH, Texas Children’s Hospital.
Forward stepwise logistic regression analysis was performed to examine the impact of the coagulation variables on the diagnosis of DIC Table 4. PT (P < .001), D-dimer (P < .001), and platelet count (P < .001) were significant predictors in both models, and fibrinogen was excluded from the model (P = .53 for TCH and P = .62 for ISTH models). The result of the analysis also indicates that after controlling for PT and platelet count, an increase of D-dimer by 1 μg/mL is more likely to be associated with DIC (odds ratio [OR], 1.16; 95% CI, 1.13–1.18). Similarly, the odds of being diagnosed with DIC increases when there is an increase of PT by 1 second (OR, 1.66; 95% CI, 1.56–1.78).
Table 4.
Stepwise Logistic Regression Analysis for Predictors of DIC Using TCH and ISTH Criteriaa
| TCH Criteria
|
ISTH Criteria
|
|||||
|---|---|---|---|---|---|---|
| Predictor Variables | Adjusted OR | 95% CI | P Value | Adjusted OR | 95% CI | P Value |
| DDb | 1.16 | 1.13–1.18 | <.001 | 1.19 | 1.16–1.22 | <.001 |
| PTc | 1.66 | 1.56–1.78 | <.001 | 1.65 | 1.56–1.76 | <.001 |
| Plateletd | 0.99 | 0.99–0.99 | <.001 | 0.96 | 0.96–0.97 | <.001 |
CI, confidence interval; DIC, disseminated intravascular coagulation; ISTH, International Society on Thrombosis and Haemostasis; OR, odds ratio; TCH, Texas Children’s Hospital.
Fibrinogen was excluded from the model (P = .53 for TCH and P = .62 for ISTH model).
D-dimer (DD) entered during step 1 of the analysis.
Prothrombin time (PT) entered during step 2.
Platelet count entered during step 3.
The sensitivity and specificity, as well as the positive predictive value (PPV) and negative predictive value (NPV), of the TCH and ISTH criteria of diagnosis when compared with the autopsy results in 24 patients are tabulated in Table 5. The sensitivity of the TCH criteria is significantly higher than the ISTH scoring system, whereas the specificity of ISTH is significantly higher than that applied by TCH. As for PPV and NPV, both are comparable.
Table 5.
ISTH and TCH Diagnoses of Overt DIC vs Autopsy Diagnosis in Patients Who Died of DIC-Related Causes (n = 24)
| ISTH | TCH | P Value | |
|---|---|---|---|
| Sensitivity | 0.65 (0.39–0.85) | 0.82 (0.56–0.95) | <.05 |
| Specificity | 0.43 (0.12–0.80) | 0.29 (0.05–0.70) | <.05 |
| PPV | 0.73 (0.45–0.91) | 0.74 (0.49–0.90) | NS |
| NPV | 0.33 (0.09–0.69) | 0.40 (0.07–0.83) | NS |
DIC, disseminated intravascular coagulation; ISTH, International Society on Thrombosis and Haemostasis; NPV, negative predictive value; NS, nonsignificant; PPV, positive predictive value; TCH, Texas Children’s Hospital.
Discussion
The ISTH DIC scoring system is used globally to identify DIC in adult patients. However, only a few studies have validated the scoring method in children. Hence, we investigated its usefulness in the pediatric age group and compared it with our diagnostic criteria and a gold standard pathologic confirmation of DIC.4 The findings of our study suggest that both the diagnostic criteria (TCH and ISTH) are comparable in predicting DIC using the 4 global coagulation tests. Several other studies have confirmed similar results in the adult population. Evaluation of the Japanese Ministry of Health and Welfare (JMHW) criteria and ISTH criteria has reported a high concordance rate in patients with trauma and hemopoietic malignant carcinomas in adults.6 Similarly, a Korean study has also reported good agreement between the ISTH and Korean Society on Thrombosis and Hemostasis criteria in the diagnosis of overt DIC.7 Takemitsu et al8 reported that all 4 independent variables (platelet count, PT, fibrinogen, and D-dimer) were significantly important for the JMHW, the Japanese Association for Acute Medicine, and the ISTH criteria for diagnosis of overt DIC.
The results presented here indicate that PT, D-dimer, and platelet count are significant predictors in both models. However, fibrinogen does not seem have a significant impact on the prediction of DIC. Fibrinogen adds no further effect to the stepwise logistic regression risk factor modeling, and it is therefore excluded while developing a parsimonious model. This is consistent with the results of the study done by Bakhtiari and colleagues,9 who concluded that the ISTH DIC scoring system was very reliable in confirming or rejecting a diagnosis of DIC in critically ill patients and that inclusion or exclusion of fibrinogen levels did not affect the accuracy of the scoring system. Fibrinogen levels have been known to be insensitive indicators of DIC, primarily due to its increase during the acute-phase response.10 As such, fibrinogen increases above baseline during inflammatory conditions that commonly underlie the pathologic disease states leading to overt DIC. So, even though DIC may cause intense consumption of fibrinogen, levels do not typically fall below the normal range. However, sequential measurement of fibrinogen, as performed in TCH, is useful in detecting decreasing trends of fibrinogen and, therefore, is more predictive of overt DIC.
Similarly, the average platelet count in patients diagnosed with DIC by the TCH criteria is significantly greater than those diagnosed by the ISTH scoring system, as seen in Table 2. In our institution, serial values are evaluated to detect successive drops in the count, and DIC is diagnosed when a trend emerges. A single measurement reflecting moderate thrombocytopenia is found in many critically ill patients due to their underlying disease; hence, the platelet count at a single time point is not a sensitive predictor of overt DIC. In addition, patients with leukemia commonly have thrombocytopenia related to the disease condition or chemotherapy. Because those patients frequently receive platelet transfusions, an evaluation of platelet count must include a careful review of transfusion history. However, sequential measurements of platelet counts that show a decrease from normal or low-normal baseline values are indicative of DIC.11
ISTH DIC scores have long been known to predict mortality and morbidity in children.4 The extent to which these scores actually predict DIC, however, has not been demonstrated in the pediatric literature, primarily because of the lack of a gold standard diagnostic test for DIC in living patients. Hence, our comparison of both diagnostic algorithms against the autopsy gold standard has clinical implications that will influence the diagnosis and treatment of DIC in children. Our results indicate that comparing the presence or absence of DIC by the TCH criteria with the autopsy results displays a sensitivity and specificity of 0.82 and 0.29, respectively. When the analysis was done for the ISTH system, the cutoff for sensitivity and specificity was 0.65 and 0.43, respectively; similar results have been reported in adult studies.8 The higher specificity allows the ISTH system to identify only a typical overt DIC but not an evolving DIC. On the contrary, the TCH scoring system displays significantly higher sensitivity due to the inclusion of sequential testing that determines the rate of change in coagulation physiology, alerting the diagnostician to the possibility of an evolving overt DIC. PICU patients show minimal or mild derangement in their coagulation profiles due to the activation of the coagulation system by their disease process. It is therefore critical to delineate evolving DIC from other disease conditions. Thus, the TCH scoring system, with its high degree of sensitivity, is able to recognize a trend in the evolution from an early-phase DIC to overt DIC, an advantage in accurately capturing the pathobiochemical scenario. This is consistent with results of the study done by Wilde et al,12 who elucidated the association between coagulation parameters obtained before death and evidence of DIC in adult autopsies. They reported that coagulation tests reflective of a single time point—whether individual or combinations of coagulation tests—were not sensitive predictors of DIC. Their consequent recommendation of sequential testing to improve the sensitivity of diagnosis is supported by our findings. A recently published review article also points out the importance of dynamically assessing the coagulation physiology in patients to improve the diagnostic accuracy as well as early identification of progressive coagulopathy.13
Our study has some limitations. The values of the coagulation tests used for the second set of comparisons of the scoring systems with the autopsy diagnosis were closest to the time of death and autopsy; these may not reflect the changes to the hemostatic system in the early phase of nonovert DIC, when the diagnosis is most needed. However, the ISTH scoring system was designed to be used in identifying the progression of overt DIC and should not be applied in diagnosing early phases of nonovert DIC in children.2
In conclusion, we found that the TCH algorithm used in our PICU exhibits a higher sensitivity than the ISTH scoring system, which makes it a preferable algorithm in the pediatric population. Most important, a single time point analysis of the laboratory tests is not as good as trends with serial values and should not be relied upon to make a diagnosis of an evolving overt DIC. Modification of the ISTH algorithm with a requirement of including serial measurements of the global coagulation tests would increase the ability of the algorithm to diagnose overt DIC at an early phase.
References
- 1.Bick RL. Disseminated intravascular coagulation: a review of etiology, pathophysiology, diagnosis, and management: guidelines for care. Clin Appl Thromb Hemost. 2002;8:1–31. doi: 10.1177/107602960200800103. [DOI] [PubMed] [Google Scholar]
- 2.Taylor FB, Jr, Toh CH, Hoots WK, et al. Towards definition, clinical and laboratory criteria, and a scoring system for disseminated intravascular coagulation. Thromb Haemost. 2001;86:1327–1330. [PubMed] [Google Scholar]
- 3.Gando S, Saitoh D, Ogura H, et al. Disseminated intravascular coagulation (DIC) diagnosed based on the Japanese Association for Acute Medicine criteria is a dependent continuum to overt DIC in patients with sepsis. Thromb Res. 2009;123:715–718. doi: 10.1016/j.thromres.2008.07.006. [DOI] [PubMed] [Google Scholar]
- 4.Khemani RG, Bart RD, Alonzo TA, et al. Disseminated intravascular coagulation score is associated with mortality for children with shock. Intensive Care Med. 2009;35:327–333. doi: 10.1007/s00134-008-1280-8. [DOI] [PubMed] [Google Scholar]
- 5.Oren H, Cingoz I, Duman M, et al. Disseminated intravascular coagulation in pediatric patients: clinical and laboratory features and prognostic factors influencing the survival. Pediatr Hematol Oncol. 2005;22:679–688. doi: 10.1080/08880010500278749. [DOI] [PubMed] [Google Scholar]
- 6.Wada H, Gabazza EC, Asakura H, et al. Comparison of diagnostic criteria for disseminated intravascular coagulation (DIC): diagnostic criteria of the International Society of Thrombosis and Hemostasis and of the Japanese Ministry of Health and Welfare for overt DIC. Am J Hematol. 2003;74:17–22. doi: 10.1002/ajh.10377. [DOI] [PubMed] [Google Scholar]
- 7.Lee JH, Song JW, Song KS. Diagnosis of overt disseminated intravascular coagulation: a comparative study using criteria from the International Society versus the Korean Society on Thrombosis and Hemostasis. Yonsei Med J. 2007;48:595–600. doi: 10.3349/ymj.2007.48.4.595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Takemitsu T, Wada H, Hatada T, et al. Prospective evaluation of three different diagnostic criteria for disseminated intravascular coagulation. Thromb Haemost. 2011;105:40–44. doi: 10.1160/TH10-05-0293. [DOI] [PubMed] [Google Scholar]
- 9.Bakhtiari K, Meijers JC, de Jonge E, et al. Prospective validation of the International Society of Thrombosis and Haemostasis scoring system for disseminated intravascular coagulation. Crit Care Med. 2004;32:2416–2421. doi: 10.1097/01.ccm.0000147769.07699.e3. [DOI] [PubMed] [Google Scholar]
- 10.Levi M, Ten Cate H. Disseminated intravascular coagulation. N Engl J Med. 1999;341:586–592. doi: 10.1056/NEJM199908193410807. [DOI] [PubMed] [Google Scholar]
- 11.Levi M, Toh CH, Thachil J, et al. for the British Committee for Standards in Haematology. Guidelines for the diagnosis and management of disseminated intravascular coagulation. Br J Haematol. 2009;145:24–33. doi: 10.1111/j.1365-2141.2009.07600.x. [DOI] [PubMed] [Google Scholar]
- 12.Wilde JT, Roberts KM, Greaves M, et al. Association between necropsy evidence of disseminated intravascular coagulation and coagulation variables before death in patients in intensive care units. J Clin Pathol. 1988;41:138–142. doi: 10.1136/jcp.41.2.138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Levi M, Meijers JC. DIC: which laboratory tests are most useful? Blood Rev. 2011;25:33–37. doi: 10.1016/j.blre.2010.09.002. [DOI] [PubMed] [Google Scholar]