Abstract
Introduction
The value of simulation in medical education and procedural skills training is well recognized. Despite this, many mannequin-based trainers are limited by the inability of the trainee to view the internal anatomical structures. This study evaluates the usability and feasibility of a 1st person point of view (POV) augmented reality (AR) trainer on needle insertion as a component of central venous catheter (CVC) placement.
Methods
Forty subjects, including medical students and anesthesiology residents and faculty participated. AR glasses were provided through which the relevant internal anatomical landmarks were projected. Following a practice period, participants were asked to place the needle in the mannequin without the benefit of the AR projected internal anatomy. The ability of the trainees to correctly place the needle was documented. Participants also completed a short survey describing their perceptions of the AR technology.
Results
Participants reported that the AR technology was realistic (77.5%) and that the ability to view the internal anatomy was helpful (92.5%). Furthermore, 85% and 82.1%, respectively, believed that the AR technology promoted learning and should be incorporated into medical training. The ability to successfully place the needle was similar between experienced and non-experienced participants, however, less experienced participants were more likely to inadvertently puncture the carotid artery.
Conclusions
Results of this pilot study demonstrated the usability and feasibility of AR technology as a potentially important adjunct to simulated medical skills training. Further development and evaluation of this innovative technology under a variety of simulated medical training settings would be an important next step.
Introduction
Despite the widespread adoption of patient simulation training and the evidence to support its value in medical education, 1,2 current patient simulators typically lack the ability of trainees to identify important internal landmarks and anatomy. However, current technological advancements are providing new modalities for simulation-based training to address this deficiency. One such promising approach is Augmented Reality (AR) which is created by combining real and virtual data with real time interactivity and 3-dimensional registration.3 An Augmented Reality environment consists of 3-D images or animations that can be displayed in the same field of view as real objects, providing an enhanced but realistic view. AR differs from Virtual Reality (VR) in that the user interaction provides a more realistic environment compared to a virtual one.4 This results from the fact that some of the viewed objects are real and some are virtual, leading to the closely related term “mixed reality” Using this approach, the trainee wears virtual reality goggles that project internal structures onto a mannequin. The goggles contain visual sensors that detect markers that are placed on the mannequin. This provides an input by which the internal anatomy is constantly displayed within the field of view of the mannequin, creating an ongoing illusion combined with a real object i.e. the mannequin. An object such as a needle can also be tagged with a marker that then can be sensed by the goggles, allowing a virtual needle to be generated with the environment. The procedure is performed as it would in routine mannequin based simulation, but with the addition of the AR generated by the goggles which allows the trainee to place the needle within the mannequin while viewing its interaction with the internal anatomy in real time. The technology also alerts the trainees in real-time with respect to complications (e.g., bleeding) or procedural errors.
Preliminary studies involving AR suggest that this technology may be effective in teaching a number of different clinical procedural skills.5,6 However, a recent review of available AR applications by Barsom et al. revealed that although use of this technology is gaining interest, data are still lacking to support its’ overall applicability and effectiveness.4 These authors however, suggest that if there is sufficient evidence to support its’ integration into medical training, AR could soon play a large role in medical education. This review highlighted that categories of current AR applications were limited to the disciplines of laparoscopy, neurosurgery and echocardiography. Only one report of use of AR in central venous catheter (CVC) insertion was identified. This study performed by Jeon et al. used ultra-sound enhanced imaging to assist in the AR imaging. The primary limitation of this study was that the ultrasound model used was a vascular phantom, and thus lacked the capacity to project true human anatomy.7
Previous development of AR technology has relied on what is termed 3rd person point of view (POV) in which the virtual anatomical images and procedure (performed by a trainer) are projected onto a remote screen that can be viewed by the trainees. While this approach facilitates group learning, the passive nature precludes individual “hands-on” participation. To obviate this limitation, we have developed a 1st person POV approach in which the individual trainee is able to visualize a stereoscopic virtual image of the anatomy in real-time through use of the augmented reality glasses or goggles. This approach thus enables seamless integration into individualized rather than group medical training. Although early iterations of AR goggles were limited by issues related to a lack of depth perception and slow refresh rates, recent advances in optical see-through AR glasses and goggles have largely overcome these early problems.
For the purposes of this study, we evaluated the usability and feasibility of a 1st person POV augmented reality application on the ability of participants with varying levels of clinical experience to correctly place a CVC in the right internal jugular vein (RIJ) of an AR capable mannequin.
Methods
This project was deemed exempt by the University of Michigan Medical School’s Institutional Review Board.
Prototype development
Using medical textbooks, the extant literature and expert opinion, graphic artists create 3-dimensional computer image models of the anatomical structures e.g., clavicle, sternocleidomastoid muscle, jugular vein, etc. The 3D image models are then manipulated using Unity® Game Engine and Vuforia® to render, scale and register the computer images virtual graphics on the mannequin. Given that CVC placement requires insertion of a flexible object (needle); rigid-body tracking cannot be used. Instead, flexible instruments are augmented with small infrared reflective markers which are detected by an infrared-seeing camera mounted at a fixed pose relative to the mannequin. (Figure 1) Video streams captured by the camera are processed to develop a statistical model representing the needle and its insertion into the mannequin. In each camera frame, pixels belonging to the infrared reflective markers are extracted by simple thresholding (on the basis of pixel intensities, infrared markers being brighter than other objects). Thus, by running an optical flow algorithm on the current and previous frames’ feature sets; an estimate of the motion of the needle is calculated. The AR glasses used in this study were Epson Moverio BT-200® Smart Glasses (Epson America, Inc., Long Beach, CA) that allowed for 1st person POV stereoscopic imaging.
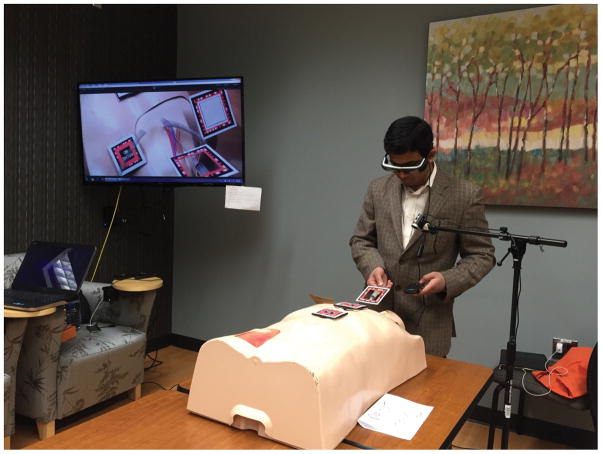
Figure 1.
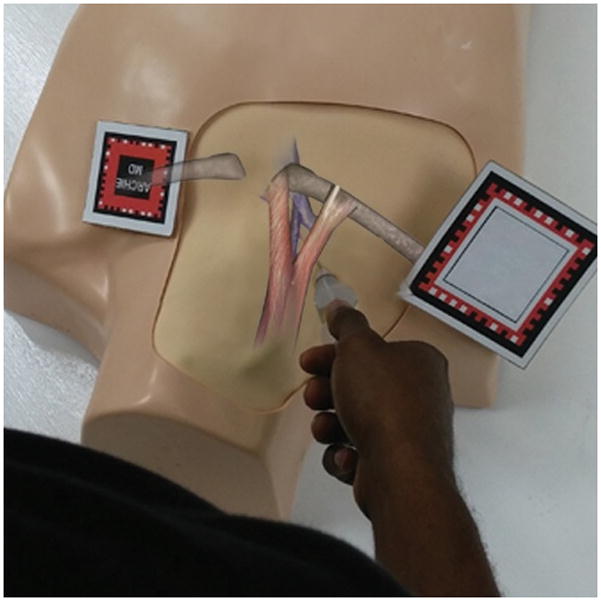
The trainee’s view of the internal anatomy as seen through the augmented reality glasses (1st person POV).
Participants
The study population included third and fourth-year medical students attending the University of Michigan’s Medical School (UMMS) together with residents, fellows, faculty and nurse anesthetists from the Department of Anesthesiology. Participants were identified through UMMS e-mail listings and face-to-face recruitment. Participants were guaranteed that performance in this project would have no effect on clinical evaluations.
Medical student participants and those with limited experience with CVC placement watched a brief video explaining the 1st person POV AR technology and what the testing would entail. All other participants received the same information verbally by two of the authors (LR, AT) based on their level of experience. Following the video or introduction, participants were then individually guided through an identical sequence of events using the AR trainer. The AR glasses were adjusted and tested to ensure comfort and visual accuracy. Participants were asked to locate the clavicle and the two heads of the sternocleidomastoid muscle by palpation. Once identified correctly, the internal anatomy was projected through the glasses and simultaneously on the accompanying television screen. The triangle formed by the sternocleidomastoid muscle and clavicle was highlighted, revealing the apex of the triangle as the target for needle insertion. Following identification of the apex, the internal jugular vein and internal carotid artery appeared, allowing for appreciation of their position relative to the previously identified anatomy. Each participant was then asked to practice needle insertion using the AR-adapted needle and with the anatomy in view. Once the participant felt confident with their technique, they were then asked to insert the needle without the anatomy in view. If the needle was inserted correctly into the vein, the needle turned red to simulate blood return and the anatomy was revealed to confirm correct placement. If the carotid artery was inadvertently punctured, the anatomy would be revealed with an expanding hematoma. Participants not being tested were able to watch from a 3rd person POV on a television screen (Figure 2).
Figure 2.
Trainee attempting central venous catheter placement on the mannequin. The trainee’s view of the projected internal anatomy is seen on the remote TV screen (3rd person POV).
Two trained raters (LR, AT) independently documented performance via an assessment (see Document, Supplemental Digital Content 1, participant assessment) checklist created in an online survey software tool (Qualtrics, Provo, UT). The checklist items reflected each step of the procedure and were dichotomous (yes/no) indicating that the participant had either correctly performed each task or had not. The primary tasks that were evaluated for completion were correct identification of anatomy, correct needle insertion angle and direction, and maintenance of the needle within the vein.8 Total time from participant start to finish as well as time to needle insertion and advancement in the RIJ vein without AR assistance were recorded.
At the conclusion of the procedure, participants completed a survey (see Document, Supplemental Digital Content 2, participant evaluation) to elicit information about their level of training, prior experience with CVC line placement, satisfaction with the AR technology, and perceptions of AR as a potential teaching tool for medical skills training. The participants were also surveyed to determine their likes and dislikes, potential barriers to successful adoption of AR technology, and any suggestions for improvement.
Statistical analysis
Data from Qualtrics were downloaded directly to SPSS version 21.0 (IBM Inc., New York, NY) for analysis. Quantitative data were analyzed using descriptive statistics; correlations between questions were assessed using chi-square or Fisher exact tests as appropriate. Inter-rater agreements between assessors’ scores were performed on approximately 40% of the population using the kappa (κ) statistic for all the items tested. Kappa values of ≥0.7 were considered acceptable. Results ranged from 0.77–1.0. Data are mean ± SD and n (%). A p-value of <0.05 was considered statistically significant. Open ended questions and free-text responses were qualitatively evaluated for repeated themes and concepts that would be used for analysis.
Sample size
This was a Phase I pilot study for determination of usability and feasibility, thus no formal power analysis sample size was required.
Results
A total of 40 participants with varied levels of experience were included. Demographics of the study sample are described in Table 1. Prior experience and training with central line placement and training are shown in Table 2. Less than half of the participants had received prior simulation-based training in CVC insertion. None of the medical students had prior experience with central line placement. All of those who had previously placed a CVC had only done so in the internal jugular location.
Table 1.
Participant demographics.
| Level of Training | n (%), N = 40 |
|---|---|
| M3(7)/M4(13) | 20 (50.0) |
| Intern (PGY-1) | 5 (12.5) |
| Resident (PGY-2 – PGY-4) | 5 (12.5) |
| Fellow | 1 (2.5) |
| CRNA | 2 (5.0) |
| Faculty | 6 (15.0) |
| Other (Anesthesia technician) | 1 (2.5) |
M = Medical student; PGY = Residency Postgraduate year; CRNA = Certified registered nurse anesthetist
Table 2.
Experience with CVC Training and Insertion
| Experience | n/N (%) |
|---|---|
| Prior CVC training (Yes) | 27/40 (67.5) |
| If prior CVC training: | |
| With simulator-Yes? | 12/27 (44.4) |
| Simulator type: | |
| Partial mannequin with ultrasound | 10/12 (83.3) |
| Multiple types | 2/12 (16.7) |
| Prior CVC insertions: | |
| None | 24/40 (60.0) |
| 1–5 | 5/40 (12.5) |
| 6–10 | 0/40 (0.0) |
| 11–20 | 1/40 (2.5) |
| >20 | 10/40 (25.0) |
| Location of prior CVC insertions: | |
| Internal jugular | 16/16 (100.0) |
CVC = Central venous catheterization
Overall, participants reported that the AR technology was realistic, easy to use, and would be a useful adjunct to current training (Table 3). Comparisons of the perceptions of the AR technology between individuals with and without prior CVC training revealed very similar findings. For example, compared with participants with no prior CVC training, those with prior CVC experience reported that the AR technology: helped them identify the anatomical landmarks (84.6% vs 88.9%, respectively); was fun to use (76.9% vs 77.8%); would improve their skills (76.9% vs 66.7%); promoted learning (84.6% vs 85.2%), and; would be useful in their medical skills training (84.6% vs 85.2%). Of those with prior training in CVC placement 59.3% reported that the AR technology was superior compared to other methods of simulated procedural skills training.
Table 3.
1st. Person Point of View Augmented Reality Trainer: Participant Evaluation
| Strongly disagree/disagree | Neither disagree nor agree | Agree/strongly agree | |
|---|---|---|---|
| AR anatomy was realistic | 5 (12.5) | 4 (10.0) | 31 (77.5) |
| AR helped identify anatomy | 2 (5.0) | 3 (7.5) | 35 (87.5) |
| Ability to view anatomy was helpful | 2 (5.0) | 1 (2.5) | 37 (92.5) |
| AR was easy to use | 6 (15.0) | 10 (25.0) | 24 (60.0) |
| AR was enjoyable | 3 (7.5) | 6 (15.0) | 31 (77.5) |
| AR will improve my CVC skills | 2 (5.0) | 10 (25.0) | 28 (70.0) |
| AR features support learning | 0 (0.0) | 6 (15.0) | 34 (85.0) |
| AR interactivity promotes learning | 2 (5.0) | 4 (10.0) | 34 (85.0) |
| AR novel features promote learning | 1 (2.5) | 4 (10.0) | 35 (87.5) |
| AR useful in my medical skills training | 2 (5.0) | 4 (10.0) | 34 (85.0) |
| Incorporate AR into medical training | 2 (5.1) | 5 (12.8) | 32 (82.1) |
AR = 1st person point of view Augmented Reality
CVC = Central venous catheterization
Evaluation of CVC insertion milestones adjusted for experience reveals that all participants were able to correctly identify the required anatomy and place the needle (Table 4). However, those with no prior training were significantly more likely to inadvertently puncture the carotid artery during the testing phase. The results in this table describe achievements by the participants without using the AR projection followed by confirmation of achievement with the AR technology.
Table 4.
Competency achievements by experience
| No Prior CVC Training (n = 13) | Prior CVC Training (n = 27) | Overall (N = 40) | |
|---|---|---|---|
| Correct identification of: | |||
| Clavicle | 13 (100.0) | 27 (100.0) | 40 (100.0) |
| Heads of Sternocleidomastoid | 13 (100.0) | 26 (96.3) | 39 (97.5) |
| Apex of triangle | 12 (92.3) | 26 (96.3) | 38 (95.0) |
| Correct: | |||
| Needle insertion site | 13 (100.0) | 24 (88.9) | 37 (92.5) |
| Insertion direction | 11 (84.6) | 26 (96.3) | 37 (92.5) |
| Insertion angle | 4 (30.8) | 13 (48.1) | 17 (42.5) |
| Vein cannulation | 10 (76.9) | 26 (96.3) | 36 (90.0) |
| Needle remained stable in vein | 9 (69.2) | 25 (92.6) | 34 (85.0) |
| Carotid puncture | 4 (30.8) | 1 (3.7)* | 5 (12.5) |
| Times (secs) from: | |||
| Identification of anatomy to vein cannulation | 152.3 ± 78.2 | 141.1 ± 41.6 | 144.9 ± 55.7 |
| Needle insertion to vein cannulation | 48.88 ±49.6 | 37.42 ±17.9 | 41.24 ± 31.9 |
CVC = Central venous catheterization
Data are n (%),
P< 0.05 vs no prior CVC training
Open-ended comments regarding the participants’ positive and negative impressions of the augmented reality prototype and its potential as a training tool for medical procedures were recorded and sorted by themes using standard qualitative techniques (e.g., proofreading, identifying repetitions, indigenous categories, and similarities/differences).9 Positive comments were primarily related to the ability to visualize the internal structures and anatomy in 3 dimensions (26/39 responses = 69.2%). Seven (17.9%) participants combined positive remarks regarding the interactive nature of the prototype and the observation that it was a fun and novel way to learn a procedure. A sample of positive comments is provided verbatim.
“Ability to see overlying anatomical structures as the procedure is in process”
“As a total beginner when it comes to CVC insertion, it was really helpful to visualize the internal anatomy. This was a helpful way to understand internal anatomy as it relates to the procedure. I think this kind of simulation is helpful for a beginner like me.”
Negative comments were largely related to bugs inherent in any prototype. In this case, the majority of negative comments addressed issues related to the fit of the goggles (particularly for those who wore eyeglasses (9/36 responses =25.0%) and the stability of the image or need to keep the head relatively still (16/36 = 44.4%). Examples of some of the negative comments are included.
“Wearing the glasses over glasses (that is, the ones I need to see) was clunky and awkward.”
“The initial anatomy of the SCM/clavicle seemed to be a bit off from what I had palpated on the mannequin. However, it lined up later. Keeping head in one specific position was somewhat difficult.”
Comments regarding perceived barriers to implementation of AR as a potential training tool were primarily related to the potential cost of implementation (10/31 responses = 32.3%) and bugs related to the alignment of images and comfort of the glasses (9/31 = 29.0%). Verbatim comments related to perceived barriers to implementation included.
“I question the cost/utility ratio. You might be able to achieve the same thing with a printed picture lying over the mannequin.”
“Different size people and individuals with corrected vision - the glasses are limiting in those people.”
Discussion
Results of this study demonstrated the usability and feasibility of a 1st person POV AR application in simulated CVC insertion training. Participants with a variety of levels of experience found the AR technology to be realistic and the features consistent with promotion of learning and skills facilitation. Furthermore, there were no significant differences in the identification of landmarks and CVC placement between experienced and inexperienced trainees, supporting the evidence that AR can be a useful tool for providers of all levels of experience. While initial results from this pilot study are encouraging, the authors recognize that there is still much work to be done to improve this technology prior to implementation as a potentially useful procedural training tool for broad levels of medical training.
Research into the potential uses of AR is quickly advancing. There is existing evidence to support its beneficial impact in many aspects of clinical medicine and medical training such as laparoscopic surgery, neurosurgery and cardiac pulmonary resuscitation (CPR).4,10–17 One study, for example found that pediatric medical workers performed better after training on a virtual-reality enhanced child mannequin18 and another showed that AR technology for CPR was deemed realistic and useful.19 Researchers have found that trainees prefer AR teaching devices over VR devices due to the addition of tactile feedback.5 A report from the National League of Nursing identified augmented reality as one of six emerging technologies that are expected to significantly impact learning, teaching and research in the near future.20
A potential advantage of AR over VR is the ability to allow the trainee to visualize the relevant internal structures in a physical anatomic model, rather than a screen based model. Whereas most standard mannequin simulators allow for recognition of external anatomical landmarks, AR technology also allows the trainee to identify the internal structures that are pertinent to the procedure being performed. In this study the AR glasses guided the trainees to the correct point of needle insertion and alerted them to the relative positioning of the internal jugular and carotid artery. The prototype used in this study was also unique in that it provided a 1st person POV of the internal anatomical landmarks. The 1st person POV provides the operator with the full tactile experience of the procedure, compared to passively watching, or 3rd person POV. Previous work has largely utilized 3rd Person POV wherein the internal landmarks are projected on a TV screen. Use of a 1st person approach better simulates the real clinical situation in that it allows the trainee to focus attention on the area of interest and not on a remote screen. To our knowledge, this is the first study to have evaluated 1st person POV AR technology for medical training.
CVC’s are inserted in more than 5 million patients each year, with an estimated complication rate as high as 15%.21 Deliberate practice by residents in simulated settings has shown improved performance in CVC insertion both in simulation-based assessment as well as during placement in actual patients.22,23 The ability to identify the location of internal landmarks, as well as visualizing normal and pathological states of the body during training would help trainees understand the relationship between their actions and what is occurring in the body.
Although this study was a pilot of a new prototype, it is important to recognize the potential limitations of the technology and how it might be incorporated into medical training curricula.24 The primary complaints of the prototype used in our study related to the constraints of the 3-D AR glasses such as fit (particularly for those wearing eye glasses), the requirement to keep the head still, and, for some, a feeling of unnatural head positioning. While we acknowledge that the adjustment of the glasses and alignment of images may have slightly delayed the time to completion of the procedure, the data suggest that the ability of the trainees to correctly identify the salient structures and place the needle correctly was not compromised by these adjustments. However, updated models of the hardware continue to be in development with the full expectation that these “bugs” will be eliminated in the future. Participants perceived the cost of AR development as a potential barrier to implementation of AR technology. Raque et al. demonstrated that using simulation-based education for surgery residents increased the cost of training each resident, with only minimal impact in training and a decrease in faculty time spent on instruction.25 Thus, for advanced tools such as AR to make a broad impact, they will have to be cost-effective. Although it is likely, as with any burgeoning technology, that developmental and production costs will decrease over time, it will be important to fully evaluate the AR technology against standard simulation methodology to ensure efficacy and cost-benefit.
As a pilot, this study is limited by its small size and focus on usability and feasibility. Future studies comparing the AR technology with standard simulation training models will thus be important. Although internal jugular placement carries other potential risks such as hemothorax, for the purposes of this evaluation, only carotid artery puncture and multiple attempts were included as complications.
In summary, this pilot study demonstrates the usability and feasibility of 1st person POV AR technology as a potentially promising training tool for central line placement. Of note was the reported unique ability of this approach to provide visualization of internal anatomical landmarks and meaningful hands-on experience. Further studies comparing AR technology with standard simulation trainers for a variety of procedural skills will thus be important prior to implementation into medical simulation-education curricula.
Supplementary Material
Supplemental Digital Content 1: Document, Participant Assessment
Supplemental Digital Content 2: Document, Participant Evaluation
Contributor Information
Lauryn R. Rochlen, Department of Anesthesiology, University of Michigan, Ann Arbor, MI.
Robert Levine, Emergency Care Center, Jackson Memorial Hospital, Miami, FL; ArchieMD, Inc., Boca Raton, FL
Alan R. Tait, Department of Anesthesiology, University of Michigan, Ann Arbor, MI; Center for Bioethics and Social Sciences in Medicine, University of Michigan, Ann Arbor, MI.
References
- 1.Cook DA, Hatala R, Brydges R, et al. Technology-enhanced simulation for health professions education: a systematic review and meta-analysis. Jama. 2011;306(9):978–988. doi: 10.1001/jama.2011.1234. [DOI] [PubMed] [Google Scholar]
- 2.Issenberg SB, McGaghie WC, Petrusa ER, Lee Gordon D, Scalese RJ. Features and uses of high-fidelity medical simulations that lead to effective learning: a BEME systematic review. Medical teacher. 2005;27(1):10–28. doi: 10.1080/01421590500046924. [DOI] [PubMed] [Google Scholar]
- 3.Ellaway R. Virtual reality in medical education. Medical teacher. 2010;32(9):791–793. doi: 10.3109/0142159X.2010.513223. [DOI] [PubMed] [Google Scholar]
- 4.Barsom EZ, Graafland M, Schijven MP. Systematic review on the effectiveness of augmented reality applications in medical training. Surg Endosc. 2016 doi: 10.1007/s00464-016-4800-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Berryman DR. Augmented reality: a review. Med Ref Serv Q. 2012;31(2):212–218. doi: 10.1080/02763869.2012.670604. [DOI] [PubMed] [Google Scholar]
- 6.Shuhaiber JH. Augmented reality in surgery. Arch Surg. 2004;139(2):170–174. doi: 10.1001/archsurg.139.2.170. [DOI] [PubMed] [Google Scholar]
- 7.Jeon Y, Choi S, Kim H. Evaluation of a simplified augmented reality device for ultrasound-guided vascular access in a vascular phantom. J Clin Anesth. 2014;26(6):485–489. doi: 10.1016/j.jclinane.2014.02.010. [DOI] [PubMed] [Google Scholar]
- 8.Huang GC, Newman LR, Schwartzstein RM, et al. Procedural competence in internal medicine residents: validity of a central venous catheter insertion assessment instrument. Academic medicine : journal of the Association of American Medical Colleges. 2009;84(8):1127–1134. doi: 10.1097/ACM.0b013e3181acf491. [DOI] [PubMed] [Google Scholar]
- 9.Ryan G, Bernard H. Techniques to identify themes. Field Methods. 2003;15(1):85–109. [Google Scholar]
- 10.Chicchi Giglioli IA, Pallavicini F, Pedroli E, Serino S, Riva G. Augmented Reality: A Brand New Challenge for the Assessment and Treatment of Psychological Disorders. Computational and mathematical methods in medicine. 2015;2015:862942. doi: 10.1155/2015/862942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Im DJ, Ku J, Kim YJ, et al. Utility of a Three-Dimensional Interactive Augmented Reality Program for Balance and Mobility Rehabilitation in the Elderly: A Feasibility Study. Annals of rehabilitation medicine. 2015;39(3):462–472. doi: 10.5535/arm.2015.39.3.462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ntourakis D, Memeo R, Soler L, Marescaux J, Mutter D, Pessaux P. Augmented Reality Guidance for the Resection of Missing Colorectal Liver Metastases: An Initial Experience. World journal of surgery. 2015 doi: 10.1007/s00268-015-3229-8. [DOI] [PubMed] [Google Scholar]
- 13.Feifer A, Delisle J, Anidjar M. Hybrid augmented reality simulator: preliminary construct validation of laparoscopic smoothness in a urology residency program. J Urol. 2008;180(4):1455–1459. doi: 10.1016/j.juro.2008.06.042. [DOI] [PubMed] [Google Scholar]
- 14.Neary PC, Boyle E, Delaney CP, Senagore AJ, Keane FB, Gallagher AG. Construct validation of a novel hybrid virtual-reality simulator for training and assessing laparoscopic colectomy; results from the first course for experienced senior laparoscopic surgeons. Surg Endosc. 2008;22(10):2301–2309. doi: 10.1007/s00464-008-9900-5. [DOI] [PubMed] [Google Scholar]
- 15.Pellen MG, Horgan LF, Barton JR, Attwood SE. Construct validity of the ProMIS laparoscopic simulator. Surg Endosc. 2009;23(1):130–139. doi: 10.1007/s00464-008-0066-y. [DOI] [PubMed] [Google Scholar]
- 16.Ritter EM, Kindelan TW, Michael C, Pimentel EA, Bowyer MW. Concurrent validity of augmented reality metrics applied to the fundamentals of laparoscopic surgery (FLS) Surg Endosc. 2007;21(8):1441–1445. doi: 10.1007/s00464-007-9261-5. [DOI] [PubMed] [Google Scholar]
- 17.Van Sickle KR, McClusky DA, Gallagher AG, Smith CD. Construct validation of the ProMIS simulator using a novel laparoscopic suturing task. Surg Endosc. 2005;19(9):1227–1231. doi: 10.1007/s00464-004-8274-6. [DOI] [PubMed] [Google Scholar]
- 18.Donoghue AJ, Durbin DR, Nadel FM, Stryjewski GR, Kost SI, Nadkarni VM. Effect of high-fidelity simulation on Pediatric Advanced Life Support training in pediatric house staff: a randomized trial. Pediatr Emerg Care. 2009;25(3):139–144. doi: 10.1097/PEC.0b013e31819a7f90. [DOI] [PubMed] [Google Scholar]
- 19.Semeraro F, Frisoli A, Bergamasco M, Cerchiari EL. Virtual reality enhanced mannequin (VREM) that is well received by resuscitation experts. Resuscitation. 2009;80(4):489–492. doi: 10.1016/j.resuscitation.2008.12.016. [DOI] [PubMed] [Google Scholar]
- 20.Skiba DJ. On the horizon: technologies coming to your school soon. Nurs Educ Perspect. 2010;31(2):114–115. [PubMed] [Google Scholar]
- 21.McGee DC, Gould MK. Preventing complications of central venous catheterization. The New England journal of medicine. 2003;348(12):1123–1133. doi: 10.1056/NEJMra011883. [DOI] [PubMed] [Google Scholar]
- 22.Barsuk JH, McGaghie WC, Cohen ER, O'Leary KJ, Wayne DB. Simulation-based mastery learning reduces complications during central venous catheter insertion in a medical intensive care unit. Critical care medicine. 2009;37(10):2697–2701. [PubMed] [Google Scholar]
- 23.Evans LV, Dodge KL, Shah TD, et al. Simulation training in central venous catheter insertion: improved performance in clinical practice. Academic medicine : journal of the Association of American Medical Colleges. 2010;85(9):1462–1469. doi: 10.1097/ACM.0b013e3181eac9a3. [DOI] [PubMed] [Google Scholar]
- 24.Wright WG. Using virtual reality to augment perception, enhance sensorimotor adaptation, and change our minds. Front Syst Neurosci. 2014;8:56. doi: 10.3389/fnsys.2014.00056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Raque J, Goble A, Jones VM, Waldman LE, Sutton E. The Relationship of Endoscopic Proficiency to Educational Expense for Virtual Reality Simulator Training Amongst Surgical Trainees. The American surgeon. 2015;81(7):747–752. doi: 10.1177/000313481508100727. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Digital Content 1: Document, Participant Assessment
Supplemental Digital Content 2: Document, Participant Evaluation