Abstract
Background
Slow coronary flow (SCF) is an angiographic finding characterized with delayed opacification of epicardial coronary arteries without obstructive coronary disease. Urotensin II (UII) is an important vascular peptide, which has an important role in hypertension, coronary artery disease, and vascular remodeling in addition to potent vasoconstrictor effect.
Objectives
We investigated UII levels, hypertension, and other atherosclerotic risk factors in patients with SCF, a variety of coronary artery disease.
Methods
We enrolled 14 patients with SCF and 29 subjects with normal coronary arteries without SCF. We compared the UII levels and the atherosclerotic risk factors between patients with SCF and control subjects with normal coronary flow.
Results
UII concentrations were significantly higher in patients with SCF compared to controls (711.0 ± 19.4 vs. 701.5 ± 27.2 ng/mL, p = 0.006). We detected a positive correlation between SCF and age (r = 0.476, p = 0.001), BMI (r = 0.404, p = .002), UII concentrations (r = 0.422, p = 0.006), and hypertension (r = 0.594, p = 0.001).
Conclusion
We identified increased UII levels in patients with SCF. We think that UII concentrations may be informative on SCF pathogenesis due to relationship with inflammation, atherosclerosis, and vascular remodeling.
Keywords: slow coronary flow, urotensin II, atherosclerosis, atherosclerotic risk factors, CRP
Introduction
Slow coronary flow (SCF) is an angiographic finding characterized with delayed opacification of epicardial coronary arteries without obstructive coronary disease [1]. SCF is a relatively common angiographic finding with a reported incidence of 1% in patients undergoing coronary angiography for the suspicion of coronary artery disease (CAD) [2]. Since the first description in 1972 by Tambe et al. [1], only a limited number of studies have focused on SCF; therefore, the precise pathophysiological mechanisms and the clinical importance of SCF are not fully understood at the moment. Several mechanisms have been proposed for SCF phenomenon including small vessel disease, microvascular vasomotor dysfunction, diffuse atherosclerosis, and endothelial dysfunction [3–6]. Occlusive disease of the small coronary arteries, which may be a form of early phase atherosclerosis, has also been suggested as a cause [7]. Moreover, SCF may cause transient myocardial hypoperfusion in patients with angina and normal coronary arteries, and these patients have higher probability of significant CAD and an apparently worse prognosis [8].
Urotensin II (UII), an undecapeptide cleaved from a precursor protein, promotes vasoconstriction and vascular smooth muscle cell proliferation [9, 10]. UII is one of the most important and the most studied peptide involved in vascular remodeling. UII, a potent vascular constrictor, is up-regulated in patients with hypertension, and atherosclerosis in addition to relevant receptors [11–13].
Even though, the pathophysiological impact of UII in atherosclerosis and coronary artery disease has been studied extensively, the role of UII in SCF as a different variety of atherosclerosis has not been clarified so far. We think that pro-atherosclerotic and inflammatory actions of UII may also act in SCF pathogenesis. Therefore, we intended to investigate UII concentrations and atherosclerotic risk factors in patients with SCF compared to control subjects with normal coronary flow (NCF).
Methods
Patient population and study protocol
Our study was prospective and cross sectional. Among 2,049 patients, coronary angiography procedures performed between September 2010 and 2011 in our hospital, we selected patients with the presence of typical stable angina pectoris and positive or equivocal results in non-invasive stress tests as the indication. Patients with obstructive CAD, left ventricular dysfunction, left ventricular hypertrophy, atrial fibrillation, valvular heart disease, pericardial and myocardial diseases, renal dysfunction (creatinine >1.5 mg/dL), anemia, thrombocytopenia, hepatic dysfunction, neoplasms, recent major surgical operation, and accompanying inflammatory diseases such as hemolytic and autoimmune disorders were excluded.
We excluded 823 patients with acute coronary syndromes. Following the careful review of remaining 1,226 patients, we identified 14 (6 males) patients with SCF. We enrolled subjects with normal coronary arteries and flow consecutively in a ratio of 1:2. Thus, 29 patients (11 males) who had normal coronary angiograms and flow were enrolled as control subjects. UII levels were measured in all subjects and compared between groups. The study has been approved by the local ethics committee and is in accordance with the Declaration of Helsinki. All patients gave informed consent before participation. Medical histories were taken and thorough examination was performed.
Hypertension was acknowledged if the patient was on antihypertensive medication or if systolic blood pressure ≥140 mmHg, diastolic blood pressure ≥90 mmHg, or both were observed during examination. Diabetes mellitus was considered if fasting blood glucose was >126 mg/dL or if the patient was on antidiabetic therapy. Patients who were using tobacco products on admission to our hospital and those quitted smoking within the last year were considered as smokers.
Coronary angiography and determination of SCF
Standard selective coronary angiography with at least four views of the left coronary artery and two views of the right coronary artery (RCA) were performed using the Judkins technique and 6-French right and left heart catheters without the use of nitroglycerin. All procedures were performed via femoral access site. Coronary angiograms were recorded in the right and left oblique planes using cranial and caudal angulations at a rate of 30 frames/s. During coronary angiography, iopromide (Ultravist 370, Schering AG, Berlin, Germany) was used as the contrast agent in all patients. The patients were assessed for the presence of SCF during coronary angiography and coronary flow rates were quantified by the thrombolysis in myocardial infarction (TIMI) frame count (TFC) method. For objective quantification of the coronary flow, two independent observers blinded to the clinical data of the study participants assessed the coronary flow in coronary arteries using TFC [14]. This method establishes the number of cine frames, recorded at 30 frames/s, required for the contrast to reach standard distal coronary landmarks in the left anterior descending artery (LAD), left circumflex artery (LCx), and RCA. Predefined distal landmarks are the distal bifurcation for the LAD, commonly referred to as the “pitchfork” or “whale’s tail,” the distal bifurcation of the segment with the longest total distance for the LCx, and the first branch of the posterolateral artery for the RCA. The standard mean values for normal visualization of coronary arteries are described as 36.2 ± 2.6 frames for LAD, 22.2 ± 4.1 frames for LCx, and 20.4 ± 3.0 frames for RCA. As the LAD is usually longer than the other major coronary arteries, the TFC for this vessel is often higher. Therefore, the TFC for LAD is divided by 1.7 to obtain the corrected TFC (cTFC). The standard corrected mean value (cTFC) for LAD coronary artery is 21.1 ± 1.5 frames. All participants with a TFC greater than the two standard deviations of the previously published range for the particular vessel were considered to have SCF [14]. The mean TFC for each patient and control participant was calculated by dividing the sum of the TFC of the corrected LAD, LCx, and RCA by three.
Biochemical analyses
Blood samples were drawn by venipuncture to measure routine blood chemistry parameters after fasting for at least 8 h. Fasting blood glucose, serum creatinine, total cholesterol, high-density lipoprotein cholesterol, low-density lipoprotein cholesterol, and triglyceride levels were recorded. Glucose, creatinine, and lipid profile were determined by standard methods. Serum C-reactive protein (CRP) was analyzed using a nephelometric technique (Beckman Coulter Immage 800; Fullerton, CA, USA; normal range: 0–0.8 mg/dL).
Measurement of UII
We collected blood samples from the antecubital vein of subjects after overnight fasting to measure blood biochemical parameters, including plasma UII levels. Blood was drawn into the tubes containing disodium ethylenediaminetetraacetic acid (1 mg/mL) and aprotinin (500 U/mL; Sigma-Aldrich, St. Louis, MO, USA), then centrifuged immediately at 3,500 × g for 10 min at 4 °C; plasma was stored at −80 °C for assay. UII levels were measured by radioimmunoassay (RIA). In brief, samples extracted through a Sep-Pak C18 cartridge were assayed by the use of an RIA kit (Phoenix Pharmaceuticals, Belmont, CA, USA). For the UII immunoreactivity assay, the cross-reactivity with human UII was 100%. The intra- and inter-assay coefficients of variation of UII for blood samples were both <10%.
Statistical analysis
The SPSS statistical software (SPSS 15.0 for windows, SPSS Inc., Chicago, IL, USA) was used for all statistical calculations. Continuous variables were given as mean ± SD or median (interquartile range) as appropriate; categorical variables were defined as percentage. Data were tested for normal distribution using the Kolmogorov–Smirnov test. The Student’s t-test was used for the univariate analysis of normally distributed continuous numerical variables and Mann–Whitney U test was used for non-normally distributed numerical variables, and the χ2-test for the categorical variables. All tests of significance were two-tailed. Statistical significance was defined as p < 0.05.
Results
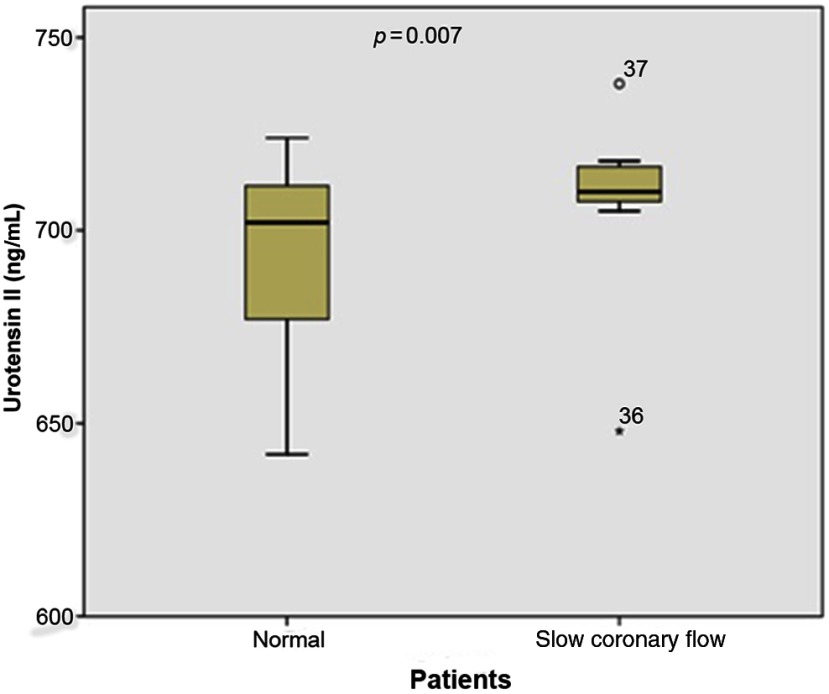
UII concentrations were significantly higher in patients with SCF compared to controls (711.0 ± 19.4 vs. 701.5 ± 27.2 ng/mL, p = 0.006). Moreover, patients with SCF tended to be older (55 ± 12 vs. 42 ± 11 years, p = 0.001), and have a higher body mass index (BMI) (30 ± 4 vs. 26 ± 4 kg/m2, p = 0.002), and more prevalent hypertension (64% vs. 10%, p = 0.001). Remaining basal characteristics and atherosclerotic risk factors were similar between groups. We detected a positive correlation between SCF and age (r = 0.476, p = 0.001), BMI (r = 0.404, p = 0.002), UII concentrations (r = 0.422, p = 0.006), and hypertension (r = 0.594, p = 0.001) (Fig. 1, Tables I and II).
Fig. 1.
UII concentrations in patients with SCF and control group
Table I.
Baseline characteristics of the study population
| Parameters (n = 43) | SCF group (n = 14) | Control group (NCF, n = 29) | p value |
|---|---|---|---|
| Age (years ± SD) | 55 ± 12 | 42 ± 11 | 0.001 |
| Sex (male), n (%) | 6 (43) | 11 (38) | 0.821 |
| Body mass index | 30 ± 4 | 26 ± 4 | 0.002 |
| Hypercholesterolemia, n (%) | 7 (50) | 11 (38) | 0.532 |
| Family history of CAD, n (%) | 7 (50) | 10 (35) | 0.334 |
| Smoking, n (%) | 4 (29) | 8 (28) | 0.902 |
| HT, n (%) | 9 (64) | 3 (10) | 0.001 |
| Diabetes mellitus, n (%) | 2 (14) | 4 (14) | 0.936 |
| Hemoglobin (g/dL) | 13.9 ± 1.2 | 13.5 ± 1.3 | 0.506 |
| Total cholesterol (mg/dL) | 195 ± 50 | 188 ± 35 | 0.639 |
| LDL (mg/dL) | 129 ± 45 | 119 ± 32 | 0.143 |
| HDL (mg/dL) | 40 ± 9 | 45 ± 9 | 0.428 |
| Triglycerides (mg/dL) | 144 ± 105 | 141 ± 63 | 0.929 |
| Urotensin II (ng/mL) [median ± IQR] | 711.0 [700–721] | 701.5 [666.5–736.5] | 0.006 |
| Glucose (mg/dL) [median ± IQR] | 103 [76–130] | 94 [81–107] | 0.050 |
| Creatinine (mg/dL) [median ± IQR] | 0.78 [0.67–0.89] | 0.75 [0.6–0.9] | 0.536 |
| TIMI frame count measurements | |||
| LAD | 31 ± 7 | 61 ± 30 | 0.001 |
| LAD (corrected) | 19 ± 4 | 35 ± 18 | 0.001 |
| LCx | 23 ± 6 | 32 ± 14 | 0.005 |
| RCA | 21 ± 5 | 43 ± 23 | 0.001 |
| Mean | 22 ± 4 | 37 ± 14 | 0.001 |
SCF, slow coronary flow; UII, urotensin II; HT, hypertension; SD, standard deviation; NCA, normal coronary flow (control group); CAD, coronary artery disease; TIMI, thrombolysis in myocardial infarction; LAD, left anterior descending artery; LCx, left circumflex artery; RCA, right coronary artery; IQR, interquartile range
Table II.
Correlations of SCF and UII with the study parameters
| Parameters | SCF | Age | BMI | UII | HT |
|---|---|---|---|---|---|
| SCF | – |
r = 0.476 p = 0.001 |
r = 0.404 p = 0.002 |
r = 0.422 p = 0.006 |
r = 0.564 p = 0.001 |
| Age |
r = 0.476 p = 0.001 |
– |
r = 0.481 p = 0.001 |
r = 0.075 p = 0.634 |
r = 0.590 p = 0.000 |
| BMI |
r = 0.404 p = 0.002 |
r = 0.481 p = 0.001 |
– |
r = 0.037 p = 0.814 |
r = 0.493 p = 0.001 |
| UII |
r = 0.422 p = 0.006 |
r = 0.075 p = 0.634 |
r = 0.037 p = 0.814 |
– |
r = 0.230 p = 0.138 |
| HT |
r = 0.564 p = 0.001 |
r = 0.590 p = 0.000 |
r = 0.493 p = 0.001 |
r = 0.230 p = 0.138 |
– |
SCF, slow coronary flow; UII, urotensin II; HT, hypertension; BMI, body mass index
Discussion
In this study, we revealed significantly higher UII levels in patients with SCF compared to patients with angiographically normal coronary arteries and NCF. Moreover, we detected that SCF significantly associated with hypertension, advanced age, and obesity.
Although the exact mechanism of SCF is not consistently determined, there are several suggested mechanisms involved in the pathogenesis of SCF. The first hypothesis that small vessel dysfunction contributes to the pathogenesis of SCF was proposed by Tambe et al. [1] and was confirmed by Mangieri et al. [3], who demonstrated microvascular abnormalities in patients with SCF [3]. Their histopathological examinations showed evidence of small vessel abnormalities such as endothelial thickening due to cell edema, capillary damage, and reduced luminal diameter of the small vessels. In addition, Kurtoğlu et al. [15] reported an improvement in microvascular tone and coronary flow with microvascular vasodilators, implying a functional increase in microvascular resistance. On the contrary, intravascular ultrasound examinations identified epicardial CAD as a pathophysiological factor for SCF, in addition to microvascular disease [4]. Abnormal slow flow pattern in coronary arteries has been deduced to be a manifestation of diffuse atherosclerotic disease due to endothelial injury without creating an angiographically visible coronary lesion [16]; therefore, SCF may be an early manifestation of diffuse atherosclerosis involving both microvascular system and epicardial coronary arteries [4]. In addition, inflammation [17, 18], platelet function disorder [19, 20], and imbalance of vasoactive substances [15, 21] have also been blamed in the pathogenesis of the SCF phenomenon. Serum paraoxonase (PON), a high-density lipoprotein bound antioxidant enzyme, acts against atherosclerosis and endothelial dysfunction. Yıldız et al. [22] reported an independent association between serum PON activity with the mean TFC, suggesting that reduced serum PON activity may be a biochemical marker of SCF. Enli et al. [23] demonstrated significantly increased serum malondialdehyde, erythrocyte superoxide dismutase, and decreased erythrocyte-reduced glutathione levels in patients with SCF compared to patients with NCF. These findings indicate that free radical damage as well as endothelial dysfunction may also take place in the pathogenesis of SCF. In contrast to these data, recently, Kopetz et al. [24] could not demonstrate any differences in endothelial function, inflammatory proteins (myeloperoxidase and high-sensitivity CRP), oxidative stress biomarkers (malondialdehyde and homocysteine), and asymmetric dimethylarginine levels in patients with SCF compared to healthy controls. Therefore, the mechanisms and pathogenesis of SCF remain controversial.
UII induces potent vasoconstriction and vascular smooth muscle cell proliferation. The UII receptor–UII interaction stimulate the release of calcium (Ca2+) in vascular smooth muscle cells through inositol triphosphate and diacylglycerol. Increased intracellular calcium concentrations lead to cellular proliferation and activation of Ca2+-dependent kinases via calmodulin binding [25].
Recent studies have shown that UII may have additional negative influence on vascular remodeling. UII and angiotensin II affect vascular endothelial growth factor (VEGF) expression in adventitial fibroblasts that have an important role in vascular remodeling. Although the exact role of VEGF in vascular remodeling induced by UII is still not clarified, adventitial fibroblast proliferation and increased collagen synthesis may ensue [26].
Studies investigating the association between UII and atherosclerosis have revealed raised plasma UII levels in patients with vascular disorders such as essential hypertension, diabetes mellitus, atherosclerosis, ischemic heart disease, and heart failure. UII is synthesized in endothelial cells, smooth muscle cells, and infiltrating macrophages of atherosclerotic lesions. Inflammation upregulates urotensin receptor expression. Stimulation of receptor by UII leads to endothelial and smooth muscle cell proliferation, foam cell formation, and chemotaxis via vascular cell adhesion molecule-1 and intercellular adhesion molecule-1 expression. In addition, UII produces reactive oxygen species through nicotinamide adenine dinucleotide phosphate oxidase system in vascular smooth muscle cells, which induces smooth muscle cell proliferation and accelerates atherosclerosis [27]. Therefore, UII seems to have a key role in progression of atherosclerotic cardiovascular diseases. Hassan et al. [28] demonstrated UII expression in endothelial cells, foam cells, and myointimal and medial vascular smooth muscle cells of atherosclerotic human coronary arteries.
Higher plasma UII concentrations that were associated with the severity of CAD were demonstrated in patients with stable CAD [29]. Increased UII concentrations have also been demonstrated in hypertension, which could be related to vasoconstrictive and pro-sympathetic effects. Animal studies demonstrated raised blood pressure and heart rate following UII injection which could be inhibited by pentolinium, indicating a direct contribution of the sympathetic nervous system [30, 31]. Another study revealed that intracerebral injection of UII induced elevated sympathetic nerve activity, which was followed by the stimulation of adrenal medulla for secretion of adrenaline [32].
Since UII has pro-atherosclerotic and vasoconstrictive effects especially in coronary resistance arteries, this particular action may have a role in SCF pathogenesis. Maguire and Davenport [33] reported UII expression in endothelial cells of both epicardial coronary arteries and intramyocardial resistance arteries (60–120 μm) but not in cardiac myocytes or vascular smooth muscle cells. Similarly, UII was detected within macrophages of the atherosclerotic plaque but not in vascular smooth muscle cells [34]. Moreover, urotensin receptors, which mediate vasoconstriction, are present in all vascular smooth muscle cells from large epicardial to small resistance arteries [35]. UII may have additional value in ischemia-reperfusion injury and thus aid in SCF phenomenon. In Langendorff, preparations for ischemia–reperfusion injury decrease coronary flow in rats, which is exacerbated by administration of UII during reperfusion [36]. Similarly, in the event of significant endothelial dysfunction, UII may cause vasoconstriction or inadequate vasodilation in coronary arteries with resultant myocardial ischemia [37, 38].
Maguire et al. [34] demonstrated that UII had more pronounced effect on small coronary arteries than epicardial vessels. This enhanced responsiveness may be important in atherosclerotic disorders such as SCF phenomenon.
Study Limitations
Our study has several limitations. First, the study population was relatively small. A larger study population would provide a higher statistical power. The main limitation of our study is the observational nature, which does not explain the exact mechanism of the relationship between increased UII and SCF. In this study, the patients did not undergo intravascular ultrasonography (IVUS) to detect atherosclerotic changes in the coronary arteries. Hence, the coexistence of non-obstructive CAD in patients with “isolated” SCF cannot be established absolutely. Nevertheless, in clinical practice, isolated SCF patients do not undergo IVUS routinely and SCF is usually diagnosed with visual assessment of coronary angiography. Other inflammatory cytokines, except CRP, might be measured to clarify possible causative mediators.
Conclusion
We demonstrated elevated UII levels in patients with SCF and revealed significant association of several atherosclerotic risk factors with SCF. Since UII is a marker of inflammation and atherosclerosis severity, elevated UII may confer an additional risk in this seemingly low-risk condition. Further studies are required to clarify this issue.
Authors’ contributions
ÖŞ and MED prepared the manuscript, MÇ and YÇ searched the literature, collected data, TE and HD made the analyses. All authors have read and approved the final form.
Conflict of interest
The authors declare that they have no conflict of interest.
Funding Statement
Funding sources: None.
References
- 1.Tambe AA, Demany MA, Zimmerman HA, Mascarenhas E: Angina pectoris and slow flow velocity of dye in coronary arteries – A new angiographic finding. Am Heart J 84, 66–71 (1972) [DOI] [PubMed] [Google Scholar]
- 2.Goel PK, Gupta SK, Agarwal A, Kapoor A: Slow coronary flow: A distinct angiographic subgroup in syndrome X. Angiology 52, 507–514 (2001) [DOI] [PubMed] [Google Scholar]
- 3.Mangieri E, Macchiarelli G, Ciavolella M, Barilla F, Avella A, Martinotti A, Dell'Italia LJ, Scibilia G, Motta P, Campa PP: Slow coronary flow: Clinical and histopathological features in patients with otherwise normal epicardial coronary arteries. Cathet Cardiovasc Diagn 37, 375–381 (1996) [DOI] [PubMed] [Google Scholar]
- 4.Cin VG, Pekdemir H, Camsar A, Cicek D, Akkuş MN, Parmaksız T, Katýrcýbaý T, Döven O: Diffuse intimal thickening of coronary arteries in slow coronary flow. Jpn Heart J 44, 907–919 (2003) [DOI] [PubMed] [Google Scholar]
- 5.Sezgin AT, Sığırcı A, Barutcu I, Topal E, Sezgin N, Ozdemir R, Yetkin E, Tandogan I, Kosar F, Ermis N, Yologlu S, Bariskaner E, Cehreli S: Vascular endothelial function in patients with slow coronary flow. Coron Artery Dis 14, 155–161 (2003) [DOI] [PubMed] [Google Scholar]
- 6.Rıza Erbay A, Turhan H, Yaşar AS, Ayaz S, Şahin O, Senen K, Sasmaz H, Yetkin E: Elevated level of plasma homocysteine in patients with slow coronary flow. Int J Cardiol 102, 419–423 (2005) [DOI] [PubMed] [Google Scholar]
- 7.Mosseri M, Yarom R, Gotsman MS, Hasin Y: Histologic evidence for small-vessel coronary artery disease in patients with angina pectoris and patent large coronary arteries. Circulation 74, 964–972 (1986) [DOI] [PubMed] [Google Scholar]
- 8.Fragasso G, Chierchia SL, Arioli F, Carandente O, Gerosa S, Carlino M, Palloshi A, Gianolli L, Calori G, Fazio F, Margonato A: Coronary slow-flow causing transient myocardial hypoperfusion in patients with cardiac syndrome X: Long-term clinical and functional prognosis. Int J Cardiol 137, 137–144 (2009) [DOI] [PubMed] [Google Scholar]
- 9.Matsushita M, Shichiri M, Fukai N, Ozawa N, Yoshimoto T, Takasu N, Hirata Y: Urotensin II is an autocrine/paracrine growth factor for the porcine renal epithelial cell line, LLCPK1. Endocrinology 144, 1825–1831 (2003) [DOI] [PubMed] [Google Scholar]
- 10.Cohen JD: Overview of physiology, vascular biology, and mechanisms of hypertension. J Manag Care Pharm 13, S6–S8 (2007) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kinoshita T, Asia T: Role of renin–angiotensin system inhibitors in patients undergoing off-pump coronary artery bypass grafting. Circ J 74, 1852–1858 (2010) [DOI] [PubMed] [Google Scholar]
- 12.Rakowski E, Hassan GS, Dhanak D, Ohlstein EH, Douglas SA, Giaid A: A role for urotensin II in restenosis following balloon angioplasty. J Mol Cell Cardiol 39, 789–791 (2005) [DOI] [PubMed] [Google Scholar]
- 13.Hassan GS, Douglas SA, Ohlstein EH, Giaid A: Expression of urotensin-II in human coronary atherosclerosis. Peptides 26, 2464–2472 (2005) [DOI] [PubMed] [Google Scholar]
- 14.Gibson CM, Cannon CP, Daley WL, Dodge JT, Jr, Alexander B, Jr, Marble SJ, McCabe CH, Raymond L, Fortin T, Poole WK, Braunwald E: TIMI frame count: A quantitative method of assessing coronary artery flow. Circulation 93, 879–888 (1996) [DOI] [PubMed] [Google Scholar]
- 15.Kurtoğlu N, Akcay A, Dindar I: Usefulness of oral dipyridamole therapy for angiographic slow coronary artery flow. Am J Cardiol 87, 777–779 (2001) [DOI] [PubMed] [Google Scholar]
- 16.De Bruyne B, Hersbach F, Pijls NH, Bartunek J, Bech JW, Heyndrickx GR, Gould KL, Wijns W: Abnormal epicardial coronary resistance in patients with diffuse atherosclerosis but “Normal” coronary angiography. Circulation 104, 2401–2406 (2001) [DOI] [PubMed] [Google Scholar]
- 17.Li JJ, Xu B, Li ZC, Qian J, Wei BQ: Is slow coronary flow associated with inflammation? Med Hypotheses 66, 504–508 (2006) [DOI] [PubMed] [Google Scholar]
- 18.Turhan H, Saydam GS, Erbay AR, Ayaz S, Yaşar AS, Aksoy Y, Basar N, Yetkin E: Increased plasma soluble adhesion molecules; ICAM-1, VCAM-1, and E-selectin levels in patients with slow coronary flow. Int J Cardiol 108, 224–230 (2006) [DOI] [PubMed] [Google Scholar]
- 19.Lanza GA, Andreotti F, Sestito A, Sciahbasi A, Crea F, Maseri A: Platelet aggregability in cardiac syndrome X. Eur Heart J 22, 1924–1930 (2001) [DOI] [PubMed] [Google Scholar]
- 20.Gokce M, Kaplan S, Tekelioğlu Y, Erdoğan T, Kucukosmanoğlu M: Platelet function disorder in patients with coronary slow flow. Clin Cardiol 28, 145–148 (2005) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Camsarı A, Pekdemir H, Cicek D, Polat G, Akkuş MN, Doven O, Cin VG, Katlrclbasl T, Parmakslz T: Endothelin-1 and nitric oxide concentrations and their response to exercise in patients with slow coronary flow. Circ J 67, 1022–1028 (2003) [DOI] [PubMed] [Google Scholar]
- 22.Yıldız A, Gur M, Yılmaz R, Demirbağ R, Polat M, Selek S, Celik H, Erel O: Association of paraoxonase activity and coronary blood flow. Atherosclerosis 197, 257–263 (2008) [DOI] [PubMed] [Google Scholar]
- 23.Enli Y, Turk M, Akbay R, Evrengul H, Tanrıverdi H, Kuru O, Seleci D, Kaftan A, Ozer O, Enli H: Oxidative stress parameters in patients with slow coronary flow. Adv Ther 25, 37–44 (2008) [DOI] [PubMed] [Google Scholar]
- 24.Kopetz V, Kennedy J, Heresztyn T, Stafford I, Willoughby SR, Beltrame JF: Endothelial function, oxidative stress and inflammatory studies in chronic coronary slow flow phenomenon patients. Cardiology 121, 197–203 (2012) [DOI] [PubMed] [Google Scholar]
- 25.Iglewski M, Grant SR: Urotensin II-induced signaling involved in proliferation of vascular smooth muscle cells. Vasc Health Risk Manag 6, 723–734 (2010) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Song N, Ding W, Chu S, Zhao J, Dong X, Di B, Tang C: Urotensin II stimulates vascular endothelial growth factor secretion from adventitial fibroblasts in synergy with angiotensin II. Circ J 76, 1267–1273 (2012) [DOI] [PubMed] [Google Scholar]
- 27.Watanabe T, Arita S, Shiraishi Y, Suguro T, Sakai T, Hongo S, Miyazaki A: Human urotensin II promotes hypertension and atherosclerotic cardiovascular diseases. Curr Med Chem 16, 550–563 (2009) [DOI] [PubMed] [Google Scholar]
- 28.Hassan GS, Douglas SA, Ohlstein EH, Giaid A: Expression of urotensin-II in human coronary atherosclerosis. Peptides 26, 2464–2472 (2005) [DOI] [PubMed] [Google Scholar]
- 29.Heringlake M, Kox T, Uzun O, Will B, Bahlmann L, Klaus S, Eleftheriadis S, Armbruster FP, Franz N, Kraatz E: The relationship between urotensin II plasma immunoreactivity and left ventricular filling pressures in coronary artery disease. Regul Pept 121, 129–136 (2004) [DOI] [PubMed] [Google Scholar]
- 30.Lin Y, Tsuchihashi T, Matsumura K, Abe I, Iida M: Central cardiovascular action of urotensin II in conscious rats. J Hypertens 21, 159–165 (2003) [DOI] [PubMed] [Google Scholar]
- 31.Lin Y, Tsuchihashi T, Matsumura K, Fukuhara M, Ohya Y, Fujii K, Iida M: Central cardiovascular action of urotensin II in spontaneously hypertensive rats. Hypertens Res 26, 839–845 (2003) [DOI] [PubMed] [Google Scholar]
- 32.Lu Y, Zou CJ, Huang DW, Tang CS: Cardiovascular effects of urotensin II in different brain areas. Peptides 23, 1631–1635 (2002) [DOI] [PubMed] [Google Scholar]
- 33.Maguire JJ, Davenport AP: Is urotensin-II the new endothelin? Br J Pharmacol 137, 579–588 (2002) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Maguire JJ, Kuc RE, Wiley KE, Kleinz MJ, Davenport AP: Cellular distribution of immunoreactive urotensin-II in human tissues with evidence of increased expression in atherosclerosis and a greater constrictor response of small compared to large coronary arteries. Peptides 25, 1767–1774 (2004) [DOI] [PubMed] [Google Scholar]
- 35.Douglas SA, Sulpizio AC, Piercy V, Sarau HM, Ames RS, Aiyar NV, Ohlstein EH, Willette RN: Differential vasoconstrictor activity of human urotensin-II in vascular tissue isolated from the rat, mouse, dog, pig, marmoset and cynomolgus monkey. Br J Pharmacol 131, 1262–1274 (2000) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Russell FD, Molenaar P: Investigation of signaling pathways that mediate the inotropic effect of urotensin-II in human heart. Cardiovasc Res 63, 673–681 (2004) [DOI] [PubMed] [Google Scholar]
- 37.Zhou P, Wu SY, Yu CF, Wang H, Tang CS, Lin L, Yuan WJ: Effects of urotensin II on isolated rat hearts under normal perfusion and ischemia reperfusion. Acta Physiol Sin 55, 442–448 (2003) [PubMed] [Google Scholar]
- 38.Paysant J, Rupin A, Simonet S, Fabiani JN, Verbeuren TJ: Comparison of the contractile responses of human coronary bypass grafts and monkey arteries to human urotensin-II. Fundam Clin Pharmacol 15, 227–231 (2001) [DOI] [PubMed] [Google Scholar]