Summary
Infections are a common cause of morbidity and mortality in burn patients, and almost 50% of infection-related deaths in burn patients are caused by pneumonia. The proportion of facial and/or neck burns (FNB) in burn centre admissions is high, and these patients have a well known respiratory risk. However, it is not well established in the literature if the occurrence of a FNB is a risk factor for respiratory infection during hospitalization. A retrospective, single-centre trial at the burn unit of the Prelada Hospital was conducted, including patients admitted between January 2011 and December 2014. The primary objective was to investigate the existence of a relation between face and/or neck burns and occurrence of respiratory infection. A total of 229 patients were included in the study, 126 with FNB and 103 without FNB. Higher total body surface area (TBSA) burned, inhalation injury and early endotracheal intubation were statistically more frequent in the FNB group. These variables were also more prevalent in the group that developed respiratory infection during the burn unit stay. Concerning FNB patients, the most frequent microbiological strains isolated in respiratory secretion cultures were Staphylococcus aureus, Pseudomonas aeruginosa and Streptococcus pneumonia, while in nFNB patients it was Klebsiella pneumoniae. In our population, only early ETI, inhalation injury and higher TBSA appear to be independent risk factors for respiratory infection in FNB patients, although age, male sex and co-morbidities are also known risk factors for respiratory infection in burn patients.
Keywords: burns, face and neck burns, respiratory infection, inhalation injury, endotracheal intubation
Abstract
Les infections sont une cause habituelle de morbidité et de mortalité chez les brûlés. Près de 50% des décès survenant dans un tableau infectieux sont dus à une pneumopathie. La proportion de brûlures cervico-faciales (BCF) parmi les patients hospitalisés en CTB est élevée et ces patients ont un risque connu de complication respiratoire. Cependant, il n’est pas bien établi si une BCF est un facteur favorisant une infection respiratoire nosocomiale. Une étude rétrospective a été conduite dans le centre de brûlés de l’hôpital de Prelada, incluant 229 patients admis entre janvier 2011 et décembre 2014, parmi lesquels 126 avaint une BCF quand 103 n’en souffraient pas. La surface brûlée était plus importante, des lésions d’inhalation et une intubation endotrachéale précoce étaient plus fréquentes dans le groupe BCF. Ces mêmes facteurs étaient plus fréquents dans le groupe qui développait des infections respiratoires nosocomiales (IRN). Dans le groupe BCF, les germes les plus fréquemment en cause étaient Staphylococcus aureus, Pseudomonas æruginosa et Streptococcus pneumoniæ, tandis que chez les brûlés ne présentant pas de BCF, c’est Klebsiella pneumoniae qui était la plus fréquente. Dans notre série, l’intubation trachéale précoce, les lésions d’inhalation et l’étendue importante de la brûlure apparaissent être des facteurs indépendants de risque d’IRN dans les BCF, bien que l’âge, le sexe male et les co morbidités soient également connus comme facteurs favorisants de ces mêmes infections respiratoires chez les brûlés.
Introduction
Infections are a common cause of morbidity and mortality burn patients,1,2 and almost 50% of infection-related deaths in burn patients are caused by pneumonia.3
The proportion of facial and/or neck burns (FNB) in burn centre admissions is about 47%, which reflects the gravity of this type of lesion.4,5 Indeed, FNB patients have a double respiratory risk resulting from potential upper airway edema and smoke inhalation injury.6 They often undergo emergency airway management in the pre-hospital setting,7 and pre-hospital intubation appears to be an independent risk factor for pneumonia. 8 Furthermore, the inhalation injury is itself a major predisposing factor to pneumonia, respiratory insufficiency and death in this population.5,9
The primary objective of this study was to investigate the existence of a relation between FNBs and the occurrence of respiratory infection, since very little literature has explored this particular subject. The secondary endpoints were to perform a multivariate analysis of risk factors for respiratory infection in FNB patients and to determine which microbial strains were most frequently isolated.
Materials and methods
Study design and patient selection
A retrospective, single-centre trial at the burn unit of the Prelada Hospital was conducted. Patients admitted to the burn unit between January 2011 and December 2014 were included; however, those who remained hospitalized less than 24 hours were excluded. The following data were retrieved from patient files: demographic data, co-morbidities, characteristics of injury scene, characteristics of first medical assistance, etiology and characteristics of the burn, airway management, results of laryngoscopy and bronchoscopy, occurrence of respiratory complications, microbiological culture results, length of hospitalization and mortality.
Statistics and data analysis
Data were analyzed using Microsoft Excel and IBM SPSS 22 software. Descriptive analysis was presented with absolute frequency (n) and percentage (%) or mean (?) ± standard deviation (s) and median (m). A value of p < 0,05 was considered statistically significant.
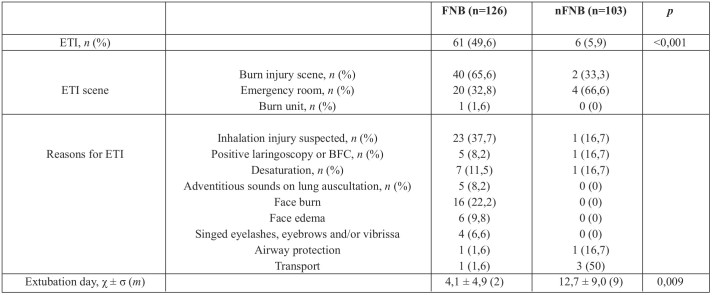
Table I. Demographic characteristics.
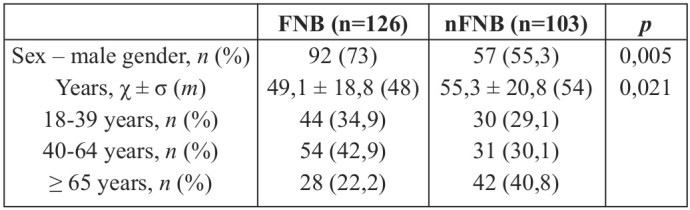
Table II. Medical history.
Results
Study population
During the 48-month study period, 233 patients were admitted to our burn unit. However, 4 patients who remained hospitalized less than 24 hours were excluded. A total of 229 patients were included in the study, 126 with FNB and 103 without FNB (nFNB).
In both groups, the majority of patients were male (n=92, 73% for FNB and n=57, 55.3% for nFNB group). The FNB group had a higher proportion of men than the nFNB group, which was statistically significant (p=0,005). However, this difference in sample composition did not affect the rate of respiratory infection (p=0,333). Mean patient age was 49,1 ± 18,8 years for the FNB group and 55,3 ± 20,8 years for the nFNB group (Table I). Although nFNB patients were significantly older (p=0,021), no correlation was detected between age and the occurrence of respiratory infection (p=0,163).
Medical history is summarized in Table II. The FNB and nFNB groups were meaningfully different only with respect to diabetes and hypertension (p<0,001 and p=0,006, respectively). This difference did not influence the rate of respiratory infection (p=0,962 and p=0,953, respectively). Although smoking habits were high in our study population (n=25, 49% for FNB; n=20, 37.7% for nFNB; p=0,246), this did not increase the incidence of respiratory infection during hospitalization (p=0,836).
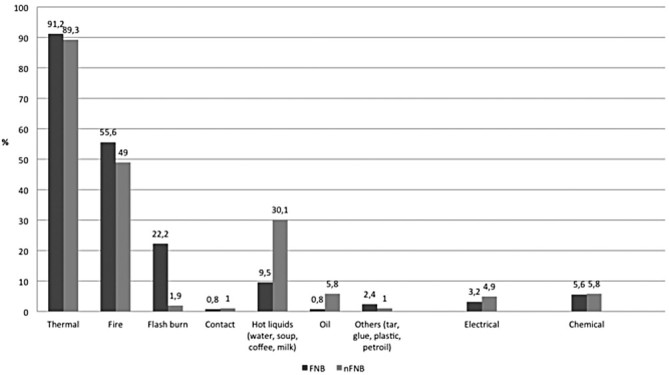
The majority of patients had thermal burns (n=155, 91.2% for FNB; n=92, 89.3% for nFNB) and just a minority had electrical (n=4, 3.2% for FNB; n=5, 4.9% for nFNB) or chemical burns (n=7, 5.6% for FNB; n=6, 5.8% for nFNB) (Fig. 1).
Fig. 1. Burn etiology.
None had important cervical or chest trauma.
Mean total body surface area (TBSA) burned was significantly higher in FNB patients (18,1 ± 16,4) compared to nFNB patients (11,4 ± 11,1), with a p value of <0,001. Fig. 2 shows that in the categories of major burns, FNB patients predominate. Higher TBSAs are also positively and significantly correlated with the occurrence of respiratory infection (p<0,001). The nFNB group had significantly more full-thickness burns than FNB patients, as shown in Table III.
Fig. 2. TBSA.
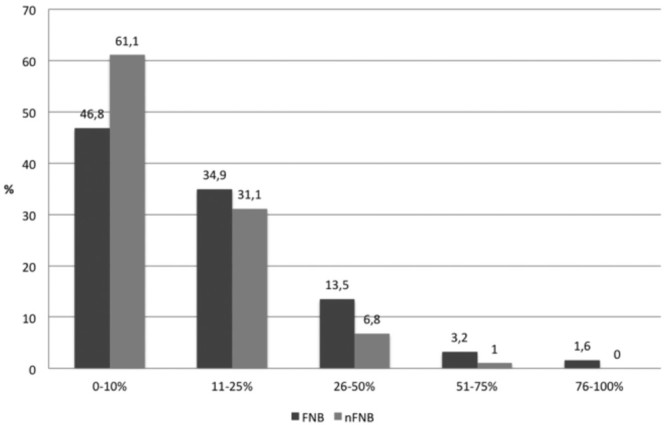
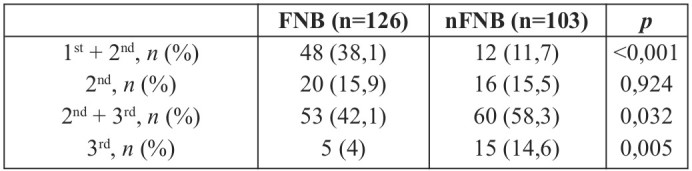
Table III. Burn depth.
Inhalation injury was more frequent in FNB than nFNB patients (n=17, 13.5% for FNB; n=3, 2.9% for nFNB, p=0,005). Likewise, inhalation injury was more prevalent among patients that developed respiratory infection than among the others (n=9, 27.3% for RI; n=7, 4.4% for nRI, p<0,001). The burn injury happened most frequently in a closed space in the FNB group (n=54, 58.7%) and in an open space in the nFNB group (n=44, 58.7%), which was not statistically different (p=0,997). The majority of FNB patients received primary medical assistance at the burn injury scene (n=63, 51.6%), while nFNB patients were primarily assisted mostly in the emergency room (n=73, 72.3%). Only a minority of patients were initially assisted in a primary health care centre (n=1, 0.8% for FNB; n=9, 8.9% for nFNB).
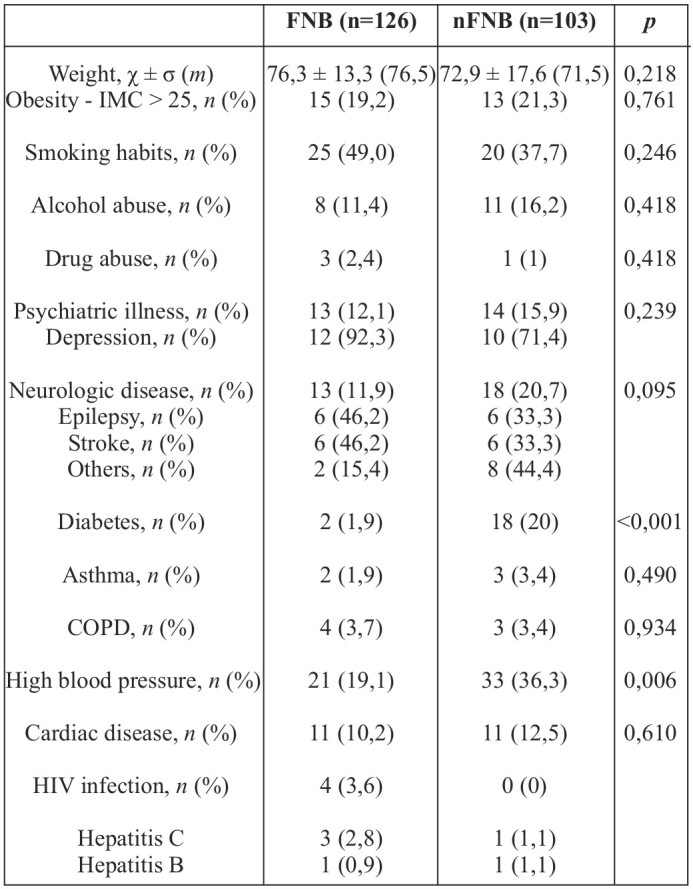
Endotracheal intubation (Table IV) was performed in 61 FNB patients (49.6%) and 6 nFNB patients (5.9%). The application of the Chi-Square test showed that this difference was statistically significant with a p-value of <0,001. Statistical analysis also revealed that intubated patients have a meaningfully increased rate of respiratory infection (p<0,001). The majority of FNB patients were intubated at the burn injury scene (n=40, 65.6%), while nFNB patients were mostly intubated in the emergency room (n=4, 66.6%), which is in accordance with the primary medical assistance scene. Only 1 patient was intubated in the burn unit at an early stage (less than 72 hours from admission). Otherwise, 3 patients were intubated in the setting of the burn unit at a late stage: 2 FNB patients (one at day 63 because of macro-aspiration, and the other at day 13 because of respiratory insufficiency type II) and 1 nFNB patient (at day 5 because of respiratory insufficiency type II). The reasons for intubation were miscellaneous. In FNB patients, the most common reasons were “suspected inhalation injury” (n=23, 37.7%) and “presence of face burn” (n=16, 22.2%). In nFNB patients, the most documented reason for intubation was “transport of the patient” (n=3, 50%). On the other hand, extubation was, on average, performed later in patients without face or neck burns (Table IV). Patients that developed respiratory tract infections, in turn, were extubated later than the others (7,3 ± 6,8 vs. 1,9 ± 1,8; p=0,015).
Table IV. Endotracheal intubation.
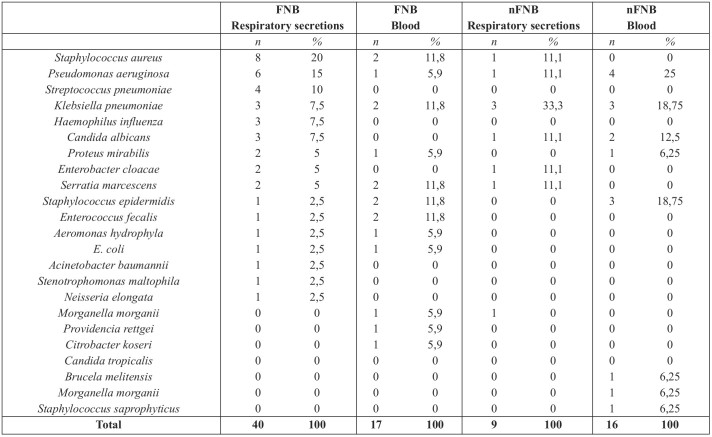
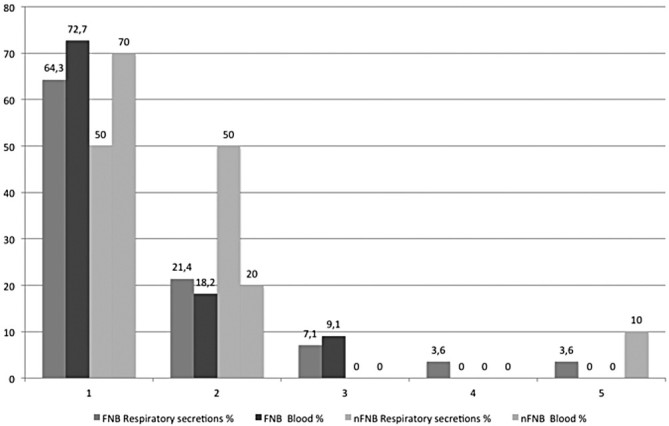
Microbiological isolates in respiratory secretions and blood cultures are summarized in Table V. Concerning FNB patients, the most frequent microbiological strains isolated in respiratory secretion cultures were Staphylococcus aureus (20%), followed by Pseudomonas aeruginosa (15%) and Streptococcus pneumoniae (10%). The most common strains isolated in blood cultures were Staphylococcus aureus, Klebsiella pneumoniae, Enterococcus fecalis, Serratia marcescens, Staphylococcus epidermidis (11.8% per strain). Concerning nFNB patients, the most frequent microbiological strain isolated in respiratory secretion cultures was Klebsiella pneumoniae (33.3%). The most common strains isolated in blood cultures were Klebsiella pneumoniae and Staphylococcus epidermidis (18.75% per strain).
Table V. Microbiological isolates.
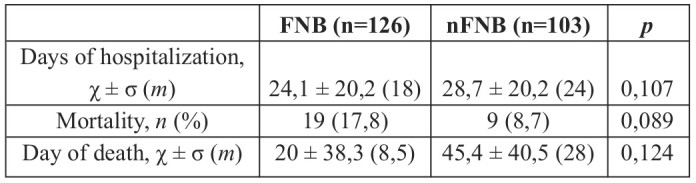
Considering patients with positive cultures, the number of microbial strains isolated in each patient ranged from 1 to 5, and the most common was the isolation of only one strain (Fig. 3). Duration of hospitalization was longer in the nFNB group (28,7 ± 20,2 vs. 24,1 ± 20,2, 0,107). Mortality rate was higher in the FNB group (n=19, 17.8% vs. n=9, 8.7%), but the difference was not statistically significant (p=0,089). Otherwise, mortality rate was higher in patients who developed respiratory infection (n=13, 52%) when compared to patients without respiratory infection (n=7, 5%) and the difference was statistically significant (p<0,001). The duration of hospitalization until death was higher in the nFNB group (45,4 ± 40,5 vs. 20 ± 38,3; p=0,124).
Fig. 3. Number of microbiological strains isolated.
Discussion
This work has shown the existence of a positive correlation between FNBs and the occurrence of respiratory infection. One of the major endpoints of this study was to determine risk factors for respiratory infection in FNB patients. Other studies demonstrate that older age, male sex, co-morbidities, higher TBSAs and inhalation injury increase the risk of pneumonia in burn patients.10
Our main results were that early ETI, presence of inhalation injury and higher TBSAs were the only independent risk factors for respiratory infection in this population.
Early ETI was more frequent in FNB patients and, in turn, it was also more frequent in patients that developed respiratory infection. These differences were both statistically significant. Interestingly, similar results have been reported in patients with early onset pneumonia (EOP), where pre-hospital intubation appears to be an independent risk factor for EOP in patients with severe face and neck burns.8 Early intubation in burn patients provides a portal for microbial contamination of the airway tract,11 which is probably the mechanism underlying the increased risk of respiratory infections that we observed in our population. On the other hand, patients with FNBs seem to be at higher risk of having a difficult intubation, estimated to be from 5% to 11%.6,12 Therefore early intubation before they enter the burn unit might be necessary.12,13 Our results should not discourage physicians from performing intubation in FNB patients, but rather encourage a serious analysis of risks and benefits when considering airway management in this population.
In our series, inhalation injury was more common in FNB patients and, in turn, it was also more common in patients that had respiratory infection. These differences were both statistically significant. Accordingly, previous literature also reports that burn patients with inhalation injury have higher rates of subsequent pneumonia14 and even that the incidence of pneumonia is higher when inhalation injury is more severe.15 Inhalation injury creates a damaged tracheobronchial mucosa, 16,17,18 which is probably the mechanism underlying the observed increased risk of respiratory tract infections.
Finally, our study determined that TBSA was also a risk factor for respiratory infection in FNB patients. Indeed, patients with FNB had higher TBSAs and, moreover, patients that developed respiratory infection also presented higher TBSAs. The differences were both statistically significant. In accordance with our results, Hoogewerf et al. showed that a more extensive burn increased the risk for facial burns,4 and Pham et al. reported that TBSA was an independent risk factor for pneumonia in burn patients over 55 years old.10
In our population, the majority of patients were male and the FNB group had a significantly higher proportion of men, but this difference did not affect the rate of respiratory infection. Previous studies have also found that being male augmented the risk for FNBs,4 and a possible explanation is that men, in our series, have a higher proportion of flash/flame work-related burns compared to women, and these injuries typically affect the face. Furthermore, the literature describes that not only male gender but also comorbidities were risk factors for pneumonia in burn patients over 55 years old.10 In fact, the only comorbidities that were significantly more prevalent in the FNB group were diabetes and hypertension, but again, it did not influence the occurrence of respiratory infection. Maybe this effect of gender and comorbidities was not detected in our study because our patients were younger. In accordance with the current literature, the risk of pneumonia is associated with preoperative and pre-hospitalization smoking.19,20 However, even taking into account that smoking habits were high in our study population, this did not increase the incidence of respiratory infection during burn unit stay.
Our work demonstrated that, although not statistically significant, mortality rate is higher in the FNB group. On the other hand, mortality rate is higher (with statistical significance) among patients that developed respiratory infection. These results are consistent with recent studies on ventilator-associated pneumonia (VAP), which demonstrate that VAP is a well recognized risk factor for mortality in general ICU patients.21 Furthermore, the literature suggests that VAP prolongs mechanical ventilation and stay in the ICU.22,23 However, in our results, FNB patients, with greater rates of intubation, have shorter hospitalizations. This bias might be related to the higher levels of early mortality in this group, which determines shorter burn unit stays.
Concerning FNB patients, the most frequent microbiological strains isolated in respiratory secretion cultures were Staphylococcus aureus, Pseudomonas aeruginosa and Streptococcus pneumonia (Table V). Similar results have been reported in the literature. The EU-VAP study has identified Staphylococcus aureus and Pseudomonas aeruginosa as the pathogens isolated most often in patients with VAP.24 Studies on severely burned face and neck patients with early onset pneumonia,8 on burn patients with early intubation and inhalation injury,11 and also on other ICU patients25 show a preponderance of Staphylococcus aureus, Streptococcus pneumonia and Haemophilus influenzae. Keen et al. have found a higher prevalence of gram negative organisms (including Pseudomonas aeruginosa) in the respiratory specimens of burn patients,26 which is also in accordance with our findings.
Table VI. Outcome.
Concerning nFNB patients, the most frequent microbiological strain isolated in respiratory secretion cultures was Klebsiella pneumoniae. Lipovy et al. also found Klebsiella pneumoniae to be the most prevalent isolate in VAP occurring later in the hospital stays of burn patients with inhalatory injury. 27 This finding might be in agreement with our results, considering that nFNB patients had longer hospitalizations and were extubated later.
The main limitation of this study is that it is a retrospective study. As a retrospective study, the temporal relationship is difficult to assess. Besides, we could not control exposure or outcome assessment but instead needed to rely on others for accurate recordkeeping, which can introduce bias on the data and analysis.
Conclusion
Early ETI, presence of inhalation injury and higher TBSAs appear to be independent risk factors for respiratory infection in FNB patients.
Inhalation injury and TBSA are independent variables. Therefore, intubation is the only risk factor that, being a dependent variable, can be controlled by health care providers. A burn on the face or neck is a warning sign of a possible inhalation injury, and early intubation before the patient enters the burn unit might be life-saving. However, unnecessary intubation may increase morbidity and mortality. Therefore, a serious analysis of risks and benefits of ETI in FNB patients is mandatory. A face/neck burn is only one sign, and intubation should only be performed in the presence of other suspicious clinical signs. Indeed, guidelines on early airway management in burn patients should be followed and, beyond that, updated.
Acknowledgments
Conflict of interest:The authors declare that they do not have any conflicts of interest.
The authors also certify that the procedures were performed in accordance with the international ethical standards on human experimentation and with the Helsinki Declaration of 1975, as revised in 2005, as well as with the national law.
References
- 1.Williams FN. The leading causes of death after burn injury in a single pediatric burn center. Crit Care. 2009;13:183–183. doi: 10.1186/cc8170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gomez R. Causes of mortality by autopsy findings of combat casualties and civilian patients admitted to a burn unit. J Am Coll Surg. 2009;208:348–354. doi: 10.1016/j.jamcollsurg.2008.11.012. [DOI] [PubMed] [Google Scholar]
- 3.D’Avignon LC. Contribution of bacterial and viral infections to attributable mortality in patients with severe burns: an autopsy series. Burns. 2010;36:773–779. doi: 10.1016/j.burns.2009.11.007. [DOI] [PubMed] [Google Scholar]
- 4.Hoogewerf CJ. Burns to the head and neck: epidemiology and predictors of surgery. Burns. 2013;39:1184–1192. doi: 10.1016/j.burns.2013.03.006. [DOI] [PubMed] [Google Scholar]
- 5.Santos DC. Pre-burn centre management of the airway in patients with face burns. Ann Burns Fire Disasters. 2015 [PMC free article] [PubMed] [Google Scholar]
- 6.Esnault p. Tracheal intubation difficulties in the setting of face and neck burns: myth or reality? Am J Emerg Med. 2014;32:1174–1178. doi: 10.1016/j.ajem.2014.07.014. [DOI] [PubMed] [Google Scholar]
- 7.Eastman AL, Arnoldo BA, Hunt JL, Purdue GF. Pre–Burn Center Management of the Burned Airway: Do We Know Enough? J Burn Care Res. 2010;31:701–705. doi: 10.1097/BCR.0b013e3181eebe4f. [DOI] [PubMed] [Google Scholar]
- 8.Cotte J. Early onset pneumonia in patients with severely burned face and neck: A 5-year retrospective study. Burns. 2013;39(5):892–896. doi: 10.1016/j.burns.2012.12.003. [DOI] [PubMed] [Google Scholar]
- 9.Lange M. A murine model of sepsis following smoke inhalation injury. Biochem Biophys Res Commun. 2010;391:1555–1560. doi: 10.1016/j.bbrc.2009.12.124. [DOI] [PubMed] [Google Scholar]
- 10.Pham TN. Risk factors for the development of pneumonia in older adults with burn injury. J Burn Care Res. 2010;31:105–110. doi: 10.1097/BCR.0b013e3181cb8c5a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mosier MJ. Microbial contamination in burn patients undergoing urgent intubation as part of their early airway management. J Burn Care Res. 2008;29:304–310. doi: 10.1097/BCR.0b013e318166daa5. [DOI] [PubMed] [Google Scholar]
- 12.Siah S. Difficult intubation problems in patients with face and neck burns. Ann Burns Fire Disasters. 2006;19:74–77. [PMC free article] [PubMed] [Google Scholar]
- 13.Cancio LC. Airway management and smoke inhalation injury in the burn patient. Clin Plast Surg. 2009;36:555–567. doi: 10.1016/j.cps.2009.05.013. [DOI] [PubMed] [Google Scholar]
- 14.Chen MC. The impact of inhalation injury in patients with small and moderate burns. Burns. 2014;40(8):1481–1486. doi: 10.1016/j.burns.2014.06.016. [DOI] [PubMed] [Google Scholar]
- 15.Albright JM. The acute pulmonary inflammatory response to the graded severity of smoke inhalation injury. Crit Care Med. 2012;40:1113–1121. doi: 10.1097/CCM.0b013e3182374a67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Prien T, Traber DL. Toxic smoke compounds and inhalation injury – a review. Burns Incl Therm Inj. 1988;14:451–460. doi: 10.1016/s0305-4179(88)80005-6. [DOI] [PubMed] [Google Scholar]
- 17.Nieman GF. The effect of smoke inhalation on pulmonary surfactant. Ann Surg. 1980;191:171–181. doi: 10.1097/00000658-198002000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Murakami K, Traber DL. Pathophysiological basis of smoke inhalation injury. News Physiol Sci. 2003;18:125–129. doi: 10.1152/nips.01427.2002. [DOI] [PubMed] [Google Scholar]
- 19.Rotstein C. Clinical practice guidelines for hospital-acquired pneumonia and ventilator-associated pneumonia in adults. Can J Infect Dis Med Microbiol. 2008;19(12):19–53. doi: 10.1155/2008/593289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Méndez E, Calderón R. Risk factors for nosocomial pneumonia in patients with abdominal surgery. Cir Cir. 2015 [Google Scholar]
- 21.Timsit JF. Attributable mortality of ventilator-associated pneumonia. Curr Opin Crit Care. 2011;17:464–471. doi: 10.1097/MCC.0b013e32834a5ae9. [DOI] [PubMed] [Google Scholar]
- 22.Rello J. Respiratory infections in patients undergoing mechanical ventilation. Lancet Respir Med. 2014;2(9):764–774. doi: 10.1016/S2213-2600(14)70171-7. [DOI] [PubMed] [Google Scholar]
- 23.Blot S et al.: Prevention of VAP: is zero rate possible? Clin Chest Med. 2011;32:591–599. doi: 10.1016/j.ccm.2011.05.008. [DOI] [PubMed] [Google Scholar]
- 24.Koulenti Spectrum of practice in the diagnosis of nosocomial pneumonia in patients requiring mechanical ventilation in European intensive care units. Crit Care Med. 2009;37:2360–2368. doi: 10.1097/CCM.0b013e3181a037ac. [DOI] [PubMed] [Google Scholar]
- 25.Anon: Guidelines for the management of adults with hospital acquired ventilator associated, and health care associated pneumonia. Am J Respir Crit Care Med. 2005;171:388–416. doi: 10.1164/rccm.200405-644ST. [DOI] [PubMed] [Google Scholar]
- 26.Keen EF. Prevalence of multidrugresistant organisms recovered at a military burn center. Burns,Burns, 2010;36:819–825. doi: 10.1016/j.burns.2009.10.013. [DOI] [PubMed] [Google Scholar]
- 27.Lipovy B. Epidemiology of ventilator associated tracheobronchitis and ventilator associated pneumonia in patients with inhalation injury at the Burn Centre in Brno (Czech Republic) Ann Burns Fire Disasters. 2011;24:120–125. [PMC free article] [PubMed] [Google Scholar]