Abstract
Brucellosis is an infectious disease that affects many organ systems. Osteoarticular involvement, especially spondylitis, is the most common complication of brucellosis, but psoas abscess is very rare. Serological tests at diagnosis of the disease are very valuable and most widely used. Herein, we report a case of psoas abscess secondary to brucellar spondylitis. In this case, interestingly, the serological test results were negative, and the diagnosis could be made by abscess culture. In patients, particularly those who live in areas endemic for brucellosis, as in our case, it should be kept in mind that a negative serological test result should not exclude the diagnosis of brucellosis.
Keywords: Brucellosis, psoas abscess, spondylitis, serological test
Introduction
Brucellosis is a common zoonosis that affects many organ systems. Osteoarticular involvement, including sacroiliitis, spondylitis, peripheral arthritis, osteomyelitis, tenosynovitis, and bursitis, is the most frequent complication of brucellosis. Brucellar spondylitis is a serious complication that may result in the formation of abscesses (1). Serological tests at diagnosis of the disease are very valuable and most widely used (2). However, a negative serological test result should not always exclude the diagnosis of brucellosis. In this study, we present a case of psoas abscess secondary to brucellar spondylitis; in this case, all serological test results were negative.
Case Presentation
A 76-year-old female presented with lower back pain that had been ongoing for a few weeks. She did not present any systemic complaints such as fever, weakness, weight loss, morning stiffness, night sweating, or incontinence. She reported consumption of fresh white cheese using unpasteurized dairy products. The physical examination revealed restricted and painful lumbar motion and paravertebral muscle spasm. Systemic examination was normal. The patient’s laboratory tests showed an erythrocyte sedimentation rate (ESR) of 90 mm/h; C-reactive protein (CRP) level was 51.6 mg/L (normal, 0–6 mg/L). Complete biochemical, hematological, and urinary analysis were normal. Standard tube agglutination tests for Brucella and Salmonella were negative. Magnetic resonance imaging (MRI) (Magnetom Symphony 1.5T, Siemens; Erlangen, Germany) of the lumbar spine revealed that the corpora and right peduncles of L2–3 vertebrae was bone marrow signal intensity changes consistent with edema. Based on the MRI findings, spondylitis was believed to be present. Blood culture was found to be negative. Consequently, needle biopsy was planned, but the patient refused further diagnostic approaches and therapy.
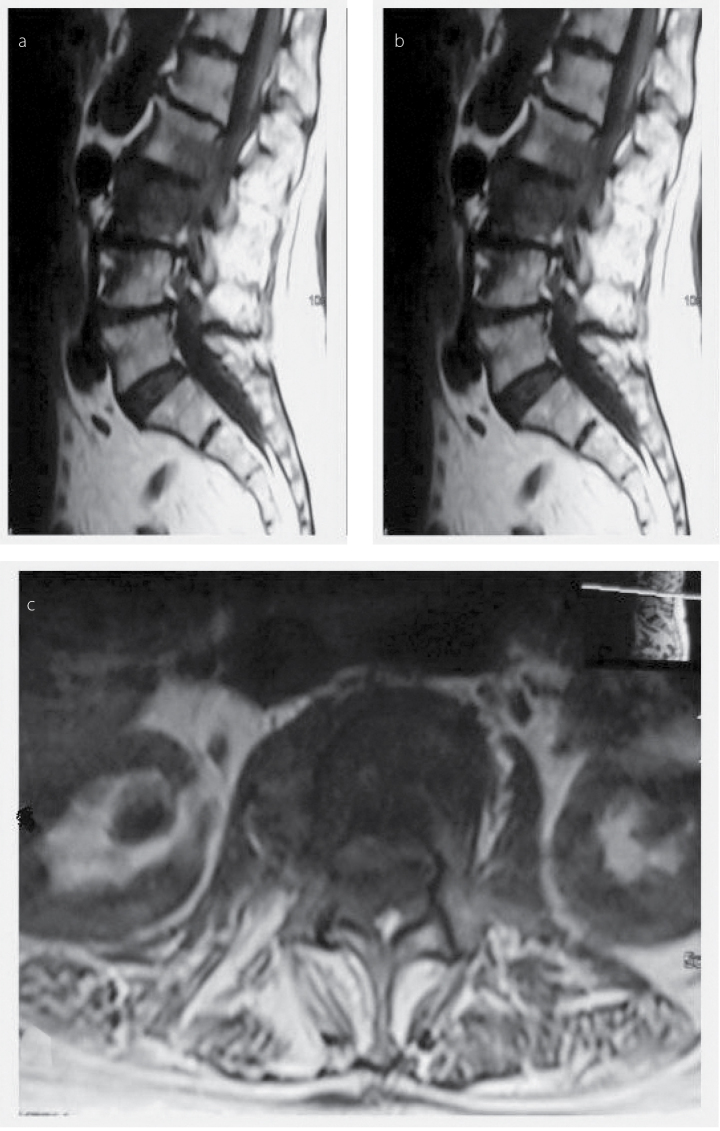
Six months later, the patient was admitted with lower back pain radiating over the right leg. She had difficulty walking and getting up from her seat. Physical examination findings remained the same. Her laboratory tests included white blood cell counts of 12,400/mm3, with 80% neutrophils; thrombocyte count was 575,000/mm3, ESR was 65 mm/h, and CRP levels were 68.2 mg/dL. The tube agglutination test for brucellosis was negative. MRI of the lumbar spine revealed distinct contour irregularity of the disc space and destruction of vertebral endplates at L2–3 vertebrae region, consistent with spondylitis, and a soft tissue abscess at the right iliopsoas muscle (Figure 1). In order to determine the causative pathogen, blood cultures were repeated, but again, the culture test results were negative. Brucella was isolated from abscess cultures from the psoas muscle. On the basis of these findings, the patient was diagnosed with brucellar spondylitis and psoas abscess.
Figure 1. a–c.
Sagittal spin-echo T1-weighted image showed decreased signal intensity in bodies of L2–3 vertebrae (a), turbo spin-echo T2-weighted image showed increased signal intensity in bodies of L2–3 vertebrae (b), and transverse T1-weighted spin-echo image showed heterogeneous enlargement of psoas muscle (c)
During the treatment, the patient was administered doxycycline (Tetradox, Actavis; Iceland) (200 mg/day) and rifampicin (Rifadin, Sanofi Aventis; France) (600 mg/day) for 3 months. Analgesics and immobilization with orthosis were used to reduce pain. After 6 weeks of treatment, a remarkable improvement in the symptoms was noted, and inflammation marker levels became normal. MRI of the lumbar spine vertebrae was defined that the abscess image in which detected by the previous MRI was disappeared and was revealed secondary changes of the spondylitis.
Discussion
Brucellosis is an infectious disease; it is caused by the spread of Brucella species via exposure to infected animals or contaminated animal products (2). It is an important problem in Turkey considering the increase in mortality during recent years (8.69 vs. 20.30 per 100,000 people in 1990 and 2003, respectively) (3). Osteoarticular involvement, including spondylitis, osteomyelitis, arthritis, tenosynovitis, and bursitis is the most common (10%–80%) presentation of brucellosis (1). Spondylitis is a serious complication because it may be associated with abscess formation. This condition is generally seen in the elderly, as in the present case (1). In 335 patients with brucellosis, osteoarticular involvement was determined in 59.2% patients; thereof, 28.6% had spondylitis. Abscess formation has been reported in 7.1% patients with brucellosis in the literature (4). Brucella has been reported to be the causative pathogen in 5.7% of 124 patients with psoas abscess and the origin was skeletal system in all cases (5). Psoas abscess has been reportedly noted in only 3 of 452 patients with brucellosis in Turkey (3). Lower rates in other studies might be due to the MRI examination being performed in only 245 patients.
Serological tests are very important in the diagnosis of brucellosis. The serum agglutination test (SAT) for brucellosis developed by Wright is still the most widely used serological test. Although there is no consensus with regard to the diagnostic level of Brucella agglutinating antibody titer in endemic countries, we uses 1:160 in Turkey, which is an endemic country for brucellosis (2). The SAT result was negative in our patient. False negative results in SAT may be obtained in the presence of blocking antibodies or absence of agglutination in low serum dilutions as called prozone phenomenon (6). Coombs test should be performed to avoid false negative SAT results in the presence of clinical suspicion. This test increases the sensitivity of the SAT (6). In a study examining 3893 patients in whom the SAT result was negative, positive Coombs test was found in 1% of these patients (7). Coombs test is used to detect antibodies in which case the agglutination in SAT is negative (to avoid the effect of blocking antibodies). This test is not required too much because the blocking antibodies are very rare in brucellosis (8). However, in endemic regions for brucellosis such as Turkey, the SAT and Coombs test should be used together. This is quite important to avoid false negative results. In our patient, both the agglutination test results were negative. The serological tests, as in our case, may be negative in 1%–2% cases of brucellosis with osteoarticular involvement (9). In the presence of clinical symptoms, the presence of Brucella species in the culture of blood, bone marrow, or tissue must be evaluated even if the serological test results are negative. The specificity of blood culture in the diagnosis of brucellosis ranges between 17% and 85% (10). The specificity decreases as the disease prolongs. Abscess culture gives positive findings in 10%–20% cases (10). In our patient, abscess culture was positive for Brucella, despite the SAT, Coombs test, and blood culture being negative. MRI is the gold standard method for imaging the spinal canal, neural elements, and the adjacent soft tissues. This method has high sensitivity for detecting spondylitis in its early stages and provides excellent definition of paravertebral and epidural area (11). However, the definitive diagnosis of brucellosis is possible by isolation of the organism via the culture of blood, bone marrow, or tissue.
In conclusion, in patients who live in areas endemic for brucellosis, brucellar spondylitis and psoas abscess should be included in differential diagnosis, particularly for those with longstanding back pain. Serological tests are very valuable for the diagnosis and should be routinely used in suspected cases. However, it should be kept in mind that sometimes, these tests may present false negative results for brucellosis, as in our case.
Footnotes
Ethics Committee Approval: N/A.
Informed Consent: Written informed consent was obtained from the patient.
Peer-review: Externally peer-reviewed.
Author Contributions: Consept - G.T.B., A.I.U.; Design - G.T.B., A.I.U., G.G.; Supervision - G.G.; Fundings - G.T.B., A.I.U.; Data Collection and/or Processing - A.I.U.; Literature Review - G.T.B.; Writer - G.T.B., A.I.U., G.G.; Critical Review - G.T.B.
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The author declared that this study has received no financial support.
References
- 1.Aydın G, Tosun A, Keleş I, Ayaşlıoğlu E, Tosun O, Orkun S. Brucellar spondylodisciticis: a case report. Int J Clin Pract. 2006;60:1502–5. doi: 10.1111/j.1742-1241.2005.00656.x. https://doi.org/10.1111/j.1742-1241.2005.00656.x. [DOI] [PubMed] [Google Scholar]
- 2.Çelik AD, Yulugkural Z, Kilincer C, Hamamcioglu MK, Kuloglu F, Akata F. Negative serology: could exclude the diagnosis of brucellosis? Rheumatol Int. 2012;32:2547–9. doi: 10.1007/s00296-010-1453-y. https://doi.org/10.1007/s00296-010-1453-y. [DOI] [PubMed] [Google Scholar]
- 3.Turgut M, Turgut AT, Kosar U. Spinal brucellosis: Turkish experience based on 452 cases published during the last century. Acta Neurochir (Wien) 2006;148:1033–44. doi: 10.1007/s00701-006-0877-3. https://doi.org/10.1007/s00701-006-0877-3. [DOI] [PubMed] [Google Scholar]
- 4.Bosilkovski M, Krteva L, Caparoska S, Dimzova M. Osteoarticular Involvement in Brucellosis: Study of 196 Cases in the Republic of Macedonia. Croat Med J. 2004;45:727–33. [PubMed] [Google Scholar]
- 5.Navarro López V, Ramos JM, Meseguer V, Pérez Arellano JL, Serrano R, García Ordóñez MA, et al. Microbiology and outcome of iliopsoas abscess in 124 patients. Medicine (Baltimore) 2009;88:120–30. doi: 10.1097/MD.0b013e31819d2748. https://doi.org/10.1097/MD.0b013e31819d2748. [DOI] [PubMed] [Google Scholar]
- 6.Guven GS, Cakir B, Oz G, Tanriover MD, Turkmen E, Sozen T. Could remembering the prozone phenomenon shorten our diagnostic journey in brucellosis? A case of Brucella spondylodiscitis. Rheumatol Int. 2006;26:933–5. doi: 10.1007/s00296-006-0118-3. https://doi.org/10.1007/s00296-006-0118-3. [DOI] [PubMed] [Google Scholar]
- 7.Alişkan H. The value of culture and serological methods in the diagnosis of human brucellosis. Mikrobiyol Bul. 2008;42:185–95. [PubMed] [Google Scholar]
- 8.Young EJ. Brucella species. In: Mandell GL, Bennet JE, Dolin R, editors. Principles and Practice of Infectious Disease. 5 edition. Churchill Livingstone; Philadelphia: 2000. p. 2386. [Google Scholar]
- 9.Janmohammadi N, Roushan MR. False negative serological tests may lead to misdiagnosis and mismanagement in osteoarticular brucellosis. Trop Doct. 2009;39:88–90. doi: 10.1258/td.2008.080042. https://doi.org/10.1258/td.2008.080042. [DOI] [PubMed] [Google Scholar]
- 10.Chelli Bouaziz M, Ladeb MF, Chakroun M, Chaabane S. Spinal brucellosis: a review. Skeletal Radiol. 2008;37:785–90. doi: 10.1007/s00256-007-0371-x. https://doi.org/10.1007/s00256-007-0371-x. [DOI] [PubMed] [Google Scholar]
- 11.Yang X, Zhang Q, Guo X. Value of magnetic resonance imaging in brucellar spondylodiscitis. Radiol Med. 2014;119:928–33. doi: 10.1007/s11547-014-0416-x. https://doi.org/10.1007/s11547-014-0416-x. [DOI] [PubMed] [Google Scholar]