Main text
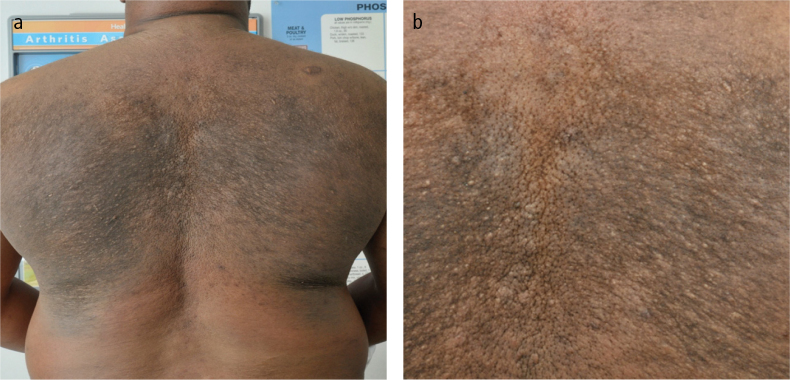
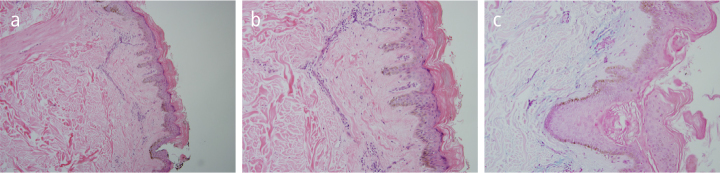
A 46-year-old African-American male with a history of type-1 diabetes (DM) was referred to the Rheumatology clinic for a further evaluation of possible systemic scleroderma. He reported a 3-year history of skin thickening and hyperpigmentation on his back and shoulders. Over the last 12 months, his symptoms progressed, involving the proximal arms, legs, and back with sparing of his hand and feet. His medical history was remarkable for insulin-dependent DM, which was complicated with diabetic retinopathy and peripheral neuropathy. Skin examination revealed a woody, hardened, indurated, hyperpigmented skin with a peau d’orange appearance involving the posterior aspect of the neck, shoulders, arms, legs, and mid-back (Figure 1a, b). The face, chest, forearms, hands, and feet were unaffected. There was no telangiectasia, sclerodactyly, fingertip ulceration, or calcinosis. The remainder of the physical examination was unremarkable. Laboratory evaluation revealed a normal complete blood count, comprehensive metabolic panel, Western sedimentation rate, C-reactive protein, creatine phosphokinase level, aldolase, and thyroid-stimulating hormone. Hemoglobin A1C level was 7.1 (normal <6). Immunofluorescence antinuclear antibodies, complement levels, and Scl-70 were all negative. Serum protein electrophoresis and urine protein electrophoresis were normal. Full thickness skin biopsy revealed a thickened dermis, with fenestrated collagen and mucin deposition in the deep dermis, which is consistent with the diagnosis of scleredema (Figure 2 a–c).
Figure 1. a, b.
A picture of the patient’s back showing; wood-like thickening of the skin of the upper and mid-back with obvious peau d’orange changes and (a), a magnified view of the mid-back showing wood-like thickening of the skin of the upper and mid-back with obvious peau d’orange changes (b)
Figure 2. a, c.
H&E staining of the skin biopsy represents (a), an unaffected epidermis, while the dermis is thicker than normal (the dermis can be up to four times thicker than normal). Edematous spaces between the collagen bundles are present at a microscopic magnification of 10x. Collagen fibers appear swollen and separated by wide spaces at a microscopic magnification of 40x (b), a focal lymphocytic infiltration of the reticular dermis with collagen bands separated by clear spaces are present at a microscopic magnification of 60x (c)
Scleredema is a sclerotic skin disease, which is a largely unknown pathogenesis, that generally occurs in association with DM, infection (particularly streptococcal infection of the upper respiratory tract), or monoclonal gammopathy. DM, particularly type II, is considered the most common form of the disease and primarily affects adults, particularly middle-aged obese individuals. In scleroderma associated with diabetes, an irreversible glycosylation of collagen as well as alterations in collagenase activity may lead to an excessive accumulation of collagen and mucin. The condition is characterized by firm, non-pitting edema that typically begins at the neck and spreads to the face, scalp, shoulders, and trunk. The hands and feet are characteristically not affected (1).
Several sclerotic disorders can share clinical features with scleredema, such as systemic sclerosis, scleromyxedema, and eosinophilic fasciitis. Physical therapy has to be initiated as soon as possible to minimize functional limitations related to reduced joint mobility. Multiple treatment approaches have been studied, including immunosuppressive agents such as cyclosporine, methotrexate, and systemic glucocorticoids (e.g., dexamethasone pulse therapy or high-dose intravenous glucocorticoids), and show promising outcomes, but further studies are required (2–4).
Footnotes
Ethics Committee Approval: N/A.
Informed Consent: Written informed consent was obtained from the patient.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept - R.N., A.A.; Design - R.N. A.A.; Supervision - R.N. A.A.; Materials - RN., A.A.; Data Collection and/or Processing - R.N., A.A.; Analysis and/or Interpretation - R.N., A.A.; Literature Review - R.N., A.A.; Writer - R.N., A.A.; Critical Review - R.N., A.A.
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: Rajaie Namas is supported by the National Institute of Arthritis and Musculoskeletal and Skin Diseases grant number T32AR007080-37.
References
- 1.Rimon D, Lurie M, Storch S, Halon D, Eisenkraft S, Laor A, et al. Cardiomyopathy and multiple myeloma. Complications of scleredema adultorum. Arc Internal Med. 1988;148:551–3. https://doi.org/10.1001/archinte.148.3.551. [PubMed] [Google Scholar]
- 2.Mattheou-Vakali G, Ioannides D, Thomas T, Lazaridou E, Tsogas P, Minas A. Cyclosporine in scleredema. J Am Acad Dermatol. 1996;35:990–1. doi: 10.1016/s0190-9622(96)90129-2. https://doi.org/10.1016/S0190-9622(96)90129-2. [DOI] [PubMed] [Google Scholar]
- 3.Seyger MM, van den Hoogen FH, de Mare S, van Haelst U, de Jong EM. A patient with a severe scleroedema diabeticorum, partially responding to low-dose methotrexate. Dermatology. 1999;198:177–9. doi: 10.1159/000018103. https://doi.org/10.1159/000018103. [DOI] [PubMed] [Google Scholar]
- 4.Kurtoglu S, Yuksel S, Gunduz Z, Per H, Narin N, Kontas O, et al. Use of high-dose intravenous corticosteroid treatment in a child with scleredema. J Emerg Med. 2004;26:245–6. doi: 10.1016/j.jemermed.2003.12.006. https://doi.org/10.1016/j.jemermed.2003.12.006. [DOI] [PubMed] [Google Scholar]