ABSTRACT
Viral entry represents the first step of every viral infection and is a determinant for the host range and disease potential of a virus. Here, we review the latest developments on cell entry of the highly pathogenic Old World arenavirus Lassa virus, providing novel insights into the complex virus-host cell interaction of this important human pathogen. We will cover new discoveries on the molecular mechanisms of receptor recognition, endocytosis, and the use of late endosomal entry factors.
KEYWORDS: endocytosis, Lassa fever, late endosome, receptor, viral entry
INTRODUCTION
Among the arenaviruses, Lassa virus (LASV) represents the most prevalent human pathogen, with several hundred thousand infections per year (1). Carried by persistent infection of the reservoir rodent host Mastomys natalensis, LASV is endemic in large parts of western Africa. Arenaviruses are enveloped negative-strand RNA viruses with a nonlytic life cycle confined to the cytosol. The arenavirus genome comprises a small (S) RNA segment encoding the envelope glycoprotein precursor (GPC) and the nucleoprotein (NP) and an L segment coding for the matrix protein (Z) as well as the viral polymerase (L) (2). The GPC is synthesized as a single polypeptide and undergoes processing, yielding a stable signal peptide (SSP), N-terminal GP1, and transmembrane GP2. GP1 binds to cellular receptors, whereas GP2 mediates viral fusion and structurally resembles class I viral fusion proteins. Upon receptor binding, LASV enters the host cell via receptor-mediated endocytosis, with subsequent transport to late endosomal compartments, where fusion occurs at low pH (3, 4). Arenavirus fusion has been covered by an excellent recent review (5) and will therefore not be described in detail here. By an unknown mechanism of “uncoating,” the viral ribonucleoprotein is released into the cytosol, where viral transcription and replication take place. The assembly and release of arenavirus infectious progeny are orchestrated by the matrix protein Z, which recruits endosomal sorting complexes required for transport (ESCRT) proteins that are crucial for virion budding.
Human LASV infection occurs mainly via reservoir-to-human transmission (6) that likely involves inhalation of contaminated aerosolized rodent excreta and ingestion of contaminated food (1). Following early viral multiplication at the site of entry, the virus disseminates via the bloodstream, reaching the lymph nodes, spleen, and liver, where productive infection is established. A predictive factor for disease outcome is the viral load early in infection, indicating a close competition between viral spread and replication and the patient's immune system (7). The pathophysiology of the fatal shock syndrome is not well understood and may involve functional changes in vascular endothelial cells, liver, adrenal gland, and other organs (8). Current treatment is limited to supportive care and the antiviral drug ribavirin, which reduces mortality when given early in disease (9). Due to its proven transmissibility via aerosol (10) and high lethality, LASV is considered a category A agent by the Centers for Disease Control and Prevention (11). The lack of a licensed vaccine and limited treatment options make the development of novel therapeutic strategies against LASV an urgent need. Antiviral drugs capable of reducing the multiplication and spread of LASV may provide the patient's immune system a window of opportunity to develop an antiviral immune response. A major challenge for the development of drugs against LASV, however, is the limited structural information available on the pathogen. As with all viruses, LASV critically depends on the molecular machinery of the host cell for its multiplication. Targeting viral entry appears to be a promising strategy for therapeutic intervention, as it allows blocking of the pathogen before it can take control of the host cell. The identification of cellular factors required for productive LASV entry and their evaluation as possible targets for therapeutic antiviral intervention are therefore of great interest.
LASSA VIRUS SHOWS COMPLEX RECEPTOR USE
The first LASV receptor was identified as dystroglycan (DG), a ubiquitously expressed conserved cellular receptor for extracellular matrix (ECM) proteins (12). In mammals, DG is found in most tissues, where it provides a molecular link between the ECM and the actin cytoskeleton. Apart from LASV, DG can serve as a receptor for most isolates of the prototypic arenavirus lymphocytic choriomeningitis virus (LCMV) and the African arenaviruses Mopeia virus and Mobala virus, as well as clade C New World arenaviruses (12, 13). The DG core protein is initially synthesized as a single polypeptide chain that undergoes autoprocessing, yielding the peripheral α-DG, which interacts with ECM proteins, and the transmembrane β-DG. At the cytosolic face, β-DG associates with the cytoskeletal adaptor proteins dystrophin and utrophin, anchoring the DG complex to the actin cytoskeleton (14). During biosynthesis, α-DG undergoes remarkably complex O-glycosylation that is essential for its biological function (15). The functional glycosylation of α-DG starts with the biosynthesis of the unusual O-linked trisaccharide O-Man-β1-4-GlcNAc-β1-3GalNAc, which undergoes phosphorylation at the O-mannosyl residue (16). A ribitol moiety links the trisaccharide to Xyl-α1-GlcA-3-β1-3 copolymers synthesized by the dually specific glycosyltransferase like-acetylglucosaminyltransferase (LARGE) (17, 18). The LARGE-derived Xyl-α1-GlcA-3-β1-3 polysaccharide is called matriglycan and recognizes laminin globular (LG) domains of ECM proteins via an unusual lectin-type binding (15, 19, 20). Modification of DG by LARGE is also crucial for arenavirus binding (21, 22), and a recent elegant haploid screen revealed that LASV GP strikingly mimics the mechanisms of receptor recognition of host-derived ECM proteins (23). While the DG core protein is ubiquitously expressed in most mammalian cells, functional glycosylation by LARGE is under tight tissue-specific control (19). Dystroglycan therefore appears as a “tunable” receptor (19), whose virus-binding affinity is influenced by the length of the LARGE-derived glycans (21). Genome-wide association studies in human populations revealed positive selection for specific LARGE alleles in populations from western Africa (6, 24, 25). Although the exact role of the selected LARGE alleles in LASV susceptibility of carriers is not yet clear, the data suggest a role of DG's posttranslational modifications in virus-host coevolution.
Binding of viruses to their receptor(s) frequently induces signaling that functions as a “knock on the door” to facilitate entry (26). The cytosolic domain of β-DG can associate with signaling molecules, including the adaptor Grb2 (27); mitogen-activated protein (MAP) kinases MEK and extracellular signal-regulated kinase (ERK) (28); and focal adhesion kinase (29). Engagement of cellular α-DG by LASV GP induced tyrosine phosphorylation of β-DG's cytosolic domain, resulting in dissociation from the cytoskeletal adaptor utrophin, which may promote internalization of the virus-receptor complex (30). Virus-receptor binding further affected signaling cross talk of DG with α6β1 integrins, another widely expressed family of ECM receptors that can functionally cooperate with DG (31, 32). However, since β1 integrins are dispensable for LASV entry, the role of this phenomenon for viral infection is currently unclear.
More recently, the Tyro3/Axl/Mer (TAM) receptor tyrosine kinases Axl and Tyro3/Dtk, as well as the C-type lectins dendritic cell (DC)-specific intracellular adhesion molecule 3 (ICAM-3)-grabbing nonintegrin (DC-SIGN) and liver and lymph node sinusoidal endothelial cell C-type lectin (LSECtin), have been identified as novel candidate receptors for LASV and LCMV (33, 34). Tyro3 and Axl are broadly expressed receptors for the phosphatidylserine (PS)-binding serum proteins Gas6 and protein S and are involved in removal of apoptotic cells (35, 36). Over the past years, TAM kinases have been implicated in viral entry by “apoptotic mimicry,” which involves recognition of PS displayed in the viral lipid envelope by cellular PS receptors and is used by a broad range of enveloped viruses (37–42). The coexpression of DG with TAM receptors in tissues infected by LASV suggests complex receptor use. However, conflicting data on the roles of TAM receptors in Old World arenavirus infection have been reported. A role for Axl and Tyro3 in LASV entry was initially discovered by expression cloning using a LASV pseudotype platform (34). Antibody perturbation experiments supported a contribution of Axl to LASV entry into cells lacking functional DG (34). However, other studies found no enhancement of LASV or LCMV entry by overexpression of TAM kinases, and the authors concluded that these PS receptors are unable to mediate productive infection (43). Notably, mice deficient in Axl remained highly susceptible to LCMV infection in vivo (44). More work will be needed to define the exact roles of TAM kinases in LASV entry into specific human target cells and their role in vivo.
Based on their more restricted expression patterns, DC-SIGN and LSECtin may contribute to LASV entry into specific cell types, including dendritic cells (DC) that represent important early targets during infection (45). In vitro studies on monocyte-derived human DC revealed that high-mannose N-glycans displayed on LASV GP1 may engage DC-SIGN during attachment (46). However, DC-SIGN seemed dispensable for subsequent viral entry. This seems in stark contrast to what occurs in arthropod-borne phleboviruses and Dengue virus (40, 47), which use DC-SIGN as a true entry receptor in DC. However, the candidate receptor expression pattern of monocyte-derived DC in vitro may differ from that of authentic DC populations in vivo, putting limitations on this model.
DYSTROGLYCAN-MEDIATED LASV ENTRY INVOLVES AN UNUSUAL PATHWAY OF MACROPINOCYTOSIS
Initial studies suggested that Old World arenaviruses enter via an unknown clathrin- and dynamin-independent pathway (48–50). More recent genome-wide RNA interference silencing screens identified sodium hydrogen exchangers (NHE) as host factors involved in the multiplication of LCMV (51). Based on these findings, Iwasaki and colleagues validated NHE as entry factors for LCMV and LASV and demonstrated, for the first time, a link between arenavirus entry and macropinocytosis (52). Employing a panel of “diagnostic inhibitors” for macropinocytosis proposed by Mercer et al. (53, 54), LASV entry into human epithelial cells was investigated. In line with earlier studies, functionally glycosylated DG served as the main receptor for LASV in epithelia, whereas other candidate receptors were either absent or dispensable (55). Consistent with previous studies (52), LASV entry was independent of dynamin, was dependent on NHE, and required the dynamics of the actin cytoskeleton. The small GTPase Cdc42 and its downstream effectors PAK1 and N-Wasp were required for the regulation of LASV entry, whereas Rac1, RhoA, the Arp2/3 complex, myosin II, and myosin light-chain kinase seemed dispensable in the cell types tested. The identification of PAK1 as a LASV entry factor was further in line with a recent screen for anti-LASV drugs that identified the PAK1 inhibitor OSU-03012 as a hit (56).
Macropinocytosis is a major pathway of cell entry used by >20 different viruses, and the pathogens seem to recruit specific sets of regulatory proteins according to their needs (54, 57). In line with this, LASV entry requires a limited subset of the known regulators of “classical” macropinocytosis. In most cells, macropinocytosis is not constitutively active but needs to be activated (53). A series of classical studies on other viruses, including the poxvirus vaccinia virus (VACV), respiratory syncytial virus, influenza A virus, echovirus 1 (58), and African swine fever virus, revealed that the pathogens are able to activate the pathway (42, 58–61). As a consequence, virus attachment to the plasma membrane induces membrane “blebbing,” triggers actin depolymerization, and increases bulk fluid uptake. In contrast, LASV entry only minimally affected the host cell's membrane and actin dynamics (55), possibly due to distinct receptor use and/or differences in virion size. Several kinases implicated in macropinocytosis are required for LASV entry, including protein kinase C (PKC), phosphoinositol 3 kinase (PI3K), epithelial growth factor receptor (EGFR), and hepatocyte growth factor receptor (HGFR) (55, 56). The data at hand suggest that DG can link LASV to a pathway related to macropinocytosis that causes only minimal perturbation of the host cell, which may be required for its nonlytic life cycle and the ability to persist in its rodent reservoir.
LAMP1 IS A LATE ENDOSOMAL ENTRY FACTOR FOR LASV THAT FACILITATES VIRAL FUSION
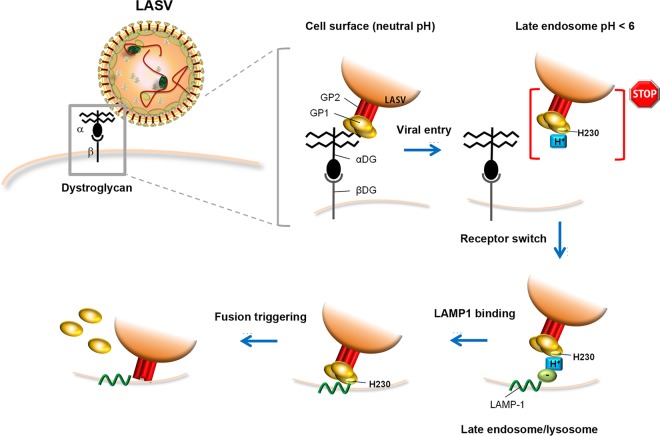
Like other early endosomal compartments, early macropinosomes undergo maturation (62). Recent studies revealed that macropinosome maturation is crucial for productive VACV entry (63), but it is unknown to what extent this applies to LASV. Moreover, the fate of late macropinosomes is unclear and may involve fusion with classical late endosomes and lysosomes. Since LASV passes through late endosomes and depends on the endosomal sorting complex required for transport for entry (49), it will be of interest to see if and at which point incoming LASV “merges” into the classical late endosomal route. Using an unbiased haploid screening approach, Jae et al. identified lysosome-associated membrane protein 1 (LAMP1) as a late endosomal entry factor required by LASV (64). Under the acidic conditions of the late endosome, the virus dissociated from its high-affinity receptor DG and engaged LAMP1, which triggered efficient fusion. Recent structural analysis of LASV GP1 combined with functional studies provided insights into the mechanisms underlying this “receptor switch” (Fig. 1). X-ray analysis revealed the existence of a stable low-pH conformation of LASV GP1 displaying a triad of histidine residues that form a binding site for LAMP1 and that is conserved among Old World arenaviruses (65). Recent electron cryotomography studies on authentic LASV particles revealed conformational changes in GP1 to occur under pH 5, in line with the X-ray data (66). Although LAMP1 is crucial for productive LASV entry (64), LAMP1 binding is not strictly required for fusion per se, evidenced by mutations within the histidine triad that were still able to undergo fusion, albeit at lower pH (67). Elegant functional studies demonstrated that residue H230 within the histidine triad on LASV GP1 undergoes protonation around pH 5.5, when GP1 starts dissociating from DG (Fig. 1). A positive charge at residue H230 had an inhibitory effect on LASV GP fusion activity, preventing premature fusion. Engagement of GP1 protonated at H230 with LAMP1 may neutralize the positive charge via a countercharge provided by LAMP1, promoting fusion triggering (67) (Fig. 1). These studies reveal a remarkable role of the histidine triad in orchestrating the fusion activity of LASV GP with the timing and location of the receptor switch from DG to LAMP1. This scenario further suggests a division of labor between DG and LAMP1 in LASV entry. Functional DG appears to serve as a high-affinity receptor that efficiently captures free virus at the cell surface via its matriglycan polysaccharides that likely reach above the glycocalyx, followed by rapid endocytosis. Whether DG requires assistance by other yet-unknown coreceptor(s) for virus internalization is currently unknown. Engagement of the late endosomal receptor LAMP1 likely guarantees optimal spatial conditions for fusion in proximity to the limiting membrane of the late endosome. The use of late endosomal entry factors by LASV has further interesting parallels to filoviruses and may reflect a more common strategy of late-penetrating viruses, as discussed in an excellent recent review (68).
FIG 1.
Current model for receptor use, cell entry, and the late endosomal receptor switch of LASV (64, 65, 67). At the cell surface, LASV GP1 engages the O-linked matriglycan polysaccharides displayed by α-DG, followed by endocytosis via an unusual pathway related to macropinocytosis. Progressive acidification of late endosomes induces a structural change in LASV GP1, which dissociates from DG and adapts a low-pH conformation displaying a histidine triad. Protonation of residue H230 “locks” GP1 in the prefusion state, preventing premature fusion. Engagement of LAMP1 neutralizes the positive charge on H230 of GP1 and triggers efficient fusion with the limiting membrane of the late endosome/lysosome (for details, please see the text).
PERSPECTIVES AND CHALLENGES
Recent developments on LASV entry provided novel insights into the complex interaction of this pathogen with the host cell. At the same time, new questions arose that need to be addressed. As pointed out above, several lines of evidence support the notion that DG's function as a LASV receptor critically depends on posttranslational modification. However, the tissue tropism of the virus does not always correlate with the extent of DG's functional glycosylation. This is illustrated by skeletal muscle that expresses DG with long matriglycan chains and high LASV binding affinity (19) but seems largely resistant to infection by LCMV (69) and LASV (70, 71). Recent studies revealed that the resistance of differentiated myotubes against LCMV lies at the level of viral entry (72), suggesting that expression of functionally glycosylated DG per se is insufficient for productive infection. Considering the complex interaction pattern of DG with cellular proteins, cell type-specific DG complexes likely represent the “functional units” of virus entry. Preexisting steady-state interactions of DG with specific cellular factors may thus influence DG's ability to function as a viral receptor. Moreover, some data at hand suggest that virus binding to DG induces receptor signaling and affects the molecular composition of the complex. It is therefore conceivable that virus engagement of the receptor induces a dynamic pattern of protein-protein interactions involved in the entry process, as recently illustrated in a groundbreaking study on hepatitis C virus entry (73). The advent of unbiased shotgun proteomics approaches, including sensitive label-free quantification, provides new and powerful techniques to address these questions (74).
Cell entry of LASV critically depends on cellular kinases (55, 56), indicating a role of signaling in LASV entry. The virus may actively induce cellular signaling to promote entry, as well as to “prime” the host cell to facilitate subsequent steps of infection. Since viruses are opportunistic and may create their own pathways by reshuffling cellular factors according to their needs, a focus on specific signaling pathways may face some limitations. Recently, quantitative phosphoproteomics was successfully used to dissect the complex signaling events following the attachment of human immunodeficiency virus type 1 (75), paving the way for similar studies on emerging viruses. Candidate signaling pathways involved in productive LASV entry might be integrated into an “LASV entry network,” allowing the identification of promising drug targets. Since candidate signaling molecules may represent already-known drug targets in other human disorders, clinically approved drugs or drug candidates in advanced stages of development may be repurposed to combat this important human pathogen.
ACKNOWLEDGMENTS
We apologize to all those colleagues whose excellent work could not be covered due to space limitations.
This research was supported by Swiss National Science Foundation grant 310030_149746 to S.K. and funds to S.K. from the University of Lausanne.
REFERENCES
- 1.McCormick JB, Fisher-Hoch SP.. 2002. Lassa fever. Curr Top Microbiol Immunol 262:75–109. [DOI] [PubMed] [Google Scholar]
- 2.Buchmeier MJ, de la Torre JC, Peters CJ. 2007. Arenaviridae: the viruses and their replication, p 1791–1828. In Knipe DL, Howley PM (ed), Fields virology, 4th ed Lippincott-Raven, Philadelphia, PA. [Google Scholar]
- 3.Cosset FL, Marianneau P, Verney G, Gallais F, Tordo N, Pecheur EI, ter Meulen J, Deubel V, Bartosch B. 2009. Characterization of Lassa virus cell entry and neutralization with Lassa virus pseudoparticles. J Virol 83:3228–3237. doi: 10.1128/JVI.01711-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Klewitz C, Klenk HD, ter Meulen J. 2007. Amino acids from both N-terminal hydrophobic regions of the Lassa virus envelope glycoprotein GP-2 are critical for pH-dependent membrane fusion and infectivity. J Gen Virol 88:2320–2328. doi: 10.1099/vir.0.82950-0. [DOI] [PubMed] [Google Scholar]
- 5.Nunberg JH, York J. 2012. The curious case of arenavirus entry, and its inhibition. Viruses 4:83–101. doi: 10.3390/v4010083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Andersen KG, Shapiro BJ, Matranga CB, Sealfon R, Lin AE, Moses LM, Folarin OA, Goba A, Odia I, Ehiane PE, Momoh M, England EM, Winnicki S, Branco LM, Gire SK, Phelan E, Tariyal R, Tewhey R, Omoniwa O, Fullah M, Fonnie R, Fonnie M, Kanneh L, Jalloh S, Gbakie M, Saffa S, Karbo K, Gladden AD, Qu J, Stremlau M, Nekoui M, Finucane HK, Tabrizi S, Vitti JJ, Birren B, Fitzgerald M, McCowan C, Ireland A, Berlin AM, Bochicchio J, Tazon-Vega B, Lennon NJ, Ryan EM, Bjornson Z, Milner DA Jr, Lukens AK, Broodie N, Rowland M, Heinrich M, Akdag M, et al. 2015. Clinical sequencing uncovers origins and evolution of Lassa virus. Cell 162:738–750. doi: 10.1016/j.cell.2015.07.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McCormick JB, King IJ, Webb PA, Johnson KM, O'Sullivan R, Smith ES, Trippel S, Tong TC. 1987. A case-control study of the clinical diagnosis and course of Lassa fever. J Infect Dis 155:445–455. doi: 10.1093/infdis/155.3.445. [DOI] [PubMed] [Google Scholar]
- 8.Geisbert TW, Jahrling PB. 2004. Exotic emerging viral diseases: progress and challenges. Nat Med 10:S110–S121. doi: 10.1038/nm1142. [DOI] [PubMed] [Google Scholar]
- 9.McCormick JB, King IJ, Webb PA, Scribner CL, Craven RB, Johnson KM, Elliott LH, Belmont-Williams R. 1986. Lassa fever. Effective therapy with ribavirin. N Engl J Med 314:20–26. [DOI] [PubMed] [Google Scholar]
- 10.Stephenson EH, Larson EW, Dominik JW. 1984. Effect of environmental factors on aerosol-induced Lassa virus infection. J Med Virol 14:295–303. doi: 10.1002/jmv.1890140402. [DOI] [PubMed] [Google Scholar]
- 11.Borio L, Inglesby T, Peters CJ, Schmaljohn AL, Hughes JM, Jahrling PB, Ksiazek T, Johnson KM, Meyerhoff A, O'Toole T, Ascher MS, Bartlett J, Breman JG, Eitzen EM Jr, Hamburg M, Hauer J, Henderson DA, Johnson RT, Kwik G, Layton M, Lillibridge S, Nabel GJ, Osterholm MT, Perl TM, Russell P, Tonat K, Working Group on Civilian Biodefense . 2002. Hemorrhagic fever viruses as biological weapons: medical and public health management. JAMA 287:2391–2405. doi: 10.1001/jama.287.18.2391. [DOI] [PubMed] [Google Scholar]
- 12.Cao W, Henry MD, Borrow P, Yamada H, Elder JH, Ravkov EV, Nichol ST, Compans RW, Campbell KP, Oldstone MB. 1998. Identification of alpha-dystroglycan as a receptor for lymphocytic choriomeningitis virus and Lassa fever virus. Science 282:2079–2081. doi: 10.1126/science.282.5396.2079. [DOI] [PubMed] [Google Scholar]
- 13.Spiropoulou CF, Kunz S, Rollin PE, Campbell KP, Oldstone MB. 2002. New World arenavirus clade C, but not clade A and B viruses, utilizes alpha-dystroglycan as its major receptor. J Virol 76:5140–5146. doi: 10.1128/JVI.76.10.5140-5146.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Barresi R, Campbell KP. 2006. Dystroglycan: from biosynthesis to pathogenesis of human disease. J Cell Sci 119:199–207. doi: 10.1242/jcs.02814. [DOI] [PubMed] [Google Scholar]
- 15.Yoshida-Moriguchi T, Campbell KP. 2015. Matriglycan: a novel polysaccharide that links dystroglycan to the basement membrane. Glycobiology 25:702–713. doi: 10.1093/glycob/cwv021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yoshida-Moriguchi T, Willer T, Anderson ME, Venzke D, Whyte T, Muntoni F, Lee H, Nelson SF, Yu L, Campbell KP. 2013. SGK196 is a glycosylation-specific O-mannose kinase required for dystroglycan function. Science 341:896–899. doi: 10.1126/science.1239951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Inamori K, Yoshida-Moriguchi T, Hara Y, Anderson ME, Yu L, Campbell KP. 2012. Dystroglycan function requires xylosyl- and glucuronyltransferase activities of LARGE. Science 335:93–96. doi: 10.1126/science.1214115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Praissman JL, Willer T, Sheikh MO, Toi A, Chitayat D, Lin YY, Lee H, Stalnaker SH, Wang S, Prabhakar PK, Nelson SF, Stemple DL, Moore SA, Moremen KW, Campbell KP, Wells L. 2016. The functional O-mannose glycan on alpha-dystroglycan contains a phospho-ribitol primed for matriglycan addition. eLife 5:e14473. doi: 10.7554/eLife.14473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Goddeeris MM, Wu B, Venzke D, Yoshida-Moriguchi T, Saito F, Matsumura K, Moore SA, Campbell KP. 2013. LARGE glycans on dystroglycan function as a tunable matrix scaffold to prevent dystrophy. Nature 503:136–140. doi: 10.1038/nature12605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Briggs DC, Yoshida-Moriguchi T, Zheng T, Venzke D, Anderson ME, Strazzulli A, Moracci M, Yu L, Hohenester E, Campbell KP. 2016. Structural basis of laminin binding to the LARGE glycans on dystroglycan. Nat Chem Biol 12:810–814. doi: 10.1038/nchembio.2146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kunz S, Rojek JM, Kanagawa M, Spiropoulou CF, Barresi R, Campbell KP, Oldstone MB. 2005. Posttranslational modification of alpha-dystroglycan, the cellular receptor for arenaviruses, by the glycosyltransferase LARGE is critical for virus binding. J Virol 79:14282–14296. doi: 10.1128/JVI.79.22.14282-14296.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rojek JM, Spiropoulou CF, Campbell KP, Kunz S. 2007. Old World and clade C New World arenaviruses mimic the molecular mechanism of receptor recognition used by alpha-dystroglycan's host-derived ligands. J Virol 81:5685–5695. doi: 10.1128/JVI.02574-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jae LT, Raaben M, Riemersma M, van Beusekom E, Blomen VA, Velds A, Kerkhoven RM, Carette JE, Topaloglu H, Meinecke P, Wessels MW, Lefeber DJ, Whelan SP, van Bokhoven H, Brummelkamp TR. 2013. Deciphering the glycosylome of dystroglycanopathies using haploid screens for Lassa virus entry. Science 340:479–483. doi: 10.1126/science.1233675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sabeti PC, Varilly P, Fry B, Lohmueller J, Hostetter E, Cotsapas C, Xie X, Byrne EH, McCarroll SA, Gaudet R, Schaffner SF, Lander ES, Frazer KA, Ballinger DG, Cox DR, Hinds DA, Stuve LL, Gibbs RA, Belmont JW, Boudreau A, Hardenbol P, Leal SM, Pasternak S, Wheeler DA, Willis TD, Yu F, Yang H, Zeng C, Gao Y, Hu H, Hu W, Li C, Lin W, Liu S, Pan H, Tang X, Wang J, Wang W, Yu J, Zhang B, Zhang Q, Zhao H, Zhou J, Gabriel SB, Barry R, Blumenstiel B, Camargo A, Defelice M, Faggart M, Goyette M, et al. 2007. Genome-wide detection and characterization of positive selection in human populations. Nature 449:913–918. doi: 10.1038/nature06250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Andersen KG, Shylakhter I, Tabrizi S, Grossman SR, Happi CT, Sabeti PC. 2012. Genome-wide scans provide evidence for positive selection of genes implicated in Lassa fever. Philos Trans R Soc Lond B Biol Sci 367:868–877. doi: 10.1098/rstb.2011.0299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Grove J, Marsh M. 2011. The cell biology of receptor-mediated virus entry. J Cell Biol 195:1071–1082. doi: 10.1083/jcb.201108131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yang B, Jung D, Motto D, Meyer J, Koretzky G, Campbell KP. 1995. SH3 domain-mediated interaction of dystroglycan and Grb2. J Biol Chem 270:11711–11714. doi: 10.1074/jbc.270.20.11711. [DOI] [PubMed] [Google Scholar]
- 28.Spence HJ, Dhillon AS, James M, Winder SJ. 2004. Dystroglycan, a scaffold for the ERK-MAP kinase cascade. EMBO Rep 5:484–489. doi: 10.1038/sj.embor.7400140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cavaldesi M, Macchia G, Barca S, Defilippi P, Tarone G, Petrucci TC. 1999. Association of the dystroglycan complex isolated from bovine brain synaptosomes with proteins involved in signal transduction. J Neurochem 72:1648–1655. [DOI] [PubMed] [Google Scholar]
- 30.Moraz ML, Pythoud C, Turk R, Rothenberger S, Pasquato A, Campbell KP, Kunz S. 2013. Cell entry of Lassa virus induces tyrosine phosphorylation of dystroglycan. Cell Microbiol 15:689–700. doi: 10.1111/cmi.12078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ferletta M, Kikkawa Y, Yu H, Talts JF, Durbeej M, Sonnenberg A, Timpl R, Campbell KP, Ekblom P, Genersch E. 2003. Opposing roles of integrin alpha6Abeta1 and dystroglycan in laminin-mediated extracellular signal-regulated kinase activation. Mol Biol Cell 14:2088–2103. doi: 10.1091/mbc.E03-01-0852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rojek JM, Moraz ML, Pythoud C, Rothenberger S, Van der Goot FG, Campbell KP, Kunz S. 2012. Binding of Lassa virus perturbs extracellular matrix-induced signal transduction via dystroglycan. Cell Microbiol 14:1122–1134. doi: 10.1111/j.1462-5822.2012.01784.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Shimojima M, Kawaoka Y. 2012. Cell surface molecules involved in infection mediated by lymphocytic choriomeningitis virus glycoprotein. J Vet Med Sci 74:1363–1366. doi: 10.1292/jvms.12-0176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Shimojima M, Stroher U, Ebihara H, Feldmann H, Kawaoka Y. 2012. Identification of cell surface molecules involved in dystroglycan-independent Lassa virus cell entry. J Virol 86:2067–2078. doi: 10.1128/JVI.06451-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lemke G, Burstyn-Cohen T. 2010. TAM receptors and the clearance of apoptotic cells. Ann N Y Acad Sci 1209:23–29. doi: 10.1111/j.1749-6632.2010.05744.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lemke G, Rothlin CV. 2008. Immunobiology of the TAM receptors. Nat Rev Immunol 8:327–336. doi: 10.1038/nri2303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Amara A, Mercer J. 2015. Viral apoptotic mimicry. Nat Rev Microbiol 13:461–469. doi: 10.1038/nrmicro3469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Morizono K, Chen IS. 2014. Role of phosphatidylserine receptors in enveloped virus infection. J Virol 88:4275–4290. doi: 10.1128/JVI.03287-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Morizono K, Xie Y, Olafsen T, Lee B, Dasgupta A, Wu AM, Chen IS. 2011. The soluble serum protein Gas6 bridges virion envelope phosphatidylserine to the TAM receptor tyrosine kinase Axl to mediate viral entry. Cell Host Microbe 9:286–298. doi: 10.1016/j.chom.2011.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Meertens L, Carnec X, Lecoin MP, Ramdasi R, Guivel-Benhassine F, Lew E, Lemke G, Schwartz O, Amara A. 2012. The TIM and TAM families of phosphatidylserine receptors mediate dengue virus entry. Cell Host Microbe 12:544–557. doi: 10.1016/j.chom.2012.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Frei AP, Jeon OY, Kilcher S, Moest H, Henning LM, Jost C, Pluckthun A, Mercer J, Aebersold R, Carreira EM, Wollscheid B. 2012. Direct identification of ligand-receptor interactions on living cells and tissues. Nat Biotechnol 30:997–1001. doi: 10.1038/nbt.2354. [DOI] [PubMed] [Google Scholar]
- 42.Mercer J, Helenius A. 2008. Vaccinia virus uses macropinocytosis and apoptotic mimicry to enter host cells. Science 320:531–535. doi: 10.1126/science.1155164. [DOI] [PubMed] [Google Scholar]
- 43.Jemielity S, Wang JJ, Chan YK, Ahmed AA, Li W, Monahan S, Bu X, Farzan M, Freeman GJ, Umetsu DT, Dekruyff RH, Choe H. 2013. TIM-family proteins promote infection of multiple enveloped viruses through virion-associated phosphatidylserine. PLoS Pathog 9:e1003232. doi: 10.1371/journal.ppat.1003232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sullivan BM, Welch MJ, Lemke G, Oldstone MB. 2013. Is the TAM receptor Axl a receptor for lymphocytic choriomeningitis virus? J Virol 87:4071–4074. doi: 10.1128/JVI.03268-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Van Breedam W, Pohlmann S, Favoreel HW, de Groot RJ, Nauwynck HJ. 2014. Bitter-sweet symphony: glycan-lectin interactions in virus biology. FEMS Microbiol Rev 38:598–632. doi: 10.1111/1574-6976.12052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Goncalves AR, Moraz ML, Pasquato A, Helenius A, Lozach PY, Kunz S. 2013. Role of DC-SIGN in Lassa virus entry into human dendritic cells. J Virol 87:11504–11515. doi: 10.1128/JVI.01893-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lozach PY, Kuhbacher A, Meier R, Mancini R, Bitto D, Bouloy M, Helenius A. 2011. DC-SIGN as a receptor for phleboviruses. Cell Host Microbe 10:75–88. doi: 10.1016/j.chom.2011.06.007. [DOI] [PubMed] [Google Scholar]
- 48.Rojek JM, Sanchez AB, Nguyen NT, de la Torre JC, Kunz S. 2008. Different mechanisms of cell entry by human-pathogenic Old World and New World arenaviruses. J Virol 82:7677–7687. doi: 10.1128/JVI.00560-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Pasqual G, Rojek JM, Masin M, Chatton JY, Kunz S. 2011. Old World arenaviruses enter the host cell via the multivesicular body and depend on the endosomal sorting complex required for transport. PLoS Pathog 7:e1002232. doi: 10.1371/journal.ppat.1002232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Quirin K, Eschli B, Scheu I, Poort L, Kartenbeck J, Helenius A. 2008. Lymphocytic choriomeningitis virus uses a novel endocytic pathway for infectious entry via late endosomes. Virology 378:21–33. doi: 10.1016/j.virol.2008.04.046. [DOI] [PubMed] [Google Scholar]
- 51.Panda D, Das A, Dinh PX, Subramaniam S, Nayak D, Barrows NJ, Pearson JL, Thompson J, Kelly DL, Ladunga I, Pattnaik AK. 2011. RNAi screening reveals requirement for host cell secretory pathway in infection by diverse families of negative-strand RNA viruses. Proc Natl Acad Sci U S A 108:19036–19041. doi: 10.1073/pnas.1113643108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Iwasaki M, Ngo N, de la Torre JC. 2014. Sodium hydrogen exchangers contribute to arenavirus cell entry. J Virol 88:643–654. doi: 10.1128/JVI.02110-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Mercer J, Schelhaas M, Helenius A. 2010. Virus entry by endocytosis. Annu Rev Biochem 79:803–833. doi: 10.1146/annurev-biochem-060208-104626. [DOI] [PubMed] [Google Scholar]
- 54.Mercer J, Helenius A. 2012. Gulping rather than sipping: macropinocytosis as a way of virus entry. Curr Opin Microbiol 15:490–499. doi: 10.1016/j.mib.2012.05.016. [DOI] [PubMed] [Google Scholar]
- 55.Oppliger J, Torriani G, Herrador A, Kunz S. 2016. Lassa virus cell entry via dystroglycan involves an unusual pathway of macropinocytosis. J Virol 90:6412–6429. doi: 10.1128/JVI.00257-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Mohr EL, McMullan LK, Lo MK, Spengler JR, Bergeron E, Albarino CG, Shrivastava-Ranjan P, Chiang CF, Nichol ST, Spiropoulou CF, Flint M. 2015. Inhibitors of cellular kinases with broad-spectrum antiviral activity for hemorrhagic fever viruses. Antiviral Res 120:40–47. doi: 10.1016/j.antiviral.2015.05.003. [DOI] [PubMed] [Google Scholar]
- 57.Mercer J, Helenius A. 2009. Virus entry by macropinocytosis. Nat Cell Biol 11:510–520. doi: 10.1038/ncb0509-510. [DOI] [PubMed] [Google Scholar]
- 58.Krieger SE, Kim C, Zhang L, Marjomaki V, Bergelson JM. 2013. Echovirus 1 entry into polarized Caco-2 cells depends on dynamin, cholesterol, and cellular factors associated with macropinocytosis. J Virol 87:8884–8895. doi: 10.1128/JVI.03415-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Krzyzaniak MA, Zumstein MT, Gerez JA, Picotti P, Helenius A. 2013. Host cell entry of respiratory syncytial virus involves macropinocytosis followed by proteolytic activation of the F protein. PLoS Pathog 9:e1003309. doi: 10.1371/journal.ppat.1003309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.de Vries E, Tscherne DM, Wienholts MJ, Cobos-Jimenez V, Scholte F, Garcia-Sastre A, Rottier PJ, de Haan CAM. 2011. Dissection of the influenza A virus endocytic routes reveals macropinocytosis as an alternative entry pathway. PLoS Pathog 7:e1001329. doi: 10.1371/journal.ppat.1001329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Sánchez EG, Quintas A, Perez-Nunez D, Nogal M, Barroso S, Carrascosa AL, Revilla Y. 2012. African swine fever virus uses macropinocytosis to enter host cells. PLoS Pathog 8:e1002754. doi: 10.1371/journal.ppat.1002754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Scott CC, Vacca F, Gruenberg J. 2014. Endosome maturation, transport and functions. Semin Cell Dev Biol 31:2–10. [DOI] [PubMed] [Google Scholar]
- 63.Rizopoulos Z, Balistreri G, Kilcher S, Martin CK, Syedbasha M, Helenius A, Mercer J. 2015. Vaccinia virus infection requires maturation of macropinosomes. Traffic 16:814–831. doi: 10.1111/tra.12290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Jae LT, Raaben M, Herbert AS, Kuehne AI, Wirchnianski AS, Soh TK, Stubbs SH, Janssen H, Damme M, Saftig P, Whelan SP, Dye JM, Brummelkamp TR. 2014. Virus entry. Lassa virus entry requires a trigger-induced receptor switch. Science 344:1506–1510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Cohen-Dvashi H, Cohen N, Israeli H, Diskin R. 2015. Molecular mechanism for LAMP1 recognition by Lassa virus. J Virol 89:7584–7592. doi: 10.1128/JVI.00651-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Li S, Sun Z, Pryce R, Parsy ML, Fehling SK, Schlie K, Siebert CA, Garten W, Bowden TA, Strecker T, Huiskonen JT. 2016. Acidic pH-induced conformations and LAMP1 binding of the Lassa virus glycoprotein spike. PLoS Pathog 12:e1005418. doi: 10.1371/journal.ppat.1005418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Cohen-Dvashi H, Israeli H, Shani O, Katz A, Diskin R. 2016. Role of LAMP1 binding and pH sensing by the spike complex of Lassa virus. J Virol 90:10329–10338. doi: 10.1128/JVI.01624-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Jae LT, Brummelkamp TR. 2015. Emerging intracellular receptors for hemorrhagic fever viruses. Trends Microbiol 23:392–400. doi: 10.1016/j.tim.2015.04.006. [DOI] [PubMed] [Google Scholar]
- 69.Fazakerley JK, Southern P, Bloom F, Buchmeier MJ. 1991. High resolution in situ hybridization to determine the cellular distribution of lymphocytic choriomeningitis virus RNA in the tissues of persistently infected mice: relevance to arenavirus disease and mechanisms of viral persistence. J Gen Virol 72:1611–1625. doi: 10.1099/0022-1317-72-7-1611. [DOI] [PubMed] [Google Scholar]
- 70.Walker DH, McCormick JB, Johnson KM, Webb PA, Komba-Kono G, Elliott LH, Gardner JJ. 1982. Pathologic and virologic study of fatal Lassa fever in man. Am J Pathol 107:349–356. [PMC free article] [PubMed] [Google Scholar]
- 71.Yun NE, Walker DH. 2012. Pathogenesis of Lassa fever. Viruses 4:2031–2048. doi: 10.3390/v4102031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Iwasaki M, Urata S, Cho Y, Ngo N, de la Torre JC. 2014. Cell entry of lymphocytic choriomeningitis virus is restricted in myotubes. Virology 458–459:22–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Gerold G, Meissner F, Bruening J, Welsch K, Perin PM, Baumert TF, Vondran FW, Kaderali L, Marcotrigiano J, Khan AG, Mann M, Rice CM, Pietschmann T. 2015. Quantitative proteomics identifies serum response factor binding protein 1 as a host factor for hepatitis C virus entry. Cell Rep 12:864–878. doi: 10.1016/j.celrep.2015.06.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Gerold G, Bruening J, Pietschmann T. 2015. Decoding protein networks during virus entry by quantitative proteomics. Virus Res 218:25–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Wojcechowskyj JA, Didigu CA, Lee JY, Parrish NF, Sinha R, Hahn BH, Bushman FD, Jensen ST, Seeholzer SH, Doms RW. 2013. Quantitative phosphoproteomics reveals extensive cellular reprogramming during HIV-1 entry. Cell Host Microbe 13:613–623. doi: 10.1016/j.chom.2013.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]