Abstract
Aims and Objectives:
To evaluate the effect of bromelain on pain and swelling after surgical removal of third molars.
Materials and Methods:
A prospective randomized clinical study was conducted among 40 patients requiring surgical removal of impacted mandibular third molars. All the impacted molars were surgically removed, and the patients were administered bromelain along with amoxicillin. Patients were recalled on day 1, day 3, and day 7 for postoperative pain assessment using visual analogue scale (VAS) and postoperative swelling assessment using facial reference points tragus and pogonion. VAS score was statistically analyzed using repeated analysis of variance with post-hoc Bonferroni test postoperatively on day 1, day 3, and day 7 using the Statistical Package for the Social Sciences software version 14.
Results:
Out of the total 40 patients, bromelain was effective in 28 (70%) patients. In these patients, there was reduction in swelling and pain after taking bromelain.
Conclusion:
Bromelain can be used as a successful oral enzyme therapy for oral surgery patients, especially after removal of impacted third molars.
Key words: Bromelain, impacted teeth, postoperative edema, third molar, trypsin
INTRODUCTION
Studies have shown that the most common impacted teeth are third molars (98%) followed by maxillary canines (1.3%).[1] Removal of impacted teeth needs a surgical procedure where soft tissue flap is raised and associated tooth or bone or both are cut and the tooth is removed. Such surgical procedures usually result in injury of tissues, involving inflammation and repair processes.[2]
In order to avoid or minimize post surgical complications, such as pain, swelling, and trismus, surgeons have either modified surgical techniques, such as using lasers and cryotherapy, or advised the patients to use proteolytic enzymes, such as trypsin, chymotrypsin, papain, serratiopeptidase, and bromelain (pineapple enzyme), along with routine antibiotics, analgesics, and corticosteroids.[3,4] The benefits of administering enzymes after surgical procedures demonstrated both in vitro and in vivo are anti-inflammatory, antithrombotic, and fibrinolytic, thereby minimizing postoperative complications.[5]
Bromelain is extracted from the stem and fruit of pineapple plant. In patients with osteoarthritis, it has been used as an alternative to nonsteroidal anti-inflammatory drugs (NSAIDs).[6]
Few studies have been conducted to determine the effect of bromelain on reducing the inflammation after extraction of third molars, demonstrating its anti-inflammatory and antiedematous action.[7,8,9] Our study was carried out to assess the effect of proteolytic enzyme bromelain in controlling pain and swelling after surgical removal of lower third molars.
Aims and Objectives
To evaluate the effect of proteolytic enzyme bromelain on controlling pain and swelling after surgical removal of third molars by visual analogue scale (VAS) and using facial reference points (tragus to pogonion distance), respectively.
MATERIALS AND METHODS
A prospective randomized clinical study (RCT) was carried out after obtaining institutional ethical committee approval among 40 patients (randomly selected) requiring surgical removal of impacted mandibular third molars who reported to the department of oral and maxillofacial surgery from October 2012 to October 2014.
Inclusion criteria
Patients in the age group of 17–45 years
Patients with unilateral/bilateral impacted mandibular third molars diagnosed for surgical extraction.
Exclusion criteria
Patients with known severe systemic diseases contraindicating tooth extraction
Known mentally challenged patients, and patients who are unable to communicate
Pregnant and lactating women
Patients on anticoagulant therapy
Patients allergic to bromelain
Immunocompromised patients.
A complete history of all the patients was taken and thorough clinical examination was done to rule out any systemic problems [Figure 1]. Orthopantomogram (OPG) and intraoral periapical radiographs for impacted mandibular third molars were taken after obtaining informed consent from the patients. The difficulty index for tooth removal was assessed using Winter's WAR lines [Figure 2]. Preoperative Tragus to Pogonion (TR-PG) distance was measured using a flexible metal scale [Figure 3].
Figure 1.

Intraoral view
Figure 2.
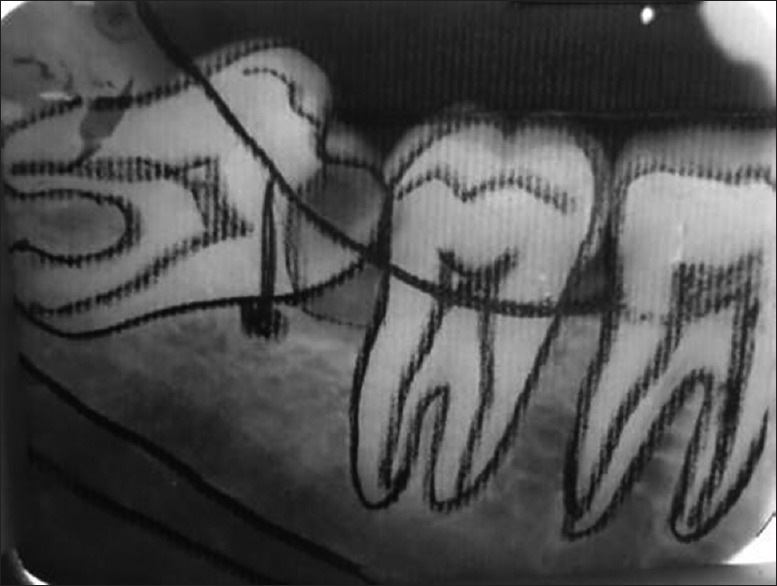
Winter's WAR lines assessment
Figure 3.
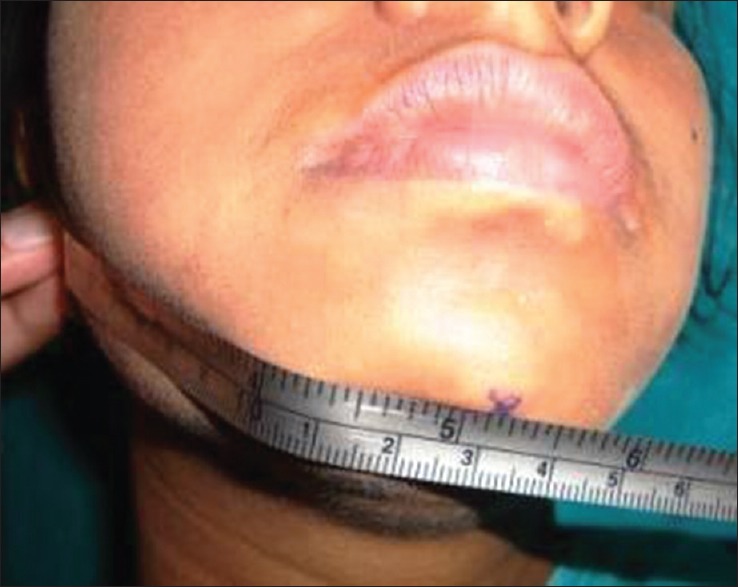
Measuring tragus to pogonion distance
Surgical procedure
To standardize the surgical procedure, all surgical procedures were performed by the same surgeon. Intraorally, inferior alveolar, lingual, and long buccal nerve blocks were given using 2% solution of lignocaine hydrochloride with 1:200000 adrenaline followed by the surgical removal of mandibular third molar using the standard procedure. After socket debridement, the wound was primarily closed with 3–0 silk sutures. Postoperatively, all patients were administered amoxicillin 500 mg TID for 5 days and tab bromozyme DT 200 mg BD for 5 days. Patients were recalled on day 1, day 3, and day 7 for postoperative pain assessment (VAS scale) and postoperative swelling assessment (facial reference points). The suture removal was done 7 days postoperatively.
RESULTS
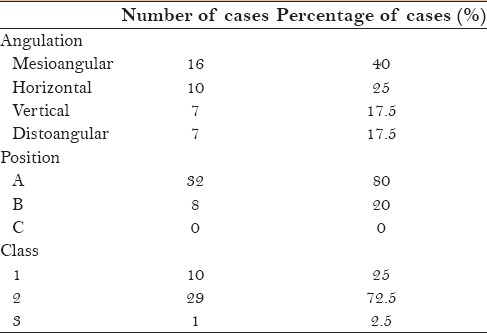
Out of the total 40 patients, 16 were with mesioangular (40%), 10 with horizontal (25%), 7 each with vertical and distoangular (17.5%) impactions. Thirty-two were position A (80%), 8 position B (20%), 10 class I (25%), 29 class II (72.5%), and 1 class III (2.5%) [Table 1, Graph 1].
Table 1.
Classification of impacted teeth based on angulation, position and class (number and percentage of cases)
Graph 1.
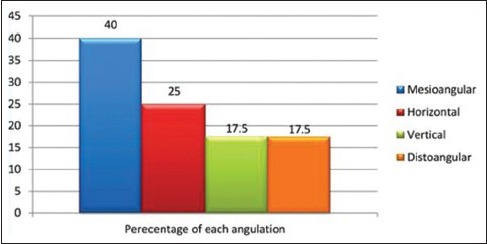
Angulation classification of impacted teeth
Effectiveness of bromelain for each difficulty index score (mild, moderate, and difficult) were evaluated. Out of the 28 cases, 13 were with mild score (46.4%), 10 with moderate score (35.7%), and 5 with difficult score (17.9%) [Table 2, Graph 2].
Table 2.
Effectiveness of bromelain for each difficulty index score-mild, moderate, and severe (number and percentage of cases)
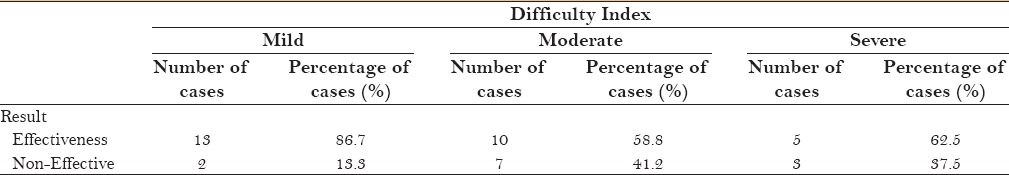
Graph 2.
Effectiveness of bromelain for each difficulty index score
In 28 cases, effectiveness of bromelain among each subtypes – angulation (mesioangular, horizontal, vertical, and distoangular), position (A, B, and C), class (I, II, and III) were evaluated. In this, 14 were mesioangular (50%), 6 were horizontal (21.4%), 5 were vertical (17.9%), and 3 were distoangular (10.7%) impactions. Twenty-one were position A (75%) and 7 position B (25%) impactions were observed. Eight class I (28.6%) and 20 class II (71.7%) types of impacted third molars were observed.
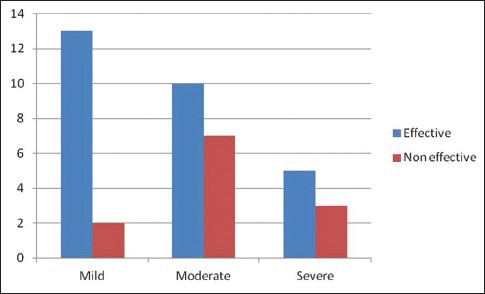
Assessment of pain
VAS score was statistically analyzed using repeated analysis of variance (ANOVA) with post-hoc Bonferroni test postoperatively on day 1, day 3, and day 7 [Table 3, Graph 3].
Table 3.
Pain assessment by visual analogue scale on days 1, 3, and 7
Graph 3.
Pain assessment by VAS score
Day 1: minimum VAS score was 3, maximum was 6, with a mean score of 4.86 (SD: 0.85).
Day 3: minimum VAS score was 2, maximum was 5, with a mean score 3.11 (SD: 0.88).
Day 7: minimum score was 0, maximum score was 2, with a mean score 0.89 (SD: 0.74).
VAS score was statistically analyzed using ANOVA with post-hoc Bonferroni test for each subtypes – angulation (mesioangular, horizontal, vertical, distoangular), position (A, B, and C), and class (I, II, and III) [Table 4].
Table 4.
Visual analogue scale score for each subtypes of impact teeth on days 1, 3, and 7
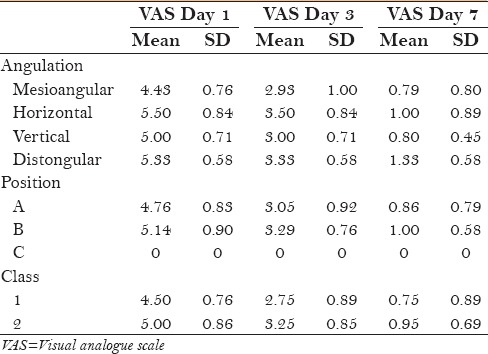
Day 1: Mean VAS score for mesioangular impactions was 4.43 (SD: 0.76), horizontal was 5.50 (SD: 0.84), vertical was 5.00 (SD: 0.71), and distoangular impactions was 5.33 (SD: 0.58).
Day 3: VAS score for mesioangular impactions was 2.93 (SD: 1.00), horizontal was 3.50 (SD: 0.84), vertical was 3.00 (SD: 0.71), and distoangular impactions was 3.33 (SD: 0.58).
Day 7: VAS score for mesioangular impactions was 0.79 (SD: 0.80), horizontal was 1.00 (SD: 0.89), vertical was 0.80 (SD: 0.45), and distoangular impactions was 1.33 (SD: 0.58).
Day 1: Mean VAS score for position A was 4.76 (SD: 0.83) and position B was 5.14 (SD: 0.90).
Day 3: VAS score for position A was 3.05 (SD: 0.92) and position B was 3.29 (SD: 0.76).
Day 7: VAS score for position A was 0.86 (SD: 0.79) and position B was 1.00 (SD: 0.58).
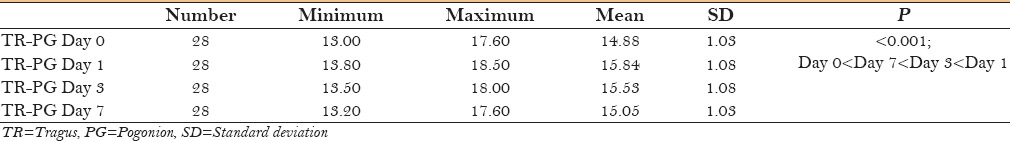
Assessment of swelling
In 28 cases, effect of bromelain on reduction of swelling on day 1, day 3, and day 7 was compared with preoperative value (TR-PG distance in cm), and the obtained data was analyzed using ANOVA with post-hoc Bonferroni test.
Preoperatively: minimum TR- PG distance was 13 cm and maximum was 17.60 cm, with a mean value of 14.88 cm (SD: 1.03).
Day 1: minimum distance was 13.80 cm, maximum was 18.50 cm, with a mean value of 15.84 cm (SD: 1.08).
Day 3: minimum distance was 13.50 cm, maximum was 18.00 cm, with a mean value of 15.53 cm (SD: 1.08).
Day 7: minimum distance was 13.20 cm, maximum was 17.60 cm, with a mean value of 15.05 cm (SD: 1.03) [Table 5 and Graph 4].
Table 5.
Assessment of swelling (tragus-pogonion distance) on preoperative day and days 1, 3, and 7
Graph 4.
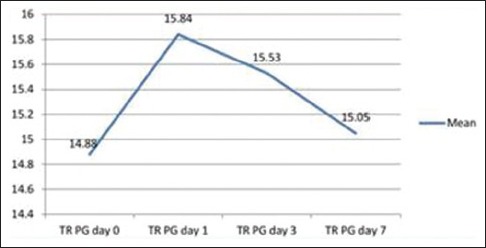
Assessment of Swelling
Similarly, effect of bromelain on reduction of swelling on day 1, day 3, and day 7 was compared with preoperative value (TR-PG distance in cm), and the results were analyzed using ANOVA with post-hoc Bonferroni test for each subtypes – angulation (mesioangular, horizontal, vertical, distoangular), position (A, B, and C), and class (I, II, and III) [Table 6].
Table 6.
Effect of bromelain on swelling reduction (tragus-pogonion distance) for each subtypes on preoperative day and days 1, 3, and 7
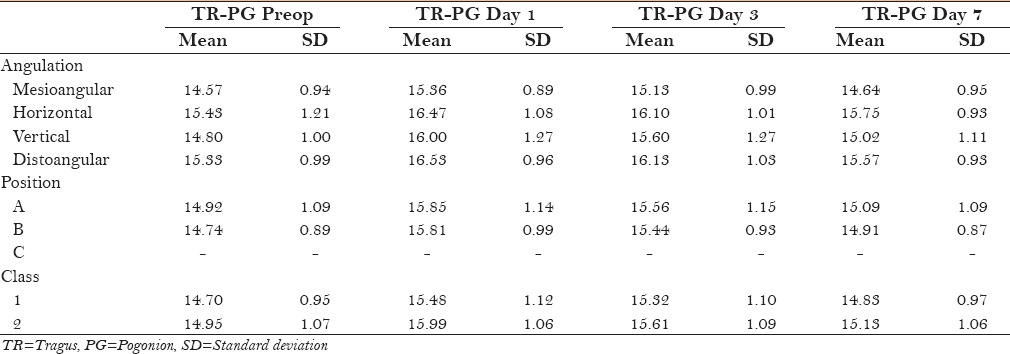
Mesioangular angulation
Preoperative mean TR-PG distance was 14.57 cm (SD: 0.94), on day 1 mean distance was 15.36 cm (SD: 0.89), on day 3 mean distance was 15.13 cm (SD: 0.99), and on day 7 mean distance was 14.64 cm (SD: 0.95).
Horizontal angulation
Preoperative mean TR-PG distance was 15.43 cm (SD: 1.21), on day 1 mean distance was 16.47 cm (SD: 1.08), on day 3 mean distance was 16.10 cm (SD: 1.01), and on day 7 mean distance was 15.75 cm (SD: 0.93).
Vertical angulation
Preoperative mean TR-PG distance was 14.80 cm (SD: 1.00), on day 1 mean distance was 16.00 cm (SD: 1.27), on day 3 mean distance was 15.60 cm (SD: 1.27), and on day 7 mean distance was 15.02 cm (SD: 1.11).
Distoangular angulation
Preoperative mean TR-PG distance was 15.33 cm (SD: 0.99), on day 1 mean distance was 16.53 cm (SD: 0.96), on day 3 mean distance was 16.13 cm (SD: 1.03), and on day 7 mean distance was 15.57 cm (SD: 0.93).
For position A
Preoperative mean TR-PG distance was 14.92 cm (SD: 1.09), on day 1 mean distance was 15.85 cm (SD: 1.14), on day 3 mean distance was 15.56 cm (SD: 1.15), and on day 7 mean distance was 15.09 cm (SD: 1.09).
For position B
Preoperative mean TR-PG distance was 14.74 cm (SD: 0.89), on day 1 mean distance was 15.81 cm (SD: 0.99), on day 3 mean distance was 15.44 cm (SD: 0.93), and on day 7 mean distance was 14.91 cm (SD: 0.87).
No effective cases were found for position C.
For class I
Preoperative mean TR-PG distance was 14.70 cm (SD: 0.95), on day 1 mean distance was 15.48 cm (SD: 1.12), on day 3 mean distance was 15.32 cm (SD: 1.10), and on day 7 mean distance was 14.83 cm (SD: 0.97).
For class II
Preoperative mean TR-PG distance was 14.95 cm (SD: 1.07), on day 1 mean distance was 15.99 cm (SD: 1.06), on day 3 mean distance was 15.61 cm (SD: 1.09), and on day 7 mean distance was 15.13 cm (SD: 1.06).
No effective cases were found for Class III.
In 12 failed cases, average VAS Score on day 1 and day 3 was calculated. On day 1, minimum VAS score was 6, maximum was 8, with a mean of 7 (SD: 0.60). Out of 12 patients, 6 patients did not continue bromelain after 2nd day because of consistent pain. On day 3, for 6 cases minimum VAS score was 5, maximum was 7, with a mean of 6.5 (SD: 0.84). The mean age of the patients was 27.72 years. Of the 40 patients, 26 were males (65%) and 14 were females (35%). Bromelain was effective in 28 (70%) patients and not effective in 12 (30%).
DISCUSSION
The common problems patients complain of after the surgical removal of impacted teeth are pain, swelling, and trismus. Various measures such as application of ice, analgesics, anti-inflammatory agents, and proteolytic enzymes have been practiced to minimize these complications.[2]
Bromelain is a blend of enzymes extracted from the stem and fruit of pineapple, Ananas comosus, and is known for its proteolytic action. It belongs to a family of sulfhydryl proteolytic enzymes, which also contain components such as acid phosphatase, peroxidase, many protease inhibitors, and organically bound calcium.[10] It is prepared by centrifugation, ultrafiltration, and lyophilisation of pineapple juice.[5]
In the past, studies have been carried out to determine the effect of orally administered bromelain in reducing the postsurgical complications; these studies suggested few mechanisms of actions such as the following.[7,11,12]
Altering pain mediators such as bradykinin
Inhibiting the synthesis of pro-inflammatory prostaglandins, mainly PGE2
Its fibrinolytic action aids in the reabsorption of edema into the blood circulation
Overall, it was found to be effective in reducing pain, swelling, and healing time. However, its actions have been found to vary in different persons and different tissues in the same person.[7]
Several clinical studies have been carried out to determine the therapeutic uses of bromelain, and it has been found to be effective in minimizing the severity of angina pectoris and transient ischemic attack, osteoarthritis, autoimmune diseases, diarrhoea, cancer (by activating apoptosis), renal diseases, and respiratory diseases such as asthma, sinusitis, and eosinophilia. The other significant benefit of bromelain is that it enhances the permeability of antibiotics such as penicillin and tetracycline, thereby increasing their absorption.[5,13]
Even though studies have shown bromelain to have very low toxicity, its IgE-mediated allergenic potential cannot be underestimated. It is recommended to administer bromelain before food and daily dosage should be 750–1000 mg/day in divided doses.[10]
The aim of our study was to assess the effectiveness of bromelain in reducing swelling and pain after surgical removal of third molars. Quantifying facial edema or swelling is very difficult because it needs a three-dimensional quantification; in our study, we estimated postoperative swelling by measuring the distance between tragus to pogonion. We measured pain assessment by using VAS scale.
We found that, in 28 out of 40 cases (70%), bromelain effectively reduced pain and swelling after extraction of third molars. Our results were in accordance with few other similar studies.[14,15]
Hozt et al. in a double blind study measured the distance between tragus and pogonion to estimate swelling after administration of placebo and bromelain (80 mg thrice daily for 6 days) after the extraction of third molars. They found a reduction in swelling. We also found the same results, however, the dose administered in our study was 200 mg twice a day (400 mg).[16]
Inchingolo et al. and de la Barrera-Nunez et al. also found a reduction in postoperative swelling after the extraction of third molars by using bromelain. They used bromelain in dose of 240 mg for 6 days and 150 mg for three days.[7,8]
Whereas Majid et al. compared the efficiency of bromelain and diclofenac sodium after surgical removal of lower third molars and found significant reduction in pain in both the groups. They supported the effectiveness of bromelain in reducing postoperative pain, swelling, and postoperative life.[17]
Ordesi et al. found significant reduction in pain and swelling after extraction of third molars in patients who have taken bromelain when compared with controls.[9] In our study, bromelain effectively reduced pain and swelling in 28 out of 40 cases. Patients experienced less than moderate pain on day 1 after surgical removal of impacted third molar (mean VAS score being 4.86), which reduced to mild pain on day 3 (VAS score of 3.11) and which later significantly reduced to almost no pain on day 7 (VAS score 0.89). Our findings of reduced pain are in accordance with Inchingolo et al. and de la Barrera-Nunez et al.[7,8]
Effectiveness of bromelain in reducing pain among each subtypes (angulations, positions, and classes) were also compared. We found bromelain to be more effective in mesioangular impactions followed by vertical, distoangular, and horizontal types. We also found bromelain to be more effective in impactions of position A than position B and class I than class II. This might be due to less tissue trauma and time taken for removal of mesioangular, position A, and class I types of impactions in later types.[8,9,17,18,19]
Effectiveness of bromelain in reducing swelling among each subtypes (angulations, positions, and classes) was also compared. We found that bromelain was most effective for mesioangular impactions and least effective for horizontal impactions. Similarly, it was more effective for position A than position B and class I than class II types. Assessment of bromelain for three different difficulty index (mild, moderate, and difficult) were also evaluated. It was found that bromelain to be most effective (86.7%) for mild difficulty index, followed by difficult index (62.5%) and moderate difficult index (58.8%). Less effectiveness of bromelain for moderate difficulty index might be due to the fact that more horizontal angulations, position B, and class II index score were added in this category, which needed more operating time and experienced more intraoperative tissue trauma.[7,8,9]
We recommend further such studies on a larger sample size and using placebo as controls to determine the effectiveness of bromelain in reducing pain and swelling after removal of impacted third molars, so that we can utilize its multitherapeutic benefits. There is also a need to conduct studies comparing different routes of administration as well as different doses of bromelain in altering pain and swelling after third molars removal.
Key findings
Bromelain effectively reduced pain and swelling in 28 out of 40 cases.
Bromelain was more effective in mesioangular impactions, position A, and class I cases.
Strengths of the study
Less cost: We used only Bromelain in our study which costs about 8 Rupee per tablet to the patient. We did not prescribe any other analgesics, which further reduced the cost.
Reliable technique: As the technique used for the evaluation of parameters such as pain and swelling was simple, our technique was cost-effective and reliable. Further, the fact that radiographic follow-up was not done, makes the technique reliable.
Limitations
Lower sample size
Many controversies between various studies regarding different anti-inflammatory effects obtained after administering bromelain might be mainly due to a lack of knowledge of the effective dosage of bromelain indicated for postoperative inflammation after the extraction of third molars. We suggest further studies focusing on the dose and time-dependant effects of bromelain in reducing postoperative inflammation after third molars extraction, as previous studies and this study has shown that lower dosage at shorter intervals of time was more effective than higher dosage at longer intervals of time.
Hence, in future, studies with a higher sample size should be carried out to know exactly the analgesic and anti-inflammatory effects of oral enzymes such as bromelain after third molars extraction.
Our study evaluated the efficacy of bromelain for winters classification (angulation, position and class) and difficulty index specifically, which was not done in any other previous studies. In our study, we highlighted indications, contraindications, dosage, side effects, and toxicity of bromelain, which should act as reference for future studies on it.
CONCLUSION
A prospective randomized clinical study was done on 40 patients requiring surgical removal of impacted mandibular third molars. All the patients were administered bromelain after surgery to assess postoperative pain and swelling on day 1, 3, and 7. It was found that, in 28 patients, there was reduction in pain and swelling. Further studies have to be carried out to establish bromelain as a successful oral enzyme therapy for oral surgery patients.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Santosh P. Impacted Mandibular Third Molars: Review of Literature and a Proposal of a Combined Clinical and Radiological Classification. Ann Med Health Sci Res. 2015;5:229–34. doi: 10.4103/2141-9248.160177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Das JR, Sreejith VP, Anooj PD, Vasudevan A. Use of Corticosteroids in third molar surgery: Review of literature. Univ Res J Dent. 2015;5:171–5. [Google Scholar]
- 3.Al-Sandook TA, Tawfik NO, Qassim DA. Clinical evaluation of the efficacy of orthal-forte (prolytic enzymes, trypsin and chymotrypsin) on postoperative sequel following the removal of lower impacted third molar. Int J Enhanc Res Sci Technol Eng. 2014;3:169–73. [Google Scholar]
- 4.Kannan R, Kavitha R. A Comparative Study of the Anti-Inflammatory Properties of Bromelain/Serratiopeptidase as add on Therapy to Conventional Treatment Following Impacted Third Molar Surgery. World J Pharma Res. 2015;4:2595–607. [Google Scholar]
- 5.Gunde MC, Amnerkar ND. Ethnobotanical And Pharmacological Properties Of Pineapple Protease (Bromelain): A Review. Eur J Pharma Med Res. 2015;2:126–35. [Google Scholar]
- 6.Kaur R, Abmwani S, Mehta B. Trypsin, Rutoside And Bromelain Alone And Fixed Dose Combination: A Natural, Safer And Effective Anti-Inflammatory Agent. J Drug Deliv Ther. 2014;4:108–10. [Google Scholar]
- 7.Inchingolo F, Tatullo M, Marrelli M, Inchingolo AM, Picciariello V, Inchingolo AD, et al. Clinical trial with bromelain in third molar exodontia. Eur Rev Med Pharmacol Sci. 2010;14:771–4. [PubMed] [Google Scholar]
- 8.de la Barrera-Nunez MC, Yanez-Vico RM, Batista-Cruzado A, Heurtebise-Saavedra JM, Castillo-de Oyague R, Torres-Lagares D. Prospective double-blind clinical trial evaluating the effectiveness of Bromelain in the third molar extraction postoperative period. Med Oral Patol Oral Cir Bucal. 2014;19:e157–62. doi: 10.4317/medoral.19105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ordesi P, Pisoni L, Nannei P. Therapeutic efficacy of bromelain in impacted 3 rd molar surgery: A randomized controlled clinical study. Quintessence Int. 2014;45:679–84. doi: 10.3290/j.qi.a32237. [DOI] [PubMed] [Google Scholar]
- 10.de Lencastre Novaes LC, Jozala AF, Lopes AM, Santos-Ebinuma VD, Mazzola PG, Pessoa Junior A. Stability, Purification, and Applications of Bromelain: A Review. Biotechnol Prog. 2015;32:5–13. doi: 10.1002/btpr.2190. [DOI] [PubMed] [Google Scholar]
- 11.Nor MZM, Ramchandran L, Duke M, Vasilijevic T. Characteristic properties of crude pineapple waste extract for bromelain purification by membrane processing. J Food Sci Technol. 2015;52:7103–12. [Google Scholar]
- 12.Pardhi V, Chivte P, Kothare A, Shanbhag T. An Overview of Purification and Activity of Bromelain. Int J Recent Sci Res. 2016;7:12860–5. [Google Scholar]
- 13.Arshad ZI, Amid A, Yusof F, Jaswir I, Ahmad K, Loke SP. Bromelain: An overview of industrial application and purification strategies. Appl Microbiol Biotechnol. 2014;98:7283–97. doi: 10.1007/s00253-014-5889-y. [DOI] [PubMed] [Google Scholar]
- 14.Brien S, Lewith G, Walker A, Hicks SM, Middleton D. Bromelain as a Treatment for Osteoarthritis: A Review of Clinical Studies. Evid Based Complement Alternat Med. 2004;1:251–7. doi: 10.1093/ecam/neh035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Majid OW, Al-Mashhadani BA. Perioperative bromelain reduces pain & swelling & improves quality of life after mandibular 3rd molar surgery: A randomized, double blind, placebo -controlled clinical trial. 2014;72:1042–8. doi: 10.1016/j.joms.2013.12.035. [DOI] [PubMed] [Google Scholar]
- 16.Hotz G, Frank T, Zöller J, Wiebelt H. Antiphlogistic effect of bromelaine following third molar removal. Dtsch Zahnarztl Z. 1989;44:830–2. [PubMed] [Google Scholar]
- 17.Majid OW, Al-Mashhadani BA. Perioperative bromelain reduces pain and swelling and improves quality of life measures after mandibular third molar surgery: A randomized, double-blind, placebo-controlled clinical trial. J Oral Maxillofac Surg. 2014;72:1043–8. doi: 10.1016/j.joms.2013.12.035. [DOI] [PubMed] [Google Scholar]
- 18.Rubin G, Rinott M, Wolovelsky A, Rosenberg L, Shoham Y, Rozen N. A new bromelain-based enzyme for the release of Dupuytren's contracture: Dupuytren's enzymatic bromelain-based release. Bone Joint Res. 2016;5:175–7. doi: 10.1302/2046-3758.55.BJR-2016-0072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chakraborty DS. Anti-Metastatic Mechanism and Efficacy of Bromelain. Int J Ayur Pharma Res. 2015;3:10–3. [Google Scholar]


