Abstract
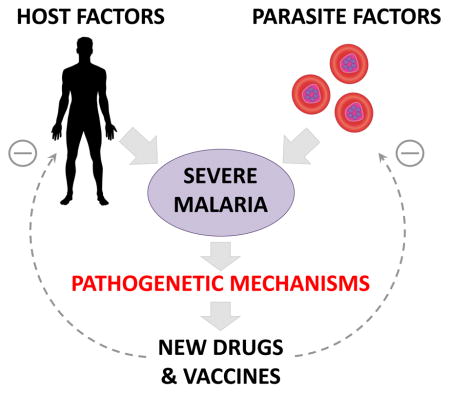
Plasmodium falciparum causes the most severe and fatal form of malaria in humans with over half a million deaths each year. Cerebral malaria (CM), a complex neurological syndrome of severe falciparum malaria, is often fatal and represents a major public health burden. Despite vigorous efforts, the pathophysiology of CM remains to be elucidated, thereby hindering the development of adjunctive therapies. In recent years, multidisciplinary and collaborative approaches have led to groundbreaking progress both in the laboratory and in the field. Here we review the latest breakthroughs in severe malaria pathogenesis, with a specific focus on new pathogenetic mechanisms leading to CM. The most recent findings point towards specific parasite phenotypes targeting brain microvasculature, endothelial dysfunction and subsequent oedema-induced brain swelling.
Keywords: Plasmodium spp, Pathophysiology, Cerebral malaria, Endothelial dysfunction, Sequestration, Malaria in pregnancy
Graphical abstract
1. Introduction
Malaria is still a leading cause of morbidity and mortality in the developing world. The virulence of Plasmodium falciparum is caused by several factors including parasite proteins on the surface of infected erythrocytes (IE). These allow the binding of these cells to the microvascular endothelium of various organs and tissues during infection. Proteins of the P. falciparum erythrocyte membrane protein 1 (PfEMP1) family mediate this adhesion through specific binding to multiple cell receptors. These include intercellular adhesion molecule-1 (ICAM-1), CD36, E-selectin, neural cell adhesion molecule (NCAM) and CD31 (PECAM-1) for endothelial beds, as well as chondroitin sulfate A (CSA) for placental syncytiotrophoblasts. Binding to endothelium results in widespread sequestration of IE, which can lead to lead to endothelial activation as well as pro-inflammatory and pro-coagulant responses.
Severe falciparum malaria encompasses a broad range of diseases, the development of which may be influenced by age, exposure and immune status (Wassmer et al., 2015). It includes complications that affect specific organs such as the brain in cerebral malaria (CM) or the placenta in malaria in pregnancy (MiP). Histopathology and laboratory studies allowed investigators to establish a causal link between placenta-specific sequestration of P. falciparum and MiP. Indeed, the ability of PfEMP1 variants to target different receptors, the expression of which varies depending on the organ, could explain why some patients with malaria develop organ-specific syndromes. Researchers have speculated that a specific PfEMP1 variant could bind receptors that are preferentially expressed in cerebral microvasculature, and could account for the focal manifestations observed in CM, the most lethal complication of P. falciparum infection. Two recent reports simultaneously shed new light on the pathogenetic mechanisms leading to CM. First, endothelial protein C receptor (EPCR) was identified as a binding partner for PfEMP1. Second, normally low levels of EPCR in brain microvessels were shown to be further down-regulated in CM, with a loss of EPCR and thrombomodulin at sites of IE sequestration. These studies provided new clues towards parasite and host cell interactions leading to CM, and connected for the first time brain-specific sequestration of EPCR-binding parasites to the loss of the protein C anti-coagulant function and endothelial cytoprotective pathways (Aird et al., 2014).
While the relative frequency of severe malaria is low, its reported case fatality rate has not substantially changed over decades, especially for CM (Manning et al., 2014). Due to the lack of specific neuro- and vasculoprotective therapies, treatments for CM are currently still precariously limited to antimalarial drugs and emergency supportive care. The former are quickly dwindling, as the resistance of P. falciparum malaria against artemisinin combination treatments, the recommended first-line therapy for infected patients, is on the rise in southeastern Asia. Multi-drug-resistant falciparum malaria is increasingly difficult to treat and new antimalarials are not expected to become available within the next few years. This underlines the necessity for molecular markers for surveillance of partner drug resistance, in conjunction with the implementation of new biomarkers for early diagnosis and outcome prediction, as well as effective adjunct therapies.
Here we review some recent data with a focus on newly developed research approaches aimed at a better understanding of the pathogenetic mechanisms of severe malaria in general and CM in particular.
2. Parasite-brain microvasculature specificity in CM: a virulence factor?
The severity of P. falciparum is linked to sequestration of IEs within the microvasculature of various organs including the brain. This sequestration is driven both by the expressed var gene in the parasite, leading to the expression of a specific variant of PfEMP-1, and the presence of its associated receptors on microvascular walls (Hviid and Jensen, 2015). Since there are considerable variations in both adhesion molecule expression and functional properties of endothelial cells depending on their position within the vascular bed of a particular tissue, it has been hypothesised that CM may result from a brain endothelial-specific adhesive type of parasite (Moxon et al., 2014). Indeed, IE expressing the domain cassettes (DC) 8 and 13 of the cytoadherent ligand PfEMP-1 adhere to EPCR (Turner et al., 2013). By interfering with EPCR anti-coagulant and pro-endothelial barrier functions, IE adhesion could promote coagulation and vascular permeability that contribute to the pathogenesis of CM (Moxon et al., 2014). To better understand parasite factors that contribute to disease severity, Gillrie et al. (2015) developed in vitro binding models for different microvascular beds to examine the adhesion of DC8- and DC13-expressing parasite lines to endothelial cells from different microvasculature, and the consequences of EPCR engagement on endothelial cell function. They reported that IE from IT4var19 (DC8) and IT4var07 (DC13) parasite lines adhere to human brain, lung and dermal endothelial cells under shear stress. However, the relative contribution of EPCR to parasite cytoadherence on different types of endothelial cell varied.
Divergent functional outcomes for DC8 cysteine-rich interdomain region (CIDR) α1.1 and DC13 CIDRα1.4 domains were also observed. IT4var07 CIDRα1.4 inhibited generation of activated protein C (APC) on lung and dermal endothelial cells and blocked the APC-EPCR binding interaction on brain endothelial cells. IT4var19 CIDRα1.1 inhibited thrombin-induced endothelial barrier dysfunction in lung endothelial cells, whereas IT4var07 CIDRα1.4 inhibited the protective effect of APC on thrombin-induced permeability. Overall, these findings reveal a much greater complexity of how CIDRα1-expressing parasites may modulate malaria pathogenesis through EPCR adhesion (Gillrie et al., 2015). DC8 PfEMP1 encode multiple endothelial binding domains, including binding activity for EPCR. These results show that PfEMP1 domains compete with protein C for EPCR binding but the extent of competition differs between domains.
Bernabeu et al. (2016) recently investigated these parasite virulence factors in adult patients in India and demonstrated that specific EPCR-binding parasites lead to severe malaria in that population. In addition, parasite phenotype and biomass are associated with patient hospitalization and disease severity. The authors show a broad range of EPCR binding activity from severe malaria isolates and even parasite domains that partially obstructed the interaction between EPCR and APC were sufficient to interfere with the cytoprotective functions of APC (Bernabeu et al., 2016). Taken together, their findings suggest that parasites may be under selection for phenotypic variation in a key host pathway that regulates coagulation and endothelial barrier properties, and has important implications for pathogenic mechanisms in severe malaria. Full-length sequences of PfEMP1 encoding transcripts were characterized in clinical isolates from children with severe malaria admitted to hospital in Tanzania, and EPCR-binding CIDRα1 domains dominated PfEMP1 transcript profiles of children suffering from CM and/or severe malarial anaemia, further strengthening the evidence for a crucial pathogenic role of the PfEMP1–EPCR interaction in severe malaria (Jespersen et al., 2016).
EPCR is not the only receptor suspected to play an important role in the development of severe malaria. Studies of parasite isolates have demonstrated high rates of in vitro ICAM-1 binding among wild strains but reported correlations between ICAM-1 binding and disease severity have been inconsistent. Recent results suggest that ICAM-1 is a co-receptor for a subset of EPCR-binding parasites (Avril et al., 2016). Indeed, Avril et al. (2016) showed that parasites expressing DC13 have dual binding specificity for EPCR and ICAM-1, suggesting for the first time that ICAM-1-binding variants can be grouped into CD36 and EPCR co-receptor-binding traits. This leads to different cytoadherence abilities on TNF-stimulated endothelial cells, which has important implications for understanding parasite organ-specific microvascular bed tropism in pro-inflammatory conditions.
3. Microvascular endothelial dysfunction: new causes and repercussions
In the recent years, convincing evidence has been presented to support the role of both endothelial cell activation and platelets in modulating the pathogenesis of severe P. falciparum malaria. Thrombin, a common factor in both processes, is now thought to be a driver of pathology in CM. The relative contribution of EPCR-binding parasites versus loss of EPCR from the endothelial surface in mediating CM is not known, although both are associated with disease in clinical studies (Turner et al., 2013; Moxon et al., 2014). The key mediator of inflammation in both cases appears to be thrombin, which is a potent mediator of both pro-and anti-inflammatory pathways, depending on the context of endothelial signalling. Thrombin engages thrombomodulin on the plasma membrane of intact endothelium, where it promotes activation of protein C. The latter is accelerated by the presence of EPCR, which binds to protein C and presents it for optimal activation by the thrombin-thrombomodulin complex. Further to its anticoagulant activity, generated APC can also trigger numerous cell-signaling pathways initiating protective cellular responses upon exposure to pro-inflammatory, pro-apoptotic, or toxic insult. IEs expressing PfEMP1 compete with protein C and APC for EPCR, thereby down-regulating protein C activation by the thrombin-thrombomodulin complex. The resulting loss of EPCR-APC–induced cytoprotective signalling is consistent with a decrease in blood-brain barrier (BBB) properties, potentially leading to vasogenic oedema in CM.
Direct protein C pathway alteration by binding of EPCR-specific IEs is not the only cause of endothelial dysfunction in CM. Indeed, P. falciparum infection also initiates early endothelial and platelet activation, leading to coagulation dysregulation and microvascular lesions locally (Wassmer et al., 2011a). Furthermore, IEs elicit a myriad of signalling pathways leading to aberrant pro-coagulant effects, ultimately resulting in enhanced endothelial activation, damage and apoptosis (O’Sullivan et al., 2016). Lastly, severe falciparum malaria has been associated with a down-regulation of normal endogenous anticoagulant pathways. EC surface expression of thrombomodulin and EPCR are both reduced, likely through cytokine-enhanced shedding, leading to an increase of their soluble levels in plasma (Moxon et al., 2013). Together, these effects combine and lead to a significant reduction in generation of anti-inflammatory and cytoprotective APC on the endothelial surface. These findings suggest new avenues for acute therapeutic intervention and match well with postmortem observations and magnetic resonance imaging (MRI) findings linked to mortality in CM.
Such an endothelial dysfunction is not only observed in severe falciparum malaria, but was also reported in severe Plasmodium vivax (Barber et al., 2015) and Plasmodium knowlesi (Yeo et al., 2007) cases, which raises the question of possible common pathogenic pathways in these various types of infection. All plasmodia species can cause severe and fatal malaria. In falciparum malaria, the most common cause of severe malaria, impaired tissue perfusion has long been recognised to arise from microvascular obstruction by IE adherent to endothelial cells. More recently recognised is the contribution of concurrent impairment of nitric oxide (NO) bioavailability, endothelial activation and microvascular dysfunction to impaired tissue perfusion and severe disease (Yeo et al., 2014). Angiopoietin-2, released from endothelial cell Weibel-Palade bodies and an NO-inhibited autocrine mediator of endothelial activation, is markedly elevated in severe falciparum malaria and consistently associated with impaired tissue perfusion and fatal outcome in both adult and paediatric severe malaria. This is independent of both total and sequestered parasite biomass, suggesting that microvascular obstruction and microvascular dysfunction make separate contributions to pathogenesis. Microvascular function, the capacity to increase flow and oxygen delivery in response to ischaemia, is decreased in severe falciparum malaria and associated with an increased risk of death. Endothelial activation, decreased endothelial NO bioavailability and microvascular dysfunction are also associated with impaired tissue perfusion in vivax and knowlesi malaria, a factor likely to contribute to organ dysfunction and severe malaria caused by infection with these species. Initial clinical trials of agents aimed at restoring NO bioavailability in severe falciparum malaria have recently been completed (Hawkes et al., 2011; Serghides et al., 2011), and microvascular function can be improved by L-arginine infusion in severe falciparum malaria (Yeo et al., 2013). These results suggest that new compounds aimed at increasing microvascular NO and microvascular functions have potential clinical benefits as adjunctive treatments in severe malaria from all species.
4. Rosetting and clumping: consequences for sequestration and microvascular obstruction
Parasite adhesion interactions in severe falciparum malaria are not restricted to the endothelium. Indeed, IEs can bind uninfected erythrocytes to form rosettes (Handunnetti et al., 1989), or platelets to form clumps (Pain et al., 2001). Both processes have been associated with severe malaria (Rowe et al., 1995; Pain et al., 2001) and CM (Carlson et al., 1990; Wassmer et al., 2008).
In this context, recent advances have been made in elucidating the molecular mechanisms underlying rosetting, with a view to development of rosette-reversing therapies. Rosetting generally requires the presence of soluble serum factors such as IgM, and the ability of IE to form rosettes and to bind non-immune IgM is correlated (Rowe et al., 2002). While the role of IgM binding in rosetting remains unclear, it appears to strengthen the bond of the central IE with the surrounding erythrocytes. Stevenson et al. (2015) recently reported that the serum protein α2-macroglobulin (α2M) is able to induce rosetting in vitro and ex vivo, using several parasite isolates. In contrast to IgM, α2M elicits rosetting alone, while the presence of IgM significantly lowers the concentration of α2M required. The authors of the study postulate that α2M allows the crosslinking of several individual PfEMP1 molecules, thereby increasing their combined avidity for carbohydrate receptors on surrounding erythrocytes and promoting the formation of rosettes. These results suggest that P. falciparum hijacks soluble host proteins for its own benefit, and avoids immune destruction by manipulating those to facilitate adhesion of IEs to low-affinity carbohydrate receptors. In addition, another report recently showed that PfEMP1 is not the only parasite ligand used in rosetting, potentially opening new rosette-disrupting approaches. Goel et al. (2015) showed in a very elegant study that the repetitive interspersed family of proteins (RIFINs) mediates binding of IEs with a preference for blood group A, leading to the formation of large rosettes of 10 or more IEs. This was not observed with IEs from group O. Indeed, blood group O is common in malaria endemic areas and IEs of that blood group were shown to form small, weak rosettes (Rowe et al., 2007). The role of RIFINs was confirmed by the disruption of rosettes in the presence of anti-RIFIN antibodies. These results suggest that RIFINs not only play a fundamental role in the development of severe malaria but also contribute to the virulence of P. falciparum.
Puzzlingly, formed rosettes have never been described in the peripheral bloodstream, suggesting that they sequester in the microvasculature and aggravate microvascular obstructions during severe malaria in general, and CM in particular. Understanding the mechanisms by which rosettes sequester (i.e., by direct binding of rosetting IE to endothelial cells, to platelets on endothelial cells or to non-rosetting cytoadherent IE is fundamental, as it may open new adjunct therapies to reduce the biomass of sequestered IE, a parameter associated with disease severity (Hendriksen et al., 2012). IE of the IT/R29 strain expressing a rosette-mediating PfEMP1 variant (IT4var09) were recently shown to cytoadhere to human brain microvascular endothelial cells using heparan sulfate proteoglycans as ligands (Adams et al., 2014). This process is distinct from rosetting, which is primarily mediated by interactions with between the NTS-DBL1α domain of PfEMP1 and complement receptor 1. This study shows for the first time that IT4var09-expressing parasites are capable of dual interactions with both endothelial cells and uninfected erythrocytes via distinct receptor-ligand interactions, and therefore could aggravate microvascular obstruction in severe malaria by facilitating the sequestration of platelet-mediated clumps.
One of the most recently described P. falciparum cytoadherence phenotypes is the ability of IEs to bind to platelets in suspension in vitro to form platelet-mediated clumps. Similar to rosetting, the formation of clumps is a common phenotype and has been reported in a variety of endemic settings (Rowe et al., 2009). This is mediated by the binding of IEs to platelet receptors which include CD36 (Pain et al., 2001), P-selectin (Wassmer et al., 2008) and globular C1q receptor (gC1qR) (Biswas et al., 2007). In all cases, the parasite ligands are unknown, although PfEMP1 is a likely candidate molecule. A recent study performed using clinical isolates from Mozambican patients to evaluate cytoadherence properties such as platelet-mediated clumping, rosetting and adhesion to purified receptors (CD36, ICAM1 and gC1qR) revealed that, compared with matched controls, prevalence of both rosetting and platelet-mediated clumping and adhesion to gC1qR was higher in severe cases (Mayor et al., 2011). Inhibition of these cytoadherence phenotypes may therefore reduce the occurrence or improve the prognosis of severe malaria outcomes. Similar to rosettes, platelet-mediated clumps have not been observed in the bloodstream and it is likely that they sequester in the microvasculature using IE or platelet receptors (or both) to cytoadhere on endothelial cells (Wassmer et al., 2011a). Since this may potentially aggravate microvascular obstruction in CM, further studies aimed at understanding the molecular process involved in their sequestration are warranted.
5. Clinical consequences of BBB opening in CM: vasogenic oedema and brain swelling
Following the report by Seydel et al. (2015), a study was initiated to investigate the different mechanisms potentially responsible for brain swelling in both pediatric and adult CM patients in India (Wassmer et al., 2015). Brain swelling was identified by MRI in over 50% of patients enrolled in the ongoing study, irrespective of their age group. The frequent occurrence of brain swelling in CM has been previously reported in separate studies on Indian adults using computed tomography (CT) (Mohanty et al., 2011), as well as in Bangladeshi adults (Maude et al., 2014) and Malawian children using MRI (Potchen et al., 2012). The cause of the swelling, which can lead to brain herniation in fatal cases (Seydel et al., 2015), remains to be identified and may be due to cytotoxic or vasogenic causes. Recent results show that patients who develop CM exhibit an over-reaction of their endothelial cells to systemic inflammation, which is not observed in uncomplicated malaria (Wassmer et al., 2011b). Such vulnerability, coupled to a loss of cytoprotective EPCR in the brain, could lead to a disruption of the BBB and the leakage of fluids and proteins from the vascular system into the extracellular space. Also called vasogenic oedema, this process is consistent with the description of ring haemorrhages, a characteristic sign of BBB disruption, in pediatric CM (Taylor et al., 2004; Dorovini-Zis et al., 2011). In addition, these ring hemorrhages correlate positively between retinal and cerebral tissues, owing to their common embryological origin from the neuroectoderm (Barrera et al., 2015; Greiner et al., 2015). Malaria retinopathies seen in pediatric CM are therefore a direct reflection of the neurovascular disease process, and the high frequency of ring haemorrhages both in the brain and in the retina in fatal disease point towards the occurrence of vasogenic oedema. However, evidence for a generalised increase in BBB permeability leading to vasogenic oedema is still debated. A study performed in Thailand showed no evidence of BBB impairment, as radioactively-labelled albumin given intravenously was not found in the cerebrospinal fluid (CSF) of CM patients during coma (Warrell et al., 1986). Additionally, post-mortem analyses of adult Vietnamese patients who died of CM showed that its pathophysiology only involved subtle functional changes in BBB integrity (Brown et al., 2000), and evidence from a different cohort demonstrated that localised loss of vascular integrity did not correlate with the occurrence of pre-mortem coma (Medana et al., 2011). Brain swelling may also occur as a result of cytotoxic oedema, which can result from cells in the cerebral tissue being unable to maintain membrane potential after the failure of Na+/K+ ATP-dependent pumps, due to hypoxia or nutrient deprivation. This may cause a redistribution of water from the extra-cellular to the intracellular compartments, ultimately leading to cell swelling, cell death and tissue damage. Ischaemic or hypoxic insults due to mechanical effects of microvascular obstruction by IEs, rosettes and platelet-mediated clumps, as well as nutrient “steal” by local metabolically active parasites could account for cytotoxic oedema in CM. This mechanism is consistent with abundant sequestration in the cerebral microvasculature during the neurologic syndrome (White et al., 2013), and the first in vivo magnetic resonance study of experimental CM revealed a preponderant role for cytotoxic oedema in fatal outcome (Penet et al., 2005).
An increase in intravascular fluid volume within the brain due to sludging of blood flow with sequestration of IEs, rosettes and platelet-mediated clumps could also cause brain swelling and would explain the diffuse mild brain swelling reported in severe malaria patients from Bangladesh (Maude et al., 2014), without evidence of either cytotoxic or vasogenic oedema. However, cytoadherence itself may not be directly or solely responsible for this clinical syndrome (Storm and Craig, 2014).
Lastly, it is entirely plausible that both mechanisms are not mutually exclusive. A study in live mice using high-field MRI with whole-brain coverage showed that vasogenic oedema occurs first in infected animals, and starts in the olfactory bulb before spreading deeper into the brain along a specific path called the rostral migratory stream, eventually reaching the brain stem. Microvascular pathology and ischemic brain injury develop only secondarily, after vasogenic oedema formation (Hoffmann et al., 2016). Additional MRI studies are currently underway in CM patients from Asia and Africa, and are aiming to elucidate these pathogenetic processes (Wassmer et al., 2015).
6. New adjunct therapies and critical care approaches in severe malaria
Even under optimal conditions, the case–fatality rate in severe malaria treated with either artemisinin derivatives or quinine remains high. In addition, multi-drug-resistant falciparum malaria is increasingly difficult to treat and new effective antimalarial agents are not expected to become available within the next few years. In an effort to reduce malaria-related mortality, numerous adjunctive therapies that may alter severe malaria-induced physiological abnormalities are being evaluated, some of which have been described in other sections of this review. Such therapies are, in nature, highly specific to distinct syndromes of severe malaria, as their aim is to target precise pathophysiological processes. For example, protein C system defects inflicted by the malaria parasite protein PfEMP1 in CM can be overcome by a soluble EPCR variant (Petersen et al., 2015), and could therefore represent a revolutionary approach to dampen the pathogenetic mechanisms and decrease mortality in affected patients. Promising advances in adjunct therapies for other severe malaria syndromes such as acute respiratory distress, acute kidney injury, severe anaemia and metabolic acidosis are still lacking.
The potential clinical benefit of fluid resuscitation was recently investigated and liberal fluid loading in adults with severe malaria showed no improvement in the acidosis and acute kidney injury, but increased the incidence of acute pulmonary oedema (Hanson et al., 2014). However, a more conservative fluid strategy, using a simple weight-based algorithm, led to a low incidence of acute respiratory distress without significant deterioration in acid-base status, renal function, electrolyte profile or systemic haemodynamics, and was associated with increased survival (Aung et al., 2015).
In addition to P. falciparum, severe cases of P. vivax and P. knowlesi have also been reported, although sequestration is not a specific feature of either infection and the relative contribution of co-morbidities to clinical manifestations, particularly in vivax malaria, remains to be investigated (Wassmer et al., 2015). Both parasitic infections can cause acute pulmonary oedema with a clinical phenotype similar to that seen in severe falciparum malaria. No studies of fluid resuscitation have been performed in these patients, but those are warranted.
7. Novel parasite factors involved in malarial pathogenesis and possible therapeutic targets
In parallel to the development of adjunct therapies, a growing effort in the search for new and effective pharmacotherapies has been triggered by the emergence of multi-drug resistance in P. falciparum. While still in their infancy, these approaches are promising and provide a wide range of new therapeutic targets. Several new parasite factors were recently identified and have emerged as potential drug target candidates. Among those, G-quadruplex (G4) DNA motifs and RecQ helicases are newly described players in virulence gene control in P. falciparum. G4s are four-stranded structures formed by the stacking of quartets of guanines, and recent work has shown that they can form in vivo as well as in vitro, affecting DNA replication, transcription, translation and telomere maintenance. Harris and Merrick (2015) first demonstrated that DNA helicases, as well as histone-modifying proteins, can influence var gene dynamics in P. falciparum. Understanding the G4-mediated regulation of the parasite virulence may open the door to novel therapeutic interventions.
Plasmodium falciparum exports parasite-encoded proteins involved in structural and functional remodelling of the host cell. This process is essential for the development of the parasite and is also associated with its virulence (Maier et al., 2009). Molecular chaperones of the heat shock protein (Hsp) family are prominent members of the exportome, including various Hsp40s and one Hsp70. The first biochemical evidence for a specific functional co-chaperone interaction between the exported malarial PFA0660w and PfHsp70-x was recently reported (Daniyan et al., 2016). PFA0660w can stimulate the ATPase activity of PfHsp70-x and work additively with it in a co-chaperone/chaperone interaction, resulting in protein aggregation suppression. The authors also showed that PFA0660w could potentially act independently as a chaperone. These findings support the proposed role of PfHsp70-x and PFA0660w in parasite protein trafficking and folding in IEs. Further studies are underway to determine the molecular basis for the specificity of this interaction, and to identify inhibitors capable of disrupting it. All of the modifications to the IEs are induced by parasite proteins, most of which initially traffic from the parasite via the secretory pathway to the parasitophorous vacuole. There, proteins interact with a translocon complex called PTEX (Plasmodium translocon of exported proteins) that transports them across the vacuole membrane into the IE. Blocking protein export through blocking PTEX function leads to the arrest of parasite growth and loss of virulence (Kalanon et al., 2016), making PTEX an excellent drug target (Gilson et al., 2016).
Post-translational modification of histones is one of the key gene regulation mechanisms during the intra-erythrocyte development cycle of P. falciparum. Studies of proteins, which recognise and interact with histone post-translational modifications, are pivotal for understanding P. falciparum pathogenesis. Bromodomain proteins bind to acetylated lysines, often on histones, and frequently play a role in regulation of gene expression. Plasmodium falciparum-specific bromodomain protein 1 (PfBDP1) binds to chromatin at transcriptional start sites of invasion-related genes and directly controls their expression. Conditional PfBDP1 knockdown causes a significant defect in parasite invasion and growth (Josling et al., 2015). In parallel to these studies, several small molecule inhibitors have recently been reported to have a high affinity and specificity to bromodomains, and could represent a new therapeutic avenue in P. falciparum infection (Padmanabhan et al., 2016).
The unique plasticity of the epigenetic regulation in P. falciparum has also emerged as a pivotal virulence and pathogenicity factor in recent years. Karmodyia et al. (2015) performed genome-wide mapping of multiple histone modifications of P. falciparum and reported H3K36me2 as a global repressive mark, with gene regulation being fine-tuned by the ratio of activation marks to H3K36me2 (Karmodiya et al., 2015). Moreover, var genes are mostly poised and marked by a unique set of activation (H4ac) and repression (H3K9me3) marks, which are mutually exclusive to other P. falciparum housekeeping genes. A better characterization of epigenetic regulation in P. falciparum will lead to the identification of potential therapeutic targets (Ay et al., 2015). Indeed, disrupting the function of proteins responsible for maintaining heterochromatin, such as HP1 (Brancucci et al., 2014), could be an effective strategy to block parasite replication during the asexual cycle. PfAP2-G, a transcription factor shown to drive gametocytogenesis, also represents a promising target to disrupt malaria transmission (Coleman et al., 2014). Extensive characterisations of the parasite epigenetic factors, as well as its post-transcriptional and translational control processes, are likely to open new avenues for drug development against P. falciparum.
8. Pathologies other than CM: MiP
Plasmodium falciparum infection during pregnancy can result in a pathology caused by the accumulation of IEs in the placental intervillous space and the infiltration of maternal monocytes/macrophages (Rogerson et al., 2003), with detrimental outcomes for both the mother and the foetus. Expression of PfEMP1-var2csa at the surface of IEs mediates their adhesion to the placenta. Adaptive immunity is progressively acquired during sequential malaria infections in pregnancy and is mediated by the production of anti-VAR2CSA antibodies, which promote IE adhesion blocking and opsonisation (Desai et al., 2007). This naturally acquired immunity is the key basis for development of a vaccine to protect women during pregnancy, and VAR2CSA is currently the leading candidate (Fried and Duffy, 2015). However, recent findings indicate that broadly neutralising antibodies of multigravidae are not depleted on VAR2CSA recombinant antigens. Using a new approach to assess VAR2CSA domains for functional epitopes recognized by naturally acquired antibodies, Doritchamou et al. (2016) recently demonstrated that different Duffy binding-like (DBL) domain-specific IgG could react to both homologous as well as heterologous antigens and parasites, suggesting that conserved epitopes are shared between allelic variants. In addition, IE binding was blocked by ID1-DBL2-ID2a, DBL4 and DBL5-specific IgG, while partial cross-inhibition activity was observed with purified IgG specific to ID1-DBL2-ID2a and DBL4 antigens. Interestingly, plasma from patients still showed broadly adherence-blocking activity after complete depletion of these VAR2CSA specificities. These results suggest that VAR2CSA vaccines based on a single construct and variant might induce antibodies with limited broad blocking activity, and confirm that a multivalent vaccine comprised of up to five different alleles or with the addition of multiple placental malaria vaccine candidates may be needed to elicit the broad blocking activity observed in African multigravidae (Avril et al., 2010; Hommel et al., 2010).
The generation of protective vaccines is becoming a priority, especially in areas where the prevalence of malaria has decreased due to control and elimination campaigns. Indeed, a recent study conducted in Mozambique showed a close relationship between antibody levels and the intensity of malaria transmission. Mayor et al. (2015) showed convincing evidence that a decline in the prevalence of malaria documented in the study area was accompanied by reductions in levels of IgG antibodies not only against VAR2CSA, but also against non-pregnancy-specific malaria antigens. In pregnant women with MiP, this was associated with an increase in parasite densities and a higher adverse effect of P. falciparum infection on maternal haemoglobin levels and newborn weights (Mayor et al., 2015). Although they also suggest that immunity may be regained as exposure increases, the findings of this study indicate that malaria control and elimination programmes could precede a resurgence of pregnancy-associated malaria pathologies.
Additionally, MiP has also recently been linked to placental pathology in a low malaria transmission area in Brazil, where P. vivax is predominant (Souza et al., 2013). While MiP was not associated with severe outcome in a second study performed by the same team in this region, an increased ratio of peripheral receptor tyrosine kinase Tie-2 to angiopoetin (Ang-1) was associated with the occurrence of MiP. Both Ang-1 and Ang-2 had similar magnitudes but inverse associations with placental barrier thickness. MiP is an effect modifier of the association between Ang-1 and placental barrier thickness (Ataide et al., 2015). These findings provide a possible pathway through which placental pathological changes occur during MiP.
Lastly, further to imbalances in cytokine cascades, IE cytoadhesion and angiogenic dysregulation, excessive or dysregulated complement activation as part of the host innate immune response to malaria infection can also exacerbate the severity of MiP, leading to poor pregnancy outcomes (McDonald et al., 2015b). Using an experimental model of MiP in conjunction with micro-CT and HPLC analysis of neurotransmitter levels, McDonald et al. (2015a) showed that complement activation, in particular C5a, contributes to foetal neuropathologic outcomes during MiP. The offspring of infected animals showed persistent neurocognitive deficits in memory and affective-like behaviour compared with unexposed controls (McDonald et al., 2015a). These impairments were linked with decreased tissue levels of neurotransmitters in regions of the brain associated with the deficits. The inhibition of maternal C5a complement receptor signaling restored the levels of neurotransmitters and reversed the associated phenotype, suggesting new targets for intervention in MiP aimed at decreasing foetal neuropathologic outcomes.
9. New investigative tools and experimental models
A vast array of new tools and models has recently become available to facilitate the investigation of severe malaria pathogenesis, with a particular focus on CM. These are detailed elsewhere (Sahu et al., 2015). Further to this, the rise of the ‘omic’ era during the past decade has provided the malaria research community with unprecedented approaches and technologies to better understand the biology, evolution and pathogenesis of different Plasmodium spp. The Malaria Host-Pathogen Interaction Centre (MaHPIC) is a large international systems biology consortium developed in 2012 and based in the USA (http://www.systemsbiology.emory.edu/index.html), which allowed the development of a variety of distinctive hypothesis-generating and hypothesis-driven collaborations with scientific teams in malaria-endemic regions. These collaborations involve investigators from several countries in South America, southeastern Asia and sub-Saharan Africa, with a focus on infections caused by the predominant, less predominant, or mixed species of Plasmodium (Anderson et al., 2015; Lapp et al., 2015), to study disease states, pathogenesis and physiological or immunobiological questions through the use of untargeted high-resolution metabolomics, as well as clinical and demographic metadata (Salinas et al., 2014). In addition, the MaHPIC team is intensively studying malaria using non-human primate model systems (macaque and New World monkey species, (Joyner et al., 2015)). An overarching goal, beyond the team’s specific research quests, is to develop and make available unique large ‘omic’ datasets (e.g., transcripts, proteins, lipids, metabolites and immune responses), integrated models and tools for the use and benefit of the research community at large. This unique and integrated combination of ‘omic’ approaches represents a revolutionary platform to identify, develop and evaluate new diagnostic tools, antimalarial drugs and vaccines for different types of malaria parasites.
In parallel, live imaging, including multi-photon approaches, has contributed to the understanding of CM pathogenesis, notably its haemodynamics (Nacer et al., 2014) and its immune cell mobilisation (Pai et al., 2014) components. Recently, in experimental CM, vibrational spectroscopies provided evidence of peroxidative stress and protein oxidation within cerebellar gray matter, which were co-localised with elevated non-haeme iron at the site of microhaemorrhages. A novel combination of chemical probe-free, multimodal imaging to quantify molecular markers of disturbed energy metabolism and peroxidative stress thus provides new insights into understanding CM pathogenesis (Hackett et al., 2015).
10. Conclusions and future perspectives
Despite the recent leap in our understanding of pathogenetic mechanisms leading to severe malaria, the translational outputs to improve the clinical outcome of patients remain meager. Collaborative and multidisciplinary approaches using clinical samples from field sites in endemic areas, in vitro and ex vivo models, as well as animal models of the disease, are crucial to allow global advances in the fight not only against severe falciparum malaria, but also emerging public health issues such as severe malaria caused by P. vivax and P. knowlesi.
Highlights.
The latest breakthroughs in severe malaria pathogenesis are presented.
The most recent insights into parasite and host-related mechanisms underlying development of cerebral malaria are reported.
In addition, updates in other severe falciparum and non-falciparum severe malaria forms are also provided.
Acknowledgments
Research reported in this publication was supported by the National Institute of Allergy and Infectious Diseases of the National Institutes of Health (USA) under Award Number U19AI089676, as well as by the National Health and Medical Research Council (Australia), the Rebecca L. Cooper Foundation (Australia) and the Australian Research Council (Australia).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Adams Y, Kuhnrae P, Higgins MK, Ghumra A, Rowe JA. Rosetting Plasmodium falciparum-infected erythrocytes bind to human brain microvascular endothelial cells in vitro, demonstrating a dual adhesion phenotype mediated by distinct P. falciparum erythrocyte membrane protein 1 domains. Infect Immun. 2014;82:949–959. doi: 10.1128/IAI.01233-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aird WC, Mosnier LO, Fairhurst RM. Plasmodium falciparum picks (on) EPCR. Blood. 2014;123:163–167. doi: 10.1182/blood-2013-09-521005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson DC, Lapp SA, Akinyi S, Meyer EV, Barnwell JW, Korir-Morrison C, Galinski MR. Plasmodium vivax trophozoite-stage proteomes. J Proteomics. 2015;115:157–176. doi: 10.1016/j.jprot.2014.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ataide R, Murillo O, Dombrowski JG, Souza RM, Lima FA, Lima GF, Hristov AD, Valle SC, Di Santi SM, Epiphanio S, Marinho CR. Malaria in Pregnancy Interacts with and Alters the Angiogenic Profiles of the Placenta. PLoS Negl Trop Dis. 2015;9:e0003824. doi: 10.1371/journal.pntd.0003824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aung NM, Kaung M, Kyi TT, Kyaw MP, Min M, Htet ZW, Anstey NM, Kyi MM, Hanson J. The Safety of a Conservative Fluid Replacement Strategy in Adults Hospitalised with Malaria. PloS One. 2015;10:e0143062. doi: 10.1371/journal.pone.0143062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Avril M, Bernabeu M, Benjamin M, Brazier AJ, Smith JD. Interaction between Endothelial Protein C Receptor and Intercellular Adhesion Molecule 1 to Mediate Binding of Plasmodium falciparum-Infected Erythrocytes to Endothelial Cells. mBio. 2016;7:e00615. doi: 10.1128/mBio.00615-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Avril M, Cartwright MM, Hathaway MJ, Hommel M, Elliott SR, Williamson K, Narum DL, Duffy PE, Fried M, Beeson JG, Smith JD. Immunization with VAR2CSA-DBL5 recombinant protein elicits broadly cross-reactive antibodies to placental Plasmodium falciparum-infected erythrocytes. Infect Immun. 2010;78:2248–2256. doi: 10.1128/IAI.00410-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ay F, Bunnik EM, Varoquaux N, Vert JP, Noble WS, Le Roch KG. Multiple dimensions of epigenetic gene regulation in the malaria parasite Plasmodium falciparum: gene regulation via histone modifications, nucleosome positioning and nuclear architecture in P. falciparum. BioEssays: News Rev Mol Cell Dev Biol. 2015;37:182–194. doi: 10.1002/bies.201400145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barber BE, William T, Grigg MJ, Parameswaran U, Piera KA, Price RN, Yeo TW, Anstey NM. Parasite biomass-related inflammation, endothelial activation, microvascular dysfunction and disease severity in vivax malaria. PLoS Pathog. 2015;11:e1004558. doi: 10.1371/journal.ppat.1004558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barrera V, Hiscott PS, Craig AG, White VA, Milner DA, Beare NA, MacCormick IJ, Kamiza S, Taylor TE, Molyneux ME, Harding SP. Severity of retinopathy parallels the degree of parasite sequestration in the eyes and brains of malawian children with fatal cerebral malaria. J Infect Dis. 2015;211:1977–1986. doi: 10.1093/infdis/jiu592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernabeu M, Danziger SA, Avril M, Vaz M, Babar PH, Brazier AJ, Herricks T, Maki JN, Pereira L, Mascarenhas A, Gomes E, Chery L, Aitchison JD, Rathod PK, Smith JD. Severe adult malaria is associated with specific PfEMP1 adhesion types and high parasite biomass. Proc Natl Acad Sci (USA) 2016;113:E3270–E3279. doi: 10.1073/pnas.1524294113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biswas AK, Hafiz A, Banerjee B, Kim KS, Datta K, Chitnis CE. Plasmodium falciparum uses gC1qR/HABP1/p32 as a receptor to bind to vascular endothelium and for platelet-mediated clumping. PLoS Pathog. 2007;3:1271–1280. doi: 10.1371/journal.ppat.0030130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brancucci NM, Bertschi NL, Zhu L, Niederwieser I, Chin WH, Wampfler R, Freymond C, Rottmann M, Felger I, Bozdech Z, Voss TS. Heterochromatin protein 1 secures survival and transmission of malaria parasites. Cell Host Microbe. 2014;16:165–176. doi: 10.1016/j.chom.2014.07.004. [DOI] [PubMed] [Google Scholar]
- Brown HC, Chau TT, Mai NT, Day NP, Sinh DX, White NJ, Hien TT, Farrar J, Turner GD. Blood-brain barrier function in cerebral malaria and CNS infections in Vietnam. Neurology. 2000;55:104–111. doi: 10.1212/wnl.55.1.104. [DOI] [PubMed] [Google Scholar]
- Carlson J, Helmby H, Hill AV, Brewster D, Greenwood BM, Wahlgren M. Human cerebral malaria: association with erythrocyte rosetting and lack of anti-rosetting antibodies. Lancet. 1990;336:1457–1460. doi: 10.1016/0140-6736(90)93174-n. [DOI] [PubMed] [Google Scholar]
- Coleman BI, Skillman KM, Jiang RH, Childs LM, Altenhofen LM, Ganter M, Leung Y, Goldowitz I, Kafsack BF, Marti M, Llinas M, Buckee CO, Duraisingh MT. A Plasmodium falciparum histone deacetylase regulates antigenic variation and gametocyte conversion. Cell Host Microbe. 2014;16:177–186. doi: 10.1016/j.chom.2014.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daniyan MO, Boshoff A, Prinsloo E, Pesce ER, Blatch GL. The Malarial Exported PFA0660w Is an Hsp40 Co-Chaperone of PfHsp70-x. PloS One. 2016;11:e0148517. doi: 10.1371/journal.pone.0148517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Desai M, ter Kuile FO, Nosten F, McGready R, Asamoa K, Brabin B, Newman RD. Epidemiology and burden of malaria in pregnancy. Lancet Infect Dis. 2007;7:93–104. doi: 10.1016/S1473-3099(07)70021-X. [DOI] [PubMed] [Google Scholar]
- Doritchamou JY, Herrera R, Aebig JA, Morrison R, Nguyen V, Reiter K, Shimp R, MacDonald NJ, Narum DL, Fried M, Duffy PE. VAR2CSA domain-specific analysis of naturally acquired functional antibodies to P. falciparum placental malaria. J Infect Dis. 2016;214:577–586. doi: 10.1093/infdis/jiw197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dorovini-Zis K, Schmidt K, Huynh H, Fu W, Whitten RO, Milner D, Kamiza S, Molyneux M, Taylor TE. The neuropathology of fatal cerebral malaria in malawian children. Am J Pathol. 2011;178:2146–2158. doi: 10.1016/j.ajpath.2011.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fried M, Duffy PE. Designing a VAR2CSA-based vaccine to prevent placental malaria. Vaccine. 2015;33:7483–7488. doi: 10.1016/j.vaccine.2015.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gillrie MR, Avril M, Brazier AJ, Davis SP, Stins MF, Smith JD, Ho M. Diverse functional outcomes of Plasmodium falciparum ligation of EPCR: potential implications for malarial pathogenesis. Cell Micro. 2015;17:1883–1899. doi: 10.1111/cmi.12479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilson PR, Chisholm SA, Crabb BS, de Koning-Ward TF. Host cell remodelling in malaria parasites: a new pool of potential drug targets. Int J Parasitol. 2016 doi: 10.1016/j.ijpara.2016.06.001. This issue. [DOI] [PubMed] [Google Scholar]
- Goel S, Palmkvist M, Moll K, Joannin N, Lara P, Akhouri RR, Moradi N, Ojemalm K, Westman M, Angeletti D, Kjellin H, Lehtio J, Blixt O, Idestrom L, Gahmberg CG, Storry JR, Hult AK, Olsson ML, von Heijne G, Nilsson I, Wahlgren M. RIFINs are adhesins implicated in severe Plasmodium falciparum malaria. Nat Med. 2015;21:314–317. doi: 10.1038/nm.3812. [DOI] [PubMed] [Google Scholar]
- Greiner J, Dorovini-Zis K, Taylor TE, Molyneux ME, Beare NA, Kamiza S, White VA. Correlation of hemorrhage, axonal damage, and blood-tissue barrier disruption in brain and retina of Malawian children with fatal cerebral malaria. Front Cell Infect Microbiol. 2015;5:18. doi: 10.3389/fcimb.2015.00018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hackett MJ, Aitken JB, El-Assaad F, McQuillan JA, Carter EA, Ball HJ, Tobin MJ, Paterson D, de Jonge MD, Siegele R, Cohen DD, Vogt S, Grau GE, Hunt NH, Lay PA. Mechanisms of murine cerebral malaria: Multimodal imaging of altered cerebral metabolism and protein oxidation at hemorrhage sites. Sci Adv. 2015;1:e1500911. doi: 10.1126/sciadv.1500911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Handunnetti SM, David PH, Perera KL, Mendis KN. Uninfected erythrocytes form “rosettes” around Plasmodium falciparum infected erythrocytes. Am J Trop Med Hyg. 1989;40:115–118. doi: 10.4269/ajtmh.1989.40.115. [DOI] [PubMed] [Google Scholar]
- Hanson J, Anstey NM, Bihari D, White NJ, Day NP, Dondorp AM. The fluid management of adults with severe malaria. Crit Care. 2014;18:642. doi: 10.1186/s13054-014-0642-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris LM, Merrick CJ. G-quadruplexes in pathogens: a common route to virulence control? PLoS Pathog. 2015;11:e1004562. doi: 10.1371/journal.ppat.1004562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkes M, Opoka RO, Namasopo S, Miller C, Conroy AL, Serghides L, Kim H, Thampi N, Liles WC, John CC, Kain KC. Nitric oxide for the adjunctive treatment of severe malaria: hypothesis and rationale. Med Hypotheses. 2011;77:437–444. doi: 10.1016/j.mehy.2011.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hendriksen IC, Mwanga-Amumpaire J, von Seidlein L, Mtove G, White LJ, Olaosebikan R, Lee SJ, Tshefu AK, Woodrow C, Amos B, Karema C, Saiwaew S, Maitland K, Gomes E, Pan-Ngum W, Gesase S, Silamut K, Reyburn H, Joseph S, Chotivanich K, Fanello CI, Day NP, White NJ, Dondorp AM. Diagnosing severe falciparum malaria in parasitaemic African children: a prospective evaluation of plasma PfHRP2 measurement. PLoS Med. 2012;9:e1001297. doi: 10.1371/journal.pmed.1001297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoffmann A, Pfeil J, Alfonso J, Kurz FT, Sahm F, Heiland S, Monyer H, Bendszus M, Mueller AK, Helluy X, Pham M. Experimental Cerebral Malaria Spreads along the Rostral Migratory Stream. PLoS Pathog. 2016;12:e1005470. doi: 10.1371/journal.ppat.1005470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hommel M, Elliott SR, Soma V, Kelly G, Fowkes FJ, Chesson JM, Duffy MF, Bockhorst J, Avril M, Mueller I, Raiko A, Stanisic DI, Rogerson SJ, Smith JD, Beeson JG. Evaluation of the antigenic diversity of placenta-binding Plasmodium falciparum variants and the antibody repertoire among pregnant women. Infect Immun. 2010;78:1963–1978. doi: 10.1128/IAI.01365-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hviid L, Jensen AT. PfEMP1 - A Parasite Protein Family of Key Importance in Plasmodium falciparum Malaria Immunity and Pathogenesis. Adv Parasitol. 2015;88:51–84. doi: 10.1016/bs.apar.2015.02.004. [DOI] [PubMed] [Google Scholar]
- Jespersen JS, Wang CW, Mkumbaye SI, Minja DT, Petersen B, Turner L, Petersen JE, Lusingu JP, Theander TG, Lavstsen T. Plasmodium falciparum var genes expressed in children with severe malaria encode CIDRalpha1 domains. EMBO Mol Med. 2016;8:839–850. doi: 10.15252/emmm.201606188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Josling GA, Petter M, Oehring SC, Gupta AP, Dietz O, Wilson DW, Schubert T, Langst G, Gilson PR, Crabb BS, Moes S, Jenoe P, Lim SW, Brown GV, Bozdech Z, Voss TS, Duffy MF. A Plasmodium falciparum Bromodomain Protein Regulates Invasion Gene Expression. Cell Host Microbe. 2015;17:741–751. doi: 10.1016/j.chom.2015.05.009. [DOI] [PubMed] [Google Scholar]
- Joyner C, Barnwell JW, Galinski MR. No more monkeying around: primate malaria model systems are key to understanding Plasmodium vivax liver-stage biology, hypnozoites, and relapses. Front Microbiol. 2015;6:145. doi: 10.3389/fmicb.2015.00145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalanon M, Bargieri D, Sturm A, Matthews K, Ghosh S, Goodman CD, Thiberge S, Mollard V, McFadden GI, Menard R, de Koning-Ward TF. The Plasmodium translocon of exported proteins component EXP2 is critical for establishing a patent malaria infection in mice. Cell Microbiol. 2016;18:399–412. doi: 10.1111/cmi.12520. [DOI] [PubMed] [Google Scholar]
- Karmodiya K, Pradhan SJ, Joshi B, Jangid R, Reddy PC, Galande S. A comprehensive epigenome map of Plasmodium falciparum reveals unique mechanisms of transcriptional regulation and identifies H3K36me2 as a global mark of gene suppression. Epigenetics Chromatin. 2015;8:32. doi: 10.1186/s13072-015-0029-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lapp SA, Mok S, Zhu L, Wu H, Preiser PR, Bozdech Z, Galinski MR. Plasmodium knowlesi gene expression differs in ex vivo compared to in vitro blood-stage cultures. Malaria J. 2015;14:110. doi: 10.1186/s12936-015-0612-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maier AG, Cooke BM, Cowman AF, Tilley L. Malaria parasite proteins that remodel the host erythrocyte. Nat Rev Microbiol. 2009;7:341–354. doi: 10.1038/nrmicro2110. [DOI] [PubMed] [Google Scholar]
- Manning L, Laman M, Davis WA, Davis TM. Clinical features and outcome in children with severe Plasmodium falciparum malaria: a meta-analysis. PloS One. 2014;9:e86737. doi: 10.1371/journal.pone.0086737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maude RJ, Barkhof F, Hassan MU, Ghose A, Hossain A, Abul Faiz M, Choudhury E, Rashid R, Abu Sayeed A, Charunwatthana P, Plewes K, Kingston H, Maude RR, Silamut K, Day NP, White NJ, Dondorp AM. Magnetic resonance imaging of the brain in adults with severe falciparum malaria. Malaria J. 2014;13:177. doi: 10.1186/1475-2875-13-177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mayor A, Bardaji A, Macete E, Nhampossa T, Fonseca AM, Gonzalez R, Maculuve S, Cistero P, Ruperez M, Campo J, Vala A, Sigauque B, Jimenez A, Machevo S, de la Fuente L, Nhama A, Luis L, Aponte JJ, Acacio S, Nhacolo A, Chitnis C, Dobano C, Sevene E, Alonso PL, Menendez C. Changing Trends in P. falciparum Burden, Immunity, and Disease in Pregnancy. New Engl J Med. 2015;373:1607–1617. doi: 10.1056/NEJMoa1406459. [DOI] [PubMed] [Google Scholar]
- Mayor A, Hafiz A, Bassat Q, Rovira-Vallbona E, Sanz S, Machevo S, Aguilar R, Cistero P, Sigauque B, Menendez C, Alonso PL, Chitnis CE. Association of severe malaria outcomes with platelet-mediated clumping and adhesion to a novel host receptor. PloS One. 2011;6:e19422. doi: 10.1371/journal.pone.0019422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDonald CR, Darling AM, Conroy AL, Tran V, Cabrera A, Liles WC, Wang M, Aboud S, Urassa W, Fawzi WW, Kain KC. Inflammatory and Angiogenic Factors at Mid-Pregnancy Are Associated with Spontaneous Preterm Birth in a Cohort of Tanzanian Women. PloS One. 2015a;10:e0134619. doi: 10.1371/journal.pone.0134619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDonald CR, Tran V, Kain KC. Complement Activation in Placental Malaria. Front Microbiol. 2015b;6:1460. doi: 10.3389/fmicb.2015.01460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Medana IM, Day NP, Sachanonta N, Mai NT, Dondorp AM, Pongponratn E, Hien TT, White NJ, Turner GD. Coma in fatal adult human malaria is not caused by cerebral oedema. Malaria J. 2011;10:267. doi: 10.1186/1475-2875-10-267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohanty S, Mishra SK, Patnaik R, Dutt AK, Pradhan S, Das B, Patnaik J, Mohanty AK, Lee SJ, Dondorp AM. Brain swelling and mannitol therapy in adult cerebral malaria: a randomized trial. Clin Infect Dis. 2011;53:349–355. doi: 10.1093/cid/cir405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moxon CA, Chisala NV, Wassmer SC, Taylor TE, Seydel KB, Molyneux ME, Faragher B, Kennedy N, Toh CH, Craig AG, Heyderman RS. Persistent endothelial activation and inflammation after Plasmodium falciparum Infection in Malawian children. J Infect Dis. 2014;209:610–615. doi: 10.1093/infdis/jit419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moxon CA, Wassmer SC, Milner DA, Jr, Chisala NV, Taylor TE, Seydel KB, Molyneux ME, Faragher B, Esmon CT, Downey C, Toh CH, Craig AG, Heyderman RS. Loss of endothelial protein C receptors links coagulation and inflammation to parasite sequestration in cerebral malaria in African children. Blood. 2013;122:842–851. doi: 10.1182/blood-2013-03-490219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nacer A, Movila A, Sohet F, Girgis NM, Gundra UM, Loke P, Daneman R, Frevert U. Experimental cerebral malaria pathogenesis--hemodynamics at the blood brain barrier. PLoS Pathog. 2014;10:e1004528. doi: 10.1371/journal.ppat.1004528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Sullivan JM, Preston RJ, O’Regan N, O’Donnell JS. Emerging roles for hemostatic dysfunction in malaria pathogenesis. Blood. 2016;127:2281–2288. doi: 10.1182/blood-2015-11-636464. [DOI] [PubMed] [Google Scholar]
- Padmanabhan B, Mathur S, Manjula R, Tripathi S. Bromodomain and extra-terminal (BET) family proteins: New therapeutic targets in major diseases. J Biosci. 2016;41:295–311. doi: 10.1007/s12038-016-9600-6. [DOI] [PubMed] [Google Scholar]
- Pai S, Qin J, Cavanagh L, Mitchell A, El-Assaad F, Jain R, Combes V, Hunt NH, Grau GE, Weninger W. Real-time imaging reveals the dynamics of leukocyte behaviour during experimental cerebral malaria pathogenesis. PLoS Pathog. 2014;10:e1004236. doi: 10.1371/journal.ppat.1004236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pain A, Ferguson DJ, Kai O, Urban BC, Lowe B, Marsh K, Roberts DJ. Platelet-mediated clumping of Plasmodium falciparum-infected erythrocytes is a common adhesive phenotype and is associated with severe malaria. Proc Natl Acad Sci (USA) 2001;98:1805–1810. doi: 10.1073/pnas.98.4.1805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Penet MF, Viola A, Confort-Gouny S, Le Fur Y, Duhamel G, Kober F, Ibarrola D, Izquierdo M, Coltel N, Gharib B, Grau GE, Cozzone PJ. Imaging experimental cerebral malaria in vivo: significant role of ischemic brain edema. J Neurosci. 2005;25:7352–7358. doi: 10.1523/JNEUROSCI.1002-05.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petersen JE, Bouwens EA, Tamayo I, Turner L, Wang CW, Stins M, Theander TG, Hermida J, Mosnier LO, Lavstsen T. Protein C system defects inflicted by the malaria parasite protein PfEMP1 can be overcome by a soluble EPCR variant. Thromb Haemost. 2015;114:1038–1048. doi: 10.1160/TH15-01-0018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Potchen MJ, Kampondeni SD, Seydel KB, Birbeck GL, Hammond CA, Bradley WG, DeMarco JK, Glover SJ, Ugorji JO, Latourette MT, Siebert JE, Molyneux ME, Taylor TE. Acute brain MRI findings in 120 Malawian children with cerebral malaria: new insights into an ancient disease. AJNR Am J Neuroradiol. 2012;33:1740–1746. doi: 10.3174/ajnr.A3035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogerson SJ, Pollina E, Getachew A, Tadesse E, Lema VM, Molyneux ME. Placental monocyte infiltrates in response to Plasmodium falciparum malaria infection and their association with adverse pregnancy outcomes. American J Trop Med Hyg. 2003;68:115–119. [PubMed] [Google Scholar]
- Rowe A, Obeiro J, Newbold CI, Marsh K. Plasmodium falciparum rosetting is associated with malaria severity in Kenya. Infect Immun. 1995;63:2323–2326. doi: 10.1128/iai.63.6.2323-2326.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rowe JA, Claessens A, Corrigan RA, Arman M. Adhesion of Plasmodium falciparum-infected erythrocytes to human cells: molecular mechanisms and therapeutic implications. Expert Rev Mol Med. 2009;11:e16. doi: 10.1017/S1462399409001082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rowe JA, Handel IG, Thera MA, Deans AM, Lyke KE, Kone A, Diallo DA, Raza A, Kai O, Marsh K, Plowe CV, Doumbo OK, Moulds JM. Blood group O protects against severe Plasmodium falciparum malaria through the mechanism of reduced rosetting. Proc Natl Acad Sci (USA) 2007;104:17471–17476. doi: 10.1073/pnas.0705390104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rowe JA, Shafi J, Kai OK, Marsh K, Raza A. Nonimmune IgM, but not IgG binds to the surface of Plasmodium falciparum-infected erythrocytes and correlates with rosetting and severe malaria. Am J Trop Med Hyg. 2002;66:692–699. doi: 10.4269/ajtmh.2002.66.692. [DOI] [PubMed] [Google Scholar]
- Sahu PK, Satpathi S, Behera PK, Mishra SK, Mohanty S, Wassmer SC. Pathogenesis of cerebral malaria: new diagnostic tools, biomarkers, and therapeutic approaches. Front Cell Infect Microbiol. 2015;5:75. doi: 10.3389/fcimb.2015.00075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salinas JL, Kissinger JC, Jones DP, Galinski MR. Metabolomics in the fight against malaria. Memorias do Instituto Oswaldo Cruz. 2014;109:589–597. doi: 10.1590/0074-0276140043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Serghides L, Kim H, Lu Z, Kain DC, Miller C, Francis RC, Liles WC, Zapol WM, Kain KC. Inhaled nitric oxide reduces endothelial activation and parasite accumulation in the brain, and enhances survival in experimental cerebral malaria. PloS One. 2011;6:e27714. doi: 10.1371/journal.pone.0027714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seydel KB, Kampondeni SD, Valim C, Potchen MJ, Milner DA, Muwalo FW, Birbeck GL, Bradley WG, Fox LL, Glover SJ, Hammond CA, Heyderman RS, Chilingulo CA, Molyneux ME, Taylor TE. Brain swelling and death in children with cerebral malaria. New Engl J Med. 2015;372:1126–1137. doi: 10.1056/NEJMoa1400116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Souza RM, Ataide R, Dombrowski JG, Ippolito V, Aitken EH, Valle SN, Alvarez JM, Epiphanio S, Marinho CR. Placental histopathological changes associated with Plasmodium vivax infection during pregnancy. PLoS Negl Trop Dis. 2013;7:e2071. doi: 10.1371/journal.pntd.0002071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stevenson L, Laursen E, Cowan GJ, Bandoh B, Barfod L, Cavanagh DR, Andersen GR, Hviid L. alpha2-Macroglobulin Can Crosslink Multiple Plasmodium falciparum Erythrocyte Membrane Protein 1 (PfEMP1) Molecules and May Facilitate Adhesion of Parasitized Erythrocytes. PLoS Pathog. 2015;11:e1005022. doi: 10.1371/journal.ppat.1005022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Storm J, Craig AG. Pathogenesis of cerebral malaria-inflammation and cytoadherence. Front Cell Infect Microbiol. 2014;4:100. doi: 10.3389/fcimb.2014.00100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor TE, Fu WJ, Carr RA, Whitten RO, Mueller JS, Fosiko NG, Lewallen S, Liomba NG, Molyneux ME. Differentiating the pathologies of cerebral malaria by postmortem parasite counts. Nat Med. 2004;10:143–145. doi: 10.1038/nm986. [DOI] [PubMed] [Google Scholar]
- Turner L, Lavstsen T, Berger SS, Wang CW, Petersen JE, Avril M, Brazier AJ, Freeth J, Jespersen JS, Nielsen MA, Magistrado P, Lusingu J, Smith JD, Higgins MK, Theander TG. Severe malaria is associated with parasite binding to endothelial protein C receptor. Nature. 2013;498:502–505. doi: 10.1038/nature12216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warrell DA, Looareesuwan S, Phillips RE, White NJ, Warrell MJ, Chapel HM, Areekul S, Tharavanij S. Function of the blood-cerebrospinal fluid barrier in human cerebral malaria: rejection of the permeability hypothesis. Am J Trop Med Hyg. 1986;35:882–889. doi: 10.4269/ajtmh.1986.35.882. [DOI] [PubMed] [Google Scholar]
- Wassmer SC, Combes V, Grau GE. Platelets and microparticles in cerebral malaria: the unusual suspects. Drug Discov Today Dis Mech. 2011a;8:e15–e23. [Google Scholar]
- Wassmer SC, Moxon CA, Taylor T, Grau GE, Molyneux ME, Craig AG. Vascular endothelial cells cultured from patients with cerebral or uncomplicated malaria exhibit differential reactivity to TNF. Cell Microbiol. 2011b;13:198–209. doi: 10.1111/j.1462-5822.2010.01528.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wassmer SC, Taylor T, Maclennan CA, Kanjala M, Mukaka M, Molyneux ME, Grau GE. Platelet-induced clumping of Plasmodium falciparum-infected erythrocytes from Malawian patients with cerebral malaria-possible modulation in vivo by thrombocytopenia. J Infect Dis. 2008;197:72–78. doi: 10.1086/523761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wassmer SC, Taylor TE, Rathod PK, Mishra SK, Mohanty S, Arevalo-Herrera M, Duraisingh MT, Smith JD. Investigating the Pathogenesis of Severe Malaria: A Multidisciplinary and Cross-Geographical Approach. Am J Trop Med Hyg. 2015;93:42–56. doi: 10.4269/ajtmh.14-0841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White NJ, Turner GD, Day NP, Dondorp AM. Lethal malaria: Marchiafava and Bignami were right. J Infect Dis. 2013;208:192–198. doi: 10.1093/infdis/jit116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeo TW, Lampah DA, Gitawati R, Tjitra E, Kenangalem E, McNeil YR, Darcy CJ, Granger DL, Weinberg JB, Lopansri BK, Price RN, Duffull SB, Celermajer DS, Anstey NM. Impaired nitric oxide bioavailability and L-arginine reversible endothelial dysfunction in adults with falciparum malaria. J Exp Med. 2007;204:2693–2704. doi: 10.1084/jem.20070819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeo TW, Lampah DA, Kenangalem E, Tjitra E, Weinberg JB, Granger DL, Price RN, Anstey NM. Decreased endothelial nitric oxide bioavailability, impaired microvascular function, and increased tissue oxygen consumption in children with falciparum malaria. J Infect Dis. 2014;210:1627–1632. doi: 10.1093/infdis/jiu308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeo TW, Lampah DA, Rooslamiati I, Gitawati R, Tjitra E, Kenangalem E, Price RN, Duffull SB, Anstey NM. A randomized pilot study of L-arginine infusion in severe falciparum malaria: preliminary safety, efficacy and pharmacokinetics. PloS One. 2013;8:e69587. doi: 10.1371/journal.pone.0069587. [DOI] [PMC free article] [PubMed] [Google Scholar]


