ABSTRACT
Active immunization is an important concern for health care workers (HCWs) susceptible subjects and potential sources of infection for patients. However, the vaccine coverage for vaccine preventable diseases (VPDs) is below recommended standards. The aims of the study were to estimate the hospitals' HCWs' susceptibility and vaccination coverage rates for VPDs and to analyze the role of HCWs' attitudes and knowledge as determinants of the immunization practices. A cross-sectional study enrolled 334 HCWs (physicians, nurses, others) at local hospital in L'Aquila (Italy). By means of an anonymous questionnaire, self-report data about history of disease and active vaccination for seasonal influenza, chickenpox, measles-mumps-rubella and hepatitis B were collected, as well as attitudes and knowledge about vaccination in HCWs. The employees showed high levels of susceptibility and insufficient vaccination coverage rates, particularly for influenza. Specific trends were detected for different VPDs across age strata and professional categories, not always consistent with literature. Overall, the level of knowledge about recommended vaccination for HCWs was low, in all categories. The active immunization status against influenza was found the most clearly associated with difference levels in 3 psychometric variables: personal responsibility, beliefs on usefulness and beliefs on risk of vaccination. A mediation mechanism was analyzed between these constructs, and an interesting indirect effect was highlighted for beliefs that could enhance the advantage of increased responsibility for HCWs. Further effort in research is needed to evaluate the black-box of longitudinal intervention studies (education, environmental changes, policies), to improve HCWs immunization.
KEYWORDS: attitudinal predictors, health care workers, immunization coverage, mediation analysis, vaccine preventable diseases
Introduction
Active immunization has a huge relevance in the fight against infectious diseases and it is an important concern for health care workers (HCWs). They are exposed to infections because of the close contact with patients and, at the same time, by protecting themselves against vaccine preventable diseases (VPDs), they avoid a further impairment of patients' health. From an economic and organizational point of view, HCWs vaccination would prevent the absenteeism, so ensure a better quality of care. Finally, HCWs are central figures in the promotion of healthy behaviors, and best immunization practice in people they take care.
However, despite the availability of effective vaccines and the recommendations from health institutions, the vaccine coverage is generally low in Italy, and in most European countries1,2 where vaccinations are not compulsory but recommended and payments not always refundable.3,4 Studies conducted in Italy to assess vaccination coverage of HCWs against the most common VPDs, have shown relatively high rates of coverage for hepatitis B5, but far below recommendations for measles, chickenpox, rubella, mumps and pertussis.5,6
Even for the vaccination against influenza, several Italian studies5,7-13 and foreign studies,14-24 show coverage rates below the minimum target of 75% required by the European Commission, with physicians more vaccination compliant than nurses.12,17,19,22-27
The reasons for not receiving influenza vaccination are: doubts about effectiveness,11,13,15,18,22-24,26,28,29 fear of side effects,15,19,20,22-24,28-31 perception of not being at risk,11,14,22,24,26,28,29 lack of time,4,21,24,28,29,31 forgetfulness13 and opinion that vaccine is not supported by adequate field trials.15 HCWs also believe that the influenza is a mild illness that does not require a specific prophylaxis7,11,13-15,19,23,26, that it is safer to contract the disease15 and, in addition, that vaccination may result in the risk of contracting diseases.14 Mandatory vaccination against influenza has been adopted by very few European countries3, and there is a wide debate about the efficacy and ethical issues of a compulsory policy.32 However, an internet survey on USA Health Care Personnel revealed that influenza vaccination coverage was highest among HCP who were required by their employer to be vaccinated.25
A negative role is also played by the lack of knowledge.20,31 The importance of information has been confirmed by studies conducted on students in medical disciplines. In a sample of Italian physicians during their specialization courses, only 11.9% were vaccinated against seasonal influenza while 49.3% declared the need for training about immunization practices.11,33 These results are consistent with a survey conducted on English students.16
The aims of the present study were to estimate the hospitals' HCWs' susceptibility and vaccination coverage rates for VPDs, and to analyze the role of HCWs' attitudes and knowledge as determinants of the immunization practices, with particular reference to vaccination against seasonal influenza.
Results
Out of 334 HCWs enrolled, 241 were female (72.2%) and 191 were aged 40–59 y (57.1%). The nurses were more represented (177, 53.0%) while either physicians and others reached about the 23% (Table 1).
Table 1.
Demographic characteristics and occupation of health care workers (N = 334).
| Characteristics | N (%) |
|---|---|
| Gender | |
| Female | 241 (72,2) |
| Male | 93 (27,8) |
| Age (in years) | |
| ≤ 29 | 31 (9,3) |
| 30–39 | 77 (23,1) |
| 40–49 | 83 (24,8) |
| 50–59 | 108 (32,3) |
| ≥60 | 35 (10,5) |
| Occupation | |
| Physician | 78 (23,3) |
| Nurse | 177 (53,0) |
| Other HCWs | 79 (23,7) |
The prevalence of “susceptible HCWs” was higher in the case of influenza (about or more than 80%) and there were not statistically significant differences between occupational or age categories. In the case of chickenpox and MMR, the prevalence never overshot the value of 40% for any occupational or age category without any statistically significant difference. The susceptibility to HBV was found to be the smallest one (in total less than 20%), but it shows a statistically significant increase with the age of HCWs: in the oldest subjects (60 y and over) it is more than double than in the middle age stratum and 5 times higher than in the youngest (respectively 38.2% vs 18.3% vs 7.5%) (Table 2).
Table 2.
Prevalence of susceptible HCWs (not-vaccinated AND/OR not-having had the disease).
| Susceptible to … |
Physician |
|
Nursing staff |
|
Other HCP |
|
Fisher's exact test |
|---|---|---|---|---|---|---|---|
| out of(1) | out of(1) | out of(1) | |||||
| Influenza | 84.0% | 75 | 79.1% | 172 | 85.9% | 71 | n.s. |
| Chickenpox | 39.4% | 71 | 31.2% | 170 | 35.4% | 65 | n.s. |
| MMR(2) | 26.1% | 69 | 28.8% | 170 | 27.5% | 69 | n.s. |
| HBV(3) | 16.9% | 77 | 15.4% | 175 | 20.0% | 75 | n.s. |
| Up to 39 ys | From 40 to 59 ys | 60 ys and more | |||||
| out of(1) | out of(1) | out of(1) | |||||
| Influenza | 85.7% | 105 | 79.3% | 179 | 82.4% | 34 | n.s. |
| Chickenpox | 28.7% | 101 | 37.4% | 174 | 32.3% | 31 | n.s. |
| MMR | 24.3% | 103 | 28.0% | 175 | 40.0% | 12 | n.s. |
| HBV | 7.5% | 107 | 18.3% | 186 | 38.2% | 34 | p < 0.001 |
Not-answering subjects have been excluded from the denominator.
Measles-Mumps-Rubella (not distinguished).
Hepatitis-B Virus.
Influenza immunization has a seasonal protection validity, so HCWs require annual vaccination every new season. Vaccines against MMR, chickenpox and HBV are routinely recommended for children in Italy, as in other countries. For this reason, in the case of influenza, more clearly than in other VPDs, to have vaccinated themselves during professional life could be considered a binary measure of an ‘active protecting’ behavior against an infection, so, against the risk of becoming a source of infectious disease for patients at the workplace. The proportion of HCWs actively protecting themselves against influenza (year of interest 2014–2015), is very low (overall, less than 20%) without statistically significant differences between occupational or age categories.
Table 3 and Fig. 1 show the values on psychometric variables assessing attitudes and knowledge of HCWs toward self and others' vaccination. Overall, the stratification highlights a statistically significant ‘worsening’ trend from physicians to nurses to other HCWs.
Table 3.
Likert scales scores for psychometric variables and knowledge stratified for different occupational categories (mean value and standard deviation) and statistical significance of differences and trend.
| Interval scale from −1 to +1 | Physicians(78) | Nursing staff (177) | Other HCP (79) | KW(1)test | Cuzick(2)test |
|---|---|---|---|---|---|
| Personal responsibility in HCWs' vaccination | 0.47 ± 0.46 | 0.40 ± 0.45 | 0.31 ± 0.47 | n.s. | p < 0.05 |
| Beliefs on preventive usefulness of vaccines | 0.57 ± 0.27 | 0.49 ± 0.34 | 0.34 ± 0.35 | p < 0.001 | p < 0.001 |
| Beliefs on vaccines-related risks | −0.40 ± 0.42 | −0.16 ± 0.43 | −0.06 ± 0.48 | p < 0.001 | p < 0.001 |
| Perceived susceptibility to infectious diseases | 0.77 ± 0.35 | 0.69 ± 0.38 | 0.49 ± 0.65 | p < 0.05 | p < 0.01 |
| Knowledge on recommended vaccines for HCWs | 0.20 ± 0.37 | 0.01 ± 0.35 | −0.10 ± 0.28 | p < 0.001 | p < 0.001 |
Kruskal - Wallis equality of populations rank test.
Cuzick nonparametric test for trend.
Figure 1.
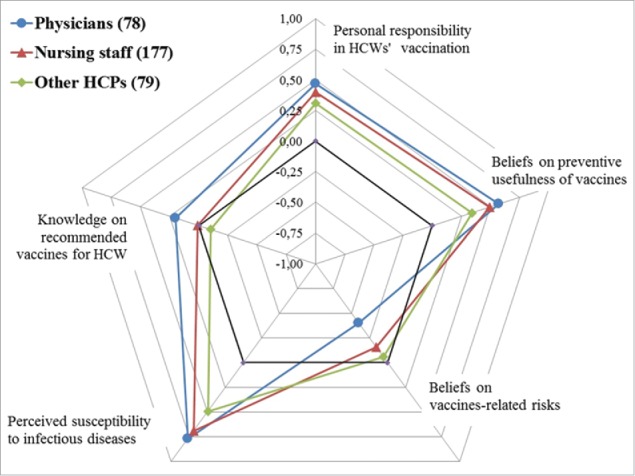
Likert scales mean scores for psychometric variables and knowledge stratified for different occupational categories.
The highest scores were obtained in ‘Perceived susceptibility’ to infectious diseases, particularly in the physicians (0.77 ± 0.35) and nurses (0.69 ± 0.38) vs other HCWs (0.49 ± 0.65; p < 0.05 at the Kruskal – Wallis' test and p < 0.01 at the Cuzick's test).
The ‘Beliefs on preventive usefulness of vaccine’ and ‘Beliefs on vaccine-related risks' were found clearly different between the 3 occupational categories, particularly the second one for which the differences between physicians and the other HCWs were higher (respectively −0.40 ± 0.42 vs −0.16 ± 0.43 in nurses and −0.06 ± 0.48 in other HCWs) and significantly decreasing (p < 0.001 both at Kruskall-Wallis' and Cuzick's tests).
The ‘Personal responsibility’ does not appear different between categories when compared to each other (Kruskall-Wallis' test n.s.), but the trend from physicians (0.47 ± 0.46) to nurses (0.40 ± 0.45) to other HCWs (0.31 ± 0.47) was statistically significant (p < 0.05 at Cuzick's test).
The lowest scores are attributable to the ‘Knowledge on recommended vaccines for HCWs’: the mean value for the physicians is 0.20 ± 0.37, it almost equals zero for the nurses (0.01 ± 0.35) and falls below zero for the others HCWs (−0.10 ± 0.28) with significant differences between categories (p < 0.001 at Kruskall-Wallis test) and worsening trend (p < 0.001 at Cuzick test).
Table 4 reports the differences between HCWs ‘actively protected’ and ‘not actively protected’ against influenza concerning the level of psychometric variables and knowledge: neither ‘Perceived susceptibility to infectious diseases' nor ‘Knowledge on recommended vaccines for HCWs’ were significantly different in any case; on the contrary, ‘Personal responsibility in HCWs’ vaccination’ was higher in ‘actively protected’ HCWs than in ‘not actively protected’; the ‘Beliefs on preventive usefulness of vaccines’ and ‘Beliefs on vaccines-related risks’ were found significantly and inversely different (p < 0.001 at Wilcoxon test)
Table 4.
Likert scales scores for psychometric variables and knowledge stratified for HCWs actively ‘protected’ status against influenza (mean value ± standard deviation and statistical significance of differences at non parametric Wilcoxon' rank-sum test).
| Against influenza |
|||
|---|---|---|---|
| Interval scale from −1 to +1 | Actively protected | Not actively protected | |
| Personal responsibility in HCWs' vaccination | 0.63 ± 0.37 | 0.35 ± 0.46 | *** |
| Beliefs on preventive usefulness of vaccines | 0.67 ± 0.67 | 0.42 ± 0.42 | *** |
| Beliefs on vaccines-related risks | −0.51 ± 0.40 | −0.13 ± 0.43 | *** |
| Perceived susceptibility to infectious diseases | 0.74 ± 0.33 | 0.67 ± 0.45 | n.s. |
| Knowledge on recommended vaccines for HCWs | 0.00 ± 0.30 | 0.04 ± 0.37 | n.s. |
Actively protected = HCWs vaccinated against influenza
Not actively protected = HCWs not-vaccinated against influenza
= p < 0.05;
= p < 0.01;
= p < 0.001.
Figure 2 focuses on the immunization against influenza and its potential determinants already tested as significantly different between ‘actively protected’ and ‘not actively protected’ subjects. A hypothetical mediation mechanism has been outlined and tested by means of ‘medeff’ function of STATA software. The mediation analysis revealed that there is a meaningful indirect effect on the relationship between Personal Responsibility and Active immunization against influenza attributable to the Beliefs on usefulness (0.142, C.I. 95% 0.049 – 0.251) and Beliefs on risks of vaccination (0.130, C.I. 95% 0.067–0.196). In other words, the influence of personal responsibility ‘passes’ in a large amount throughout the change in the positive (61.9% of total effect) and in the negative (63.6% of total effect) beliefs.
Figure 2.
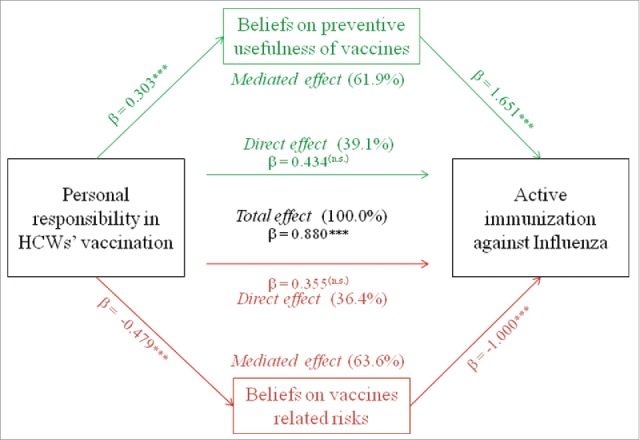
Relationship between personal responsibility and active immunization against influenza and hypothetical pathways mediated by beliefs on usefulness and risks of vaccinations. *** = p < 0.001.
Discussion
The HCWs enrolled in this study show, overall, significant levels of susceptibility and insufficient rates of vaccination for VPDs recommended by Italian Minister of Health.34
This study highlights a proportion of susceptible HCWs for chickenpox and MMR respectively of 34.0% and of 28.0% in the total sample, values comparable with those of Fortunato et al5 but higher than those of Taddei et al6 and Cologni et al35. The proportion of HCWs susceptible to hepatitis B is low but not negligible (16.8%), although lower than other national surveys.5
As frequently reported in literature, a high proportion of HCWs do not vaccinate for influenza14,15,17,19,21-24,36 and, as in other Italian and European surveys,5,7,10,18,37 a huge part of our sample (about 80%) were susceptible to seasonal influenza, despite national and international health recommendations that indicates a minimum vaccination coverage of 75%.38
The uptake of vaccine against influenza appears associated with the HCWs' age since the proportion vaccinated in the youngest HCWs is lower than that in the oldest as in other surveys10,21,22,26,30,39 maybe because of a lack of consolidated role or a non clear perception of their own vulnerability to infections. In fact, the history of vaccination against influenza (probably increasing with seniority) has been shown to be a significant predictor of ‘revaccination’26,36, as well as disease experience.40
Unlike other Italian surveys5 the proportion of subjects vaccinated against influenza among physicians is higher than in other HCWs.8,12,17,19,22-26
All attitudinal and cognitive variables considered in our study had previously been found to be associated with vaccination behaviors and intention in original research, reviews or meta analyses.
The Susceptibility perception to infectious diseases was found to be the variable with the highest score in our sample, but there are not significant differences in relation to vaccine utilization in HCWs, in contrast with the literature in which it was indicated among the most important reasons to protect oneself by vaccinating.26,31,37 This construct was indicated as a significant predictor of active immunization against seasonal and pandemic influenza31,41, as well as predictor of intention to use vaccine36,42 also against other VPDs.6
In all HCWs' categories, on average, the score of the variable Beliefs on vaccines-related risks was always found in the range of disagreement, revealing a general trusting attitude about the vaccine safety. In the specific case of influenza, we found statistically significant differences between HCWs actively protected and HCWs not-actively protected, confirming the importance of beliefs about the risks as a barrier to vaccination against these VPDs already shown by previous studies20,26,31,41 although not always as relevant.6,42 This observation confirms the importance of providing HCWs with additional education about vaccine safety, also because they are a source of information and recommendations for their patients.26 This study revealed that less than one half of HCWs (47.0%) reported that they recommend vaccination to their patients at least ‘sometimes’ (data not showed in results). This ‘proactive’ behavior is statistically less frequent in the youngest HCWs than in the middle-aged and older HCWs as also found in Italian pediatricians.43 Moreover, the physicians are more proactive than nursing staff and other HCWs, confirming the tendency reported by Torun et al.23
The score on Beliefs on preventive usefulness of vaccines was always in the range of agreement, demonstrating a positive confidence in preventing diseases. We detected a statistically significant difference between HCWs actively protected and HCWs not-actively protected confirming the findings that not believing in the effectiveness of vaccines could be a barrier.31 Moreover, this construct is negatively associated with the failure to vaccinate for influenza20,37 or to not to have intention to get vaccinated for influenza.36
Concerning Knowledge on recommended immunization for HCWs, we found, on average, an insufficient score and non statistically significant differences in relation to use of VPDs' vaccine. Nevertheless, in literature, this construct was indicated as an important reinforcing and enabling factor, to be considered in initiatives promoting vaccination.31,37,42
On average, the scores on Personal responsibility toward vaccination were located at intermediate level compared with other constructs. Only in this attitudinal variable there were not found any statistically significant differences between professional categories, however it shows the highest deviations between vaccinated vs not-vaccinated HCWs for influenza, as in a huge amount of studies, in which it was highly associated with vaccination behavior20,26,31,37 or with intention to get vaccinated.36,42
It is particularly relevant to deepen the predictor of responsibility and analyze the relationship with other constructs. This analysis focused on influenza since the vaccination against this VPD can best highlight the motivation of protecting patients, for whom the influenza can be a very serious illness even with lethal consequences, rather than protecting oneself, as for HCWs it is more likely a favorable disease course. We used the mediation analysis as previous authors did on the same predictor.42 Starting from observation that high feeling of personal responsibility was associated with having been vaccinated, we found a meaningful mediation effect attributable to beliefs on risk and usefulness of vaccines. In other words, the influence of personal responsibility ‘passes’, in a large amount, through the change in the HCWs beliefs. So, with the aim of increasing the immunization prevalence among the HCWs, besides addressing the feeling of responsibility, it should be necessary to improve the positive beliefs and reduce negative beliefs (i.e. a correct information of workers) to enhance the overall effect.
The study highlighted some differences between the various professionals: in particular all predictors appear lower in nurses and other professionals than in physicians. This trend has been also observed in other studies where the effect of knowledge and of the attitudes on immunization practice is more pronounced among nurses, suggesting the importance of education programs targeted and ‘profession-sensitive’.31 Moreover, it is a reason of concern in relation to a proactive behavior in recommending vaccination since nurses have close and more frequent contacts with patients compared with physicians.37
The results confirmed the high susceptibility to VPDs of HCWs, in particular toward influenza, as a serious concern in healthcare settings. The intervention studies to improve vaccine uptake by HCWs could be realized at different levels: individual (i.e., education), setting (i.e. refunding or offering vaccination on-site), and overall policies (i.e., mandatory/voluntary). In Italy, as in most European countries, the vaccinations for HCWs are recommended but not mandatory.3 So, to sustain voluntary policies, it is relevant to consider the determinant at individual level (i.e. attitudinal) and to study the mechanisms of influencing them as a contribution to Public Health, that is the aim of this study.
In literature concerning the attitudinal determinants of HCWs' vaccination, there is a lack of homogeneity with respect to the type, number, methods of assessment, analysis and, finally, to the possible theoretical models underlying the studies, as already noted.31 So, as a novel contribution, our findings focused on the interesting mediation effect attributable to beliefs about risks and usefulness of vaccination that could enhance the advantage of increased responsibility for HCWs. Those variables - significant mediators in our analyses - could be improved by means of education actions, that HICPAC and ACIP in the USA considered as the primary recommended place for influenza vaccination of Health-Care Personnel: “Educate HCP regarding the benefits of influenza vaccination and the potential health consequences of influenza illness for themselves and their patients […] in accordance with their level of responsibility in preventing health-care associated influenza.”29
The self-report method of data collection about immunization status of HCWs is a significant limitation in this study. This is different from recent European studies using the serology.44-46 Concerning epidemiological reliability of data, in some surveys, there has been found a low predictive value of self-reported data on history of disease or vaccination.47 Moreover, in the case of HBV, it is important to establish the real immune protection in the HCWs already vaccinated. The proportion of participants appear low, suggesting a possible response bias, but it is higher than in other surveys.36 We used the mediation analysis on cross-sectional data. As a future research perspective, that analysis could be appropriate in evaluating the black-box of longitudinal intervention studies, such as HCWs' education, environmental changes, policies on active vaccination offer, and on quality of patient safety.29
Material and methods
Design and data collection
A cross-sectional study was carried out in April-May 2015 at “San Salvatore” Hospital, with 363 inpatient-beds, located in L'Aquila (Abruzzo Region, Italy), and with 1,081 medical and paramedical employees. An anonymous self-report questionnaire, previously used in the European Hproimmune Project48, was proposed to HCWs. 371 employees voluntarily joined the study, but only 334 questionnaires were valid for the analysis (participation rate of 30.9% of total employees).
The questionnaire comprises the demographic information and 7 questions (in total, 33 items) about immunization status, opinions and knowledge concerning vaccination recommended for HCWs by the Italian Health Ministry. The questionnaire was accompanied by a letter from the Hospital Sanitary Director and an informed consent form detailing the aims of the study and the scope of data utilization. Each HCW signed the informed consent form before filling the questionnaire.
The study protocol has been submitted to the institutional review board for ethical issues approval.
Variables
Immunization status against influenza, chickenpox, measles-mumps-rubella (MMR-not distinguished) and hepatitis B (HBV) was assessed as binary variables and proportions were calculated as follows: “susceptible HCWs” have been defined as subjects not vaccinated against a specific VPD and/or not have had the same disease (numerator) among all respondents (denominator). Only in the case of influenza, because the annual variability of human viruses, the “susceptible HCWs” are equivalent of “not-vaccinated HCWs,” so we used the expression “actively protected HCWs” to define subjects vaccinated against influenza (numerator) among all HCWs interviewed, during the 2014–2015 epidemic season.
Variables on psychometric constructs were measured on 5-points Likert scale ranging from −1 (totally disagree) to + 1 (totally agree). By means of a preliminary factor analysis (not shown here for brevity), the items measuring the same underlying construct were averaged into a single quantitative scaling variable as shown in Table 5: Personal responsibility in HCWs' vaccination; Beliefs on preventive usefulness of vaccines; Beliefs on vaccines-related risks; Perceived susceptibility to infectious diseases. The level of knowledge about HCWs recommended immunization was measured by a single variable (quantitative scale ranging from −1 to +1) as average of 8 items concerning specific vaccinations.
Table 5.
Scaling and internal consistency of psychometric variables measuring the attitudinal predictors in HCWs.
| Psychometric constructs | Items | Range | Cronbach's alpha | |
|---|---|---|---|---|
| No. | Content | |||
| Personal responsibility in HCWs' vaccination | 2 | I believe that immunization among HCWs is an indispensable requirement to work in a health care settingI believe that immunization among HCWs is a duty because HCWs should represent a model for their patients | From −1 to +1 | 0.75 |
| Beliefs on preventive usefulness of vaccines | 4 | I believe vaccines are important for reducing or eliminating serious diseasesI believe that vaccines are useful in particular settings for example in the developing worldI believe in challenging natural immunity by contracting the disease rather than getting vaccinated [to reverse]I believe that vaccines aren't effective [to reverse] | From −1 to +1 | 0.68 |
| Beliefs on vaccines-related risks | 4 | I don't believe in vaccination, I believe that they do more harm than goodI'm afraid of the side effectsI'm afraid of getting sick after vaccinationI am suspicious of the long-term effects on the health from vaccination | From −1 to +1 | 0.84 |
| Perceived susceptibility to infectious diseases | 1 | I do not think I'm at risk of contracting any infectious disease | From −1 to +1 | — |
Statistical analysis
Software STATA IC/12.1 was used for statistical analysis. Significance of association between categorical variables was tested by means of Fisher exact test. To demonstrate HCWs' attitudinal differences toward vaccination, non parametric tests were used to compare quantitative variables between categories (Wilcoxon's and Kruskall-Wallis' test) and to evaluate the significance of their trend (Cuzick's test), in particular considering the immunization against influenza.
To test the mediation effect in the relationship between one psychometric variable and the binary variable measuring active immunization against influenza, the STATA function ‘medeff’ was used.49 An OLS regression model estimated the coefficients in the paths between continuous predictor and continuous mediators and a probit regression estimated the coefficients between continuous predictor or mediators and the binary outcome. The pathways are described as Average Causal Mediation Effect (ACME, or ‘indirect effect’), as Average Direct Effect (ADE, or ‘direct effect’) both expressed also as percentage of ‘Total effect’.
Abbreviations
- HCWs
Health Care Workers
- VPDs
Vaccine Preventable Diseases
- MMR
Measles-Mumps-Rubella
- HBV
Hepatitis B Virus
- OLS
Ordinary Least Squares
- ACME
Average Causal Mediation Effect
- ADE
Average Direct Effect
Disclosure of potential conflicts of interest
All the authors have no conflicts of interest to declare.
References
- [1].European Centre for Disease Prevention and Control Review of outbreaks and barriers to MMR vaccination coverage among hard-to-reach populations in Europe. Stockholm: ECDC; 2013. http://ecdc.europa.eu/en/publications/Publications/MMR-vaccination-hard-to-reach-population-review-2013.pdf [accessed on 16.February.2016] [Google Scholar]
- [2].European Centre for Disease Prevention and Control Implementation of the Council Recommendation on seasonal influenza vaccination (2009/1019/EU). Stockholm: ECDC; 2014. http://ecdc.europa.eu/en/publications/Publications/Implementation-seasonal-Influenza-vaccination-Council-Recommendation-Jan-2014.pdf [accessed on 16.February.2016] [Google Scholar]
- [3].Maltezou HC, Poland GA. Vaccination policies for healthcare workers in Europe. Vaccine 2014; 32:4876-80; PMID:24161573; http://dx.doi.org/ 10.1016/j.vaccine.2013.10.046 [DOI] [PubMed] [Google Scholar]
- [4].Music T. Protecting patients, protecting healthcare workers: a review of the role of influenza vaccination. Int Nurs Rev 2012; 59(2):161-7; PMID:22591085; http://dx.doi.org/ 10.1111/j.1466-7657.2011.00961.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Fortunato F, Tafuri S, Cozza V, Martinelli D, Prato R. Low vaccination coverage among italian healthcare workers in 2013. Hum Vaccin Immunother 2014; 19:e34415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Taddei C, Ceccherini V, Niccolai G, Porchia BR, Boccalini S, Levi M, Tiscione E, Santini MG, Baretti S, Bonanni P, et al.. Attitude toward immunization and risk perception of measles, rubella, mumps, varicella, and pertussis in health care workers working in 6 hospitals of Florence, Italy 2011. Hum Vaccin Immunother 2014; 10(9):2612-22; PMID:25483489; http://dx.doi.org/ 10.4161/21645515.2014.970879 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Albano L, Mattuozzo A, Marinelli P, Di Giuseppe G. Knowledge, attitudes and behaviour of hospital health-care workers regarding influenza A/H1N1: a cross sectional survey. BMC Infect Dis 2014; 14:208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Alicino C, Iudici R, Barberis I, Paganino C, Cacciani R, Zacconi M, et al.. Influenza vaccination among healthcare workers in Italy. Hum Vaccin Immunoter 2015; 11(1):95-100; http://dx.doi.org/ 10.4161/hv.34362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Amodio E, Restivo V, Firenze A, Mammina C, Tramuto F, Vitale F. Can influenza vaccination coverage among healthcare workers influence the risk of nosocomial influenza-like illness in hospitalized patients? J Hosp Infect 2014; 86:182-7; PMID:24581755; http://dx.doi.org/ 10.1016/j.jhin.2014.01.005 [DOI] [PubMed] [Google Scholar]
- [10].Barbadoro P, Marigliano A, Di Tondo E, Chiatti C, Di Stanislao F, D'Errico MM, Prospero E. Determinants of influenza vaccination uptake among Italian healthcare workers. Hum Vaccin Immunother 2013; 9(4):911-6; PMID:24064543; http://dx.doi.org/ 10.4161/hv.22997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Costantino C, Mazzucco W, Azzolini E, Baldini C, Bergomi M, Biafiore AD, Bianco M, Borsari L, Cacciari P, Cadeddu C, et al.. Influenza vaccination coverage among medical residents. An Italian multicenter survey. Hum Vaccin Immunther 2014; 10(5):1204-10; http://dx.doi.org/ 10.4161/hv.28081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Giannattanasio A, Mariano M, Romano R, Chiatto F, Liguoro I, Borgia G, Guarino A, Lo Vecchio A. Sustained low influenza vaccination in health care workers after H1N1 pandemic: a cross sectional study in an Italian health care setting for at-risk patients. BMC Infect Dis 2015; 15:329; PMID:26265328; http://dx.doi.org/ 10.1186/s12879-015-1090-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].La Torre G, Mannocci A, Ursillo P, Bontempi C, Firenze A, Panico MG, Sferrazza A, Ronga C, D'Anna A, Amodio E, et al.. Prevalence of influenza vaccination among nurses and ancillary workers in Italy. Hum Vaccin 2011; 7(7):728-33; PMID:21705859; http://dx.doi.org/ 10.4161/hv.7.7.15413 [DOI] [PubMed] [Google Scholar]
- [14].Alshammari TM, AlFehaid LS, AlFraih JK, Aljadhey HS. Health care professionals' awareness of, knowledge about and attitude to influenza vaccination. Vaccine 2014; 32:5957-61; PMID:25218193; http://dx.doi.org/ 10.1016/j.vaccine.2014.08.061 [DOI] [PubMed] [Google Scholar]
- [15].Arda B, Durusoy R, Yamazhan T, Sipahi OR, Tasbakan M, Pullukcu H, Erdem E, Ulusoy S. Did the pandemic have an impact on influenza vaccination attitude? A survey among health care workers. BMC Infect Dis 2011; 11:87; PMID:21473763; http://dx.doi.org/ 10.1186/1471-2334-11-87 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Blank DL, Bodansky DMS, Forbes A, Garde E, Story F, Roalfe AK, Tait L. Influenza vaccination of future healthcare workers: a cross-sectional study of uptake, knowledge and attitudes. Vaccine 2010; 28:4668-72; PMID:20451640; http://dx.doi.org/ 10.1016/j.vaccine.2010.04.066 [DOI] [PubMed] [Google Scholar]
- [17].Civljak R, Papic N, Stamenic V, Kalenic S, Kuzman I, Car J. Influenza and hepatitis B vaccination coverage among healthcare workers in Croatian hospitals: a series of cross-sectional surveys, 2006–2011. BMC Infect Dis 2013; 13:520; PMID:24192278; http://dx.doi.org/ 10.1186/1471-2334-13-520 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Lehmann BA, Ruiter RA, Wicker S, van Dam D, Kok G. “I don't see an added value for myself:” a qualitative study exploring the social cognitive variables associated with influenza vaccination of Belgian, Dutch and German healthcare personnel. BMC Public Health 2014; 14:407; PMID:24775096; http://dx.doi.org/ 10.1186/1471-2458-14-407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Lewthwaite P, Campion K, Blackburn B, Kemp E, Major D, Sarangi K. Healthcare workers' attitude towards influenza vaccination after the 2009 pandemic. Occup Med (Lond) 2014; 64(5):348-51; PMID:24717444; http://dx.doi.org/ 10.1093/occmed/kqu048 [DOI] [PubMed] [Google Scholar]
- [20].Little KE, Goodridge S, Lewis H, Lingard SW, Din S, Tidley M, Roberts RJ, Williams NS, Hayes S. Occupational vaccination of health care workers: uptake, attitudes and potential solutions. Public Health 2015; 129:755-62; PMID:25834928; http://dx.doi.org/ 10.1016/j.puhe.2015.02.031 [DOI] [PubMed] [Google Scholar]
- [21].Takayanagi IJ, Cardoso MR, Costa SF, Araya ME, Machado CM. Attitudes of health care workers to influenza vaccination: why are they not vaccinated? Am J Infect Control 2007; 35(1):56-61; PMID:17276792; http://dx.doi.org/ 10.1016/j.ajic.2006.06.002 [DOI] [PubMed] [Google Scholar]
- [22].Tanguy M, Boyeau C, Pean S, Marijon E, Delhumeau A, Fanello S. Acceptance of seasonal and pandemic a (H1N1) 2009 influenza vaccination by healthcare workers in a French Teaching Hospital. Vaccine 2011; 29(25):4190-94; PMID:21497636; http://dx.doi.org/ 10.1016/j.vaccine.2011.03.107 [DOI] [PubMed] [Google Scholar]
- [23].Torun SD, Torun F. Vaccination against pandemic influenza A/H1N1 among healthcare workers and reasons for refusing vaccination in Istanbul in last pandemic alert phase. Vaccine 2010; 28(35):5703-10; PMID:20600497; http://dx.doi.org/ 10.1016/j.vaccine.2010.06.049 [DOI] [PubMed] [Google Scholar]
- [24].Vírseda S, Restrepo MA, Arranz E, Magán-Tapia MP, Fernández-Ruiz M, de la Cámara AG, Aguado JM, López-Medrano F. Seasonal and Pandemic A (H1N1) 2009 influenza vaccination coverage and attitudes among health-care workers in a Spanish University Hospital. Vaccine 2010; 28(30):4751-7; http://dx.doi.org/ 10.1016/j.vaccine.2010.04.101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Black CL, Yue X, Ball SW, Donahue SM, Izrael D, de Perio MA, Laney AS, Williams WW, Lindley MC, Graitcer SB. Influenza Vaccination Coverage Among Health Care Personnel–United States, 2014–15 Influenza Season. MMWR Morb Mortal Wkly Rep 2015; 64(36):993-9; PMID:26389743; http://dx.doi.org/ 10.15585/mmwr.mm6436a1 [DOI] [PubMed] [Google Scholar]
- [26].Naleway AL, Henkle EM, Ball S, Bozeman S, Gaglani MJ, Kennedy ED, Thompson MG. Barriers and facilitators to influenza vaccination and vaccine coverage in a cohort of health care personnel. Am J Infect Control 2014; 42(4):371-5; PMID:24679562; http://dx.doi.org/ 10.1016/j.ajic.2013.11.003 [DOI] [PubMed] [Google Scholar]
- [27].Wicker S, Rose MA. Health care workers and pertussis: an underestimated issue. Med Klin (Munich). 2010; 105(12):882-6; PMID:21240587 [DOI] [PubMed] [Google Scholar]
- [28].Bali NK, Asharaf M, Ahamad F, Khan UH, Widdowson MA, Lal RB, Koul PA. Knowledge, attitude, and practices about the seasonal influenza vaccination among healthcare workers in Srinagar, India. Influenza Other Respir Viruses 2013; 7(4):540-5; PMID:22862774; http://dx.doi.org/ 10.1111/j.1750-2659.2012.00416.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Pearson ML, Bridges CB, Harper SA. Healthcare Infection Control Practices Advisory Committee (HICPAC); Advisory Committee on Immunization Practices (ACIP). Influenza vaccination of health-care personnel: recommendations of the Healthcare Infection Control Practices Advisory Committee (HICPAC) and the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep 2006; 55(RR-2):1-16; PMID:16498385 [PubMed] [Google Scholar]
- [30].Corace K, Prematunge C, McCarthy A, Nair RC, Roth V, Hayes T, Suh KN, Balfour L, Garber G. Predicting influenza vaccination uptake among health care workers: what are the key motivators? Am J Infect Control 2013; 41(8):679-84; PMID:23523520; http://dx.doi.org/ 10.1016/j.ajic.2013.01.014 [DOI] [PubMed] [Google Scholar]
- [31].Hollmeyer HG, Hayden F, Poland G, Buchholz U. Influenza vaccination of health care workers in hospitals-a review of studies on attitudes and predictors. Vaccine 2009; 27(30):3935-44; PMID:19467744; http://dx.doi.org/ 10.1016/j.vaccine.2009.03.056 [DOI] [PubMed] [Google Scholar]
- [32].Galanakis E, Jansen A, Lopalco PL, Giesecke J. Ethics of mandatory vaccination for healthcare workers. Euro Surveill 2013; 18(45):20627; PMID:24229791; http://dx.doi.org/ 10.2807/1560-7917.ES2013.18.45.20627 [DOI] [PubMed] [Google Scholar]
- [33].Amodio E, Tramuto F, Maringhini G, Asciutto R, Firenze A, Vitale F, Costantino C, Calamusa G. Are medical residents a “core group” for future improvment to influenza vaccination coverage in health-care workers? A study among medical residents at the University Hospital of Palermo (Sicily). Vaccine 2011; 29:8113-17; PMID:21856362; http://dx.doi.org/ 10.1016/j.vaccine.2011.08.033 [DOI] [PubMed] [Google Scholar]
- [34].Italian Minister of Health. Recommendations for Health Care Workers' Vaccination. Available at : http://www.salute.gov.it/portale/temi/p2_6.jsp?lingua=italiano&id=645&area=Malattie%20infettive&menu=vaccinazioni (accessed on February 16, 2016) [Google Scholar]
- [35].Cologni L, Belotti L, Bacis M, Moioli F, Goglio A, Mosconi G. measles, mups, rubella and varicella: antibody titration and vaccinations in a large hospital. G Ital Med Lav Ergon 2012; 34(3):272-4; PMID:23405639 [PubMed] [Google Scholar]
- [36].Lehmann BA, Ruiter RAC, van Dam D, Wicker S, Kok G. Sociocognitive predictors of the intention of healthcare workers to receive the influenza vaccine in Belgian, Dutch and German hospital settings. J Hosp Infect 2015; 89(3):202-9; PMID:25586987; http://dx.doi.org/ 10.1016/j.jhin.2014.11.009 [DOI] [PubMed] [Google Scholar]
- [37].Cozza V, Alfonsi V, Rota MC, Paolini V, Ciofi degli Atti ML. Promotion of influenza vaccination among health care workers: findings from a tertiary care children's hospital in Italy. BMC Public Health 2015; 15:697; PMID:26204896; http://dx.doi.org/ 10.1186/s12889-015-2067-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Italian Ministry of Health Prevention and control of influenza: recommendations for the 2015–2016 season. http://www.trovanorme.salute.gov.it/norme/renderNormsanPdf?anno=0&codLeg=52703&parte=1%20&serie= (accessed on February 16, 2016) [Google Scholar]
- [39].Bonfiglioli R, Vignoli M, Guglielmi D, Depolo M, Violante FS. Getting vaccinated or not getting vaccinated? Different reason for getting vaccinated aginst seasonal or pandemic influenza. BMC Public Health 2013; 13:1221; PMID:24359091; http://dx.doi.org/ 10.1186/1471-2458-13-1221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Awali RA, Samuel PS, Marwaha B, Ahmad N, Gupta P, Kumar V, Ellsworth J, Flanagan E, Upfal M, Russell J, et al.. Understanding health care personnel's attitudes toward mandatory influenza vaccination. Am J Infect Control 2014; 42(6):649-52; PMID:24837116; http://dx.doi.org/ 10.1016/j.ajic.2014.02.025 [DOI] [PubMed] [Google Scholar]
- [41].Prematunge C, Corace K, McCarthy A, Nair RC, Roth V, Suh KN, Garber G. Qualitative motivators and barriers to pandemic vs. seasonal influenza vaccination among healthcare workers: A content analysis. Vaccine 2014; 32(52):7128-34; PMID:25454876; http://dx.doi.org/ 10.1016/j.vaccine.2014.10.023 [DOI] [PubMed] [Google Scholar]
- [42].Lehmann BA, Ruiter RA, Chapman G, Kok G. The intention to get vaccinated against influenza and actual vaccination uptake of Dutch healthcare personnel. Vaccine 2014; 32(51):6986-91; PMID:25454867; http://dx.doi.org/ 10.1016/j.vaccine.2014.10.034 [DOI] [PubMed] [Google Scholar]
- [43].Ciofi degli Atti M, Rizzo C, del Manso C, Azzari C, Bartolazzi G, Esposito S, et al.. I pediatri e i determinanti della vaccinazione anti-influenzale: un'indagine di conoscenza, attitudine e pratica. Rivista di Immunologia e Allergologia pediatrica 2011; 6:36-43. http://www.riaponline.it/wp-content/uploads/2015/03/RivRiap6_11.pdf (accessed on February 17, 2016) [Google Scholar]
- [44].Sernia S, Ortis M, Antoniozzi T, Maffongelli E, La Torre G. Levels of antibody in HBV-vaccinated students enrolled in the faculty of Medicine, dentistry and health Professions of large Italian University. Biomed Res Int 2015; 2015:712020; PMID:25629052; http://dx.doi.org/ 10.1155/2015/712020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Borràs E, Campins M, Esteve M, Urbiztondo L, Broner S, Bayas JM, Costa J, Domínguez A.. Are healthcare workers immune to rubella? Hum Vaccin Immunther 2014; 10(3):686-91; http://dx.doi.org/ 10.4161/hv.27498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Basu S, Giri P, Adisesh A, McNaught R. healthcare workers and measles-mumps-rubella (MMR) status: how worried should we be about further outbreaks? Epidemiol Infect 2014; 142(8):1688-94; PMID:24229805; http://dx.doi.org/ 10.1017/S0950268813002859 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47].Alp E, Cevahir F, Gökahmetoglu S, Demiraslan H, Doganay M. Prevaccination screening of health-care workers for immunity to measles, rubella, mups, and varicella in a developing country: What do we save? J Infect Public Health 2012; 5(2):127-32; PMID:22541258; http://dx.doi.org/ 10.1016/j.jiph.2011.11.003 [DOI] [PubMed] [Google Scholar]
- [48].Istituto Superiore di Sanita (ISS):Progetto HPROImmune, Questionario rivolto agli operatori sanitari http://www.epicentro.iss.it/temi/vaccinazioni/pdf/20-6-2014/questionaio_pre.pdf [accessed on 15.February2016] [Google Scholar]
- [49].Hicks R, Tingley D. Causal mediation analysis. STATA J 2011; 11(4):605-19. [Google Scholar]


