Abstract
Honey allergy is a very rare, but serious health condition. In this study, we presented 1 patient who had anaphylaxis after the honey allergological investigation with skin prick-prick test with honey. Honey as a food has been associated to allergic reactions and as the increased consumption of honey in health food may increase the incidence of honey-related allergic reactions.
Keywords: Honey, Anaphylaxis, Prick-to-prick test
INTRODUCTION
Honey is widely consumed all over the world, especially in Portugal, but until now very few cases of honey allergy has been reported. Honey is known as a potential allergenic food and can cause reactions ranging from mild symptoms such as cough to severe as anaphylaxis.
Honey contains a large number of components derived from bees (gland secretions and wax), as well as from substances related to their foraging activity (flower nectar and pollens). Pollen proteins (Compositae pollen) and glandular proteins from bees have been referred as the main allergens involved in this type of allergy [1,2].
Allergy to honey is rare. Although the actual incidence of allergy to honey in the general population is unknown, it is estimated to be <0.001% [3]. There are few cases described in the literature [4,5,6,7].
CASE REPORT
We report a case of a 40-year-old female referred to our clinic with suspected allergy to honey. At the age of 36 she had 2 episodes of generalized urticaria 20 minutes after ingestion of foods with honey (honey cake and a banana with honey) and at the age of 37, five minutes after an inadvertent contact with a teaspoon with traces of honey, she got swollen lips and within 10 minutes urticaria, angioedema. The symptoms resolved after oral corticosteroids and antihistamines. The patient reported prior ingestion and application of royal jelly for cosmetic purposes with no complaints. Her physical examination and routine laboratory analyses were normal at admission.
She had not a relevant personal history of atopy and neither referred Hymenoptera sting hypersensitivity.
Skin prick tests (SPT) with a standard panel of extracts from aeroallergens and common allergenic foods (sunflower seeds, sesame, rye, barley, maize, wheat, oats, banana, egg, and milk) were negative. SPT and intradermic tests with bee venom extract were negative.
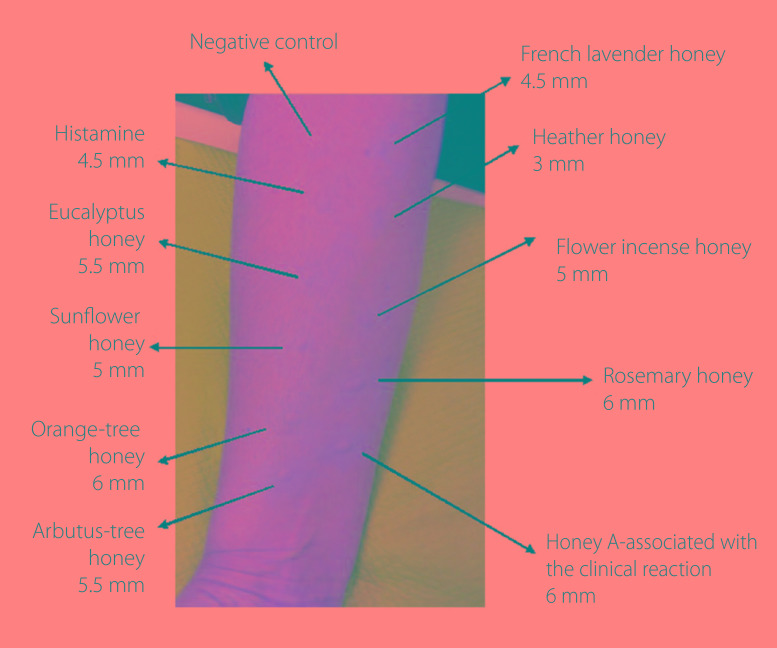
Prick-to-prick tests (PPT) were performed with several kinds of honey (one that she consumed with allergy reaction [honey A], and 8 other varieties which are frequently consumed in our country: Eucalyptus, Sunflower, Orange-tree, Arbutus-tree, French lavender, Heather, Flower incense, Rosemary) and the results were positive for all (Fig. 1).
Fig. 1. Prick-prick tests with different kinds of honey.
The same PPT with these 9 different kinds of honey were performed after informed consent in 6 volunteers controls with usual intake of honey without symptoms of honey allergy (3 healthy controls and 3 atopic with pollen sensitization and rhinitis) and none of them had a positive skin reaction.
Thirty minutes after carrying out the PPT, the patient suffered from anaphylaxis: generalized urticaria, swollen of lips-tongue-uvula, and hypotension. Adrenaline was administered with success and she was under surveillance for 24 hours.
PPT to royal jelly extract and to propolis (the resinous substance collected by honeybees from various plant sources) were negative. Serum total IgE-98 kU/L, specific IgE to honey-1.1 kUA/L (specific assay develop from rosemary honey extract).
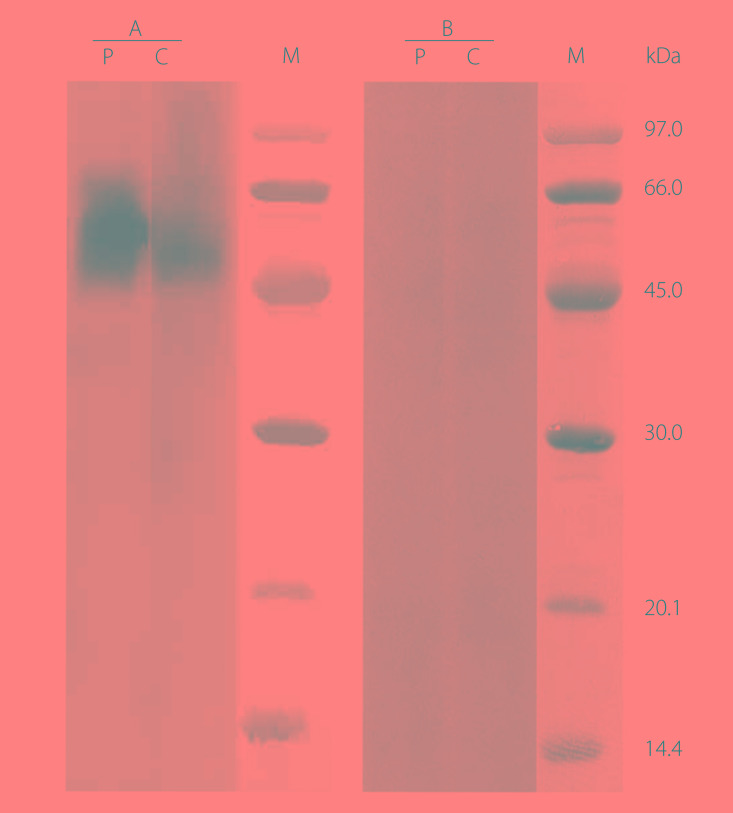
Sodium dodecyl sulfate-polyacrylamide gel electrophoresis immunoblotting assay with a honey extract obtained from a sample of honey A, revealed an IgE-binding band of 56 kDa, when the assay was carried out with bee venom extract, no IgE binding was observed (Fig. 2).
Fig. 2. Sodium dodecyl sulfate-polyacrylamide gel electrophoresis immunoblotting: (A) honey A extract, (B) bee venom extract. Lane P, patient serum; lane C, control serum (pool of sera from nonatopic subjects); lane M, molecular mass standard.
The patient was informed about honey allergy and the importance of honey avoidance. Adrenaline auto-injection kit 0.3 mg was prescribed and the patient was educated for its usage. Until now, she has been able to avoid honey and remain asymptomatic.
DISCUSSION
Anaphylaxis is a severe form of allergic disease, and when such a response occurs as a food allergy it is important to confirm the causative food component to prevent recurrence. Severe allergic reactions caused by honey are rare.
Sensitization to pollens and bee venoms was not observed in our patient. Bauer et al. [8] describe the presence of bee proteins in honey that behave like allergens in patients who ingested this honey. These proteins have a molecular weight similar to the one detected in our study (54–60 kDa). However, we did not detect any IgE-binding band in immunoblotting with bee venom extract, so this result does not support the assumption that the 56-kDa band identified in honey A (heather honey) would be a protein derived from bee venom. Could it be an unidentified allergen/protein from another allergenic source that is neither pollen nor bee venom? The PPT positive results obtained with all types of honey tested, point out some bee protein as the possible allergen.
Furthermore, to the best of our knowledge, this is the first adult case of anaphylaxis caused by PPT with honey.
Honey is a complex and heterogeneous mixture of flower nectars, sugars, proteins, and glandular secretions of bees (salivary and pharyngeal) [1]. The reported main allergens involved in the honey allergy are pollen proteins (Compositae plants: ragweed, sagebrush) and proteins (enzymes) from the salivary and pharyngeal glands secretions of the hymenoptera; less frequently sensitization to the other components of the bee's body, sensitization to fungal spores and sensitization to algae and other organic residues contained in honey have been described [8].
Discussion on the various sources of honey proteins and their allergenicity began in 1957. There are several theories on type I hypersensitivity to honey: due to cross reactivity among pollens of the Compositae family (e.g., sagebrush) or due to the presence of proteins from the bee venom [1].
Honey contains a small amount of wax (<0.05%). The beeswax alone does not have allergenic properties. Propolis—a substance used by bees during honeycomb building—is known as contact allergen.
Honey may be present in hidden forms in chocolate bars, candies, cakes, gingerbread, and cereals.
Honey allergy is still a rare condition, but increased consumption of honey in health food may increase the incidence of honey-related allergic reactions. Therefore, we suggest that warning information should be clearly labeled on every preparation containing honey, because our case suggests that honey is a causative allergen in food-induced anaphylaxis and symptoms of anaphylaxis seen in subjects following ingestion of honey can be true IgE-mediated hypersensitivity reactions.
References
- 1.Lombardi C, Senna GE, Gatti B, Feligioni M, Riva G, Bonadonna P, Dama AR, Canonica GW, Passalacqua G. Allergic reactions to honey and royal jelly and their relationship with sensitization to compositae. Allergol Immunopathol (Madr) 1998;26:288–290. [PubMed] [Google Scholar]
- 2.Fuiano N, Incorvaia C, Riario-Sforza GG, Casino G. Anaphylaxis to honey in pollinosis to mugwort: a case report. Eur Ann Allergy Clin Immunol. 2006;38:364–365. [PubMed] [Google Scholar]
- 3.Hofer T, Wüthrich B. Food allergy. II. Prevalence of organ manifestations of allergy-inducing food. A study on the basis of 173 cases, 1978-1982. Schweiz Med Wochenschr. 1985;115:1437–1442. [PubMed] [Google Scholar]
- 4.Karakaya G, Fuat Kalyoncu A. Honey allergy in adult allergy practice. Allergol Immunopathol (Madr) 1999;27:271–272. [PubMed] [Google Scholar]
- 5.Kalyoncu AF. Honey allergy and rhinitis in Ankara, Turkey. Allergy. 1997;52:876–877. doi: 10.1111/j.1398-9995.1997.tb02165.x. [DOI] [PubMed] [Google Scholar]
- 6.Cifuentes L. Allergy to honeybee … not only stings. Curr Opin Allergy Clin Immunol. 2015;15:364–368. doi: 10.1097/ACI.0000000000000191. [DOI] [PubMed] [Google Scholar]
- 7.Katayama M, Aoki M, Kawana S. Case of anaphylaxis caused by ingestion of royal jelly. J Dermatol. 2008;35:222–224. doi: 10.1111/j.1346-8138.2008.00448.x. [DOI] [PubMed] [Google Scholar]
- 8.Bauer L, Kohlich A, Hirschwehr R, Siemann U, Ebner H, Scheiner O, Kraft D, Ebner C. Food allergy to honey: pollen or bee products? Characterization of allergenic proteins in honey by means of immunoblotting. J Allergy Clin Immunol. 1996;97(1 Pt 1):65–73. doi: 10.1016/s0091-6749(96)70284-1. [DOI] [PubMed] [Google Scholar]