Abstract
Despite being the most prevalent form of child maltreatment, the correlates and consequences of neglect are poorly understood, particularly during early adulthood. The present multi-wave, longitudinal study sought to address this gap in this literature by examining physical and emotional neglect in emerging adults in a diverse community sample. 580 adolescents (AgeMean = 18.25; AgeSD = 0.59; 58.3% female; 31% Hispanic, 28.9% Caucasian; 26.2% African-American; 13.9% other) completed self-report measures for child maltreatment at baseline, and measures for depression, posttraumatic stress disorder, generalized anxiety disorder, and substance use every year for three years. For our analyses, we used both variable-centered (mixed-level modeling) and person-centered (latent profile analysis) analyses to best understand a) how physical and emotional neglect relate to other forms of maltreatment and b) to determine physical and emotional neglect’s unique impact on prospective mental health functioning. Our person-centered analyses revealed that a three-profile model provided the best solution for our data (“No Trauma,” “Abuse”, and “Neglect”). In longitudinal analyses, the “the neglect” group had significantly elevated scores compared to the “no trauma” group on all outcomes except alcohol use (p < .01). Results from our variable-centered analyses showed comparable findings between physical and emotional neglect, with higher scores corresponding to elevated symptoms of depression, PTSD, illicit substance use, and cigarette use over time (p < .01). In conclusion, our results suggest that early neglect-exposure poses a risk for the subsequent development of internalizing symptoms and substance use behaviors among emerging adults.
Keywords: Neglect, Maltreatment, Emerging Adulthood, Internalizing Symptoms, Substance Use
The Distal Consequences of Physical and Emotional Neglect in Emerging Adults: A Person-Centered, Multi-Wave, Longitudinal Study
Physical neglect (i.e., the failure to meet a child’s basic physical needs, such as food, clothing, shelter, personal hygiene, and medical care) and emotional neglect (i.e., not meeting the child’s developmental or emotional needs, including inadequate nurturance or affection; Proctor & Dubowitz, 2014) are the most prevalent forms of child maltreatment worldwide. Approximately one in five children will experience emotional and/or physical neglect by the age of 17 (Finkelhor, Turner, Shattuck, & Hamby, 2013; Stoltenborgh, Bakermans-Kranenburg, & van IJzendoorn, 2013). In 2014, of the 6.6 million children referred to child protective services (CPS) agencies in the United States, an overwhelming 75% involved allegations of neglect (U.S. Department of Health & Human Services, 2016). Equally troubling, while strategies focused on reducing childhood adversities attenuated the occurrence of most maltreatment subtypes over a five year span (e.g., sexual abuse and emotional abuse), rates for neglect remained stagnant (Finkelhor et al., 2010). In response, research has increasingly focused on neglect to better understand this adverse family environment (see Boyce & Maholmes, 2013). The goal for this collective research is to ultimately reduce the occurrence of neglect within at-risk families (e.g., Dubowitz, Feigelman, Lane, & Kim, 2009) and promote the healthy development of neglect-exposed individuals (e.g., Swenson, Schaffer, Heggeler, Fadowski, & Mayhew, 2010).
The present multi-wave, longitudinal study sought to advance our understanding of the psychological consequences of physical and emotional neglect in three important ways. First, we focused on neglect’s potential impact during the transition from late adolescence into early adulthood (i.e., ages 18–25), a critical period with regard to interpersonal and achievement domains (Arnett, 2007, 2014) and a sensitive period to the development of childhood trauma-related distress (Khrapatina & Berman, 2010; Thompson et al., 2015). Second, we examined the prospective impact of physical and emotional neglect in a large, diverse community sample. Past studies have focused on CPS (e.g., Cicchetti & Rogosch, 2002; Widom, 2013) or clinical (e.g., Adams et al., 2016) samples leading to a potential “tip of the iceberg” problem where only the most severe cases of neglect are being studied. Examining our hypotheses within a community sample can illuminate the continuum of neglect (Proctor & Dubowitz, 2014; Stoltenberg et al., 2013) and identify potential sex and race differences with regard to neglect (Chaffin, Kelleher, & Hollenberg, 1996). Finally, we used a parallel analytic approach where both variable-centered and person-centered analyses were used to examine physical and emotional neglect (Petrenko, Friend, Garrido, Taussig, & Culhane, 2012). This analytic approach, coupled with our longitudinal design, can provide foundational knowledge concerning childhood neglect’s impact on psychological distress during the challenging transition into adulthood.
Neglect and Mental Health in Emerging Adulthood
Neglect is a potent risk factor for the development of psychological distress, especially internalizing disorders (Norman et al., 2012). Early exposure to childhood neglect is closely associated with the proximal development of depression and anxiety in youth (Hildyard & Wolfe, 2002), and distal internalizing consequences in adults (Norman et al., 2012; Spinhoven et al., 2010; Widom, DuMont, & Czaja, 2007). Despite being unaffiliated with a Criterion A event by definition, associations between childhood neglect-exposure and posttraumatic stress disorder (PTSD) have also been identified in both youth and adult populations (Milot, St-laurent, Louise, & Provost, 2010; Nikulina, Widom, & Czaja, 2011). While there is little debate concerning neglect’s role as a potent risk factor for internalizing distress, it is less clear whether certain subtypes of neglect may be particularly detrimental (Mersky & Topitzes, 2010). Studies typically focus on either physical (e.g., Widom et al., 2007) or emotional neglect (e.g., Spinhoven et al., 2010; Young, Lennie, & Minnis, 2011), making specificity analyses challenging. A collection of research suggests that physical neglect may confer greater risk for internalizing symptoms in childhood (Hildyard & Wolfe, 2002; Kim & Cicchetti, 2006), while findings for both emotional (Spinhoven et al., 2010) and physical (Widom et al., 2007) neglect show deleterious outcomes in adults. Interestingly, emotional neglect may uniquely confer greater risk for internalizing symptoms in clinical (van Vugt, Lanctot, Paquette, Collin-Vezina, & Lemieux, 2014) and community (Campbell-Sills, Cohan, & Stein, 2006) samples of emerging adults. Prospectively examining the relation between physical/emotional neglect and internalizing symptoms in a large community sample can help determine whether emotional, as opposed to physical, neglect exerts a greater influence on internalizing distress in early adulthood.
In contrast to the literature on internalizing distress, the association with neglect and externalizing behavior, particularly substance use, is less clear. Some studies show that neglect contributes to increased drug and alcohol use across ages (e.g., adolescents and adults) and samples (e.g., clinical and community; Alvarez-Alonso et al., 2016; Mills, Alati, Strathearn, & Najman, 2013; Rosenkranz, Muller, & Henderson, 2012; Schilling, Aseltine, & Gore, 2007; White & Widom, 2008). Meanwhile, other studies have failed to replicate these associations, showing that while physical and sexual abuse predicted alcohol and illicit substance use, patterns of physical/emotional neglect do not significantly relate to problematic substance use patterns in adolescents (Cheng & Lo, 2010) or adults (Galaif, Stein, Newcomb, & Bernstein, 2001). Inconsistent findings concerning neglect’s association with substance use may be due to a reliance on cross-sectional data, inconsistent inclusion/analytic treatment of other maltreatment subtypes, and potential demographic differences relevant to neglect-exposure.
Demographic Considerations
Early adulthood represents a critical period for identity development and long-term stability in interpersonal and career functioning (Arnett 2007, 2014). Exposure to physical and emotional neglect in childhood can lead to biological, cognitive, and interpersonal deficits in childhood and early adolescence which lay the foundation for psychological distress in early adulthood (Hildyard & Wolfe, 2002; Kazemian, Widom, & Farrington, 2011; Sheridan & McLaughlin, 2014) To date, however, the majority of maltreatment, let alone neglect research, has ignored the developmental period between adolescence and adulthood leaving it unclear what the specific relation between neglect and psychological functioning is during this developmental stage (Schulenberg, Sameroff, & Cicchetti, 2004; Toth & Cicchetti, 2013). Due to the complex relation between maltreatment experiences and other risk and protective factors, it is reasonable to expect that distinct developmental stages may forecast specific manifestations of resilience and distress as one copes with developmentally-salient challenges across the lifespan (Cicchetti & Toth, 1995; Mersky & Topitzes, 2010).
While examining neglect’s role within early adulthood, it is also important to consider potential differences with regard to sex and race. To date, some research has found males to be at increased risk for neglect-exposure (Hines, Kantor, & Holt, 2006), while other research posits equivalent exposure rates between males and females (Finkelhor et al., 2013; Stoltenborgh et al., 2013). Other findings show neglect-exposed females tend to experience elevated levels of internalizing distress (Wolfe, Scott, Wekerle, & Pittman, 2001) and substance use problems (Wekerle, Leung, Goldstein, Thornton, & Tonmyr, 2009; White & Widom, 2008; Widom, Marmorstein, & White, 2006; Widom et al., 2007; see Schilling et al., 2007 for an exception) compared to their male counterparts. As for racial differences, CPS data suggests that African-Americans may be at increased risk for experiencing physical/emotional neglect (Mennen et al., 2010), while Latino youth may be less likely to experience neglect (Mennen et al., 2010). This finding illustrates that Latino youth may be protected against neglect through cultural processes (e.g., familialism, religiosity, social support; Putnam-Hornstein, Needell, King, Johnson-Motoyama, 2013), or that Latino youth are less likely to come in contact with CPS providers (Borjas, 2011; Putnam-Hornstein et al., 2013). Finally, in CPS-samples, neglect-exposed African-Americans are at heightened risk for internalizing distress, while Latinos were more vulnerable to substance use outcomes (Widom, Czaja, Wilson, Allwood, & Chauhan, 2013). It is unknown whether these provocative demographic differences replicate within non-CPS samples.
Variable vs. Person-Centered Approaches in Maltreatment
Examining neglect in isolation can mask important differences among youth who experience neglect within the context of other maltreatment subtypes (Adams et al., 2016; Kazdin, 2011). As polyvictimization (i.e., experiencing multiple childhood adversities) is the norm rather than the exception (Finkelhor et al., 2013), it is recommended to include other potential maltreatment experiences when investigating a specific trauma experience (Ford, Elhai, Connor, & Frueh, 2010; Pears, Kim, & Fisher, 2008). Variable-centered approaches, in which the aggregate or interactive effects of experiencing multiple forms of maltreatment are examined, have shown that neglect-exposure is especially detrimental within the context of emotional (Mills et al., 2013) and physical abuse (Ney, Fung, & Wickett, 1994). However, due to issues of multicollinearity (Charak & Koot, 2015), and theoretical limitations of additive or interactive variable-centered approaches (Cohen et al., 2015), a person-centered approach may provide a more coherent examination of different maltreatment experiences. These approaches, ideally latent profile/class analyses (LPA; Ford et al., 2010), are able to empirically identify maltreatment experiences that tend to co-occur in subpopulations. By using both a person-centered and variable-centered approach, physical and emotional neglect’s link with other maltreatment types and prospective mental health impact can be clarified (Petrenko et al., 2012).
Despite the popularity of LPAs in recent years, few inferences can be made about physical and emotional neglect. Neither Ford and colleagues (2010) nor Berzenski and Yates (2011), in the two largest LPA examinations of maltreatment subtypes in community samples (4,836 adolescents and 2,637 emerging adults respectively), included neglect-exposure. Pears and colleagues (2008) and Petrenko and colleagues (2012) examined physical and supervisory neglect with a CPS-involved sample of children, along with a broad emotional maltreatment (emotional abuse and emotional neglect) category. Both identified a 4-class solution, with Pears and colleagues (2008) identifying neglect co-occurring with other abuse subtypes, and Petrenko and colleagues (2012) identifying both neglect-only, and neglect-abuse subtypes. To date, only two studies have examined physical and emotional neglect using an LPA approach. In a sample with a clinical/CPS-affiliated sample of adolescents, Hazen and colleagues (2009) identified a 3-class solution: Low maltreatment, all maltreatment subtypes except sexual abuse, and all maltreatment subtypes. Meanwhile, Charak and Koot (2015) identified a 4-class solution within a community sample of Indian adolescents: Low maltreatment, all abuse subtypes and physical neglect, emotional and physical neglect, and an abuse only profile. The current study seeks to build off of these collective findings by investigating the presence of neglect subtypes within North American emerging adults, and the psychological outcomes for this subpopulation.
The Present Study
The present study examined maltreatment experiences as a predictor of symptoms of depression, anxiety, PTSD, and substance use (i.e., alcohol, illicit drugs, cigarettes) over the course of three years. Based on past research with community samples (Berzenski & Yates, 2011; Charak & Koot, 2015; Ford et al., 2010), we expected to identify anywhere between 2–6 maltreatment profiles, with at least one being defined by neglect experiences in the absence of abuse. We hypothesized that African-Americans would be overrepresented in neglect profiles, while Latino youth would be underrepresented (Mennen et al., 2010). As far as prospective outcomes, based on past research with emerging adults we suspected that emotional neglect, would confer greater risk for internalizing symptoms (Campbell-Sills et al., 2006; van Vugt et al., 2014), while physical and emotional neglect would both confer risk for substance use behavior (Widom et al., 2006; Widom, 2013). Finally, we hypothesized that neglect’s influence on psychological outcomes would be exacerbated for females (Wolfe et al., 2001; Wekerle et al., 2009; Widom et al., 2006; Widom et al., 2007), and exploratory analyses tested whether neglect-exposure and psychological distress’s relation varied as a function of race.
Methods
Study Sample
The current study uses data from Waves 4 (spring 2013), 5 (spring 2014) and 6 (spring 2015) of (The Anonymous), an ongoing longitudinal study of adolescent risk behaviors. 1,042 freshman and sophomore high school students were recruited from seven Houston-area public schools in spring 2010 (Wave 1) and followed annually. At Wave 4, a subset of 580 students (58.3% female; AgeMean = 18.25; AgeSD = 0.59) completed self-report measures on childhood maltreatment exposure and various mental health indices. Students in their original schools at Wave 4 (2013) completed these inventories via paper-pencil survey at school. Students no longer at their original school (dropped out, graduated, changed schools), including all participants at Waves 5 and 6 completed surveys online. Of the 580 students who completed the baseline survey (Wave 4), 446 completed Wave 5 (77% of Wave 4 participants), and 476 completed Wave 6 (107% of Wave 5 participants). The baseline sample identified as 31% Hispanic (N = 180), 28.9% Caucasian (N = 168), 26.2% African-American (N = 152), 4.3% Asian (N =25), and 9.6% as bi-racial or other (N = 56). 45.5% of participants reported living with both parents, while 24% lived only with their mother. Approximately 25% of youth had either their mother (26.4%) or father (22.1%) finish college, while 14.9% of participants lived in households where both parents completed college. Incentives for participating in the study ranged from $20 - $30 gift cards for each wave of data collection. Written parental consent and student assent were obtained prior to administering surveys. The study was approved by the IRB at last author’s institution.
Measures
Childhood trauma
Child abuse and neglect was measured with the Childhood Trauma Questionnaire- Short Form (CTQ-SF; Bernstein et al., 2003). The CTQ-SF is a 28-item measure with items asking participants to rate their childhood experiences on a scale of 1 (never true) to 5 (very often true). The measure demonstrated good criterion-related validity in adolescents (Bernstein et al., 2003). Reliability for emotional neglect (α = .88), physical neglect (α = .59), sexual abuse (α = .94), physical abuse (α = .72), and emotional abuse (α = .78) was consistent with past research (Bernstein et al., 2003).
Depression
Depression symptoms were measured with the Center for Epidemiologic Studies Depression Scale (CESD)-10 (Bradley, Bagnell, & Brannen, 2010). The 10-item measure asked participants to indicate on a scale of 0 (rarely or none of the time) to 3 (all of the time) how often they experience each of the ten symptoms. A score of 10 or higher indicates clinically significant depressive symptoms. CES-10 has good reliability in adolescent populations (α = .85; Bradley et al., 2010). In the current study, reliability for the measure was adequate across all three waves (α = .77, 79, .79).
Posttraumatic Stress Disorder
PTSD was measured with the 4-item Primary Care- PTSD (PC-PTSD) questionnaire (Prins et al., 2003). The four items have a yes/no response format. The PC-PTSD has good test-retest reliability and had good operating characteristics when compared to PTSD diagnosis in a VA population (Prins et al., 2003). In the present study, internal reliability was α = .81, .81, and .82 across the three waves.
Anxiety
Anxiety symptoms were measured with the Generalized Anxiety Disorder subscale (GAD) of the Screen for Child Anxiety Related Emotional Disorders (SCARED; Birmaher et al., 1999). The GAD is a 9-item measure with responses ranging from 0 (almost never) to 2 (often) and demonstrated good internal consistency in a clinical sample of adolescents (Birmaher et al., 1999). The measure exhibited good reliability across the three years in the present study (α = .88, .91, .92).
Substance use
Substance use measures were adapted from Monitoring the Futures (Johnston et al., 2010), and asked participants to indicate their past year alcohol, cigarette, and illicit substance (i.e. marijuana, cocaine, amphetamines, inhalants, ecstasy, and prescription medication not prescribed by a health professional) use. Participants indicated yes/no to all items. Substance use counting variables were computed for all three waves.
Covariates
Other covariates included age, race, and sex from baseline (Wave 1).
Data Analytic Approach
The present study’s analyses were conducted in two phases. The first phase consisted of a latent profile approach (LPA) to examine maltreatment patterns related to physical and emotional neglect. LPA is a “top down” approach which requires the investigator to specify the number of hypothesized profiles in the data. For each participant, the probability of being in a given profile is estimated, and classification into one of the profiles is determined by that individual’s highest profile probability. Based on past research, we hypothesized that anywhere between 2- and 6-profile solutions would most accurately describe the different maltreatment subtypes within our sample (Charak & Koot, 2015; Hazen et al., 2009; Ford et al., 2010). To determine the superior profile solution, an iterative approach starting at 2 profiles and ending at 6 profiles was used. Model fit was evaluated using the Lo-Mendell-Rubin Adjusted Likelihood Test (LMRT) and Vuong-LMRT (V-LMRT), which indicate the number of profiles that best fit the data. The LMRT and V-LMRT statistically compare the fit of a target model to a model that specifies one fewer profiles. A non-significant LMRT/V-LMRT test suggests that the additional profile did not significantly improve the fit of the model. Information based indices (i.e., AIC, BIC) as well as the entropy criterion were also inspected for each model to determine the best fit. Chi-square analyses were used to examine any race and sex differences with regard to profile membership.
In the second phase, a multilevel modeling approach was utilized to examine the prospective impact of neglect during late adolescence. Both variable-centered (i.e., scores on emotional and physical neglect subscales) and person-centered (i.e., LPA profiles) neglect variables were independently assessed. A random intercept was entered for each model to account for individual differences in baseline symptom scores. Time was included as a fixed effect to determine if the relation between neglect and psychological distress increased over time (i.e., a significant interaction between time and the IV) or if elevated symptoms at baseline were maintained over time (i.e., significant main effect for the IV with time as a covariate). When the latter was true, time was re-centered as 0 at each time point to provide a more stringent test of our hypotheses. Sex and race were retained as covariates for all analyses, and two- and three-way interactions were formed to examine if our findings varied as a function of sex and/or race. Given the large sample size, alpha was set at p ≤ .01 and effect sizes were calculated for each significant result to provide a clinical context for our findings. For all significant findings concerning internalizing and substance use outcomes, co-occurring symptoms were controlled for to test whether neglect exerted a unique influence for that specific symptom pattern (e.g., for PTSD and substance use, depression was entered as a covariate).
Results
Preliminary Analyses
Means and standard deviations for all study variables at baseline are presented in Table 1. Table 2 includes bivariate correlations between baseline measures in our study.
Table 1.
Means and Standard Deviations for maltreatment experiences and psychological symptoms at baseline
| N | M (SD) | |
|---|---|---|
| Physical Neglect | 580 | 7.54 (2.91) |
| Emotional Neglect | 580 | 10.26 (4.77) |
| Emotional Abuse | 579 | 7.81 (3.59) |
| Sexual Abuse | 580 | 6.11 (3.48) |
| Physical Abuse | 580 | 6.93 (2.72) |
| Depression | 580 | 18.39 (5.27) |
| PTSD | 576 | 1.00 (1.37) |
| GAD | 581 | 8.34 (4.80) |
| Alcohol Use | 581 | .70 (.46) |
| Illicit Drug Use | 575 | .68 (1.06) |
| Cigarette Use | 579 | .24 (.43) |
Note: Physical Neglect = Childhood Trauma Questionnaire-Short Form (CTQ-SF)-Physical Neglect Subscale; Emotional Neglect = Childhood Trauma Questionnaire-Short Form (CTQ-SF)-Emotional Neglect Subscale; Emotional Abuse = Childhood Trauma Questionnaire-Short Form (CTQ-SF)-Emotional Abuse Subscale; Sexual Abuse = Childhood Trauma Questionnaire-Short Form (CTQ-SF)-Sexual Abuse Subscale; Physical Abuse = Childhood Trauma Questionnaire-Short Form (CTQ-SF)-Physical Abuse Subscale. Depression = Center for Epidemiological Studies (CESD)-10; PTSD = Primary Care-Posttraumatic Stress Disorder (PC-PSTD); GAD = Screen for Child Anxiety Related Emotional Disorders (SCARED)-Generalized Anxiety Disorder Subscale; Alcohol Use = Monitoring The Future-Alcohol Subscale; Illicit Drug Use = Monitoring The Future-Illicit Drug Use Subscale; Cigarette Use = Monitoring The Future-Cigarette Subscale.
Table 2.
Bivariate correlations between symptoms, maltreatment exposure, and sex.
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Physical Neglect | |||||||||||
| 2. Emotional Neglect | .67** | ||||||||||
| 3. Emotional Abuse | .45** | .54** | |||||||||
| 4. Sexual Abuse | .22** | .18** | .49** | ||||||||
| 5. Physical Abuse | .32** | .33** | .57** | .33** | |||||||
| 6. Depression | .26** | .38** | .44** | .17** | .23** | ||||||
| 7. PTSD | .16** | .21** | .31** | .18** | .17** | .47** | |||||
| 8. GAD | −.01 | .14** | .27** | .09** | .11** | .46** | .29** | ||||
| 9. Alcohol Use | .07 | .05 | .10* | .02 | .02 | .10* | .10* | .04 | |||
| 10. Illicit Drug Use | .16** | .13** | .13** | .07 | .10* | .09* | .10* | .04 | .30** | ||
| 11. Cigarette Use | .16** | .19** | .21** | .06 | .16** | .18** | .17** | .07 | .28** | .40** | |
| 12. Sex | .10** | .02 | −.12** | −.13** | −.02 | −.13** | −.10** | −.22** | .05 | .18** | .13** |
Note: Physical Neglect = Childhood Trauma Questionnaire-Short Form (CTQ-SF)-Physical Neglect Subscale; Emotional Neglect = Childhood Trauma Questionnaire-Short Form (CTQ-SF)-Emotional Neglect Subscale; Emotional Abuse = Childhood Trauma Questionnaire-Short Form (CTQ-SF)-Emotional Abuse Subscale; Sexual Abuse = Childhood Trauma Questionnaire-Short Form (CTQ-SF)-Sexual Abuse Subscale; Physical Abuse = Childhood Trauma Questionnaire-Short Form (CTQ-SF)-Physical Abuse Subscale. Depression = Center for Epidemiological Studies (CESD)-10; PTSD = Primary Care-Posttraumatic Stress Disorder (PC-PSTD); GAD = Screen for Child Anxiety Related Emotional Disorders (SCARED)-Generalized Anxiety Disorder Subscale; Alcohol Use = Monitoring The Future-Alcohol Subscale; Illicit Drug Use = Monitoring The Future-Illicit Drug Use Subscale; Cigarette Use = Monitoring The Future-Cigarette Subscale; Sex (Female = 0; Male =1).
p < .01;
p < .05.
Person-Centered Analysis
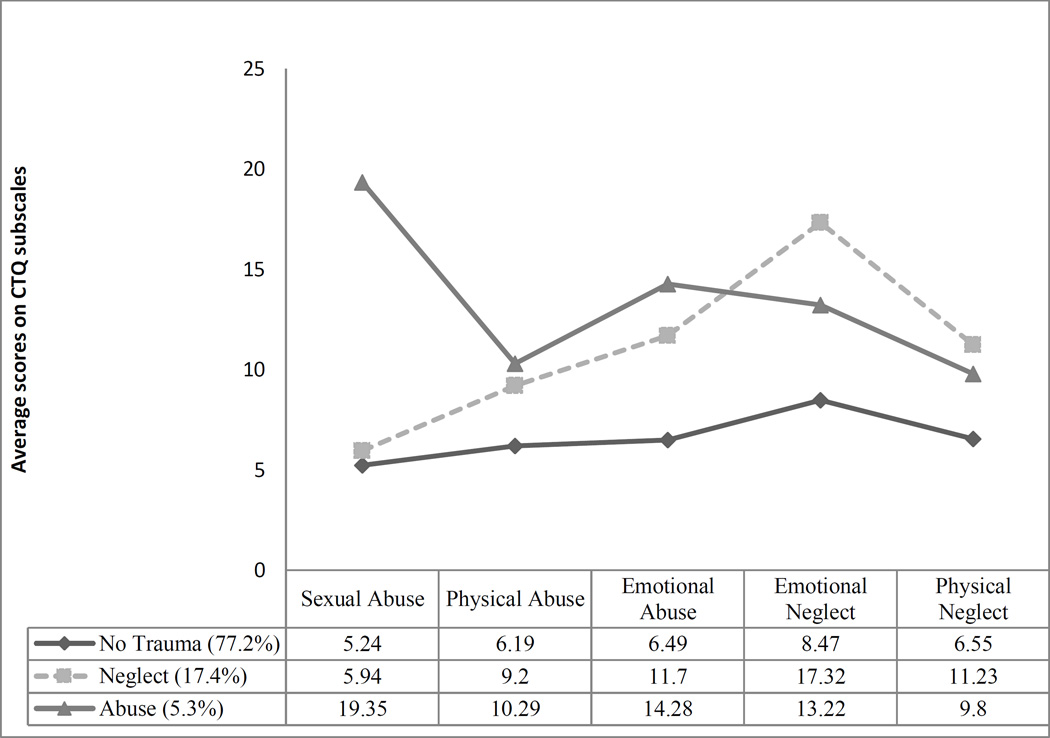
Table 3 includes the summary of the potential profile models for our maltreatment variables. Fit indices collectively indicate that the three-profile model provided the best solution for our data. Differences among the 5 maltreatment indicators are displayed in Figure 1. Post-hoc analyses suggest that the three subtypes significantly differ on each maltreatment subtype. Profile 1 (77.2%), defined by minimal endorsement of trauma types was labeled the “No Trauma” Group. Profile 2 was characterized by elevated physical and emotional neglect was labeled the “Neglect” group (17.4%) and Profile 3 was defined by the highest rates of sexual abuse, physical abuse, and emotional abuse and labeled the “Abuse” group (5.3%). With regard to demographic differences, chi-square analyses revealed significant sex (X2(2) = 6.65, p < .05) and racial (X2(8) 24.85 = 6.65, p < .01) differences across subtypes. Specifically, females and African-Americans were disproportionately more likely to be represented in the “abuse” subtype, while Hispanics were less likely to be represented in the “neglect” subtype.
Table 3.
Comparisons between the different person-centered solutions
| Model | AIC | BIC | Entropy | LMRT | VLMRT |
|---|---|---|---|---|---|
| 2-Profile | 14542.15 | 14611.96 | .94 | 835.70** | −7863.87** |
| 3-Profile | 13871.93 | 13967.1 | .94 | 591.45** | −7217.44** |
| 4-Profile | 13706.19 | 13828.36 | .91 | 173.21 | −6913.97 |
| 5-Profile | 13628.86 | 13777.20 | .92 | −122.64 | −6717.50 |
| 6-Profile | 13053.03 | 13227.55 | .94 | 147.52 | −6562.21 |
Note: AIC = Akaike information criterion; BIC = Bayesian information criterion; LMRT = Lo–Mendell–Rubin likelihood ratio test; VLMRT = Vuong-Lo-Mendell-Rubin likelihood ratio test.
p < .01.
The null hypotheses for the LMRT and VLMRT significance values indicate that a solution with the given number of classes provides the same fit to the data as a solution with one less class (i.e., adding an additional profile does not improve the model fit).
Figure 1. Estimated probabilities of exposure to each childhood maltreatment subtype.
Note: Maltreatment subtypes measured by Childhood Trauma Questionnaire (CTQ)-Short Form; Percentages represent the proportion of our sample within each profile. Scores on the Y-axis and within the table represent average scores for specific maltreatment subtype for each profile.
Longitudinal Analyses
Next, we utilized our MLM models to test how childhood experiences in neglect corresponded to prospective outcomes. We began by using our variable-centered approach and testing whether any of our clinical outcomes varied as a function of sex and/or race. The only significant interaction was between sex and emotional neglect for forecasting GAD symptoms. Specifically, girls who experienced elevated levels of emotional neglect were more likely to experience anxiety symptoms (t(580) = 5.11, p <.01). Main effect analyses were conducted with regard to the rest of the clinical outcomes. Findings for these independent MLM models can be found in Table 4. Of note, both physical and emotional neglect positively predicted symptoms of depression, PTSD, illicit substance use and cigarette smoking. Effect sizes were slightly elevated for emotional neglect compared to physical neglect for forecasting internalizing symptoms, while findings were comparable between neglect subtypes for substance use outcomes. Findings across mental health outcomes did not vary as a function of time. The pattern of findings was identical when the time point was reentered at 0 for subsequent time points. Finally, the pattern of findings remained similar when controlling for co-occurring symptoms (e.g., including PTSD as a covariate when examining depression outcomes; including cigarette use as a covariate when examining illicit substance use outcomes).
Table 4.
Summary of mixed-level model outcomes for variable-centered approach
| B | SE | t | df | Reffect | |
|---|---|---|---|---|---|
| Emotional Neglect | |||||
| Depression | .41 | .04 | 10.01** | 636 | .37 łł |
| PTSD | .06 | .01 | 5.42** | 725 | .20 ł |
| GAD | .14 | .04 | 3.42** | 689 | .13 ł |
| Illicit Drug Use | .03 | .01 | 3.68** | 746 | .13 ł |
| Alcohol | .01 | .00 | 1.72 | 786 | .06 |
| Cigarettes | .02 | .00 | 4.83** | 723 | .18 ł |
| Physical Neglect | |||||
| Depression | .47 | .07 | 6.61** | 635 | .25 ł |
| PTSD | .08 | .02 | 4.00** | 720 | .15 ł |
| GAD | .01 | .07 | .19 | 688 | .01 |
| Illicit Drug Use | .06 | .01 | 4.23** | 745 | .15 ł |
| Alcohol | .01 | .01 | 1.50 | 779 | .05 |
| Cigarettes | .02 | .01 | 3.55** | 714 | .13ł |
Note: Emotional Neglect = Childhood Trauma Questionnaire-Short Form (CTQ-SF)-Emotional Neglect Subscale; Depression = Center for Epidemiological Studies (CESD)-10; PTSD = Primary Care-Posttraumatic Stress Disorder (PC-PSTD); GAD = Screen for Child Anxiety Related Emotional Disorders (SCARED)-Generalized Anxiety Disorder Subscale; Illicit Drug Use = Monitoring The Future-Illicit Drug Use Subscale; Alcohol = Monitoring The Future-Alcohol Subscale; Cigarettes = Monitoring The Future-Cigarette Subscale.
p< .01;
Small effect size.
Medium effect size.
Prospective outcomes were run for the maltreatment subtypes identified using LPA. No significant three-way or two-way interactions emerged (p > .10). As for depressive symptoms, we identified significant differences between the profiles (t(576) = 5.50, p < .001, reffect = .22), with the neglect profile exhibiting elevated levels of depression compared to the non-trauma profile (p =.006) and similar levels compared to the abuse profile (p = .67). Similar patterns were found for the PTSD (t(570) = 4.33, p < .001, reffect = .18), GAD (t(580) = 2.09, p < .001, reffect = .09), illicit substance use ((t(552) = 2.99, p < .001, reffect = .13), and cigarette use (t(564) = 3.26, p < .001, reffect = .14) with the neglect profile experiencing elevated levels compared to the non-trauma profile but similar levels to the abuse profile.1 No significant differences emerged for alcohol use (p > .10).2 As with our variable-centered analyses, findings were significant while including comorbid symptoms as a covariate, symptoms for adolescents in the neglect profile did not increase/decrease over time, and baseline differences remained significant throughout the course of the study.
Discussion
As the “neglect of neglect” (Worlock & Horowitz, 1984) among researchers begins to fade, the unique and deleterious consequences of being exposed to this maltreatment subtype are becoming clear (Boyce & Maholmes, 2013; Norman et al., 2012). Our study demonstrated that in a large community sample, nearly one in five individuals endorsed growing up in a family environment characterized by caregiver deprivation without abuse. Across variable-centered and person-centered approaches, results suggested that emerging adults exposed to physical and emotional neglect as children were at elevated risk for internalizing distress and substance use behavior during this developmental period. Below we discuss the implications of these findings.
A recent meta-analysis posited that CPS statistics underestimate the prevalence of neglect worldwide. Relying on self-report, as opposed to informant data, Stoltenborgh et al. (2013) found that 16.3% of youth reported coming from families characterized by emotional neglect, while 18.4% of youth described physical neglect-exposure at a young age. The remarkably close number of emerging adults categorized within our “neglect” profile (17.4%) provides validity to our person-centered solutions. Person-centered assessments including neglect have been largely absent in the literature (Berzenski & Yates, 2011; Ford et al., 2010). In CPS samples of children and adolescents (Hazen et al., 2009; Pears et al., 2008; Petrenko et al., 2012), findings suggested that neglect was usually comorbid with other abuse presentations. However, in the one person-centered approach that investigated physical and emotional neglect in a community sample, Charak and Koot (2015) identified a “neglect only” profile. The identification of distinct neglect and abuse profiles, while somewhat simplistic, is consistent with other recent conceptualizations within the trauma literature along “deprivation” and “threat” (Sheridan & McLaughlin, 2014). Our results support the need to distinguish neglect experiences from other chronic, maladaptive family processes such as emotional abuse, in order to best characterize individuals exposed to chronic patterns of interpersonal deprivation.
Disparate prevalence estimates and polyvictimization profiles between CPS and community studies illustrate the importance of examining neglect-exposure in both contexts. Despite being the most common form of maltreatment reported to CPS, it is rarely reported in the absence of other maltreatment subtypes (Mennen et al., 2010; Sedlak et al., 2010). The most obvious explanation for this pattern is that abuse is defined as the commission of a behavior while neglect is characterized by the omission of caregiver behaviors, making it more difficult to identify (Proctor & Dubowtiz, 2014). Within this explanation, the act of physical and emotional neglect may be similar, however, CPS-samples generally involve youth in which the neglect was identified secondary to a presenting abuse allegation. On the other hand, there may be more fundamental differences between patterns of neglect. Neglect within the CPS context may represent a more severe form of physical and neglect behaviors, which once reaching a certain threshold corresponds to different polyvictimization profiles (Saunders & Adams, 2014). Alternatively, documented neglect within a CPS sample uses a “parent-focused” definition, in which the parent is at specific fault for youth not receiving their basic needs. A “child-focused” definition of neglect, in which youth report not experiencing basic needs from caregivers for any number of reasons (Proctor & Dubowitz, 2014) may be more representative self-reported neglect-exposure within community samples. As poverty does not equate to physical neglect (Nikulina et al., 2011), and low parental social support is not the same as emotional neglect (Cohen et al., 2015), examining neglect both within community and CPS samples can provide incremental knowledge on the heterogeneity of this maltreatment subtype.
Across almost all psychological outcomes, physical and emotional neglect forecasted deleterious symptom patterns in emerging adults. Consistent with past research (Hildyard & Wolfe, 2002; Norman et al., 2012), we found that physical and emotional neglect corresponded to elevated levels of depression and PTSD. Higher effect sizes for emotional, as opposed to physical neglect, for internalizing outcomes was consistent with past research focused on neglect’s impact during early adulthood (Campbell-Sills et al., 2006; van Vugt et al., 2014); however, the relatively similar pattern of findings between neglect subtypes, and the results of the person-centered analyses, raises questions concerning the incremental significance of distinguishing between neglect subtypes from a developmental psychopathology perspective. In other words, while identifying neglect subtypes provides clarity to the definition of neglect (Proctor & Dubowitz, 2014), the value of these distinctions may be reserved for descriptive, as opposed to inferential purposes. Continuing to test whether meaningful maltreatment and mental health differences exist between neglect subtypes can help determine whether inferences from studies that test a variety of neglect subtypes (e.g., supervisory neglect; Manly, Kim, Rogosch, & Cicchetti, 2001) can be applied to youth exposed to neglect-environments more broadly.
Findings concerning substance use were mixed, as across analyses neglect-exposure was a risk factor for illicit substance use and cigarette smoking, but not alcohol use. Neglect’s relation with illicit substance use and cigarette smoking does not seem to merely be a functioning of coping with internalizing distress (Goldstein, Faulkner, & Wekerle, 2013) as evidenced by associations remaining significant even when co-varying out internalizing symptoms. In a recent meta-analysis on the long-term consequences of neglect, Norman and colleagues (2012) found “robust” evidence for illicit drug use, but weak/inconsistent evidence for neglect’s role in alcohol or smoking cigarettes. Our findings are largely consistent with these findings with the exception of cigarette use. Past research shows that cigarette use often follows a discontinuous trajectory across the lifespan with increasing trajectories in adolescence with use peaking in emerging adulthood especially within those adolescents who do not attend college, and then declining later in life (Riggs, Chou, Li, Pentz, 2007). Given that maltreated adolescents are less likely to attend college (Mersky & Topitzes, 2010) elevated cigarette use in our study was not surprising. Thus, it may be assumed that physically and emotionally neglected youth are at increased risk for illicit drug use across adulthood, but not alcohol use, while increased cigarette use may be seen during developmentally sensitive periods such as emerging adulthood.
A strength of our study was its large, diverse population, and the ability to adequately test whether any of our findings varied as a function of sex and race. Consistent with past research, we found that Latino youth were at decreased risk for neglect exposure. These findings, congruent with CPS samples, suggest that culturally-relevant protective factors (e.g., familiasm; Putnam-Hornstein et al., 2013) may lead to lower rates of neglect exposure for these youth. Examining the specific processes that lead to attenuated neglect rates may be fruitful in augmenting current neglect prevention programs (e.g., Safe Environment for Every Kid; Dubowitz et al., 2009). Of interest, African-Americans were not more likely to experience neglect as previously found in CPS samples (Mennen et al., 2010) suggesting that past reported differences may reflect disproportionate involvement with CPS services as opposed to anything specific to African-American culture. As for sex differences, we did not find any significant differences with regard to neglect-exposure, which is consistent with recent community-based studies (Finkelhor et al., 2013; Stoltenborgh et al., 2013). Finally, with the exception for anxiety with females reporting higher levels, it seems that childhood neglect-exposure confers similar risk for poor clinical outcomes across all emerging adults, suggesting there may be universal benefit from clinical protocols tailored to address neglect experiences.
Our collective findings should be interpreted in light of several limitations. First, reports of maltreatment were retrospective meaning that current symptom patterns could have biased caregiver perceptions (Hardt & Rutter, 2004). Second, our neglect measure did not allow us to examine age of onset or chronicity with regard to maltreatment exposure, characteristics of maltreatment experiences which can have an important impact on clinical outcomes and identifying unique maltreatment subtypes (Kaplow & Widow, 2007; Manly et al., 2001). Fourth, our study was limited to maltreatment experiences, leaving out potentially important stressor experiences, such as academic stressors or interpersonal peer conflict. A more inclusive, dimensional treatment of adverse childhood experiences could lead to alternate profile solutions. Finally, we were unable to control for other variables that could influence the relation between neglect, abuse, and psychopathology (e.g., poverty; Nikulina et al., 2011).
In spite of these limitations, our results add to our collective understanding of childhood neglect-exposure. Similar to other trauma profiles, emerging adults who experienced physical or emotional neglect are at increased risk for emotional distress and substance use behaviors. To target the myriad of symptoms that can emerge in the context of trauma, empirically-based practices advocate to directly target the trauma-experience in order to attenuate negative emotional responses and change the belief structure around the event (Resick, Monson, & Chard, 2008). However, adapting this therapeutic approach for individuals whose trauma-experience is defined by the omission, as opposed to the commission, of an event is challenging. To date, limited research has investigated clinical protocols aimed at attenuating symptoms in neglect-exposed children (Swenson et al., 2010) and no study has examined treatments for adults with childhood neglect-exposure.
Future developmental traumatology research can inform new evidence-based practices for this population by elucidating which traumatic-stress pathways best explain the relation between neglect-exposure in childhood and specific outcomes in early adulthood. For instance, the broad adverse childhood experiences (ACE) literature posits several biological, interpersonal, and psychological reorganizations which occur across the developmental lifespan in the aftermath of trauma-exposure (Cicchetti & Toth, 1995). Recent research suggests that these psychobiological associations may be unique for individuals exposed to experiences characterized by deprivation (i.e., multidimensional poverty) and threat (i.e., violence-exposure) (Sheridan & McLauhglin, 2014); however, the exclusion of neglect within the deprivation conceptualization makes inferences concerning neglect challenging. Identifying which developmental pathways identified within the adverse childhood experiences literature apply to neglect-exposure in the absence of other abuse experiences can provide an empirical foundation for best practices when working with this population.
Acknowledgments
This research was supported by Award Number K23HD059916 (PI: Temple) from the Eunice Kennedy Shriver National Institute of Child Health & Human Development (NICHD) and 2012-WG-BX-0005 (PI: Temple) from the National Institute of Justice (NIJ). The content is solely the responsibility of the authors and does not necessarily represent the official views of NICHD or NIJ.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Bonferroni post-hoc tests with GAD demonstrated a significant difference between the neglect and non-trauma profiles at the p < .05 level. Thus, given our a-priori p values these differences should only be seen as marginally significant.
References
- Adams ZW, Moreland A, Cohen JR, Lee RC, Hanson RF, Danielson CK, … Briggs EC. Polyvictimization: latent profiles and mental health outcomes in a clinical sample of adolescents. Psychology of Violence. 2016;6(1):145–155. doi: 10.1037/a0039713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alvarez-Alonso M, Jurado-Barba R, Martinez-Martin N, Espin-Jaime JC, Bolaños-Porrero C, Ordoñez-Franco A, Rodriguez-Lopez JA, Lora-Pablos D, de la Cruz-Bértolo J, Jimenez-Arriero MA, Manzanares J, Rubio G. Association between maltreatment and polydrug use among adolescents. Child Abuse & Neglect. 2016;51:379–389. doi: 10.1016/j.chiabu.2015.07.014. [DOI] [PubMed] [Google Scholar]
- Arnett JJ. Emerging adulthood: What is it, and what is it good for? Child Development Perspectives. 2007;1:68–73. [Google Scholar]
- Arnett JJ. The emergence of emerging adulthood: A personal history. Emerging Adulthood. 2014;2:155–162. [Google Scholar]
- Bernstein DP, Stein JA, Newcomb MD, Walker E, Pogge D, Ahluvalia T, Stokes J, Handelsman L, Medrano M, Desmond D, Zule W. Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse & Neglect. 2003;27:169–190. doi: 10.1016/s0145-2134(02)00541-0. [DOI] [PubMed] [Google Scholar]
- Berzenski SR, Yates TM. Classes and consequences of multiple maltreatment: a person-centered analysis. Child Maltreatment. 2011;16:250–261. doi: 10.1177/1077559511428353. [DOI] [PubMed] [Google Scholar]
- Birmaher B, Brent DA, Chiappetta L, Bridge J, Monga S, Baugher M. Psychometric properties of the Screen for Child Anxiety Related Emotional Disorders (SCARED): a replication study. Journal of the American Academy of Child & Adolescent Psychiatry. 1999;38(10):1230–1236. doi: 10.1097/00004583-199910000-00011. [DOI] [PubMed] [Google Scholar]
- Borjas GJ. Poverty and program participation among immigrant children. Future Child. 2011;21(1):247–266. doi: 10.1353/foc.2011.0006. [DOI] [PubMed] [Google Scholar]
- Boyce CA, Maholmes V. Attention to the neglected: prospects for research on child neglect for the next decade. Child Maltreatment. 2013;18(1):65–68. doi: 10.1177/1077559513480426. [DOI] [PubMed] [Google Scholar]
- Bradley KL, Bagnell AL, Brannen CL. Factorial validity of the Center for Epidemiological Studies Depression 10 in adolescents. Issues in Mental Health Nursing. 2010;31(6):408–412. doi: 10.3109/01612840903484105. [DOI] [PubMed] [Google Scholar]
- Campbell-Sills L, Cohan SL, Stein MB. Relationship of resilience to personality, coping, and psychiatric symptoms in young adults. Behavior Research & Therapy. 2006;44(4):585–599. doi: 10.1016/j.brat.2005.05.001. [DOI] [PubMed] [Google Scholar]
- Chaffin M, Kelleher K, Hollenberg J. Onset of physical abuse and neglect: psychiatric, substance abuse, and social risk factors from prospective community data. Child Abuse & Neglect. 1996;20(3):191–203. doi: 10.1016/s0145-2134(95)00144-1. [DOI] [PubMed] [Google Scholar]
- Charak R, Koot HM. Severity of maltreatment and personality pathology in adolescents of Jammu, India: A latent class approach. Child Abuse & Neglect. 2015;50:56–66. doi: 10.1016/j.chiabu.2015.05.010. [DOI] [PubMed] [Google Scholar]
- Cheng TC, Lo CC. Drug use among maltreated adolescents receiving child welfare services. Children and Youth Services Review. 2010;32(12):1735–1739. [Google Scholar]
- Cicchetti D, Rogosch FA. A developmental psychopathology perspective on adolescence. Journal of Consulting & Clinical Psychology. 2002;70(1):6–20. doi: 10.1037//0022-006x.70.1.6. [DOI] [PubMed] [Google Scholar]
- Cicchetti D, Toth SL. A developmental psychopathology perspective on child abuse and neglect. Journal of the American Academy of Child & Adolescent Psychiatry. 1995;34:541–565. doi: 10.1097/00004583-199505000-00008. [DOI] [PubMed] [Google Scholar]
- Cohen JR, Spiro CN, Young JF, Gibb BE, Hankin BL, Abela JRZ. Interpersonal risk profiles for youth depression: a person-centered, multi-wave, longitudinal study. Journal of Abnormal Child Psychology. 2015;43:1415–1426. doi: 10.1007/s10802-015-0023-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dubowitz H. Tackling child neglect: A role for pediatricians. Pediatric Clinics of North America. 2009;56:363–378. doi: 10.1016/j.pcl.2009.01.003. [DOI] [PubMed] [Google Scholar]
- Dubowitz H, Feigelman S, Lane W, Kim J. Pediatric primary care to help prevent child maltreatment: the Safe Environment for Every Kid (SEEK) Model. Pediatrics. 2009;123(3):858–864. doi: 10.1542/peds.2008-1376. [DOI] [PubMed] [Google Scholar]
- Finkelhor D, Turner HA, Shattuck A, Hamby SL. Violence, crime, and abuse exposure in a national sample of children and youth: An update. JAMA Pediatrics. 2013;167(7):614–621. doi: 10.1001/jamapediatrics.2013.42. [DOI] [PubMed] [Google Scholar]
- Ford JD, Elhai JD, Connor DF, Frueh BC. Poly-victimization and risk of posttraumatic, depressive, and substance use disorders and involvement in delinquency in a national sample of adolescents. Journal of Adolescent Health. 2010;46:545–552. doi: 10.1016/j.jadohealth.2009.11.212. http://dx.doi.org/10.1016/j.jadohealth.2009.11.212. [DOI] [PubMed] [Google Scholar]
- Galaif ER, Stein JA, Newcomb MD, Bernstein DP. Gender differences in the prediction of problem alcohol use in adulthood: exploring the influence of family factors and childhood maltreatment. Journal of Studies on Alcohol & Drugs. 2001;62(4):486–493. doi: 10.15288/jsa.2001.62.486. [DOI] [PubMed] [Google Scholar]
- Goldstein AL, Faulkner B, Wekerle C. The relationship among internal resilience, smoking, alcohol use, and depression symptoms in emerging adults transitioning out of child welfare. Child Abuse & Neglect. 2013;37(1):22–32. doi: 10.1016/j.chiabu.2012.08.007. dx.doi.org/10.1016/j.chiabu.2012.08.007. [DOI] [PubMed] [Google Scholar]
- Hardt J, Rutter M. Validity of adult retrospective reports of adverse childhood experiences: review of the evidence. Journal of Child Psychology and Psychiatry and Allied Disciplines. 2004;45:260–273. doi: 10.1111/j.1469-7610.2004.00218.x. [DOI] [PubMed] [Google Scholar]
- Hazen AL, Connelly CD, Roesch SC, Hough RL, Landsverk JA. Child maltreatment profiles and adjustment problems in high-risk adolescents. Journal of Interpersonal Violence. 2009;24(2):361–378. doi: 10.1177/0886260508316476. [DOI] [PubMed] [Google Scholar]
- Hildyard KL, Wolfe DA. Child neglect: developmental issues and outcomes. Child Abuse & Neglect. 2002;26(6–7):679–695. doi: 10.1016/s0145-2134(02)00341-1. [DOI] [PubMed] [Google Scholar]
- Hines DA, Kantor GK, Holt MK. Similarities in siblings’ experiences of neglectful parenting behaviors. Child Abuse & Neglect. 2006;30(6):619–637. doi: 10.1016/j.chiabu.2005.11.008. [DOI] [PubMed] [Google Scholar]
- Johnston LD, O’Malley PM, Bachman JG, Schulenberg JE. Monitoring the Future national survey results on drug use, 1975–2009. Volume I: Secondary school students (NIH Publication No. 10-7584) Bethesda, MD: National Institute on Drug Abuse; 2010. p. 734. [Google Scholar]
- Kaplow JB, Widom CS. Age of onset of child maltreatment predicts long-term mental health outcomes. Journal of Abnormal Psychology. 2007;116(1):176–187. doi: 10.1037/0021-843X.116.1.176. [DOI] [PubMed] [Google Scholar]
- Kazemian L, Widom C, Farrington DP. A prospective examination of the relationship between childhood neglect and juvenile delinquency in the Cambridge study in delinquent development. International Journal of Child Youth and Family Studies. 2011;1(2):65–82. [Google Scholar]
- Khrapatina I, Berman P. The Impact of Adverse Childhood Experiences on Health in College Students. Journal of Child & Adolescent Trauma. 2010:1–13. [Google Scholar]
- Kim J, Cicchetti D. Longitudinal trajectories of self-system processes and depressive symptoms among maltreated and nonmaltreated children. Child Development. 2006;77:624–639. doi: 10.1111/j.1467-8624.2006.00894.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manly JT, Kim JE, Rogosch FA, Cicchetti D. Dimensions of child maltreatment and children’s adjustment: Contributions of developmental timing and subtype. Development and Psychopathology. 2001;13(4):759–782. [PubMed] [Google Scholar]
- Mennen FE, Kim K, Sang J, Trickett PK. Child neglect: definition and identification of youth’s experiences in official reports of maltreatment. Child Abuse & Neglect. 2010;34(9):647–658. doi: 10.1016/j.chiabu.2010.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mersky JP, Topitzes J. Comparing early adult outcomes of maltreated and non-maltreated children, A prospective longitudinal investigation. Children & Youth Services Review. 2010;32:1086–1096. doi: 10.1016/j.childyouth.2009.10.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mills R, Alati R, Strathearn L, Najman JM. Alcohol and tobacco use among maltreated and non-maltreated adolescents in a birth cohort. Addiction. 2013;109:672–680. doi: 10.1111/add.12447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milot T, St-laurent D, Louise SE, Provost MA. Trauma-related symptoms in neglected preschoolers and affective quality of mother - child communication. Child Maltreatment. 2010;15(4):293–304. doi: 10.1177/1077559510379153. [DOI] [PubMed] [Google Scholar]
- Ney P, Fung T, Wickett A. The worst combinations of child abuse and neglect. Child Abuse & Neglect. 1994;18:705–714. doi: 10.1016/0145-2134(94)00037-9. [DOI] [PubMed] [Google Scholar]
- Nikulina V, Widom CS, Czaja S. The role of childhood neglect and childhood poverty in predicting mental health, academic achievement and crime in adulthood. American Journal of Community Psychology. 2011;48(3–4):309–321. doi: 10.1007/s10464-010-9385-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norman RE, Byambaa M, De R, Butchart A, Scott J, et al. The long-term health consequences of child physical abuse, emotional abuse, and neglect: a systematic review and meta-analysis. PLoS Med. 2012;9(11) doi: 10.1371/journal.pmed.1001349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pears KC, Kim HK, Fisher PA. Psychosocial and cognitive functioning of children with specific profiles of maltreatment. Child Abuse & Neglect. 2008;32(10):958–971. doi: 10.1016/j.chiabu.2007.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petrenko CLM, Friend A, Garrido EF, Taussig HN, Culhane SE. Does subtype matter? Assessing the effects of maltreatment on functioning in preadolescent youth in out-of-home care. Child Abuse & Neglect. 2012;36(9):633–644. doi: 10.1016/j.chiabu.2012.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prins A, Ouimette PC, Kimerling R, Cameron RP, Hugelshofer DS, Shaw-Hegwer J, Thrailkill A, Gusman FD, Sheikh JI. The primary care PTSD screen (PC-PTSD): Development and operating characteristics. 2003 [Google Scholar]
- Proctor LJ, Dubowitz H. Child neglect: Challenges and controversies. In: Korbin JE, Krugman RD, editors. Handbook of child maltreatment. Dordrecht: Springer; 2014. pp. 27–61. [Google Scholar]
- Putnam-Hornstein E, Needell B, King B, Johnson-Motoyama M. Racial and ethnic disparities: a population-based examination of risk factors for involvement with child protective services. Child Abuse & Neglect. 2013;37(1):33–46. doi: 10.1016/j.chiabu.2012.08.005. [DOI] [PubMed] [Google Scholar]
- Resick PA, Monson CM, Chard KM. Cognitive processing therapy: Veteran/military version. Washington, DC: Department of Veterans’ Affairs; 2008. [Google Scholar]
- Riggs NR, Chou CP, Li C, Pentz MA. Adolescent to emerging adulthood smoking trajectories: when do smoking trajectories diverge, and do they predict early adulthood nicotine dependence? Nicotine & Tobacco Research. 2007;9(11):1147–1154. doi: 10.1080/14622200701648359. [DOI] [PubMed] [Google Scholar]
- Rosenkranz SE, Muller RT, Henderson JL. Psychological maltreatment in relation to substance use problem severity among youth. Child Abuse & Neglect. 2012;36(5):438–448. doi: 10.1016/j.chiabu.2012.01.005. [DOI] [PubMed] [Google Scholar]
- Saunders BE, Adams ZW. Epidemiology of traumatic experiences in childhood. Child and Adolescent Psychiatric Clinics of North America. 2014;23(2):167–184. doi: 10.1016/j.chc.2013.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schilling EA, Aseltine RH, Jr, Gore S. Adverse childhood experiences and mental health in young adults: a longitudinal survey. BMC Public Health. 2007;7:7–30. doi: 10.1186/1471-2458-7-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulenberg JE, Sameroff AJ, Cicchetti D. The transition to adulthood as a critical juncture in the course of psychopathology and mental health. Developmental Psychopathology. 2004;16(4):799–806. doi: 10.1017/s0954579404040015. [DOI] [PubMed] [Google Scholar]
- Sedlak AJ, Mettenburg J, Basena M, Petta I, McPherson K, Greene A, et al. Fourth National Incidence Study of Child Abuse and Neglect (NIS–4): Report to Congress. Washington, DC: U.S. Department of Health and Human Services, Administration for Children and Families; 2010. [Google Scholar]
- Sheridan MA, McLaughlin KA. Dimensions of early experience and neural development: deprivation and threat. Trends in cognitive sciences. 2014;18(11):580–585. doi: 10.1016/j.tics.2014.09.001. http://dx.doi.org/10.1016/j.tics.2014.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spinhoven P, Elzinga BM, Hovens JG, Roelofs K, Zitman FG, van Oppen P, Penninx BW. The specificity of childhood adversities and negative life events across the life span to anxiety and depressive disorders. Journal of Affective Disorders. 2010;126:103–112. doi: 10.1016/j.jad.2010.02.132. [DOI] [PubMed] [Google Scholar]
- Stoltenborgh M, Bakermans-Kranenburg MJ, van Ijzendoorn MH. The neglect of child neglect: a meta-analytic review of the prevalence of neglect. Social Psychiatry and Psychiatric Epidemiology. 2013;8(3):345–355. doi: 10.1007/s00127-012-0549-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swenson CC, Schaeffer CM, Henggeler SW, Faldowski R, Mayhew AM. Multisystemic therapy for child abuse and neglect: a randomized effectiveness trial. Journal of Family Psychology. 2010;24(4):497–507. doi: 10.1037/a0020324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson R, Flaherty EG, English DJ, Litrownik AJ, Dubowitz H, Kotch JB, Runyan DK. Trajectories of adverse childhood experiences and self-reported health at age 18. Academic pediatrics. 2015;15(5):503–509. doi: 10.1016/j.acap.2014.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toth SL, Cicchetti D. A developmental psychopathology perspective on child maltreatment. Child Maltreatment. 2013;18(3):135–139. doi: 10.1177/1077559513500380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Health & Human Services, Administration for Children and Families, Administration on Children, Youth and Families, Children’s Bureau. Child Maltreatment 2014. 2016 Available from http://www.acf.hhs.gov/programs/cb/research-data-technology/statistics-research/child-maltreatment.
- van Vugt E, Lanctôt N, Paquette G, Collin-Vézina D, Lemieux A. Girls in residential care: from child maltreatment to trauma-related symptoms in emerging adulthood. Child Abuse and Neglect. 2014;38(1):114–122. doi: 10.1016/j.chiabu.2013.10.015. [DOI] [PubMed] [Google Scholar]
- Wekerle C, Leung E, Goldstein A, Thornton T, Tonmyr L. Substance use among adolescents in child welfare versus adolescents in the general population: a comparison of the Maltreatment and Adolescent Pathways (MAP) Longitudinal Study and the Ontario Student Drug Use Survey (OSDUS) Datasets. London: University of Western Ontario; 2009. [Google Scholar]
- White HR, Widom CS. Three potential mediators of the effects of child abuse and neglect on adulthood substance use among women. Journal of Studies on Alcohol & Drugs. 2008;69(3):337–347. doi: 10.15288/jsad.2008.69.337. [DOI] [PubMed] [Google Scholar]
- Widom CS. Translational research on child neglect: progress and future needs. Child Maltreatment. 2013;18(1):3–7. doi: 10.1177/1077559513479917. [DOI] [PubMed] [Google Scholar]
- Widom CS, Czaja S, Wilson HW, Allwood M, Chauhan P. Do the long-term consequences of neglect differ for children of different races and ethnic backgrounds? Child Maltreatment. 2013;18(1):42–55. doi: 10.1177/1077559512460728. [DOI] [PubMed] [Google Scholar]
- Widom CS, DuMont K, Czaja SJ. A prospective investigation of major depressive disorder and comorbidity in abused and neglected children grown up. Archives of General Psychiatry. 2007;64:49–56. doi: 10.1001/archpsyc.64.1.49. [DOI] [PubMed] [Google Scholar]
- Widom CS, Marmorstein NR, White HR. Childhood victimization and illicit drug use in middle adulthood. Psychology of Addictive Behaviors. 2006;20:394–403. doi: 10.1037/0893-164X.20.4.394. [DOI] [PubMed] [Google Scholar]
- Wolfe DA, Scott K, Wekerle C, Pittman AL. Child maltreatment: risk of adjustment problems and dating violence in adolescence. Journal of the American Academy of Child & Adolescent Psychiatry. 2001;40(3):282–289. doi: 10.1097/00004583-200103000-00007. [DOI] [PubMed] [Google Scholar]
- Wolock I, Horowitz B. Child maltreatment as a social problem: the neglect of neglect. American Journal of Orthopsychiatry. 1984;54(4):530–543. doi: 10.1111/j.1939-0025.1984.tb01524.x. [DOI] [PubMed] [Google Scholar]
- Young R, Lennie S, Minnis H. Children’s perceptions of parental emotional neglect and control and psychopathology. Journal of Child Psychology and Psychiatry. 2011;52(8):889–897. doi: 10.1111/j.1469-7610.2011.02390.x. [DOI] [PMC free article] [PubMed] [Google Scholar]