Summary
There is a paucity of evidence regarding incidence and causes of hypothermia in patients with major burns and its impact on outcomes. This paper identifies contributing factors to hypothermia and its relationship with the severity of physiological scoring systems on admission to a tertiary centre. Patients with burns >20% TBSA admitted between March 2010 and July 2013 comprised this retrospective survey. Data relating to causative factors at time of burn, during transfer, physiological outcome scores (BOBI, SOFA, RTS and APACHE II), length of hospital stay and mortality were collected. SPSS statistical software was used for analysis. The study included 31 patients (medians: age 32 years, burn size 30% TBSA). 13% (n=4) of patients died during hospital admission. 42% (n=13) of patients had a temperature <36.0C on arrival. Temperature on arrival at the burns centre was related to the severity of all physiological scores (p=<0.001). There was no difference between groups in terms of mortality in hospital (p=0.151) or length of hospital stay (p=0.547). Our results show that hypothermia is related to burn severity and patient physiological status. They do not show a relationship between hypothermia and external factors at the time of the burn. This paper prompts further investigation into the prevention of hypothermia in patients with major burns.
Keywords: burns, hypothermia, transfer, intensive care, outcome
Abstract
Il n’existe que peu de données sur l’incidence et les causes de survenue d’une hypothermie chez les brûlés, ni de son incidence sur le devenir. Cette étude répertorie les facteurs contribuant à l’hypothermie à l’admission dans un centre de référence et sa relation avec les scores de gravité initiaux. Cette étude rétrospective a concerné les patients brûlés sur plus de 20% de SCT admis entre mars 2010 et juillet 2013. Les données concernant les causes d’hypothermie au moment de la brûlure et pendant le transfert, les scores de gravité (BOBI, SOFA, RTS et APACHE II), la durée de séjour et la mortalité ont été relevées. Trente et un dossiers ont été étudiés (âge médian 32 ans, surface brûlée 30%). Quatre (13%) d’ente eux décédés. Treize (42%) avait une température <36°C à l’admission et il existait une corrélation entre la température et les scores de gravité (p<0.001). Il n’y avait pas de différence en termes de mortalité ni de durée de séjour. Cette étude montre que l’hypothermie est corrélée à la gravité de la brûlure et à la gravité générale des patients. On ne retrouve pas de relation entre les facteurs environnementaux au moment de la brûlure et l’hypothermie. Des données supplémentaires sont nécessaires pour la prévention de l’hypothermie liée à la brûlure.
Introduction
Hypothermia is variably defined as a core body temperature less than 36°C or less than 35°C.1,2 Normothermia, a body temperature above 36°C, is required to maintain the functioning of body systems, and a drop in temperature can have widespread physiological effects. These consequences depend on the cause of the temperature drop, its severity and the general condition of the patient.
In patients who have suffered trauma, the negative effects of hypothermia are significant and well documented.3 Hypothermia combined with coagulopathy and acidosis in trauma patients is described as a ‘lethal triad’ as each factor exacerbates the others.4 The incidence of admission hypothermia in trauma patients ranges from 10-66% and there is an increase in both mortality and morbidity in this group.3 Hypothermic trauma patients need greater fluid administration, more blood transfusions and require longer hospital stays when compared to those who are normothermic.4,5,6
There is evidence that hypothermia also has negative consequences in burns patients, although it has been less well studied in this group. Two large retrospective reviews of trauma registries in the US have shown an association between hypothermia and mortality in burns patients.7,8 These studies suggest a number of factors to be associated with the development of hypothermia. These include increasing burn size, season of injury, association with polytrauma, a Glasgow Coma Score (GCS) less than 8 and age greater than 60 years.7
Burns patients are at risk of becoming hypothermic both at the scene of injury and during transfer to hospital. There are factors intrinsic to the type and severity of injury that may predispose to the development of hypothermia and also external factors at scene and in transfer that may contribute. These factors have not previously been investigated. It is the aim of our study to assess the incidence of hypothermia in patients with major burns and the causative factors in these patients.
Methods
This retrospective survey was conducted in accordance with the UK GCP code (clinical governance reference number CAPP 954). It was performed at Chelsea and Westminster Hospital Burns Unit, London, UK. The burns service at this hospital treats approximately 1,300 new inpatients every year and is the only burns service in central London providing care for adults and children with complex injuries. There are 9 adult inpatient beds, 2 high dependency beds and 2 intensive care beds, and a further 6 inpatient paediatric beds.
Data was collected from the hospital records – both the hard copy and computerised records. Patients with burns greater than 20% Total Body Surface Area (TBSA) admitted to the burns centre between March 2010 and July 2013 were included. Patients were excluded if they were not transferred to the burns centre for their initial care.
For each patient, data was collected pertaining to demographic variables including sex and age. Data was also collected relating to the mechanism of the burn, the extent of the injury, the initial first-aid management, details relating to the transfer of the patient, the core temperature of the patient at each stage of their transfer, and physiological parameters of the patient both on arrival at the referring hospital and on arrival and after 24 hours at Chelsea and Westminster burns unit.
Temperature measurements were taken at the scene, in A&E and on the wards at both the referring hospital and Chelsea and Westminster, using either tympanic measurements or tempadot©, and in the intensive care unit using oesophageal monitoring (Smith’s Medical oesophageal temperature sensor). A number of different warming methods for the prevention of heat loss in transfer were employed, including wrapping the burns in cling film, wrapping patients in bubble wrap, or using warming blankets and infusions of warmed saline.
Physiological outcome scores were calculated. Firstly, the Revised Trauma Score8 (RTS), which is a scoring system that indicates the severity of the injury at triage. Secondly, the Belgian Outcome in Burn Injury9 (BOBI) score, which indicates the severity of the injury and gives an indicator of the predicted mortality. Thirdly, the Sepsis-related Organ Failure Assessment10 (SOFA), which describes organ dysfunction or failure and aids with daily management of the patient. Lastly, the Acute Physiology and Chronic Health Evaluation score11 (APACHE II), which is a severity of disease classification and indicates overall response to injury in the first 24 hours. These scores have all been validated as accurate predictors of mortality in burns patients.9,12,13,14
Patients were divided into 2 groups for data analyses – those that had a temperature less than 36.0°C on arrival at Chelsea and Westminster (the hypothermic group) and those that had a temperature greater than 36.0°C on arrival (the nonhypothermic group). Data analysis was carried out using SPSS statistical software. Chi-squared tests were used for categorical variables such as mortality. Mann-Whitney U tests were used for comparing continuous data that was not normally distributed. Spearman’s Rank correlation coefficient was used to measure the strength of association between groups of nonparametric data. Temperatures were converted into percentage of 37.0°C for analyses using Spearman’s rank correlation coefficient. P values of less than 0.05 were considered significant. Data is represented as a median plus the range. For non-parametric data the interquartile range (IQR) is quoted.
Patients were secondarily divided into hypothermic and non-hypothermic groups based on their temperature on arrival at the referring hospital and all data analysis was repeated based on dividing the patients into these groups
Results
Patient demographics
During the period of study (March 2010 – July 2013) fifty patients were admitted to Chelsea and Westminster with burns of greater than 20% TBSA. A total of 19 patients were excluded from the survey, 13 because their initial management was carried out at another burns centre and they were referred to us only for ongoing care, and 6 because insufficient data was available (as illustrated in Fig. 1).
Fig. 1. Included and excluded patients (CONSORT flow diagram).
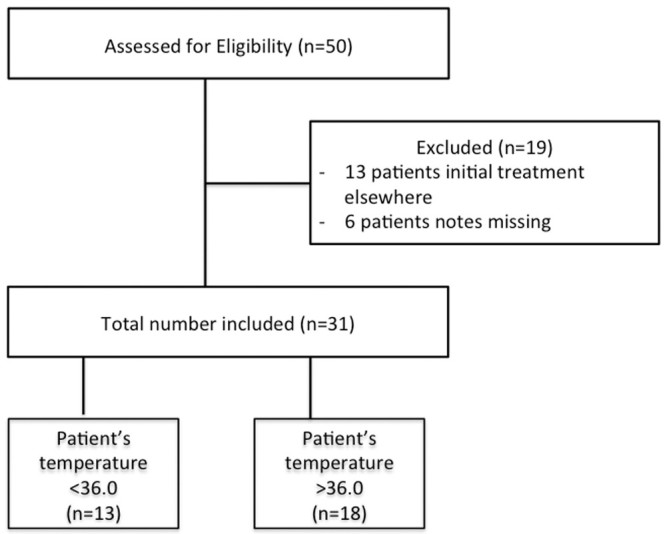
Patient demographics are shown in Table I. A total of 31 patients were included in the study. Fourteen of these patients were female and 17 male. The median age was 32 years (range 4-96 years). Four patients died during their inpatient stay, of these 3 were hypothermic on arrival at the burns unit.
Table I. Patient demographics.
On arrival at Chelsea and Westminster, temperature was recorded in all patients and 42% (n=13) of patients had a core temperature less than 36.0°C. Of the hypothermic group, 10 had a temperature between 35.0°C and 36.0°C and 3 had a temperature less than 35.0°C. The median temperature on arrival at Chelsea and Westminster was 36.0°C (IQR 35.6-36.7°C). Temperature was recorded at the scene in only 26% (n=8) of patients.
Patients’ burn injuries more commonly occurred during the night (61% n=19) and more in Spring or Summer (81%, n=25) than in Autumn or Winter (19%, n=6). The most common mechanism of burning was flame (71%, n=22), followed by scald (16%, n=5) and electrical (13%, n=4). Injuries occurred more frequently indoors (71%, n=22) than outdoors (29% n=9). Adequate first aid was only provided in 42% of patients (n=13). No difference was shown between hypothermic or non-hypothermic groups both on arrival at Chelsea and Westminster and on arrival at the referring hospital for time of day, season, mechanism of burn, location of injury or dependent on whether adequate first aid was provided. There was no difference between hypothermic or non-hypothermic groups both on arrival at Chelsea and Westminster or at the referring hospital in terms of mortality or length of hospital stay
Methods to prevent heat loss during transfer were documented for 84% (n=26) of patients. The most common method of preventing heat loss documented was the use of cling film (80%, n=25). Other methods documented included blankets (3%, n=1), Bair hugger (3%, n=1), bubble wrap (3%, n=1) and warmed saline (3%, n=1).
Patient transfers comprised the transfer from scene to hospital (transfer A) and from referring hospital to Chelsea and Westminster (transfer B). The median total time in transfer (A+B) was 85 minutes (IQR 45-105 miles). Change in temperature between the referring hospital and Chelsea and Westminster was significantly related to total length of time spent in transfer (p<0.001). Temperature on arrival at Chelsea and Westminster was not related to total time spent in transfer.
The median total distance of transfer (A+B) was 13.0 miles (IQR 10.8-27.5 miles). Change in temperature between hospitals was not related to total distance of transfer. Temperature on arrival at Chelsea and Westminster was not related to total distance of transfer. There was no difference between hypothermic and non-hypothermic groups on arrival at Chelsea and Westminster in terms of total distance of transfer.
Transfer B was by ambulance (82%, n=23) or by helicopter plus ambulance (18%, n=5). The difference between hypothermic and non-hypothermic groups on arrival at Chelsea and Westminster in terms of mode of transport during transfer B came close to significance (p=0.097). Four of the five patients transferred by helicopter from the referring hospital to Chelsea and Westminster were hypothermic on arrival.
Table II shows the relationships between transfer time and distance and temperature on arrival at the referring hospital and Chelsea and Westminster. Table III shows the modes of transport and relationships with hypothermia.
Table II. Relationships between transfer time and distance and temperature on arrival at referring hospital and Chelsea and Westminster.
Table III. Modes of transport and relationships with hypothermia on arrival at referring hospital and Chelsea and Westminster.
Physiological scoring systems and outcomes
The median Belgian Outcome in Burn Injury (BOBI) score for all patients was 2 (IQR 1-4). The median APACHE II score for all patients was 8.5 (IQR 5.3–12). The median Sepsis related Organ Failure Assessment (SOFA) score for all patients in the first 24 hours at Chelsea and Westminster was 4 (IQR 2- 5) and in the second 24 hours 4 (IQR 2-7). The median Revised Trauma Score was 12 (IQR 12-12). Temperature on arrival at Chelsea and Westminster was correlated with BOBI, APACHE II and SOFA scores at 24 and 48 hours (all P values <0.001). There was a significant difference between hypothermic and non-hypothermic groups on arrival at Chelsea and Westminster in terms of RTS (p=0.015) and SOFA score in the second 24 hours (p=0.045). There was no significant difference between these groups in terms of BOBI, APACHE II or SOFA score in the first 24 hours.
Four patients who were included in the study died during their inpatient stay. The median length of hospital stay was 33 days (IQR 17-57.5 days). Mortality was not related to hypothermia either on arrival at the referring hospital or arrival at Chelsea and Westminster. Length of hospital stay was not related to hypothermia or temperature on arrival at Chelsea and Westminster Hospital
Discussion
Our study has shown that 42% of patients with major burns are hypothermic on arrival at our burns centre. Furthermore this study has examined a broad spectrum of factors that could influence the development of hypothermia in this group of patients.
Patients are at significant risk of becoming hypothermic during transfer. Our results have shown a relationship between the length of time patients spent in transfer and the change in temperature between referring hospital and burns unit. Our results have also shown a relationship between the mode of transport in transfer between referring hospital and burns unit and hypothermia that comes close to significance.
Our results suggest a link between helicopter transfers and hypothermia. A previous study by Chipp et al.15 examining air ambulance transfer of patients to a UK regional burns centre found that the average temperature of patients on arrival at the burns centre was 35.8°C and 19% of patients had a peripheral temperature of less than 35.0°C. These results combined with our study support the fact that the UK HEMS clinical guidelines give clear guidance on maintaining body temperature in burns patients being transferred by helicopter.
UK guidelines for the maintenance of temperature in burns patients during transfer exist for both ambulance and helicopter transfers.16,17 The results of this study show that in the majority of patients cling film was the method of choice to prevent heat loss during transfer. Whilst this will help to prevent heat loss from the burn, it will not help to maintain the body temperature of the patient.
There is not yet clarity on the best methods for maintaining patient body temperature in transfer of burns patients. No study has been carried out to compare methods of temperature maintenance in burns patients during transfer. In patients with accidental hypothermia, evidence suggests that for patients with a core body temperature = 28°C without cardiac instability active external and minimally invasive rewarming techniques are sufficient. 18 Kjellman et al.19 compared ambient, air-convection and fluid-convection heating techniques in treating hypothermic burn patients in a burns unit and found that the fluid-convection technique was the only method that consistently increased a patient’s core temperature. Only one patient in our study was treated with warmed fluids. The results of the Kjellman study suggest that this is a method of re-warming that is under-utilised.
As well as during transfer, patients are also at risk of becoming hypothermic at the scene of injury. During management of patients at the scene there is a difficult balance between cooling the burn and maintaining patient body temperature. This study has however shown that there is no difference between hypothermic and non-hypothermic groups in terms of whether or not the burn has been adequately cooled. This is reassuring that no compromise should be made in the provision of first aid to patients with major burns.
The results of this study showed no relationship between time of day, season, location of burn (indoors vs. outdoors), mechanism of burn and whether patients were hypothermic or not on arrival at hospital. This is in contrast with the recent study by Weaver et al.7 which found that hypothermia was associated with mechanism of burn and time of year. However, their study looked at a much broader group of burns patients than this study, which looked only at burns greater than 20% TBSA, and this may account for the difference in results. Furthermore, if a greater number of the patients in our study had their temperature measured at the scene of the injury, the link between these factors and resulting temperature could have been analysed more directly.
In terms of severity of injury, this study has shown that there is a link between hypothermia and increased severity of injury as measured by the Revised Trauma Score (RTS), the Belgian Outcome in Burn Injury Score, APACHE II and SOFA scores both on admission and in the second 24 hours of admission. These results correlate with the results of previous studies that have also shown hypothermia in burns patients to be related to injury severity as measured by the Injury Severity Score (ISS).7,8,20
Only one previous study by Hostler et al.20 specifically assessed the relationship between hypothermia and mortality. That study, which looked at 12,097 burns visits and a wide group in terms of burn injury, found that admission hypothermia to a burns centre was independently associated with mortality. In trauma patients, risk of mortality is related to the severity of hypothermia.19 The size of our study prohibited further investigation into the relationship between severity of hypothermia and mortality but this is something that warrants further investigation.
In conclusion, there is a significant risk of hypothermia in patients with major burns. Hypothermia is related to injury severity and physiological response to injury. It is also related to factors in patient transfer including mode of transport and time spent in transfer. The optimum method for maintaining patient temperature in transfer is the subject for further work. Until such further work has been carried out, temperature in patients with major burns should always be assessed at the scene of injury and current guidelines followed to ensure that the risk of hypothermia in transfer is minimised
Acknowledgments
Acknowledgements.Clare Glover - for her valued assistance with the statistical analyses.
References
- 1.Mallet ML. Pathophysiology of accidental hypothermia. Q J Med. 2002;95:775–786. doi: 10.1093/qjmed/95.12.775. [DOI] [PubMed] [Google Scholar]
- 2.Peng RY, Bongard FS. Hypothermia in Trauma Patients. J Am Coll Surg. 1999;1888(6):685–696. doi: 10.1016/s1072-7515(99)00035-6. [DOI] [PubMed] [Google Scholar]
- 3.Jurkovich GJ, Greiser WB, Luterman A. Hypothermia in trauma victims: an ominous predictor of survival. J Trauma. 27;1987:1019–1024. [PubMed] [Google Scholar]
- 4.Gerecht R. The lethal triad. Hypothermia, acidosis & coagulopathy create a deadly cycle for trauma patients. JEMS. 2014;39(4):56–60. [PubMed] [Google Scholar]
- 5.Gunning KA, Sugrue M, Sloane D. Hypothermia and severe trauma. Aust N Z J Surg. 1995;65:80–82. doi: 10.1111/j.1445-2197.1995.tb07265.x. [DOI] [PubMed] [Google Scholar]
- 6.Leben J, Tryba M, Bading B. Clinical consequences of hypothermia in trauma patients. Acta Anaesthesiol Scand Suppl. 1996;109:39–41. [PubMed] [Google Scholar]
- 7.Weaver MD, Rittenberger JC, Patterson PD. Risk Factors for hypothermia in EMS-treated burn patients. Prehosp Emerg Care. 2014;18(3):335–341. doi: 10.3109/10903127.2013.864354. [DOI] [PubMed] [Google Scholar]
- 8.Champion HR, Sacco WJ, Copes WS. A revision of the Trauma Score. The Journal of Trauma. 1989;29(5):623–629. doi: 10.1097/00005373-198905000-00017. [DOI] [PubMed] [Google Scholar]
- 9.Belgian Outcome in Burn Injury Study Group. Development and validation of a model for prediction of mortality in patients with acute burn injury. Br J Surg. 2009;96(1):111–117. doi: 10.1002/bjs.6329. [DOI] [PubMed] [Google Scholar]
- 10.Vincent JL, Moreno R, Takala J. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med. 1996;22(7):707–710. doi: 10.1007/BF01709751. [DOI] [PubMed] [Google Scholar]
- 11.Knaus WA, Draper EA, Wagner DP. APACHE II: a severity of disease classification system. Crit Care Med. 1985;13(10):818–829. [PubMed] [Google Scholar]
- 12.Lorente JA, Vallejo A, Galeiras R. Organ dysfunction as estimated by the sequential organ failure assessment score is related to outcome in critically ill burn patients. Shock. 2009;31(2):125–131. doi: 10.1097/SHK.0b013e31817fc3ef. [DOI] [PubMed] [Google Scholar]
- 13.Douglas HE, Ratcliffe A, Sandhu R. Comparison of mortality prediction models in burns ICU patients in Pinderfields Hospital over 3 years. Burns. 2015;41(1):49–52. doi: 10.1016/j.burns.2014.05.009. [DOI] [PubMed] [Google Scholar]
- 14.Davis JS, Prescott AT, Varas RP. A new algorithm to allow early prediction of mortality in elderly burn patients. Burns. 2012;38(8):1114–1118. doi: 10.1016/j.burns.2012.08.018. [DOI] [PubMed] [Google Scholar]
- 15.Chipp E, Warner RM, McGill DJ. Air ambulance transfer of adult patients to a UK regional burns centre: who needs to fly? Burns. 2010;36(8):1201–1207. doi: 10.1016/j.burns.2010.05.023. [DOI] [PubMed] [Google Scholar]
- 16.UK ambulance service clinical practice guidelines. http://www2.warwick.ac.uk/fac/med/research/hsri/emergencycare/prehospitalcare/jrcalcstakeholderwebsite/guidelines/ [accessed May 2015]; [Google Scholar]
- 17.http://www.ukhems.co.uk/Burns.pdf. [accessed May 2014];UK Hems Standard Operating Procedure for burns. Online information. [Google Scholar]
- 18.Brugger H, Putzer G, Paal P. Accidental Hypothermia. Anaesthesist. 2013;62(8):624–631. doi: 10.1007/s00101-013-2205-7. [DOI] [PubMed] [Google Scholar]
- 19.Kjellman B-M, Fredrikson M, Glad-Mattsson G. Comparing ambient, air-convection, and fluid convection heating techniques in treating hypothermic burn patients, a clinical RCT. Annals of Surgical Innovation and Research. 2011;5:4–4. doi: 10.1186/1750-1164-5-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hostler D, Weaver MD, Ziembicki JA. Admission temperature and survival in patients admitted to burn centers. J Burn Care Res. 2013;34(5):498–506. doi: 10.1097/BCR.0b013e3182a231fb. [DOI] [PubMed] [Google Scholar]





