ABSTRACT
In the United States, influenza and pneumonia account significantly to emergency room use and hospitalization of adults >65 y. The Centers for Disease Control and Prevention recommends use of the annual influenza vaccine and 2 pneumococcal vaccines for older adults to decrease risks of morbidity and mortality. However, actual vaccine up-take is estimated at 61.3% for pneumococcal vaccines and 65% for influenza vaccine in the 2013–2014 season. Vaccine up-take is affected by multiple socio-cultural and economic factors including general healthcare access and utilization, social networks and norms, communication with health providers and health information sources, as well as perceptions related to vaccines and targeted diseases. In this study, 8 focus group discussions (total N = 48) were conducted with adults 65+ years living in urban and suburban communities in the Detroit Metropolitan Area. The research objective was to increase understanding of barriers and facilitators to vaccine up-take in this age cohort within the context of general healthcare availability and accessibility, social networks, information sources, and personal perceptions of diseases and vaccines. The data suggest the need to integrate broader health care service experiences, concepts of knowledge of one's own well-being and vulnerabilities, and self-advocacy as factors associated with older adults' vaccine-use decisions. These data also support recognition of multiple levels of vaccine acceptance which can be disease specific. Implications include potential for increasing vaccine up-take through general improvement in health care delivery and services, as well as specific vaccine-focused patient and provider education programs.
KEYWORDS: healthcare accessibility, influenza, older adults, pneumococcal disease, vaccination up-take
Introduction
In the United States, influenza and Streptococcus pneumonia (pneumococcus) contribute significantly to outpatient clinic visits, emergency department use, and inpatient hospitalizations particularly for older adults (≥ 65 years). Economic analysis indicates that a total of $15.3 billion are spent for adults ≥ 65 y on vaccine preventable diseases. Nearly 80% of these costs ($12.1 billion) are associated with influenza and pneumococcus.1 Older adults often have multiple co-morbidities which increase risks for complications and death from vaccine-preventable diseases.2 In a study of influenza seasons 2010–2013, older adults experienced a disproportionate burden of hospitalizations (54–70%) and deaths (73–85%) compared to younger age groups. There are an estimated 400,000 hospitalizations annually for pneumococcal pneumonia with an overall case-fatality rate of 5–7% - however, this rate is estimated to be much higher for older adults.3
The Advisory Committee of Immunization Practices (ACIP) recommends the seasonal influenza vaccine for are all persons ≥6 months who do not have contraindications.4-5 Current recommendations for maximum protection against common serotypes of S. pneumonia among older adults include the use of both PPSV 23 [Pneumovax23©, Merck & Co., Inc.] and PCV13 [Prevnar 13©, Wyeth Pharmaceuticals, Inc.] at specified intervals.6 In 2014, an estimated 61.3% of older adults had received recommended pneumococcal vaccines.7 In 2013–2014, influenza vaccine uptake among older adults was 65%.8 Despite recommendations and the clear impact of these 2 vaccine-preventable diseases on morbidity and mortality among older adults, significant progress will need to be made to reach ‘Health People 2020’ targets of 90% up-take for both influenza and pneumococcal vaccines for this population cohort.9
In recent years, global attention has been directed toward understanding the complex and integrated factors which contribute to decisions related to use of vaccines. Evidence suggests that barriers and facilitators for vaccine up-take vary by multiple, integrated and complex socio-cultural and economic contexts as well as differences based on specific vaccine preventable diseases and associated vaccines.10-11 As such, the current study utilized a vaccine up-take framework which was developed to increase understanding of decision-making in regards to use of vaccines within a broader vision of socio-cultural factors, health system infrastructure, social networks, as well as individuals' disease and vaccine-related experiences, perceptions and beliefs (Fig. 1).12-13
Figure 1.
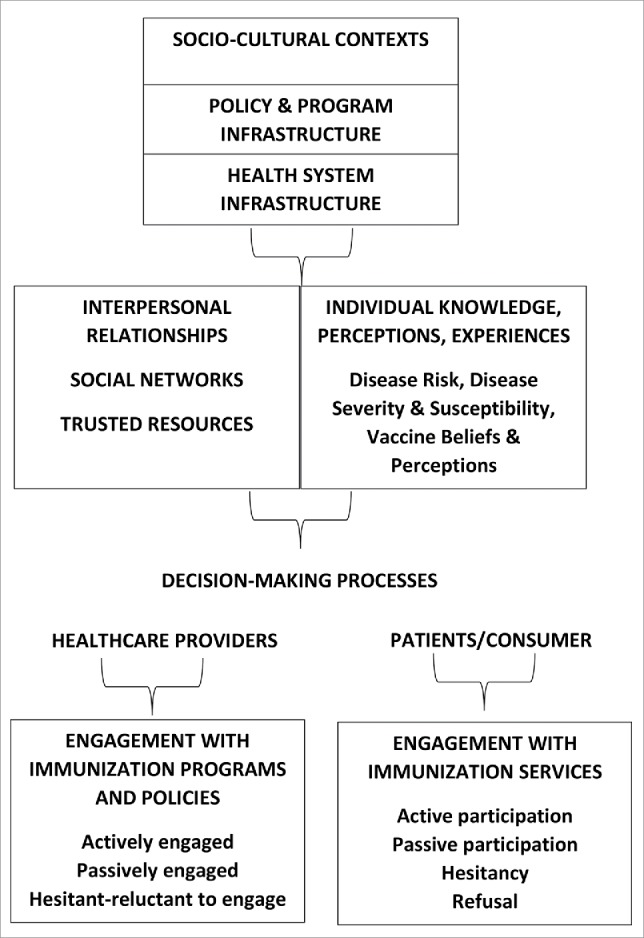
Vaccine up-take framework.
In this paper, we explore barriers and facilitators for US older adults in relation to influenza and pneumococcal vaccine up-take focused on: 1) healthcare access and utilization; 2) information resources and trust in those resources; 3) social networks and norms for vaccine use; 4) experiences and perceptions regarding influenza and pneumonia; and, 5) experiences and perceptions regarding vaccines in general and seasonal influenza and pneumococcal vaccines.
Results
Demographics
Forty-eight out-patients participated in 8 focus group discussions including 4 each in urban and suburban clinics. In the urban clinics, 92.9% of participants were female and 100% were African American. In the suburban clinics, 70.6% of participants were female and 52.9% were African American, 41.1% White, 3% Latino, and 3% no response. Mean participant age was 67.1 y.
Healthcare access and utilization
Respondents discussed multiple barriers and facilitators to accessing care. Primary issues were costs and transportation. One factor affecting participants' use of health facilities was the need to travel to multiple sites particularly in relation to insurance coverage.
“Not being able to get a prescription at the most convenient place. Like if your doctor's here and the pharmacy is here, but your insurance won't cover it (at that pharmacy), you've got to go somewhere else….” (Suburban)
In some conversations, participants associated costs with quality of care. Participants also discussed making choices about their healthcare and providers based on perceptions of care.
“You go to some clinics and don't have insurance. You in and out like a number….” (Urban)
“You might be dead trying to be cheaper.” (Suburban)
“…that's like going to the store. You ain't going to go to the store and pick up no seven day old bread when you can get a fresh loaf over here for the same thing…And the doctor, you want the best doctor for yourself…And since I done got sick with cancer, I don't short myself on nothing…if I got the money, I'm going to buy it….” (Urban)
Respondents discussed self-treatment for many symptoms associated with influenza and pneumonia. Such treatments included cough drops, use of a humidifier, OTC pain and cold medications. Respondents stated that they ‘know their own body’ and “you have to be your own advocate.”
“…with all my gadgets and medicine I got in the cabinet, I'm going to try all that first, and then if it don't do no good, I'm gone (to the doctor)…” (Urban)
“…if I feel alright without taking (the medication) I do not take them. Because I mean every time I go to the doctor they just find something new…” (Suburban)
“Sometimes I don't agree with what the doctor might want me to do. And so that is when I have difficulty following through. Because in my mind (doctors) are really good with emergency situations, but as far as staying healthy, they don't have a clue. That's the way I feel about doctors….” (Suburban)
Use of emergency rooms was also discussed. Some respondents were reluctant to use the emergency room because of cost and waiting time. In terms of the latter, one respondent said that she used EMT services in order to get in the “back door.”
“[if you use an ambulance] they have to take you right in…” (Urban)
“…go to the store and…take care of yourself before you actually go to the emergency. Because emergency, they charge a lot of money. If they don't keep you, you got to pay…” (Urban)
“…if you go to the doctor, it is only $25 or $35 (co-pay). But if you go to the ER, with a cough and they send you home. That's $100….” (Suburban)
Communication and information sources
A key issue throughout the discussions was communication between patient and providers. Trust in health provider was an integral component of communication and response to information provided.
“I could go to a 24 hour (urgent care clinic), but I want some care that I'm used to getting from a particular doctor.” (Suburban)
Respondents were well aware of time limits of health providers, and in relation to self-advocacy argued that patients need to be prepared to ask questions and clarify information and instructions.
“…when I get my prescription and I don't understand it, I stand right there and let the pharmacist tell me….” (Urban)
“I've never been to medical school, so I don't understand that (information).” (Urban)
“…you have to ask them…yeah, because they ain't going to tell you nothing if you don't say nothing…they'll give you the short version…I know with my doctor you get the short of everything and then the more you ask the more he tells…they ain't got time to explain all them details to every individual….” (Urban)
“…one of the things when I go to a doctor, I try and write down all of my questions ahead of time…cause I want to know those answers….” (Urban)
A few respondents also discussed getting mixed messages from different sources.
“The pharmacist is telling you one thing the doctor is telling you something else. [You need] to put both of them together….” (Urban)
Respondents want to be heard and related instances in which they complained about poor service. One respondent noted that she appreciated an opportunity given by the health system for patient feedback.
“And the [health system] is also very good about your visits to the doctor or emergency or tests…they're going to send of survey of what did you think about your visit and you can give feedback. And it's very helpful because if it wasn't good…somebody's going to call you and say ‘what happened’?” [Urban]
Respondents use a broad range of health information sources. These include written materials (e.g., pamphlets), posters, internet, and television shows. One respondent suggested that health insurance companies should provide clients with written material about vaccines.
In general, respondents' decision-making regarding healthcare and use of vaccines is significantly influenced by health providers' in-put or recommendations. Alternatively, a few respondents felt that health providers are not always forthcoming.
“The doctor wouldn't even offer it to you if he or she thought it was going to bring harm to you….” (Urban)
“…if I've never heard of it, I don't care what it is, a pop or a medicine… a TV ad is not going to make me use it. On the other hand, if I go to see my doctor and he says, ‘listen you really need to take this shot, this is the information on this shot’, then I'll read it…but if you just hand me a paper, that is like somebody handing me a flyer as I'm walking up the street…” (Urban)
“He's (the doctor) not going to tell you that there's formaldehyde in the flu shot….” (Suburban)
Social networks
A number of respondents discussed how their decisions regarding adult vaccines were affected by experiences and family members and friends. A few respondents also talked about influencing others to use vaccines including parents who are not vaccinating their children.
“People are scared due to other people getting sick from the shot….” (Urban)
“…I told my mother to get it…even though she's in her 80s, she said she never had it before…she won't get a lot of shots…but I talked to her and told her and she went and got it this year….” (Suburban)
“Have you go grandkids who the parents say, oh I don't want my kids to get autism…please talk to them. Cite an example if you have to….” (Suburban)
Despite social influences on respondents' decisions about vaccines, some respondents stated that personal experiences were of greater importance.
“I wouldn't take it (influenza vaccine) before because everybody said it would make you sick and I just didn't wanna take it…I decided just to take it the first time…and then I felt fine, so I took it the next time” (Urban)
Disease experience, knowledge, and perceptions
All of the respondents were well aware of symptoms and causes of influenza and pneumonia. Overall, both conditions were considered serious although in general respondents felt that pneumonia is more serious than the flu.
“(the flu) is like a brick wall fell on you….” (Urban)
“…you die quicker with pneumonia than you do with the flu….” (Urban)
Most participants had some personal experience with influenza. Fewer had experience with pneumonia, however one respondent talked about a friend who died from “double pneumonia.” Respondents felt that elderly and children were more vulnerable to both diseases. Other factors which they felt increased susceptibility were a compromised immune system, chronic respiratory conditions, use of tobacco, and environmental pollutants.
“I think since I've gotten older, I can't shake the flu as quick as I used to….” (Urban)
“And I would say using myself as an example, I get many many more flus than my husband because I have asthma….and he doesn't even get the shot” (Suburban)
A few respondents stated that they seldom if ever get sick.
“I don't even catch colds. I haven't had a cold in about four or five years, and when I do catch a cold, it is like a day or two…I contribute [this] to the fact that I eat healthy” (Urban)
Vaccine experience, knowledge, and perceptions
Respondents had a wide range of experiences with use of vaccines, as well as perceptions regarding the efficacy and risks and benefits associated with vaccine use. For some respondents, less than 100% efficacy is perceived as acceptable ‘odds’, while for others the feeling is that the risks outweigh the benefits.
“So, then you have all the risks that come with the vaccines and you don't have 100% benefit” (Suburban)
“Well, pneumonia (vaccine) because of your age you're at risk. I think it makes sense and I believe it. The odds are in your favor” (Urban)
Respondents were concerned about short- and long-term side effects and getting sick from the vaccine. Many concerns were based on personal experiences of feeling sick or contracting influenza after use of the vaccine. Some respondents felt that information was not readily available about risks from vaccine use.
“Well, I take it not to get sick, but I know last year after I got the shot it hurt for about a week, and I was like good God, that was a bad shot” (Urban)
“So we got a list of everything that's in the vaccines and how they're tied to certain things like autism which, you know, medical society is refuting that. But there's a lot of issues with the vaccines that their not telling the public” (Suburban)
“…a long time ago, the polio shot had something to do with monkey blood. Then they said AIDS came from monkey blood. So now a lot of people say, “Do we have the gene in us already”? So, I wanna make sure that these shots doesn't cause something else down the road…” (Urban)
Respondents were also concerned about how vaccines are developed and tested. There were issues raised in relation to ‘new vaccines’ and whether vaccines had been adequately tested with different groups of people.
“Since this is a new vaccine, how would you be able to determine if you're allergic to a new vaccine?” (Suburban)
“You know they gotta see what it's going to do to you, what kind of effect…particularly for [different] age groups…I want to know who they were testing it on the first ten years” (Urban)
“…how many of those people (in trials) died and what happened?” (Urban)
The focus group participants expressed various levels of acceptance of vaccines. One woman and her husband had participated in a trial. For others, their positive experiences increased their willingness to be vaccinated. Some respondents stated that they would use some vaccines but not others, and a few were adamant that they do not intend to use any vaccine.
“My husband and I were part of …the study about zoster, the shingles…I have a lot of people in my family who had the shingles and I know how painful it is. So, I was very interested in preventing that…” (Surburban)
“…when (my doctor) says pneumonia shot, I just say ‘okay’” (Suburban)
“I started taking flu shots about 17 years ago. I never had the flu. Five or six years I failed to take a flu shot. I came down with the flu for two weeks. I've been taking one ever since….” (Urban)
“…they ask me to get (shingles vaccine), I told them no. They asked me to take influenza, I said no. They asked me to take pneumonia, I said yes…because I had pneumonia…” (Suburban)
“I really didn't want the flu vaccine, however the pneumonia vaccine, I wanted that one” (Urban)
“I figure if the flu causes the pneumonia, if you take a flu shot why would you need to take the pneumonia shot?” (Urban)
“I've never had the flu in my life. I've never took the flu shot. I don't take no shots…” (Urban)
Discussion
Globally, vaccines are becoming an integral component of preventive healthcare for adults. In the United States, older adults are targeted for influenza and pneumococcal vaccines, as well as Zoster and Tdap. Significant research has been conducted to determine factors associated with vaccine up-take and vaccine hesitancy. Many of these studies have focused on socio-demographic factors, e.g., gender, ethnicity, education level, and behavioral factors, e.g., tobacco use, alcohol use, as potential predictors of vaccine use.14-16 Other research has focused on social and cultural variables including perceptions and beliefs about targeted diseases, perceived prevention efficacy, and attitudes regarding vaccines.17-18 In addition, economic factors including insurance status are associated with consumers' vaccination decisions.7
In this study, decisions about vaccination use among older adults were assessed within the contexts of barriers to healthcare, perceptions and experiences communicating with health providers, general attitudes regarding health services and use of medications, social networks and norms, and personal experiences and perceptions of influenza and pneumonia and associated vaccines. Through these discussions, respondents reveal multiple challenges in relation to costs of care, lack of transportation, and quality of health services. A key facilitator to care is development of trust in the health system and the providers.
Respondents report health care providers as key sources of information about vaccines. However, respondents also expressed concern about the limited time available to talk with their providers. Health providers, particularly those in large health systems, have a short period of time for face-to-face interaction with patients. This can mean that providers need to prioritize patient needs and use available time as the efficiently as possible. More recently, health providers are increasingly using email to communicate to patients outside of the time constraints of an office visit. Use of these alternative communication methods can be used to promote preventive medicine including use of adult vaccines. More research is needed to document effectiveness of such communication strategies between health providers and various patient populations.19
Throughout the discussions, participants describe the need to be an advocate for oneself, to have an opportunity to ask questions, and to have a mechanism through which they can report complaints about health services. This advocacy is based in part on a belief that an individual knows ‘one's own body’ better than anyone else, and therefore should have the final decision about use of medications and vaccines. Such a perspective is culture-specific, as research in other settings indicate strong beliefs in external factors in disease cause and treatment efficacy.20 This self-knowledge was also reflected in discussions of susceptibility to influenza and pneumonia. Respondents described themselves as having ‘weak immune systems’ or alternatively as ‘healthy’ and ‘never or seldom getting sick’. While this perspective increases self-expression and communication with health providers, in some instances self-advocacy may foster greater reliance on self-treatment or cessation in use of prescribed medications. Such outcomes can delay treatment and/or increase risk of complications.
Social networks provided respondents with information about others' experiences with vaccines and vaccine side effects, as well as support for vaccine use. Friends' and family members' perspectives and experiences clearly affect decisions about vaccine use. Less valuable and trusted information sources include television shows and pharmaceutical advertisements.
While concerns about side effects are well-documented reasons for vaccine hesitancy, respondents also discussed their understanding and trust in the development and testing of vaccines. To date, there has been limited discussion about increasing the scientific literacy of the public in order to facilitate knowledge exchange about vaccines and vaccine trials.21
As indicated in the vaccine framework, respondents report multiple levels of ‘acceptance’. While some respondents describe consistent use of vaccines over time and/or adherent to their health providers' advice, others are selective in terms of which vaccines they need. And while some respondents are open to possible use of ‘new’ vaccines, others are reluctant. A few respondents' statements suggest an anti-vaccine perspective which likely translates to refusal to use vaccines regardless of recommendations and information provided.
Data from the current study supplements quantitative research which indicate socio-economic, demographic, and attitudinal variables associated with vaccine up-take among older adults. These data provide information regarding more contextual and interpersonal factors, e.g., general experiences with the health system, provider-patient communication, as well as perceptions of self-care and management, and advocacy. Qualitative data by its nature allows for emergent issues and an iterative approach to document meanings and subjectivities of respondents. Qualitative research has been conducted globally to elucidate various population groups' perceptions of disease, prevention, and vaccines - - leading to identification of a range of factors associated with vaccine up-take including household and familiar lifestyles and context, body perceptions, balancing risks-benefits, perceptions of disease causality, immunity, and susceptibility, and trust in information resources.22-27 The current study adds to this body of literature.
Data from this study were used to develop educational materials about influenza and pneumococcal disease and vaccines specifically designed for older adults. These data are also being used to develop educational workshops for health care providers, establishment of health care provider ‘vaccine champions’ in primary care out-patient clinics, and system-level changes including physician reminders and reporting adult patient vaccine up-take to the Michigan Care Improvement Registry similar to regulations for childhood vaccines.
The study was conducted in 3 clinics in a large integrated health system in Detroit. As with other qualitative research, the data provide important in-depth information regarding respondents' experiences and perceptions; however, generalizability of the data is limited. Further confirmatory qualitative research with older adults in local communities or attending other clinics/health systems is needed to increase external validity of data. In addition, quantitative research with the same population base would enhance information about differences and similarities in knowledge, experiences and perceptions within and across socio-economic groups.
For older adults in a US metropolitan setting, decision-making in relation to vaccines is centered within individuals' health and healthcare experiences, and knowledge, and perceptions of themselves as self-advocates. Recognizing these linkages can facilitate development of educational programs and system changes that will improve the broader health care experiences for older adults and acknowledge and utilize perspectives of knowing oneself as a means of enabling an informed decision in relation to vaccines and other preventive and treatment modalities.
Materials and methods
Research sites and population
The Henry Ford Health System (HFHS) is a large integrated health system in the Detroit Metropolitan Area. In 2014, over 290,000 patients visited 30 primary care clinics with 28% of those patients 65 y and older. Data were collected at 3 of these primary care clinics including one in downtown Detroit serving primarily African American and lower- and lower-middle-income communities and 2 in suburban locations serving a more ethnically diverse mix of lower-middle and middle-income communities. Eligibility criteria for participation in the focus groups included being 65 y and older and a patient at one of the 3 targeted primary care clinics.
Participant recruitment
Participants were recruited by research staff during routine office visits. Potential participants were provided with information about the study and given information about time, and place of the focus groups. Reminder phone call were made the day before each group.
Instrument development
Focus group guides were developed and utilized to ensure that all topics were covered during each focus group discussion. The guides were based on the vaccine up-take framework. Minor changes were made to the instrument during data collection to allow exploration of emerging issues.
Data collection
Focus group discussions were digitally audio recorded and transcribed by a professional transcription service. A short demographic form was completed by each participant.
Data management and analysis
Transcribed data were entered into a qualitative data management program for coding and data searches. A coding dictionary was developed based on the vaccine-uptake framework. Text was reviewed and coded. The software enabled multiple codes to be assigned to single portions of text. Data were searched, and organized under the 5 key research constructs: 1) healthcare access and utilization; 2) information resources and trust in those resources; 3) social networks and norms for vaccine use; 4) experiences and perceptions regarding influenza and pneumonia; and, 5) experiences and perceptions regarding vaccines in general and seasonal influenza and pneumococcal vaccines. Patterns were identified within and across these constructs and exemplary text was extracted to support observed patterns. Demographic data were entered into Excel and descriptive statistics were calculated for gender, age, and ethnicity.
Ethics
All procedures performed were in accordance with the ethical standards of the institutional research committee at Henry Ford Health System and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Written informed consent was obtained from all participants included in the study.
Disclosure of potential conflicts of interest
No potential conflicts of interest were disclosed.
Acknowledgments
We would like to thank the clinic staff at our data collection sites within the Henry Ford Health System and the patients who contributed their time and shared their experiences and opinions. We would also like to thank the project research assistant Mr. Maurice Bulls and Ms. Brittany Nelson from Wayne State University College of Nursing who interned with us during the summer of 2013. Mr. Bulls and Ms. Nelson were actively involved with recruitment and conduct of the focus group discussions.
Funding
The current study was funded by Pfizer Pharmaceuticals (grant # H10184).
References
- [1].McLaughlin JM, McGinnis JJ, Tan L, Mercatante A, Fortuna J. Estimated human and economic burden of four major adult vaccine-preventable diseases in the United States, 2013. J Primary Prevent 2015; 36:259-73; http://dx.doi.org/ 10.1007/s10935-015-0394-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Cilloniz C, Polverino E, Ewig S, Aliberti S, Gabarrus A, Menendez R. Impact of age and comorbidity on cause and outcome in community-acquired pneumonia. Chest 2013; 144(3):999-1007; PMID:23670047; http://dx.doi.org/ 10.1378/chest.13-0062 [DOI] [PubMed] [Google Scholar]
- [3].Centers for Disease Control and Prevention Pneumococcal Disease. [Internet] 2013. [cited 2016June6]: Available from: http://www.cdc.gov/vaccines/pubs/pinkbook/downloads/pneumo.pdf [Google Scholar]
- [4].Centers for Disease Control and Prevention . Prevention and control of influenza with vaccines: Recommendations of the Advisory Committee Practices, United States, 2015–16 influenza season. MMWR 2015; 64(30):818-25; PMID:26247435 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Pilshvili T, Bennett NM. Pneumococcal disease prevention among adults: strategies for use of pneumococcal vaccines. Am J Prev Med 2015; 49(6 Suppl 4):S383-90; PMID:26590438; http://dx.doi.org/ 10.1016/j.amepre.2015.09.008 [DOI] [PubMed] [Google Scholar]
- [6].Centers for Disease Control and Prevention . Use of 13-valent pneumococcal conjugate vaccine and 23-valent pneumococcal polysaccharide vaccine among adults aged >65 years: recommends of the advisory committee on immunization practices (ACIP). MMWR 2014; 63(37):822-5; PMID:25233284 [PMC free article] [PubMed] [Google Scholar]
- [7].Williams WW, Lu PJ, O'Halloran A, Kim DK, Grohskopf LA, Pilishvili T, Skoff TH, Nelson NP, Harpaz R, Markowitz LE, et al.. Surveillance of vaccination coverage among adult populations, United States, 2014. MMWR 2016; 65(1):1-36; PMID:26844596; http://dx.doi.org/ 10.15585/mmwr.su6501a1 [DOI] [PubMed] [Google Scholar]
- [8].Centers for Disease Control and Prevention Flu 2013–2014 [Internet] 2014. [cited 2016June6]: Available from: http://www.cdc.gov/flu/fluvaxview/coverage-1314estimates.htm [Google Scholar]
- [9].Centers for Disease Control and Prevention Healthy People 2020 [Internet] 2016 [cited 2016August3]: Available from: http://www.cdc.gov/aging/agingdata/data-portal/healthy-people.html [Google Scholar]
- [10].Larson HJ, Jarrett C, Eckersberger E, Smith DM, Paterson P. Understanding vaccine hesitancy around vaccines and vaccination from a global perspective: a systematic review of published literature, 2007–2012. Vaccine 2014; 32(19):2150-9; PMID:24598724; http://dx.doi.org/ 10.1016/j.vaccine.2014.01.081 [DOI] [PubMed] [Google Scholar]
- [11].Kaljee LM, Pack R, Pach A, Nyamete A, Stanton BF. Sociobehavioural research methods for the introduction of vaccines in the diseases of the most impoverished programme. J Health Popul Nutr 2004; 22(3):293-303; PMID:15609782 [PubMed] [Google Scholar]
- [12].Kar SK, Pach A, Sah B, Kerketta AS, Patnaik B, Moqasale V, Kim YH, Rath SB, Shin S, Khuntia HK, et al.. Up-take during an oral cholera vaccine pilot demonstration program, Odisah India. Hum Vac Immuno 2014; 10(10):2834-42; http://dx.doi.org/ 10.4161/21645515.2014.971655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Sur D, Manna B, Chakrabarty N, Kaljee L, Riel R, Pach A, Kanungo S, Deen J, Ochiai RL, Clemens J, et al.. Vaccine desirability during an effectiveness trial of the typhoid fever polysaccharide Vi vaccine, Kolkata India. Hum Vaccine 2009; 5(9):614-20; http://dx.doi.org/ 10.4161/hv.9313 [DOI] [PubMed] [Google Scholar]
- [14].Shahrabani S, Benzion U. The effects of socioeconomic factors on the decision to be vaccinated: the case of flu shot vaccination. Isr Med Assoc J 2006; 8(9):630-4; PMID:17058415 [PubMed] [Google Scholar]
- [15].Andrew MK, McNeil S, Merry H, Rockwood K. Rates of influenza vaccination in older adults and factors associated with vaccine use: a secondary analysis of the Canadian Study of Health and Aging. BMC Public Health 2004; 11(4):36; http://dx.doi.org/ 10.1186/1471-2458-4-36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Krueger P, St. Amant O, Loeb M. Predictors of pneumococcal vaccination among older adults with pneumonia: findings from the community acquired pneumonia impact study. BMC Geriatr 2010; 30(10):44; http://dx.doi.org/ 10.1186/1471-2318-10-44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Wooton KG, Wortley PM, Singleton JA, Euler G. Perceptions matter: beliefs about influenza vaccine and vaccination behavior among elderly white, black and Hispanic Americans. Vaccine 2012; 30(48):6927-34; PMID:22939908; http://dx.doi.org/ 10.1016/j.vaccine.2012.08.036 [DOI] [PubMed] [Google Scholar]
- [18].Nowak GJ, Sheedy K, Bursey K, Smith TM, Basket M. Promoting influenza vaccination: insights from a qualitative meta-analysis of 14 years of influenza-related communications research by US. Centers for Disease Control and Prevention (CDC) . Vaccine 2015; 33(24):2741-56; PMID:25936726 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Cook N, Maganti M, Dobriyal A, Sheinis M, Wei AC, Ringash J, Krzyzanowska MK. E-mail communication practices and preferences among patients and providers in a large comprehensive cancer center. J Oncol Pract 2016; 12(7):676-84; PMID:27352950; http://dx.doi.org/ 10.1200/JOP.2015.008722 [DOI] [PubMed] [Google Scholar]
- [20].Kaljee L, Pach A, Thriemer K, Ley B, Ali SM, Jiddawi M, Puri M, von Seidlein L, Deen J, Ochiai L, et al.. Utilization and accessibility of health care on Pemba Island, Tanzania: implications for health outcomes and surveillance for typhoid fever. Am J Trop Med Hyg 2013; 88(1):144-152; PMID:23208887; http://dx.doi.org/ 10.4269/ajtmh.2012.12-0288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Kaljee L, Pach A, Stanton B. Applied anthropology, vaccine trials and feasibility studies: intersections of local knowledge, biomedicine, and policy. Practicing Anthropology 2011. 33(4):39-43; http://dx.doi.org/ 10.17730/praa.33.4.j14752n270j1w761 [DOI] [Google Scholar]
- [22].Fadda M, Depping MK, Schulz PJ. Addressing issues of vaccination literacy and psychological empowerment in the measles-mumps-rubella (MMR) vaccination decision-making: a qualitative study. BMC Publish Health 2015; 15:836; http://dx.doi.org/ 10.1186/s12889-015-2200-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Harmsen IA, Mollema L, Ruiter RA, Paulussen TG, de Melker HE, Kok G. Why parents refuse childhood vaccination: a qualitative study using online focus groups. BMC Public Health 2013; 13:1183; PMID:24341406; http://dx.doi.org/ 10.1186/1471-2458-13-1183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Reich JA. Of natural bodies and antibodies: parents' vaccine refusal and the dichotomies of natural and artificial. Soc Sci Med 2016; 157:103-10; PMID:27082021; http://dx.doi.org/ 10.1016/j.socscimed.2016.04.001 [DOI] [PubMed] [Google Scholar]
- [25].Blaisdell LL, Gutheil C, Hootsmans NA, Han PK. Unknown risks: parental hesitation about vaccination. Med Decis Making 2016; 36(4):479-89; PMID:26506958; http://dx.doi.org/ 10.1177/0272989X15607855 [DOI] [PubMed] [Google Scholar]
- [26].Brown T, Goldman SN, Acosta F, Garrett AM, Lee JY, Persell SD, Cameron KA. Understanding black patients' refusal of pneumococcal vaccination. J Racial Ethn Health Disparities 2015; [Epub ahead of print]; PMID:27294765; http://dx.doi.org/26293806 10.1007/240615-015-0193-9 [DOI] [PubMed] [Google Scholar]
- [27].Salad J, Verdonk P, de Boer F, Abma TA. “A Somali girl is Muslim and does not have premarital sex. Is vaccination really necessary?:” a qualitative study into the perceptions of Somali women in the Netherlands about the prevention of cervical cancer. Int J Equity Health 2015; 14:68; PMID:26293806; http://dx.doi.org/ 10.1186/s12939-015-0198-3 [DOI] [PMC free article] [PubMed] [Google Scholar]


