Abstract
Background:
Innovation in the treatment of lower extremity lymphedema has received low priority from the governments and pharmaceutical industry. Advancing lymphedema is irreversible and initiates fibrosis in the dermis, reactive changes in the epidermis and subcutis. Most medical treatments offered for lymphedema are either too demanding with a less than satisfactory response or patients have low concordance due to complex schedules. A priority setting partnership (PSP) was established to decide on the future priorities in lymphedema research.
Methods:
A table of abstracts following a literature search was published in workshop website. Stake holders were requested to upload their priorities. Their questions were listed, randomized, and sent to lymphologists for ranking. High ranked ten research priorities, obtained through median score, were presented in final prioritization work shop attended by invited stake holders. A free medical camp was organized during workshop to understand patients’ priorities.
Results:
One hundred research priorities were selected from priorities uploaded to website. Ten priorities were short listed through a peer review process involving 12 lymphologists, for final discussion. They were related to simplification of integrative treatment for lymphedema, cellular changes in lymphedema and mechanisms of its reversal, eliminating bacterial entry lesions to reduce cellulitis episodes, exploring evidence for therapies in traditional medicine, improving patient concordance to compression therapy, epidemiology of lymphatic filariasis (LF), and economic benefit of integrative treatments of lymphedema.
Conclusion:
A robust research priority setting process, organized as described in James Lind Alliance guidebook, identified seven priority areas to achieve effective morbidity control of lymphedema including LF. All stake holders including Department of Health Research, Government of India, participated in the PSP.
Keywords: Ayurveda, integrative medicine, lymphatic filariasis, lymphedema, priority setting partnership, Yoga
What was known?
Global alliance to eliminate lymphatic filariasis (LF) is persuading governments of endemic nations to roll out morbidity control program for LF. Lymphedema, due to any cause, is a complex, chronic problem difficult to manage. Lymphedema endemic nations have limited health care budgets. Research priority setting involving government and stakeholders are essential to work out plans to reduce expenditure. James Lind Alliance has set guidelines to establish partnership and evolve consensus in research priority setting.
Introduction
Lymphatic filariasis (LF) commonly causes lower extremity lymphedema, albeit it affects genital and other anatomical parts. Secondary causes of lymphedema include breast cancer and other malignancies, trauma, etc., Primary lymphedema manifests at birth or as late as the third decade of life. Recurrent episodes of bacterial acute dermato lymphangio adenitis (ADLA) play a major role in worsening of lymphedema and time off work. Microfilarial infection in LF causes damage to the lymphatics and failure of the lymphatic system. This results in lymphedema with consequent retention of interstitial fluid, which is rich in proteins. In other forms of lymphedema, trauma to lymphatics/lymph nodes, either from surgery or by accident, induce edema. The lymphedema initiates fibrosis in the dermis and reactive changes in the epidermis and subcutis for which biomedicine has not been able to find a satisfactory medical or surgical solution. Most medical treatments offered for lymphedema either too demanding with a less than satisfactory response or patients have low concordance due to complex schedules.
The global program for elimination of LF was launched in 2000 by the World Health Organization (WHO). Its morbidity control schedule is currently focusing on the patients of 78 developing nations, where in LF is endemic. However, there is no consensus on uniformly applicable treatment options for lymphedema and opinions of patients and treating teams especially therapists have so far been little heard. Innovation in the treatment of LF has received low priority from the governments and pharmaceutical industry. Priority setting partnership (PSP) was organized inviting all stakeholders in lymphedema to decide on the future priorities for research on morbidity control of lymphedema. This paper summarizes the process of PSP in lymphedema, discussions during the final prioritization workshop (FPW), and recommendation on the top seven priorities for future research in lymphedema and a brief roadmap.
Methods
The Institute of Applied Dermatology (IAD) and the Central University of Kerala (CUK), Government of India jointly organized PSP broadly adhering to the James Lind Alliance guidebook.[1] The process is briefly explained below.
Step 1: Initiation and setting up a coordinating committee
The faculty of the IAD and CUK participated in the committee that led the coordination.
Step 2: Literature search
PubMed,[2] the Cochrane Library,[3] and Ayurveda, Yoga and Naturopathy, Unani, Siddha and Homoeopathy (AYUSH) portal,[4] a database containing the bibliographic information on published articles of AYUSH, were searched to identify the studies on interventions for lymphedema. A search strategy was designed to include the maximum number of studies and all types of the interventions published so far on lymphedema. The search strategy for identifying studies in PubMed and the Cochrane Central Register of Controlled Trials was designed as follows (primary lymphedema OR secondary lymphedema OR filarial lymphedema OR LF OR lipedema OR milroy lymphedema OR phlebo lymphedema OR lymphedema) AND (treatment OR management OR morbidity management) AND (limb volume OR volume OR limb circumference OR circumference OR limb girth measurement OR girth measurement OR girth OR quality of life OR health-related quality of life OR bacterial entry points [BEPs] OR bacterial entry lesions OR entry lesions OR ADLA care OR inflammatory episode OR inflammatory episodes) NOT (upper limb lymphedema OR breast cancer related lymphedema OR postmastectomy lymphedema OR mastectomy OR breast cancer). Three coordinators (S. R. Narahari [ first author], Madhur Guruprasad Aggithaya [second author] and K V Sushma [last author]) independently screened all studies, classified and tabulated the relevant portions of the abstracts. The details of the intervention, number of patients studied, and study design, outcomes used in the study and collective comments of three coordinators were published in the website www.indiandermatology.org.
Step 3: Contacting stakeholders (i.e., health-care providers and patients)
The physicians, lymphologists (91), basic scientists (including pathologists) (24), social science experts, AYUSH doctors, paramedical experts (therapists and nurses) (134) and patients (638) suffering from lymphedema were informed about the PSP and requested to look at the literature review table in the website and participate by uploading their research question.
Step 4: Listing priorities for research
The stakeholders were requested to submit their priority for future research on any aspects of morbidity control of lymphedema to the website (http://www.indiandermatology.org) within 2 months of receiving the E-mail invitation.
Step 5: Random collation of priorities
All the questions submitted within 2 months were downloaded. This list was randomized using Microsoft Excel Worksheet and published in the same website.
Step 6: Ranking exercises
A randomly collated list of priorities was sent to 14 experts in the field of lymphedema to rank them from 1 to 100, and 12 ranked lists were received. The rankings were listed together; median score was taken and arranged in ascending order. The median is the numerical value separating the higher half of a data sample, from the lower half. High ranked priorities appeared in the top of the list. Multiple priorities bearing the same rank from the top ten priorities were randomized and ranked again to find out the most favored one.
Step 7: Free lymphedema medical camp
A free medical camp for lymphedema patients was organized as part of the FPW. The lymphologists and other health-care providers consulted 116 patients from different parts of India. This provided the opportunity to understand the patients’ priorities and to get the opinion about the integrative medicine (IM) treatment. Patients attending the lymphedema camp were also encouraged voluntarily participate in the discussions being held during the workshop and give their inputs if any.
Step 8: Final prioritization workshop
A discussion on research proposals for future priorities in morbidity control of lymphedema and IM was conducted in FPW. The FPW was held on December 8–10, 2013 at IAD, for 2 days. Presentation on shortlisted ten research priorities included the lacunae for the enabling planning of future roadmap strategies. The patients also participated in the ensuing discussion. A panel of experts who moderated discussion also shared their views on priorities. The panel comprised T. J. Ryan, Christine Moffatt, Vaughan Keeley, Dr. Nagesh Prabhu, Joint Secretary, Department of Health Research, Government of India, New Delhi, Ms. Jalaja Sinha, IAS (Rtd.), Former secretary of Department of AYUSH, Government of India, and N. K. Kumar. Peter Mortimer, Professor, Dermatological Medicine, St George's Hospital, London, Claire Fuller, Chair of International Foundation for Dermatology, Chelsea and Westminster Hospital, London and Prof. Neil Piller, Director International Lymphedema Framework and Director, Lymphoedema Research Unit, Flinders University, Adelaide, Australia, appeared through Skype and participated in the discussion. Two days of deliberations reframed the top ten priorities into seven. Finally, the priorities were put to the vote.
Results
Literature search
The search on Cochrane Central yielded 39 studies. 16 studies were relevant for morbidity control. PubMed search yielded 449 studies; 112 were relevant. Studies included lymphovenous anastomosis, omental plasty, skin and soft tissue excision, complex decongestive physiotherapy, compression therapy, integrative treatments, drug therapy, advice on wash and hygiene, manual lymph drainage, and medical devices for lymphedema. The literature search on traditional medicine (AYUSH treatments) for morbidity management of lymphedema retrieved 46 studies through AYUSH portal. They included 11 studies related to Ayurveda, 2 on Homeopathy and 3 on Unani.
Priority questions on morbidity control of lymphedema
A total of 137 respondents uploaded their priorities for lymphedema research. One hundred research priorities were listed after eliminating repetitions. The top ten priorities selected by the referees for discussion during FPW were:
What is the economic benefit from IM for the morbidity reduction of lymphedema?
What are the cellular changes following lymphedema treatment? Can lymphedema be reversed following integrative treatment?
What factors determine whether patients comply with the use of the bandaging techniques for long-term management? Would patients consider wearing made to measure compression garments for long-term management instead of bandages? Would there be an improved outcome?
Morbidity control of LF by randomizing the interventions washing, emollient, and compression versus Ayurvedic and Yoga interventions
How to create a biomedical model for Ayurvedic treatments for chronic dermatoses?
How to eliminate BEPs especially intertrigo between toes in lymphedema patients working in the fishing industry of the coastal region? Which are the frequently grown bacteria and fungi in the intertrigo of lymphedema? What are their antibiotic sensitivity patterns?
What is the active principle in Ayurvedic medicines causing the change in lymphedema?
What is the epidemiology of LF morbidity? What is the relative frequency/prevalence of various morbidities due to LF? Are all cases diagnosed clinically as LF genuine cases or do other phenotypes get misdiagnosed as filariasis?
What are the comorbid conditions prevalent with filarial lymphedema patients? How do these conditions affect the management of lymphedema?
How to simplify lymphedema integrative home management?
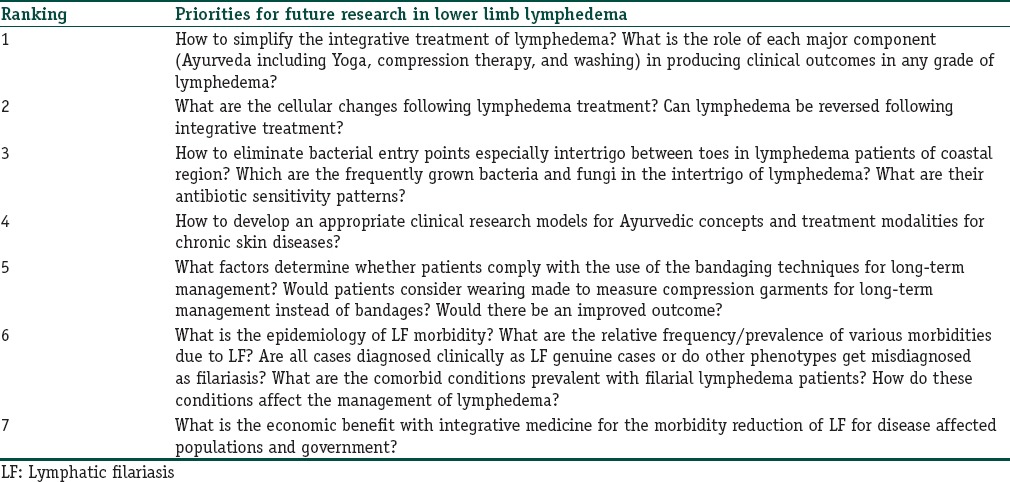
The FPW was attended by 116 patients and 36 national and international experts, 8 AYUSH doctors, 24 other health-care workers, 7 senior bureaucrats, representatives of Department of Health Research, Government of India and Science and Technology Council of Government, of Kerala, students and faculty from IAD and CUK and other delegates. Fifty-one delegates voted on the future priorities for lymphedema research. The priorities regrouped and decided through voting in the descending order are listed in Table 1.
Table 1.
The priorities for future research in lymphedema, decided through national priority setting workshop held at Institute of Applied Dermatology, Kasaragod, Kerala, India
Discussion
Seven research questions on morbidity control of lower leg lymphedema were recommended by the FPW. The consultation process involved all stakeholders of lymphedema especially patients who attempted multiple treatment options. Guidance of international experts was available at all stages and during 2 days of workshop. FPW examined all shortlisted research questions which physicians, basic scientists, and paramedical workers felt important in their routine practice.
Patients have often tried several treatments over a long period, and they can judge the benefits of these treatments. They have thoughts on which treatments should be evaluated or modified. Patients, who received integrative treatment for lymphedema at IAD, participated throughout PSP. Their questions were also considered before finalizing the priorities for future research in lymphedema.
Major scientific databases were searched to find out available evidence and contemporary research focus. PubMed was searched based on the “PICO,” specifying the types of population (participants), types of interventions (and comparators), and the types of outcomes that are of interest in lymphedema. There were two Cochrane reviews, on diethylcarbamazine-medicated salt for community-based control[5] and lymphadenectomy for the management of endometrial cancer.[6] However, there were no systematic reviews done on other treatment modalities. The results of these studies were summarized and presented in the website for the reference of those participating in PSP.
Future research proposals
Ten priorities were shortlisted with different areas of research on lymphedema and its management in resource-poor village settings using locally available treatments. Three of them (first, fourth, tenth) were related to the integrative treatment for lymphedema developed by IAD. A WHO publication described the IAD as one among the leading lymphology clinics in the world.[7] IAD has successfully evolved an IM combining the therapies of biomedicine, Ayurveda, and Yoga, delivered simultaneously in such a way as to be acceptable to lymphedema communities[8] for reducing the clinically diagnosed lymphedema and its resultant physical and socioeconomic inconveniences. Two were aimed at creating an evidence base for Ayurvedic research (fifth and seventh), other three (sixth, seventh and ninth) were related to LF prevalence. Discussions during FPW led to regrouping of ten research questions into seven as listed in Table 1. They are briefly discussed below.
The first priority was to simplify lymphedema integrative home management. Patients participating FPW gave their opinion on how this can be achieved. The major focus was on reducing the time for treatment and self-care by giving the self-Indian Manual Lymph Drainage (IMLD) and compression. The simplified protocol, by demonstrating the skin wash, BEPs care and Yoga exercises in community level lymphedema camps is beneficial since community level participation is helpful to reach the maximum number of patients in endemic villages. A model for these Lymphedema camps developed by Aggithaya et al. 2013 was discussed.[9] Multimodality interventions, just as much as single interventions, have to be supported by the evidence of efficacy. The role of each component of integrative treatment considered to be important while simplifying the treatment. This can be achieved by conducting a randomized control trial by randomizing the interventions washing and emollient, compression with Ayurvedic and Yoga interventions. Hence, it was decided to combine the first and fourth among initial ten priorities. The FPW discussed a protocol by comparing the three interventions, i.e., Ayurvedic Skin Care, Biomedical Skin Care and compression therapy with integrative treatment as a control group. This allows the component-wise analysis of the integrative treatment protocol. A three arms trial is also possible by comparing the conventional treatment with Ayurvedic treatments. FPW recommended it to be done as a community trial in endemic villages. Earlier publications have recommended the simplification of the integrative treatment of lymphedema developed by IAD.[8]
The second priority was to find out the cellular changes following reversal of grade following lymphedema treatment. Prof. Ryan lectured on “Lymphoedema as a consequence of skin failure” and CUK and JSS University (JSSU) faculty reviewed the literature on cellular changes and possible research opportunities in lymphedema. Microfilarial infection causes damage to the lymphatics and failure of the lymphatic system. This results in lymphedema with consequent retention of interstitial fluid rich in proteins. This initiates fibrosis in the dermis and hyperplastic changes in the epidermis. Recurrent episodes of bacterial cellulitis/ADLA induce the release of pro-inflammatory Th2 cytokines (interleukin [IL]-4, IL-6 and IL-10) and pro-fibrotic cytokines (IL-5, IL-13, and transforming growth factor-beta). They cause additional damage to the lymphatic system leading to progression of lymphedema with fibrosis. The altered ratio of matrix metalloproteinase-1/tissue inhibitor of metalloproteinase 4 (TIMP4) and matrix metalloproteinase-8/TIMP4, angiogenesis (due to decreased clearance of vascular endothelial growth factor), collagen up-regulation, marked destruction and reduction in elastic fibers and high mast cell content are observed in various studies.[10,11] Although fat deposition is a defining clinical characteristic of lymphedema, the cellular mechanisms that regulate this response remain largely unknown.[12] Whatever the role of additional promoting factors in lymphedema, the ultimate tissue response is a failure of the lymphatic system and fibrosis of the dermis with hyperplastic changes in the epidermis and the subcutis. FPW focused the discussion on results from a pilot analysis of biopsies from International Society of Lymphology Grade 3 lymphedema patients jointly undertaken by IAD and JSSU. FPW recommended histopathological studies, immunohistochemical stains, cell and molecular level studies including fibrosis and extracellular matrix remodeling analysis, inflammatory response analysis, adipogenic factor analysis, and comparative transcriptome analysis (comparative analysis of total gene expression profile) on pretreatment biopsies and posttreatment biopsies to understand the complete mechanism of changes achieved by integrative treatment of lymphedema. FPW voted this as number 2 priority.
The third priority is to develop a solution to eliminate BEP, especially intertrigo between toes in lymphedema patients of the coastal region and the monsoon and identify the frequently grown bacteria and fungi and their antibiotic sensitivity patterns. More than a decades ago, Group A Streptococci have been isolated from BEP.[13] Only 18% of the lesions had positive microscopy or culture for fungi (dermatophytes and Scytalidium)[14] and simple maceration can be blamed for intertrigo. Further, epidemiological surveys can be conducted by doing bacteriological examination of swabs from the entry lesions to identify the bacterial and fungal types and antibiotic sensitive patterns.
The fourth priority is to create a biomedical model for Ayurvedic treatments for chronic dermatoses. This question was raised following the demonstration by IAD that Ayurveda and Yoga therapy could be successfully used for lymphedema. Many lymphedema patients also suffered from other chronic disabilities. Patients were keen to know whether the biomedical model as used for lymphedema could be applied to Ayurveda therapy, especially because Ayurveda drugs were expected to show high levels of safety. There should be proper understanding and knowledge about each medical system, before creating the biomedical model for Ayurveda. IAD's observational studies showed evidence for Ayurvedic treatments.[15,16] The future research could be built on those fundamental observations. There are clinical features such as color changes, morphological appearance, and other signs of skin diseases explained in Ayurvedic texts. Using the biomedical, clinical methods, all of them should be validated for the individual disease under study and lead to the application of biomedical model to Ayurveda therapy. This may not necessarily produce new molecular drugs.[17] In lymphedema patients, data should be obtained during the baseline and at follow-ups to develop a reliable model and best fitting variable (or variables in combination). They could be selected as a clinical or biological marker for the treatment response in Ayurveda. This will help in scientific understanding of the mechanisms involved in the effectiveness of the treatment and basic pathophysiology of lymphedema at the molecular level.
The seventh priority among ten priorities, what is the active ingredient in Ayurvedic medicines causing the change in lymphedema? was discussed and combined “How to develop an appropriate clinical research models for Ayurvedic concepts and treatment modalities for chronic skin diseases?” The workshop felt that it would be difficult to identify the active ingredient in multimodal interventions like integrative treatment of lymphedema, since, as commonly believed by those who study herbal properties, a complex of constituents, may be responsible for the changes.
The fifth priority is to find out the patient's compliance with the use of the bandaging techniques for long-term management. Occupational hazards cost of compression bandages, difficulty in social participation, and quality/availability of the long stretch bandages are the factors determining noncompliance for compression bandaging. The absence of any home carer also has a negative impact. Studies to find out the usefulness of a well-fit compression garments and issues related to using compression garments for irregular shapes of the limb, comorbidity, and complications, occupational hazard, nonavailability of compression garments and other materials in endemic area were discussed. The possibility of future collaboration with patient support groups and special fabric manufacturers were also discussed.
Currently, more than 1.4 billion people in 78 countries are at risk of LF. Approximately, 65% of those infected live in the WHO South-East Asia Region, 30% in the African Region, and the remainder in other tropical areas. However, there are no reports regarding the prevalence of various morbidities due to lymphedema. The sixth research question was to find out the epidemiology and relative frequency/prevalence of various morbidities due to LF; are all lymphedema seen in endemic areas of developing nations due to filarial? FPW felt that well-designed community level studies should be conducted to identify the prevalence and diagnose genuine cases of LF and other phenotypes. Identifying the comorbid conditions prevalent with filarial lymphedema patients and its impact on the management of lymphedema can be the part of the community-level studies. Hence, the ninth of ten priorities was added to sixth priority of final seven. Patients participating in FPW quickly listed the associated diseases. They included venous insufficiency, cardiac ailments, osteoarthritis, rheumatoid arthritis, anemia, and deep vein thrombosis (DVT). Acute DVT has been considered a contraindication to compression bandaging but the early use of compression is advisable.[18] It reduces the incidence of postthrombotic syndrome and does not increase clinically significant pulmonary embolism. Varicosity was often complicated by associated gravitational eczema and wounds. Osteoarthritis and rheumatoid arthritis complicate the disability associated with lymphedema. Other common diseases listed by patients were hypertension, diabetes mellitus, urinary tract infection, renal ailments and hepatobiliary disease, psoriasis, arteriovenous malformation, desmoid tumor, neurofibromatosis, and hyper/hypothyroidism. All of them would require epidemiological studies with causal association assessments.
The seventh priority was to find the economic benefit from IM for morbidity reduction of lymphedema. The integrative treatment includes skin wash using single brand soap, soaking with herbalized liquid (Phanta), BEP care using modern dermatology drugs, IMLD, pre-IMLD Yoga postures, compression bandaging and post-IMLD Yoga.[19] The cost of treatment has been estimated periodically at IAD. The total cost of treatment of unilateral lymphedema for 2 weeks of supervised treatment and 3 months treatment at home was INR 21,809.39 (USD 352.85). This was INR 24,510.19 (USD 396.54) for bilateral lymphedema.[8] The cost included the salary of the treatment team, establishment cost, medicine, and compression bandaging cost. IAD is a not for profit organization and despite several attempts has failed to obtain any significant government grants. Therefore, the treatment cost for lymphedema is charged to patients albeit 25% of patients are provided sponsorship of 90% of the total cost through donor contribution. Total cost per patient varied depending on unilateral and bilateral lymphedema, number of days of treatment and presence and size of any accompanying ulcer. The integrative treatment does not require hospitalization and initial treatment which includes training of patients in self-care as domiciliary treatment is given as a day care program. It is self-care training to patients and involves/treating BEP. Locally available materials and medicines are used. Interventional studies need to progress from efficacy trials to effectiveness trials.[20] Integrative treatment has already been found to be effective[21] in terms of a reduction in limb volume, BEP, and improvement in the quality of life. Efficacy studies and cost analysis can be ideal to find out the overall efficacy. However, to estimate the economic benefit field programs should be conducted in the model of Aggithaya et al. 2013[9] and Narahari et al. 2013.[8] The quality of life changes[22] and economic benefits[23] should be assessed before and after treatment. Costing studies done in IAD could not be translated to the actual costs at the community level treatment. Therefore, FPW recommended a cost-benefit research from IM. This research question was voted number 7 by FPW.
The patient participation was the key in this FPW. Three hours were devoted both days to examine the patients in the free lymphedema medical camp. This allowed a patient-centric discussion and made all stakeholders to understand the morbidity and its complication associated with lymphedema. Free medical camps also encouraged participation of patients in the workshop. The camp was organized from 08.00 to 11.00 am. Patients separately demonstrated different aspects of complex integrative treatment during the session.
The priorities related to surgical interventions were not included in the PSP, which is a limitation. The study is based on the James Lind Alliance method of prioritization. The prioritization was based on voting, and it depends on the opinion of delegates present during voting. During prioritization process, we had little response from surgeons despite repeated requests. This may be the reason for exclusion of surgical treatments in prioritization. The patients also have fear for undergoing surgery, which prevents them to add surgical treatments as future priorities. Since IAD provides medical treatments, bias in favor of nonsurgical treatments is possible.
Conclusion
FPW discussions led to collating shortlisted ten research questions to seven priority areas. This was a robust PSP for future research in the morbidity control of lymphedema. The workshop followed an established PSP method.
Financial support and sponsorship
Department of Health Research, Government of India, Department of Science and Technology, Government of India, Kerala State Council for Science, Technology and Environment and Indian Council of Medical Research, Government of India.
Conflicts of interest
There are no conflicts of interest.
What is new?
This article summarizes the consensus research priorities for scaling up morbidity control program to reach large affected population. Indian treatment for lymphedema has shown promises to scale up as self-care, home based treatment for lymphatic filariasis in rural communities of endemic nations.
Acknowledgment
We thank Prof. Gail Davey, Professor of Global Health Epidemiology, Brighton and Sussex Medical School, Professor Neil Piller, Director International Lymphedema Framework, Director Lymphedema Research Unit, Australia, Dr. A. C. Dhariwal, Director, NVBDCP, New Delhi, Prof. B. Unnikrishnan, Head, Department of Community Medicine, Kasturba Medical College, Mangalore, Dr. Sairu Philip, Additional Professor, Department of Community Medicine, T. D. Medical College, Alleppey, Kerala, Dr. Veena Agrawal, District Hospital Korba, Chhattisgarh, Dr. K. N. Panicker, Professor Emeritus, The Amrita Institute of Medical Sciences, Kochi, Kerala for ranking of priorities. We also thank Dr. Nagesh Prabhu, Joint Secretary, Department of Health Research, Government of India, New Delhi and Ms. Jalaja Sinha, IAS Rtd., Former Secretary, Department of AYUSH, New Delhi for their support.
References
- 1.James Lind Alliance Guidebook. The James Lind Alliance. Southampton. [Last accessed on 2016 Jan 10]. Available from: http://www.jlaguidebook.org .
- 2.PubMed. US National Library of Medicine. National Institutes of Health. USA, Bethesda. [Last accessed on 2016 Jan 10]. Available from: http://www.ncbi.nlm.nih.gov/pubmed .
- 3.The Cochrane Library. The Cochrane Collaboration. West Sussex, UK: John Wiley and Sons Ltd; [Last accessed on 2016 Jan 10]. Available from: http://www.thecochranelibrary.com/ [Google Scholar]
- 4.AYUSH Research Portal. Department of AYUSH, Ministry of Health & Family Welfare, Government of India. [Last accessed on 2016 Jan 10]. Available from: http://www.ayushportal.ap.nic.in/
- 5.Adinarayanan S, Critchley J, Das PK, Gelband H. Diethylcarbamazine (DEC)-medicated salt for community-based control of lymphatic filariasis. Cochrane Database Syst Rev. 2007 doi: 10.1002/14651858.CD003758.pub2. CD003758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Frost JA, Webster KE, Bryant A, Morrison J. Lymphadenectomy for the management of endometrial cancer. Cochrane Database Syst Rev. 2015 doi: 10.1002/14651858.CD007585.pub3. CD007585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Macdonald JM, Ryan TJ. Lymphoedema and the chronic wound: The role of compression and other interventions. In: Macdonald JM, Geyer MJ, editors. Wound and Lymphoedema Management. Switzerland, Geneva: World Health Organization; 2010. pp. 63–83. [Google Scholar]
- 8.Narahari SR, Bose KS, Aggithaya MG, Swamy GK, Ryan TJ, Unnikrishnan B, et al. Community level morbidity control of lymphoedema using self care and integrative treatment in two lymphatic filariasis endemic districts of South India: A non randomized interventional study. Trans R Soc Trop Med Hyg. 2013;107:566–77. doi: 10.1093/trstmh/trt054. [DOI] [PubMed] [Google Scholar]
- 9.Aggithaya MG, Narahari SR, Vayalil S, Shefuvan M, Jacob NK, Sushma KV. Self care integrative treatment demonstrated in rural community setting improves health related quality of life of lymphatic filariasis patients in endemic villages. Acta Trop. 2013;126:198–204. doi: 10.1016/j.actatropica.2013.02.022. [DOI] [PubMed] [Google Scholar]
- 10.Anuradha R, George JP, Pavankumar N, Kumaraswami V, Nutman TB, Babu S. Altered circulating levels of matrix metalloproteinases and inhibitors associated with elevated type 2 cytokines in lymphatic filarial disease. PLoS Negl Trop Dis. 2012;6:e1681. doi: 10.1371/journal.pntd.0001681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ryan TJ. The first commandment: Oil it! An appreciation of the science underlying water and emollients for skincare. Community Dermatol. 2004;1:3–5. [Google Scholar]
- 12.Zampell JC, Aschen S, Weitman ES, Yan A, Elhadad S, De Brot M, et al. Regulation of adipogenesis by lymphatic fluid stasis: Part I. Adipogenesis, fibrosis, and inflammation. Plast Reconstr Surg. 2012;129:825–34. doi: 10.1097/PRS.0b013e3182450b2d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Suma TK, Shenoy RK, Varghese J, Kuttikkal VV, Kumaraswami V. Estimation of ASO titer as an indicator of streptococcal infection precipitating acute adenolymphangitis in brugian lymphatic filariasis. Southeast Asian J Trop Med Public Health. 1997;28:826–30. [PubMed] [Google Scholar]
- 14.McPherson T, Persaud S, Singh S, Fay MP, Addiss D, Nutman TB, et al. Interdigital lesions and frequency of acute dermatolymphangioadenitis in lymphoedema in a filariasis-endemic area. Br J Dermatol. 2006;154:933–41. doi: 10.1111/j.1365-2133.2005.07081.x. [DOI] [PubMed] [Google Scholar]
- 15.Narahari SR, Ryan TJ, Aggithaya MG, Bose KS, Prasanna KS. Evidence-based approaches for the Ayurvedic traditional herbal formulations: Toward an Ayurvedic CONSORT model. J Altern Complement Med. 2008;14:769–76. doi: 10.1089/acm.2007.0818. [DOI] [PubMed] [Google Scholar]
- 16.Aggithaya MG, Narahari SR, Vijaya S, Sushma KV, Kumar NP, Prajeesh P. Navarakizhi and pinda sweda as muscle-nourishing Ayurveda procedures in hemiplegia: Double-blind randomized comparative pilot clinical trial. J Altern Complement Med. 2014;20:57–64. doi: 10.1089/acm.2012.0919. [DOI] [PubMed] [Google Scholar]
- 17.Narahari SR. Collaboration culture in medicine. Indian J Dermatol. 2013;58:124–6. doi: 10.4103/0019-5154.108042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Partsch H. Compression therapy: Clinical and experimental evidence. Ann Vasc Dis. 2012;5:416–22. doi: 10.3400/avd.ra.12.00068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Narahari SR, Ryan TJ, Mahadevan PE, Bose KS, Prasanna KS. Integrated management of filarial lymphedema for rural communities. Lymphology. 2007;40:3–13. [PubMed] [Google Scholar]
- 20.Singal AG, Higgins PD, Waljee AK. A primer on effectiveness and efficacy trials. Clin Transl Gastroenterol. 2014;5:e45. doi: 10.1038/ctg.2013.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Narahari SR, Ryan TJ, Bose KS, Prasanna KS, Aggithaya GM. Integrating modern dermatology and Ayurveda in the treatment of vitiligo and lymphedema in India. Int J Dermatol. 2011;50:310–34. doi: 10.1111/j.1365-4632.2010.04744.x. [DOI] [PubMed] [Google Scholar]
- 22.Thomas C, Narahari SR, Bose KS, Vivekananda K, Nwe S, West DP, et al. Comparison of three quality of life instruments in lymphatic filariasis: DLQI, WHODAS 2.0, and LFSQQ. PLoS Negl Trop Dis. 2014;8:e2716. doi: 10.1371/journal.pntd.0002716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Narahari SR, Ryan TJ, Aggithaya MG, Bose KS, Swamy GK. Community dermatology in practice: Control of morbidity in lymphatic filariasis patients in Indian villages. Contin Med Educ. 2013;31:240–2. [Google Scholar]


