Abstract
A 72-year-old woman was admitted to our hospital with a solitary right lung nodule. She had no symptoms and no abnormal physical findings except for bladder cancer. Tumor markers were mildly elevated but no other abnormal laboratory data were found. The nodule was diagnosed to be pulmonary mucosa-associated lymphoid tissue lymphoma on computed tomography-guided needle biopsy. Thereafter, she first underwent surgery for bladder cancer. The lung nodule was found to have slightly increased at three months and then disappeared at 15 months after the biopsy. The notable clinical course of this rare disease suggests the effectiveness of a non-interventional treatment strategy.
Keywords: mucosa-associated lymphoid tissue lymphoma, spontaneous regression, computed tomography-guided needle biopsy
Introduction
Mucosa-associated lymphoid tissue (MALT) lymphomas occur frequently in the stomach and rarely in the lungs. The prevalence rate of pulmonary MALT lymphoma accounts for approximately 0.3-0.45% of all lung malignant tumors (1). Prospective trials have not so far been conducted for analyzing the appropriate treatment of pulmonary MALT lymphomas because the number of cases is extremely small. Therefore, no optimal treatment modality for this disease has yet been established (2). In general, localized tumors have been treated by surgical resection or radiation therapy and extended tumors have been treated by systemic chemotherapy (3). Therefore, little is known about the progressive course of untreated pulmonary MALT lymphomas. In general, pulmonary MALT lymphomas tend to progress indolently and have favorable outcomes (2); however, the spontaneous regression of this disease is very rare.
We herein report an unusual case of a localized pulmonary MALT lymphoma that disappeared spontaneously after the patient underwent a percutaneous needle biopsy and bladder cancer surgery.
Although conducting future clinical trials for the treatment of this disease will be difficult, if similar series of case reports are eventually accumulated, then the observation of pulmonary MALT lymphoma may be one of the recommended therapeutic choices.
Case Report
A 72-year-old woman with an abnormal shadow of the right lung and no symptoms presented to our hospital. The patient had a past history of chronic gastritis, surgery for a uterine myoma, and fever and diarrhea after the ingestion of sho-saiko-to. She had a 20-pack-year history of smoking and had no unusual family history. She had repeatedly undergone transurethral resections of bladder tumors (TUR-BT) for 15 years, and a total cystectomy with an ileal conduit was planned because a cancerous tumor had progressed. Before the operation, chest computed tomography (CT) was taken, and it revealed a solitary nodule in the right lower lobe of the lung. The lung nodule had remained undiagnosed by bronchofiberoscopy at her previous hospital, and she was thus referred to our hospital for diagnosis.
Physical examination showed no findings except for a surgical scar on the abdomen. Laboratory investigation revealed that carcinoembryonic antigen (CEA) was 5.8 ng/mL (normal: ≤3.4 ng/mL) and cytokeratin 19 fragment (CYFRA) was 3.8 ng/mL (normal: ≤3.5 ng/mL). Lactate dehydrogenase (LDH) and soluble interleukin-2 receptor were within the normal ranges. β-D glucan and fungal antigens were normal. A chest X-ray and chest CT showed a nodule measuring 12-mm diameter localized in the right lower lobe (Figure 1A, 2A). We performed a CT-guided needle biopsy of the nodule.
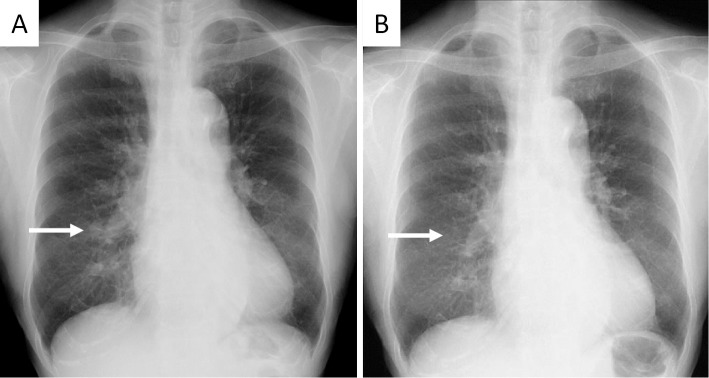
Figure 1.
A: Chest X-ray shows a nodule in the right lower lung (arrow). B: Nine months after performing a biopsy, the nodule has become vague (arrow).
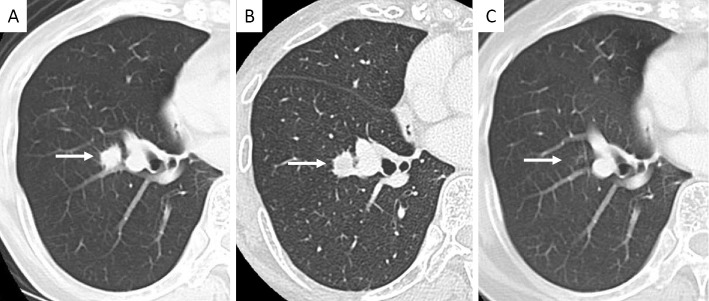
Figure 2.
A: Chest computed tomography showed a solitary nodule (12 mm in diameter) in the right lower lobe just before undergoing biopsy (arrow). B: Three months after the biopsy, the diameter of the nodule has slightly increased (arrow). C: Fifteen months after the biopsy, the nodule has disappeared (arrow).
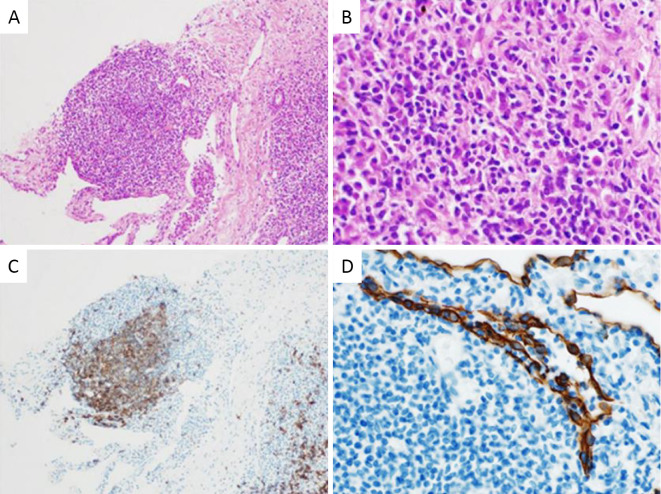
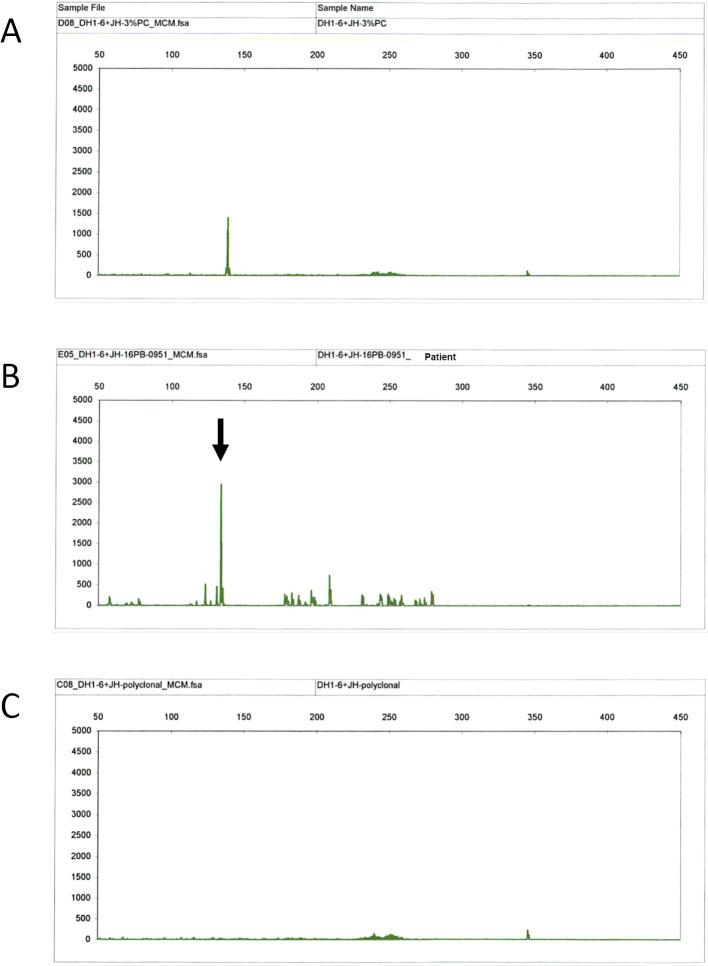
Histological examination with Hematoxylin and Eosin (H&E) staining showed the proliferation of small lymphocytes with little atypia (Fig. 3A and B). Immunohistochemical staining proved that most of the cells in the lymphatic follicles were clusters of differentiation (CD) 20 positive (Fig. 3C). Immunostaining of cytokeratin confirmed the presence of a lympho-epithelial lesion (LEL), which indicated the infiltration of lymphocytes into the epithelium of the gland duct (Fig. 3D). In addition, we performed molecular analyses to evaluate the clonality of the tumor using paraffin-embedded tissue specimens. We detected the gene rearrangement of the immunoglobulin heavy chain (IGH) DH1-6-JH by polymerase chain reaction (Fig. 4), although we did not detect the API2/MALT1 fusion gene by fluorescence in situ hybridization (FISH) and the monoclonal distribution of kappa/lambda light chains by in situ hybridization (ISH). According to these findings, we diagnosed the nodule to be pulmonary MALT lymphoma.
Figure 3.
A: Histological examinations showed an accumulation of small lymphoid cells [Hematoxylin and Eosin (H&E) staining, ×40]. B: Lymphoid cells consist of atypical small lymphocytes (H&E staining, ×200). C: Cells in the lymphatic follicle include clusters of differentiation (CD) 20 positive (CD20 stain, ×40). D: Infiltration of lymphoid cells into the epithelium, defined as lympho-epithelial lesion (LEL) (Cytokeratin stain, ×200).
Figure 4.
GeneScan results of polymerase chain reaction products of the biopsied sample showing the gene rearrangement of the immunoglobulin heavy chain DH1-6-JH. The x-axes represent the molecular size (base pairs), and the y-axes represent the fluorescence intensity. A: Positive control of the peak of DH1-6-JH. B: DH1-6-JH gene products of the tumor (arrow) showing a higher peak than the positive control (A). C: Polyclonal control.
As the lymphoma was localized and the patient was asymptomatic, bladder cancer surgery was initially performed, and we observed the progress of the lymphoma by imaging until the patient had recovered from surgery. The solitary lung nodule increased slightly on the CT image at three months after the biopsy (Fig. 2B), but subsequently became unclear on a chest X-ray nine months after the biopsy (Fig. 1B), and then it completely disappeared on the CT image 15 months after the biopsy (Fig. 2C). To date, no recurrence has been found either in the lung or at any other sites as of 40 months after the initial biopsy.
Discussion
MALT lymphomas were initially suggested by Isaacson and Wright in 1983 (4) and described in the World Health Organization classification of tumors of hematopoietic and lymphoid tissues as an extranodal marginal zone B-cell lymphoma of the MALT type, which is a type of low-grade extranodal lymphoma (5). MALT lymphoma most frequently arises from the stomach, and it can involve the small intestine, salivary gland, lung, head and neck, ocular adnexa, skin, thyroid, and breast (5). Helicobacter pylori infection has been proved to be a potential cause of gastric MALT lymphoma, and the eradication of the pathogen could resolve the tumor (6). However, the etiology of pulmonary MALT lymphomas remains to be elucidated.
The prevalence of pulmonary MALT lymphoma is very small; Kurtin reported that among the 10,046 new diagnoses of non-Hogkin lymphoma, 106 (1.1%) originated from the lung and 50 (0.5%) of such cases were pulmonary MALT lymphomas (7). Pulmonary MALT lymphomas present with the following pathologic features: intraparenchymal masses composed of centrocyte-like cells, plasmacytoid lymphocytes and plasma cells that form LEL, the infiltration of neoplastic lymphocytes into the bronchial or bronchiolar epithelium, and a lymphangitic growth pattern (7). Because pulmonary MALT lymphoma is difficult to diagnose from small lung specimens, the diagnosis is often made by lung surgery that also serves as therapy for the localized disease (1). In fact, the proportion of patients who were diagnosed as having lymphoma by transbronchial biopsy or radiologically-guided transthoracic core-needle biopsy is only one-third, while the remaining two-thirds required video-assisted thoracoscopic surgery or thoracotomy to achieve definitive diagnoses (3). In the present case, using needle-biopsied specimens, pulmonary MALT lymphoma was diagnosed based on the histological proliferation of small lymphocytes with little atypia, the infiltration of CD20-positive cells in the lymphatic follicles, LEL, and the identification of the gene rearrangement of IGH DH1-6-JH.
Everson and Cole defined the spontaneous regression of cancer as the partial or complete disappearance of a malignant tumor in the absence of therapy which is considered to exert an influence on neoplastic diseases (8), and indicated the frequency of occurrence was one in 60,000-100,000 cases of cancer. Among a total of 741 cases of spontaneous cancer regression originating from various organs, the patients with cancer originating in the lung consisted of 23 cases [3.1% (8-10)]. The mechanism of spontaneous regression is unknown, however, several of these regressions occurred after invasive procedures such as biopsies, or after complications with bacterial infection (11, 12); some may have activated immune reactions, which might have contributed to the resolution of the disease. Cole. showed that 71 (41%) cases of 176 spontaneous regressions were associated with surgery or surgical trauma (11). In the present case, stimulation by needle biopsy may have directly triggered a regional immune reaction or the trauma due to the bladder surgery may have activated the patient's systemic immunity, which could have led to tumor remission.
The first report of spontaneous regression of pulmonary MALT lymphomas was presented by Troch et al (13). In that report, six of 11 patients with non-treated pulmonary MALT lymphomas showed spontaneous regression, but not complete remission, during an observation period with a median of 28 months (13). In some patients from that study, this phenomenon was only seen in the lung, while extrapulmonary lesions did not change significantly. These facts indicate that the circumstances of lung tissue surrounding the tumor or the nature of the lymphoma originating from lung might be distinct from those of other sites. In addition, three out of six patients with spontaneous regression have at least one episode of tumor increase before regression (13). These courses were similar to that of the present case. A possible mechanism of the change in tumor size was the fact that the tumor initially increased in size after the invasive biopsy and healed after activation of the immune system. Sato et al. described a pulmonary MALT lymphoma of an 82-year-old man that regressed spontaneously after a bronchoscopic biopsy and had not relapsed during a 20-month period (14). Recently, Kang et al. described a 57-year-old woman with spontaneously disappeared pulmonary MALT lymphoma after thoracoscopic lung biopsy, although the lymphoma remained in her bone marrow (15). We summarized the clinical characteristics of these eight cases of pulmonary MALT lymphomas with spontaneous regression as well as the present case (Table). All cases were diagnosed by invasive procedure: endobronchial biopsy, CT-guided needle biopsy, or surgical biopsy (details of all patients are not known). The present case was a patient with a higher age and localized disease in a unilateral lung, which completely disappeared after the trauma induced by the CT-guided needle biopsy and bladder cancer surgery.
Table.
Summary of 8 Reported Cases and the Present Case of Pulmonary Mucosa-associated Lymphoid Tissue Lymphoma with Spontaneously Regression.
| 8 reported cases * | The present case | |
|---|---|---|
| Age (years) | Median 55 (range 42-82) | 72 |
| Gender | Male 2, Female 6 | Female |
| Bilateral/unilateral lung lesion | Bilateral 3, Unilateral 5 | Unilateral |
| Extra-pulmonary organ involvement | Yes 4, No 4 | No |
| Autoimmune disease coincidence | Sjögren's syndrome 2, None 6 | None |
| Degree of regression | Complete 2, Incomplete 6 | Complete |
* References (13–15)
The prognostic factors of pulmonary MALT lymphoma other than lymphoma-specific therapy were indicated in the past studies. Patients whose lymphomas with LEL had better outcomes than those without LEL, and patients with amyloid-containing tumors showed a poorer prognosis than those without amyloid (7). The present case identified LEL, but not amyloid deposition in the biopsied lung specimens.
We herein reported a rare case of pulmonary MALT lymphoma that showed spontaneous regression, which completely disappeared after a CT-guided needle biopsy. When pulmonary MALT lymphoma is asymptomatic and not progressive, observation without immediate therapy should therefore be considered as a treatment option until the lymphoma size increases. In order to determine the appropriate management for pulmonary MALT lymphoma, more information concerning the progressive course of this disease should be obtained.
The authors state that they have no Conflict of Interest (COI).
References
- 1. Ferraro P, Trastek VF, Adlakha H, Deschamps C, Allen MS, Pairolero PC. Primary non-Hodgkin's lymphoma of the lung. Ann Thorac Surg 69: 993-997, 2000. [DOI] [PubMed] [Google Scholar]
- 2. Borie R, Wislez M, Thabut G, et al. . Clinical characteristics and prognostic factors of pulmonary MALT lymphoma. Eur Respir J 34: 1408-1416, 2009. [DOI] [PubMed] [Google Scholar]
- 3. Ahmed S, Kussick SJ, Siddiqui AK, et al. . Bronchial-associated lymphoid tissue lymphoma: a clinical study of a rare disease. Eur J Cancer 40: 1320-1326, 2004. [DOI] [PubMed] [Google Scholar]
- 4. Isaacson PG, Wright DH. Malignant lymphoma of mucosa-associated lymphoid tissue. A distinctive type of B-cell lymphoma. Cancer 52: 1410-1416, 1983. [DOI] [PubMed] [Google Scholar]
- 5. Swerdlow SH, Campo E, Harris NL, et al. In: WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues. IARC Press, Lyon, France, 2008. [Google Scholar]
- 6. Wotherspoon AC, Doglioni C, Diss TC, et al. . Regression of primary low-grade B-cell gastric lymphoma of mucosa-associated lymphoid tissue type after eradication of Helicobacter pylori. Lancet 342: 575-577, 1993. [DOI] [PubMed] [Google Scholar]
- 7. Kurtin PJ, Myers JL, Adlakha H, et al. . Pathologic and clinical features of primary pulmonary extranodal marginal zone B-cell lymphoma of MALT type. Am J Surg Pathol 25: 997-1008, 2001. [DOI] [PubMed] [Google Scholar]
- 8. Everson TC, Cole WH In: Spontaneous Regression of Cancer: A Study and Abstract of Reports in the World Medical Literature and of Personal Communications Concerning Spontaneous Regression of Malignant Disease. WB Saunders Com., Philadelphia, 1966: 3-10. [Google Scholar]
- 9. Boyd W. In: The Spontaneous Regression of Cancer. Charles C Thomas, Springfield, 1966. [Google Scholar]
- 10. Challis GB, Stam HJ. The spontaneous regression of cancer. A review of cases from 1900 to 1987. Acta Oncologica 29: 545-550, 1990. [DOI] [PubMed] [Google Scholar]
- 11. Cole WH. Efforts to explain spontaneous regression of cancer. J Surg Oncol 17: 201-209, 1981. [DOI] [PubMed] [Google Scholar]
- 12. Horino T, Takao T, Yamamoto M, Geshi T, Hashimoto K. Spontaneous remission of small cell lung cancer: a case report and review in the literature. Lung Cancer 53: 249-252, 2006. [DOI] [PubMed] [Google Scholar]
- 13. Troch M, Streubel B, Petkov V, Turetschek K, Chott A, Raderer M. Does MALT lymphoma of the lung require immediate treatment? An analysis of 11 untreated cases with long-term follow-up. Anticancer Res 27: 3633-3637, 2007. [PubMed] [Google Scholar]
- 14. Sato C, Suzuki H, Watanabe M, Kojima K, Tsuchida F, Takeda H. Spontaneous regression of mucosa-associated lymphoid tissue lymphoma of the lung. Nihon Kokyuki Gakkai Zasshi 48: 677-682, 2010. (in Japanese, Abstract in English). [PubMed] [Google Scholar]
- 15. Kang HS, Lee HY, Kim SJ, et al. . An unusual presentation of pulmonary mucosa-associated lymphoid tissue lymphoma as diffuse pulmonary infiltrates with spontaneous regression. Cancer Res Treat 47: 943-948, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]