Abstract
Introduction:
Natural orifice transluminal endoscopic surgery (NOTES) is a challenging minimally invasive procedure. Although laparoscopic techniques for liver resection are gaining acceptance worldwide, few studies have investigated NOTES liver resection. We used a porcine model to assess the feasibility and safety of transvaginal NOTES liver resection (TV NOTES LR).
Materials and Methods:
Nine female pigs underwent TV NOTES LR. A nonsurvival acute porcine model with general anesthesia was used in all cases. Using hybrid NOTES technique, we placed only 1 umbilical 12-mm umbilical trocar in the abdominal wall, which was used to create pneumoperitoneum. A laparoscope was then advanced to obtain intra-abdominal visualization. A 15-mm vaginal trocar was inserted under direct laparoscopic vision, and a flexible endoscope was introduced through the vaginal trocar. A long, flexible grasper and endocavity retractor were used to stably retract the liver. The liver edge was partially transected using energy devices inserted through the umbilical trocar. To transect the left lateral lobe, a flexible linear stapler was inserted alongside the vaginal trocar. A specimen extraction bag was deployed and extracted transvaginally. Blood loss, bile leakage, operative time, and specimen size were evaluated. Necropsy studies were performed after the procedures.
Results:
Eighteen transvaginal NOTES partial liver resections and 4 transvaginal NOTES left lateral lobectomies were successfully performed on 9 pigs. Mean operative time was 165.8 minutes, and mean estimated blood loss was 76.6 mL. All TV NOTES LRs were performed without complications or deaths. Necropsy showed no bile leakage from remnant liver.
Conclusions:
Our porcine model suggests that TV NOTES LR is technically feasible and safe and has the potential for clinical use as a minimally invasive alternative to conventional laparoscopic liver resection.
Key Words: transvaginal, NOTES, liver, hepatectomy, porcine, animal model
Natural orifice transluminal endoscopic surgery (NOTES) is an emerging minimally invasive procedure that requires no external body incisions. Scarless surgery is appealing to many clinicians, as it is the ultimate goal of minimally invasive surgery. However, development of NOTES has been gradual because technological evolution in surgical instrumentation has been slow to catch up with this innovation.
The first animal study of NOTES was reported by Kallo et al,1 in 2004. A variety of approaches have been used in animal models of NOTES, including cholecystectomy, splenectomy, gastrojejunostomy, tubal ligation, and oophorectomy.2–6 Clinical transvaginal (TV) NOTES cholecystectomy was described in 2007.7,8 A recent study found that NOTES resulted in less postoperative pain9,10 and excellent cosmetic results.11–13 Downsizing of incisions, trocar size, and trocar number can help decrease postoperative pain and increase postoperative quality of life.14 Data from large case series and case registries suggest that TV hybrid NOTES cholecystectomy is safe when performed by surgeons well trained in minimally invasive techniques.15–17 A recent systematic review and meta-analysis of TV hybrid NOTES cholecystectomy18 supports those findings.
Laparoscopic liver resection (LLR) was initially performed by Reich et al,19 in 1991. Initially, this procedure was highly specialized due to technical difficulties mainly related to achieving hemostasis during liver parenchymal transection. The development of surgical devices to separate the hepatic parenchyma has enabled bloodless dissection.20 The International Consensus Meeting on Laparoscopic Liver Surgery was held twice, in 2008 and 2014. Their first statement affirmed that laparoscopic liver surgery is safe and effective for management of surgical liver disease when performed by trained surgeons with experience in hepatobiliary and laparoscopic surgery.21 Although the evidence is somewhat limited, systematic reviews and meta-analyses of the benefits of LLR suggest that there are significant improvements in intraoperative bleeding, transfusion rate, postoperative complications, and duration of hospital stay.22–31 The Second Consensus Meeting evaluated the current status of laparoscopic liver surgery and provided recommendations for future development.32 The feasibility and safety of LLR were confirmed in this international consensus meeting. Thus, recognition of LLR has increased, and the procedure is now widely performed.
NOTES liver resection (NOTES LR) has the potential advantages of NOTES and LLR, as it is less invasive than conventional LLR, results in less postoperative pain and better cosmetic outcomes, and avoids incision-related complications. We used a porcine model of TV NOTES LR to evaluate the safety and feasibility of this procedure.
MATERIALS AND METHODS
This study was a collaboration between Toho University and University of California, San Diego (UCSD), and all procedures were performed in accordance with the institutional animal care and use committee protocols of Toho University and UCSD. Nine female pigs (5 at Toho University, 4 at UCSD; weight 45 to 50 kg) underwent TV NOTES LR by means of hybrid technique. Before each procedure, general anesthesia was administered in the form of an intramuscular preanesthetic injection of ketamine (33 mg/kg), xylazine (2 mg/kg), and atropine (0.05 mg/kg). Intravenous access was established by way of a large ear vein, after which anesthesia was induced. After intubation and administration of propofol (2.4 mg/kg), general anesthesia was maintained with isoflurane (1% to 2%). The pig was placed in supine position with both hind legs abducted, and a 12-Fr Foley catheter was used to decompress the bladder (Fig. 1). TV NOTES partial liver resection of the edge of the right and left median lobe and left lateral lobectomy were performed.
FIGURE 1.
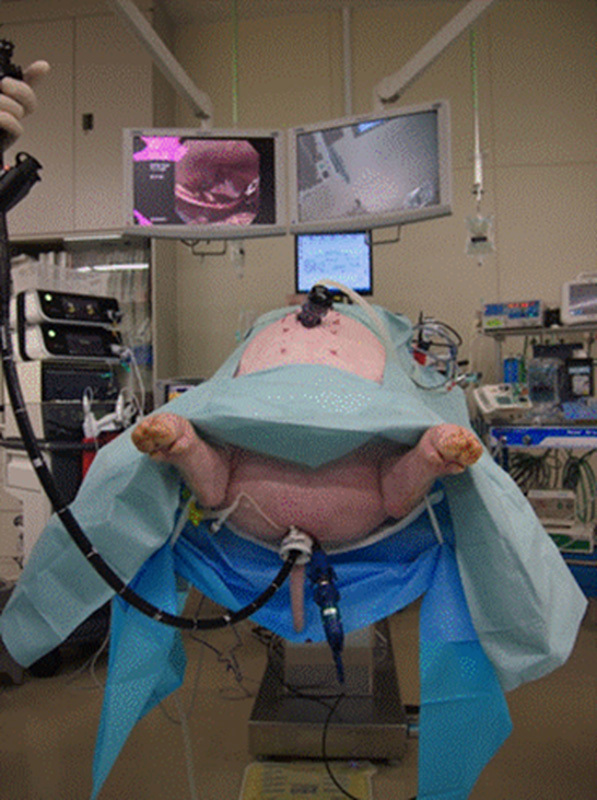
Operative position and setting during TV NOTES liver resection. TV NOTES indicates transvaginal natural orifice transluminal endoscopic surgery.
Duration of TV access, hepatectomy, total operative time, blood loss, and size of the resected specimen were measured. The pigs were then euthanized in accordance with the centers’ animal care protocols. Presence of hemorrhage, bile leak, and organ injury was then determined during necropsy.
Operative Procedure
TV Access for Hybrid NOTES
Using standard open technique, first 12-mm trocar was inserted at the side of the umbilicus. Pneumoperitoneum was created at a pressure of 10 mm Hg, and a 10-mm, 30- degree rigid camera (Stryker, Kalamazoo, MI) was inserted into the abdominal cavity. The operating table was tilted to a Trendelenburg position. A 15-mm TV trocar (length, 15 cm) was inserted under direct laparoscopic vision through the umbilical trocar, to avoid organ injury. A dual-channel gastroscope (Olympus GIF 2T240; Tokyo, Japan) was then inserted into the abdominal cavity through the TV trocar (Fig. 2). A long flexible grasper (Novare, Cupertino, CA) was inserted alongside the vaginal trocar. The gastroscope and grasper were positioned in the right upper abdomen by laparoscopic view. The pig was then placed in a reverse Trendelenburg position and observation was changed to a flexible endoscopic view.
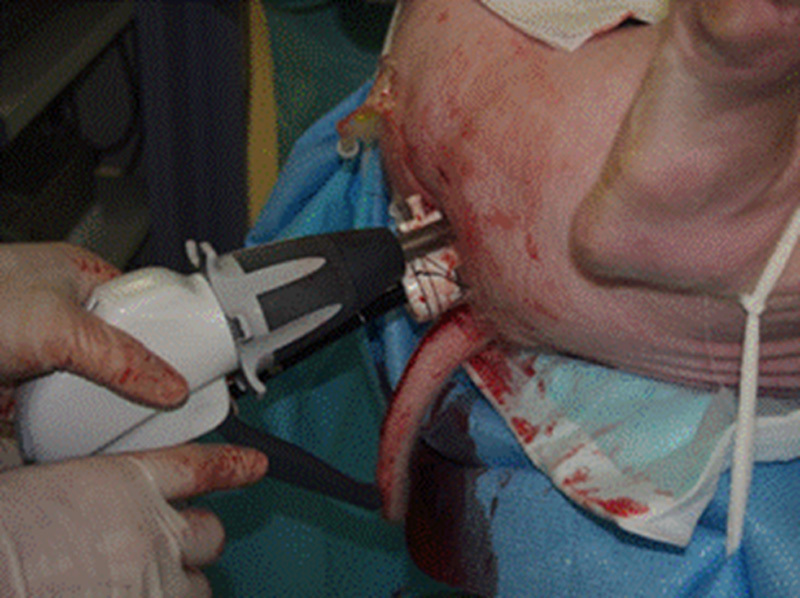
FIGURE 2.
The flexible endoscope is inserted through the vaginal trocar.
Partial Liver Resection in TV NOTES
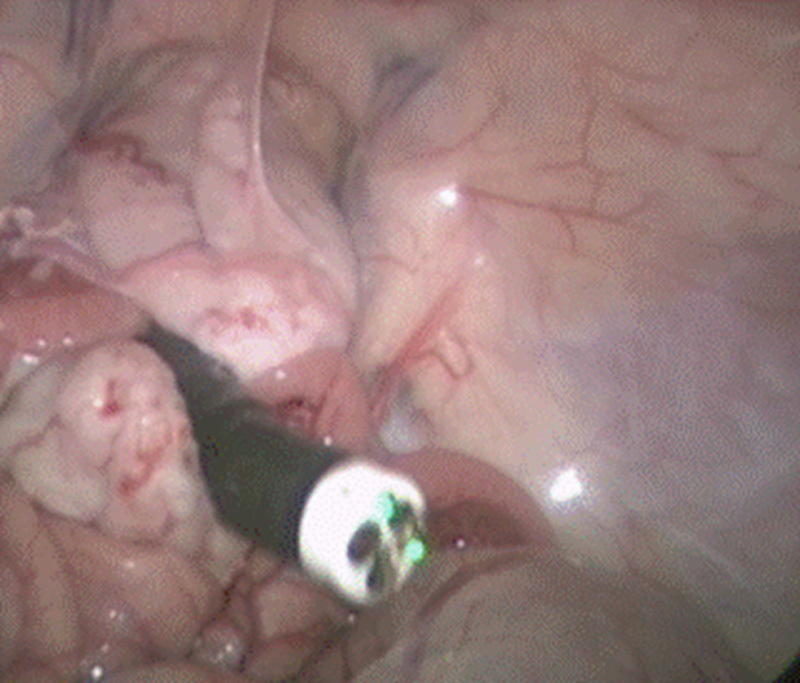
Electric cautery was used to mark the presumptive tumor and liver resection lines on the liver edge (Fig. 3). The liver edge was then grasped with the long grasper transvaginally. A self-retaining intracorporeal retractor, the Cinch Organ Retractor System (Aesculap, Tuttlingen, Germany), was used to obtain sufficient exposure during the procedure. The liver was transected using laparoscopic coagulating shears (Fig. 4). Because of the presence of intrahepatic vessels, the deep liver layer was transected by using a laparoscopic bipolar sealing device. Bleeding was managed by a forceps electrocautery device inserted through the working channel of the flexible endoscope. A saline-enhanced radiofrequency ablation device (IO-Advance electrode; AMCO Inc., Tokyo Japan) was used for management of persistent bleeding. Specimens were removed transvaginally by using a retrieval pouch (EndoCatch II; Covidien, Mansfield, MA) (Fig. 5).
FIGURE 3.

The presumptive tumor and resection lines are marked on the liver surface.
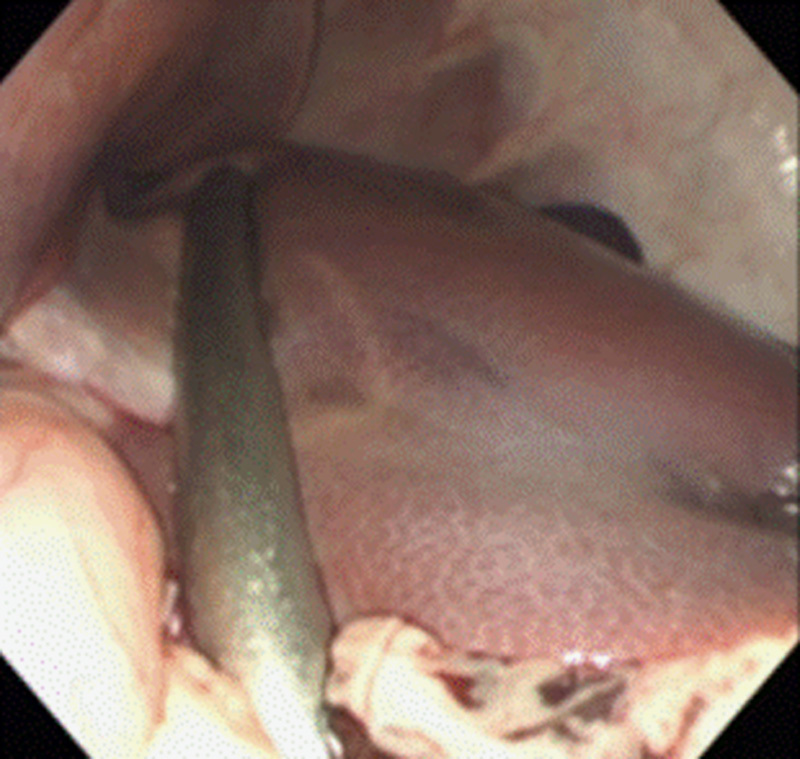
FIGURE 4.
The liver edge was resected by using laparoscopic coagulating shears inserted through the umbilical port.
FIGURE 5.
The specimen was easily removed through the vagina.
Left Lateral Lobectomy in TV NOTES
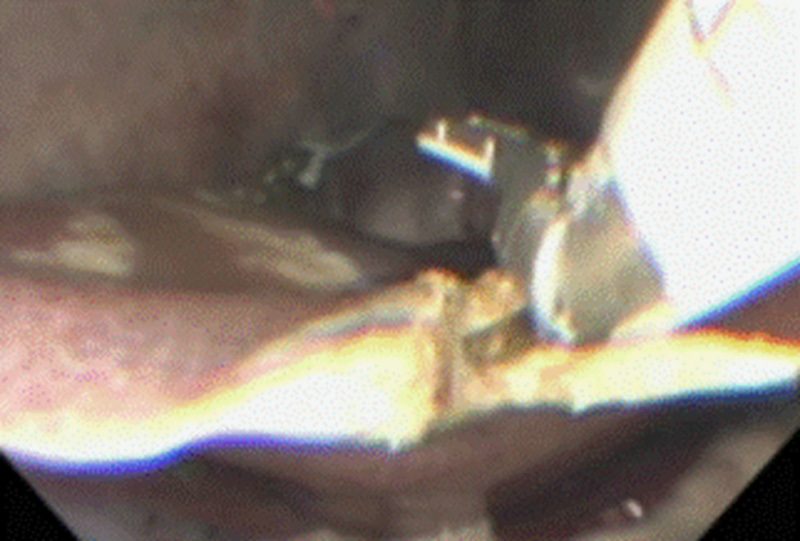
The operating table was adjusted to the Trendelenburg position, to use gravity for emptying the pelvic cavity. The Echelon LONG60A (Ethicon EndoSurgery, Cincinnati, OH) was inserted carefully alongside the vaginal trocar (Fig. 6). The pig was then placed back in the reverse Trendelenburg position. A Cinch Organ Retractor System inserted through the umbilical trocar was used to lift the left medial lobe, to allow for sufficient exposure of Glisson’s pedicles in the left lateral lobe. Liver parenchymal transection with division of intrahepatic vessels was performed by using the Gold cartridge of the Echelon LONG60A (Fig. 7). The stapler was used 2 or 3 times to transect the entire left lateral lobe. The specimen was removed transvaginally with an EndoCatch II bag, under transumbilical laparoscopic view.
FIGURE 6.
The long laparoscopic linear stapler was inserted alongside the vaginal trocar, for transection of the left lateral lobe.
FIGURE 7.
The left lateral lobe is transected with the laparoscopic linear stapler.
RESULTS
Eighteen partial liver resections were performed in 9 pigs. Four left lateral lobectomies were performed in 4 pigs. All resections were performed by TV NOTES with no conversion to conventional laparoscopic or open hepatectomy. There were no intraoperative complications or deaths. The average duration of TV access was 31.9 minutes (range, 15 to 50 min). Average duration of resection was 37.6 minutes (range, 23 to 56 min) for partial liver resection and 34.5 minutes (range, 25 to 41 min) for left lateral lobectomy. Overall operative duration was 165.8 minutes (range, 112 to 230 min). Average estimated blood loss was 76.6 mL (range, 10 to 254 mL).
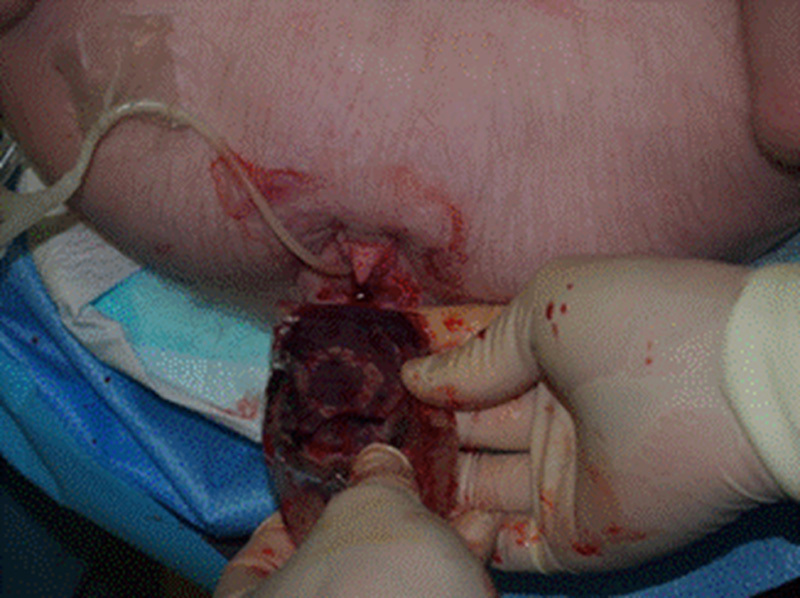
All specimens were easily removed transvaginally in partial resection cases. However, during the procedure for the first case, specimens could not be removed transvaginally to the pelvic cavity during left lateral lobectomy, due to the large volume of the liver. Therefore, laparoscopic scissors were used for intra-abdominal reduction of specimens to half the original size. For the second and subsequent cases, specimens were removed transvaginally. The average specimen size for partial liver resections was 6.2×5.0 cm. The average size for 1 of the 2 specimens retrieved during left lateral lobectomies was 14.6×10.6 cm (Fig. 8). No hemorrhage, bile leakage, or other organ injury was noted in necropsy studies.
FIGURE 8.
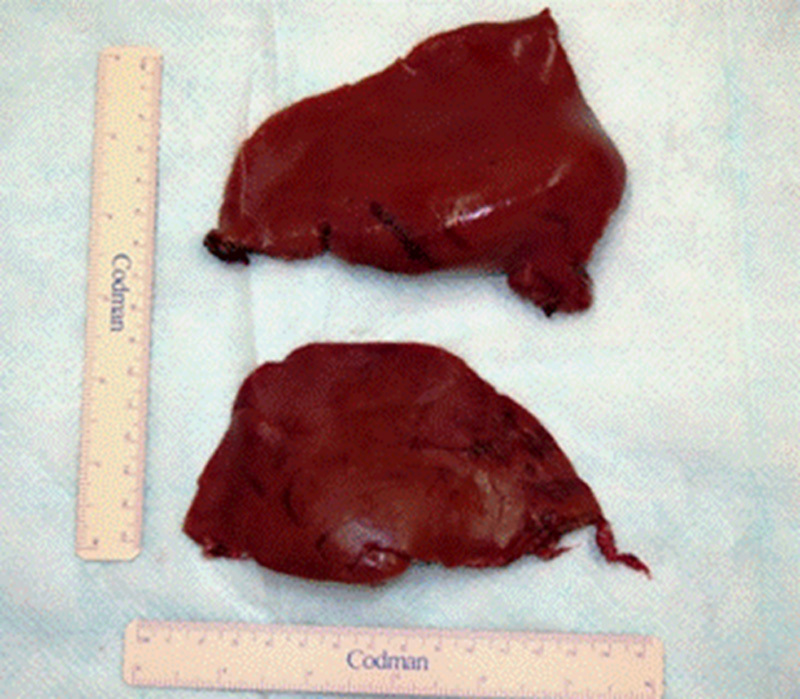
The specimens were retrieved transvaginally.
DISCUSSION
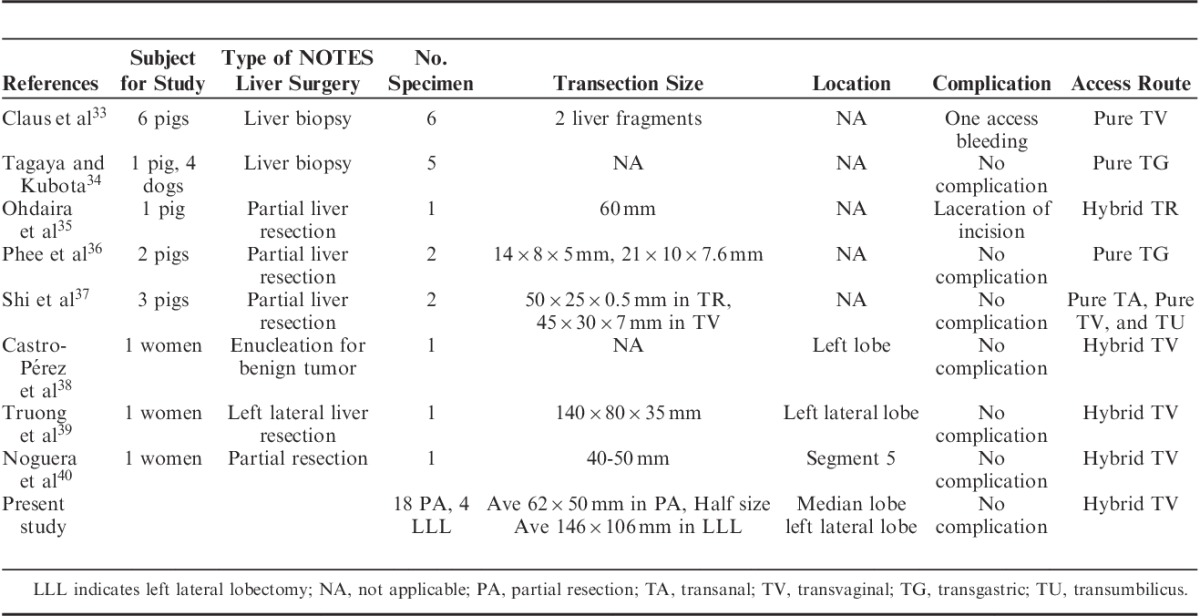
In theory, NOTES LR provides the benefits of NOTES and conventional LLR. However, few studies have evaluated NOTES liver surgery in animals or humans33–40 (Table 1). All experimental studies of NOTES LR involved only liver biopsy33,34 or a small number of local resections (1 to 2 wedge liver resections35–37). Only 3 human clinical case reports described the use of NOTES LR for partial liver resection or left lateral sectionectomy.38–40 Thus, NOTES LR remains a nascent technique. We believe that the present study is the first to establish a technical model for TV NOTES LR in a porcine model. NOTES LR uses various natural orifices, including the vagina,33 stomach,34 rectum,35,37 and umbilicus, as access routes. Natural orifices are used for far more than specimen extraction by means of natural orifice specimen extraction (NOSE).41–45 NOSE is appealing because it maximizes the benefits of laparoscopic surgery while reducing potential abdominal extraction wound complications. In addition, smaller incisions improve cosmetic results and decrease postoperative pain, which is directly associated with incision length.41–48 Transvaginal access is the most frequently used route for clinical NOTES49 and NOSE procedures,41–45 and the TV approach provides safe entry, easy access, and lower risk of contamination of the abdominal cavity, as compared with gut access.50–52 The vaginal wall can be easily closed using standard suturing methods under direct vision. Moreover, direction for the manipulation toward the liver can be straight angle by the TV approach, similar to conventional LLR. Therefore, all previous clinical studies of NOTES LR used a TV approach.38–40 The primary technical issue in NOTES LR is overcoming difficulties in the operative field and procedure, which are related to the limited maneuverability afforded by the natural orifice. Exposure of the hepatic parenchymal transection plane is a key achievement in successful liver resection and is best accomplished by hybrid NOTES, which uses laparoscopic trocars for assistance. Almost all clinical studies of NOTES used hybrid technique with the assistance of 2 or more abdominal trocars.38–40 The present study used only 1 trocar—a 12-mm umbilical trocar—which was minimal but extremely helpful. In addition, the long articulating grasper and self-retaining retractor helped obtain optimal exposure of the operative field, by retracting the liver during the procedure.
TABLE 1.
Review and Our Case of NOTES Procedures
Transection of liver parenchyma with adequate control of bleeding is essential during liver surgery. Appropriate selection and use of energy devices are indispensable, especially in endoscopic procedures, during which management of unexpected bleeding is more difficult than in open surgery.53 The energy devices used in liver transection each have important roles: ultrasonic shears are used for tissue transection of the superficial layer, the bipolar tissue sealing device for the deep layer, and the saline-enhanced monopolar device for tissue coagulation and hemostasis. A long stapling device that traverses the distance from the vagina to the liver is available for liver parenchymal transection in hybrid TV NOTES procedures and is described in our previous study of clinical liver resection.54
In our series, transected specimens could be easily removed from the vagina in all partial liver resection cases. In contrast, it was not possible to remove the entire left lateral lobe through the porcine vagina. Of course, there are anatomic differences between the porcine and human pelvic cavity and vagina. Truong et al39 reported that they were able to remove a 14-cm left lateral liver section through the vagina. However, intracorporeal downsizing with scrupulous attention to avoid exposure of malignancies may be necessary to retrieve large specimens through a natural orifice. In addition, future studies should evaluate vaginal trauma after specimen removal.
CONCLUSIONS
TV NOTES LR is technically feasible and safely reproducible for liver resections of the lower edge and left lateral section of the liver. Our experience indicates that this procedure is indicated for selected cases when performed by surgeons with appropriate training and knowledge of conventional LLR.
ACKNOWLEDGMENTS
The authors are grateful thank for the collaboration of the staff at UCSD and Toho University.
Footnotes
Supported by a grant from Japan NOTES.
B.J.S. received financial support from ValenTx Inc. for work not related to the present research. The remaining authors declare no conflicts of interest.
REFERENCES
- 1.Kalloo AN, Singh VK, Jagannath SB, et al. Flexible transgastric peritoneoscopy: A novel approach to diagnostic and therapeutic interventions in the peritoneal cavity. Gastrointest Endosc. 2004;60:114–117. [DOI] [PubMed] [Google Scholar]
- 2.Jagannath SB, Kantesovoy SV, Vaughn CA, et al. Per oral transgastric endoscopic ligation of fallopian tubes with long term survival in poricine model. Gastrointest Endosc. 2005;61:449–453. [DOI] [PubMed] [Google Scholar]
- 3.Wagh MS, Merrifield BF, Thompson CC. Survival studies after transgastricoophorectomy and tubectomy in a porcine model. Gastrointest Endosc. 2006;63:473–478. [DOI] [PubMed] [Google Scholar]
- 4.Kantesovoy SV, Hu B, Jagannath SB, et al. Transgastric endoscopic splenectomy: Is it possible? Surg Endosc. 2006;20:522–525. [DOI] [PubMed] [Google Scholar]
- 5.Bergstrom M, Ikeda K, Swain P, et al. Transgastric anastomosis by using flexible endoscopy in a porcine model (with video). Gastrointest Endosc. 2006;63:307–312. [DOI] [PubMed] [Google Scholar]
- 6.Pai RD, Fong DG, Bundga ME, et al. Transcolonic endoscopic cholecystectomy; a NOTES survival study in a porcine model (with video). Gastrointest Endosc. 2006;64:428–434. [DOI] [PubMed] [Google Scholar]
- 7.Marescaux J, Dallemagne B, Perretta S, et al. Surgery without scars: report of transluminal cholecystectomy in human being. Arch Surg. 2007;142:823–826. [DOI] [PubMed] [Google Scholar]
- 8.Bessler M, Stevens PD, Milone L, et al. Transvaginal laparoscopically assisted endoscopic cholecystectomy: a hybrid approach to natural orifice surgery. Gastrointest Endosc. 2007;66:1243–1245. [DOI] [PubMed] [Google Scholar]
- 9.Hensel M, Schernikau U, Schmidt A, et al. Comparison between transvaginal and laparoscopic cholecystectomy: a retrospective case-control study. Zentralbl Chir. 2012;137:48–54. [DOI] [PubMed] [Google Scholar]
- 10.Kilian M, Raue W, Menenakos C, et al. Transvaginal-hybrid vs. single-port-access vs. ‘conventional’ laparoscopic cholecystectomy: a prospective observational study. Langenbecks Arch Surg. 2011;396:709–715. [DOI] [PubMed] [Google Scholar]
- 11.Bulian DR, Trump L, Knuth J, et al. Long-term results of transvaginal/transumbilical versus classical laparoscopiccholecystectomy—an analysis of 88 patients. Langenbecks Arch Surg. 2013;398:571–579. [DOI] [PubMed] [Google Scholar]
- 12.van den Boezem PB, Velthuis S, Lourens HJ, et al. Single-incision and NOTES cholecystectomy, are there clinical or cosmetic advantages when compared to conventional laparoscopic cholecystectomy? A case-control study comparing single-incision, transvaginal, and conventional laparoscopic technique for cholecystectomy. World J Surg. 2014;38:25–32. [DOI] [PubMed] [Google Scholar]
- 13.Bulian DR, Knuth J, Cerasani N, et al. Transvaginal/transumbilical hybrid-NOTES versus 3-trocar needlescopic cholecystectomy: short-term results of a randomized clinical trial. Ann Surg Ann Surg. 2015;261:451–458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hildebrand P, Roblick UJ, Keller R, et al. What is the value of minimizing access trauma for patients? Chirurg. 2007;78:494–496–500. [DOI] [PubMed] [Google Scholar]
- 15.Nijhawan S, Barajas-Gamboa JS, Majid S, et al. NOTES transvaginal hybrid cholecystectomy: the United States human experience. Surg Endosc. 2013;27:514–517. [DOI] [PubMed] [Google Scholar]
- 16.Lehmann KS, Ritz JP, Wibmer A, et al. The German registry for natural orifice translumenal endoscopic surgery: report of the first 551 patients. Ann Surg. 2010;252:263–270. [DOI] [PubMed] [Google Scholar]
- 17.Arezzo A, Zornig C, Mofid H, et al. The EURO-NOTES clinical registry for natural orifice transluminal endoscopic surgery: a 2-year activity report. Surg Endosc. 2013;27:3073–3084. [DOI] [PubMed] [Google Scholar]
- 18.Sodergren MH, Markar S, Pucher PH, et al. Safety of transvaginal hybrid NOTES cholecystectomy: a systematic review and meta-analysis. Surg Endosc. 2015;29:2077–2090. [DOI] [PubMed] [Google Scholar]
- 19.Reich H, McGlynn F, DeCaprio J, et al. Laparoscopic excision of benign liver lesions. Obstet Gynecol. 1991;78:956–958. [PubMed] [Google Scholar]
- 20.Otsuka Y, Tsuchiya M, Maeda T, et al. Laparoscopic hepatectomy for liver tumors: proposals for standardization. J Hepatobiliary Pancreat Surg. 2009;16:720–725. [DOI] [PubMed] [Google Scholar]
- 21.Buell JF, Cherqui D, Geller DA, et al. World Consensus Conference on Laparoscopic Surgery. The International Position on Laparoscopic Liver SurgeryThe Louisville Statement, 2008. Ann Surg. 2009;250:825–830. [DOI] [PubMed] [Google Scholar]
- 22.Mizuguchi T, Kawamoto M, Meguro M, et al. Laparoscopic hepatectomy: a systematic review, meta-analysis,and power analysis. Surg Today. 2011;41:39–47. [DOI] [PubMed] [Google Scholar]
- 23.Viganò L, Tayar C, Laurent A, et al. Laparoscopic liver resection: a systematic review. J Hepatobiliary Pancreat Surg. 2009;16:410–421. [DOI] [PubMed] [Google Scholar]
- 24.Rao A, Rao G, Ahmed I. Laparoscopic or open liver resection? Let systematic review decide it. Am J Surg. 2012;204:222–231. [DOI] [PubMed] [Google Scholar]
- 25.Ratti F, Ferla F, Paganelli M, et al. Biliary cystadenoma: short- and long-term outcome after radical hepatic resection. Updates Surg. 2012;64:13–18. [DOI] [PubMed] [Google Scholar]
- 26.Toro A, Gagner M, Di Carlo I. Has laparoscopy increased surgical indications for benign tumors of the liver? Langenbecks Arch Surg. 2013;398:195–210. [DOI] [PubMed] [Google Scholar]
- 27.Ardito F, Tayar C, Laurent A, et al. Laparoscopic liver resection for benign disease. Arch Surg. 2007;142:1188–1193. [DOI] [PubMed] [Google Scholar]
- 28.Tang CN, Tai CK, Ha JP. Laparoscopy versus open left lateral segmentectomy for recurrent pyogenic cholangitis. Surg Endosc. 2005;19:1232–1236. [DOI] [PubMed] [Google Scholar]
- 29.Tang CN, Li MK. Hand-assisted laparoscopic segmentectomy in recurrent pyogenic cholangitis. Surg Endosc. 2003;17:324–327. [DOI] [PubMed] [Google Scholar]
- 30.Jang JY, Yoon YS, Kang MJ, et al. Laparoscopic excision of a choledochal cyst in 82 consecutive patients. Surg Endosc. 2013;27:1648–1652. [DOI] [PubMed] [Google Scholar]
- 31.Katkhouda N, Hurwitz M, Gugenheim J, et al. Laparoscopic management of benign solid and cystic lesions of the liver. Ann Surg. 1999;229:460–466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wakabayashi G, Cherqui D, Geller DA, et al. Recommendations for laparoscopic liver resection: a report from the second international consensus conference held in Morioka. Ann Surg. 2015;261:619–629. [DOI] [PubMed] [Google Scholar]
- 33.Claus CM, Bonin EA, Torres MF, et al. Liver and peritoneal biopsy by laparoscopy or notes in pigs: comparison of operative parameters and postoperative evolution. Rev Col Bras Cir. 2011;38:253–259. [DOI] [PubMed] [Google Scholar]
- 34.Tagaya N, Kubota K. NOTES: approach to the liver and spleen. J Hepatobiliary Pancreat Surg. 2009;16:283–287. [DOI] [PubMed] [Google Scholar]
- 35.Ohdaira T, Endo K, Abe N, et al. Transintestinal hepatectomy performed by hybrid NOTES using a customized X-TRACT Tissue Morcellator with an electrifiable round cutter. J Hepatobiliary Pancreat Surg. 2009;16:274–282. [DOI] [PubMed] [Google Scholar]
- 36.Phee SJ, Ho KY, Lomanto D, et al. Natural orifice transgastric endoscopic wedge hepatic resection in an experimental model using an intuitively controlled master and slave transluminal endoscopic robot (MASTER). Surg Endosc. 2010;24:2293–2298. [DOI] [PubMed] [Google Scholar]
- 37.Shi H, Jiang SJ, Li B, et al. Natural orifice translumeninal endoscopic wedge hepatic resection with a water-jet hybrid knife in a non-survival porcine model. World J Gastroenterol. 2011;17:926–931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Castro-Pérez R, Dopico-Reyes E, Acosta-González LR. Minilaparoscopic-assisted transvaginal approach in benign liver lesions. Rev Esp Enferm Dig. 2010;102:357–364. [DOI] [PubMed] [Google Scholar]
- 39.Truong T, Arnaoutakis D, Awad ZT. Laparoscopic hybrid NOTES liver resection for metastatic colorectal cancer. Surg Laparosc Endosc Percutan Tech. 2012;22:e5–e7. [DOI] [PubMed] [Google Scholar]
- 40.Noguera JF, Dolz C, Cuadrado A, et al. Transvaginal liver resection (NOTES) combined with minilaparoscopy. Rev Esp Enferm Dig. 2008;100:411–415. [DOI] [PubMed] [Google Scholar]
- 41.Wilson JI, Dogiparthi KK, Hebblethwaite N, et al. Laparoscopic right hemicolectomy with posterior colpotomy for transvaginal specimen retrieval. Colorectal Dis. 2007;9:662. [DOI] [PubMed] [Google Scholar]
- 42.Palanivelu C, Rangarajan M, Jategaonkar PA, et al. An innovative technique for colorectal specimen retrieval: a new era of “natural orifice specimen extraction” (N.O.S.E). Dis Colon Rectum. 2008;51:1120–1124. [DOI] [PubMed] [Google Scholar]
- 43.Choi GS, Park IJ, Kang BM, et al. A novel approach of robotic-assisted anterior resection with transanal of transvaginal retrieval of the specimen for colorectal cancer. Surg Endosc. 2009;23:2831–2835. [DOI] [PubMed] [Google Scholar]
- 44.Franklin ME, Jr, Kelley H, Kelley M, et al. Transvaginal extraction of the specimen after total laparoscopic right hemicolectomy with intracorporeal anastomosis. Surg Laparosc Endosc Percutan Tech. 2008;18:294–298. [DOI] [PubMed] [Google Scholar]
- 45.McKenzie S, Baek JH, Wakabayashi M, et al. Totally laparoscopic right colectomy with transvaginal specimen extraction: the author’s initial institutional experience. Surg Endosc. 2010;24:2048–2052. [DOI] [PubMed] [Google Scholar]
- 46.Tarantino I, Linke GR, Lange J, et al. Transvaginal rigid-hybrid natural orifice transluminal endoscopic surgery technique for anterior resection treatment of diverticulitis: a feasibility study. Surg Endosc. 2011;25:3034–3042. [DOI] [PubMed] [Google Scholar]
- 47.Park JS, Choi GS, Kim HJ, et al. Natural orifice specimen extraction versus conventional laparoscopically assisted right hemicolectomy. Br J Surg. 2011;98:710–715. [DOI] [PubMed] [Google Scholar]
- 48.Diana M, Perretta S, Wall J, et al. Transvaginal specimen extraction in colorectal surgery: current state of the art. Colorectal Dis. 2011;13:e104–e111. [DOI] [PubMed] [Google Scholar]
- 49.Senft JD, Warschkow R, Diener MK, et al. The transvaginal hybrid NOTES versus conventionally assisted laparoscopic sigmoid resection for diverticular disease (TRANSVERSAL) trial: study protocol for a randomized controlled trial. Trials. 2014;15:454 10.1186/1745-6215-15-454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ghezzi F, Raio L, Mueller MD, et al. Vaginal extraction of pelvic masses following operative laparoscopy. Surg Endosc. 2002;16:1691–1696. [DOI] [PubMed] [Google Scholar]
- 51.Horng SG, Huang KG, Lo TS, et al. Bladder injury after LAVH: A prospective, randomized comparison of vaginal and laparoscopic approaches to colpotomy during LAVH. J Am Assoc Gynecol Laparosc. 2004;11:42–46. [DOI] [PubMed] [Google Scholar]
- 52.Teng FY, Muzsnai D, Pérez R, et al. A comparative study of laparoscopy and colpotomy for the removal of ovarian dermoid cysts. Obstet Gynecol. 1996;87:1009–1013. [DOI] [PubMed] [Google Scholar]
- 53.Otsuka Y, Kaneko H, Cleary SP, et al. What is the best technique in parenchymal transection in laparoscopic liver resection? Comprehensive review for the clinical question on the 2nd International Consensus Conference on Laparoscopic Liver Resection. J Hepatobiliary Pancreat Sci. 2015;22:363–370. [DOI] [PubMed] [Google Scholar]
- 54.Kaneko H, Ohtsuka Y, Takagi S, et al. Hepatic resection using stapling devices. Am J Surg. 2004;187:280–284. [DOI] [PubMed] [Google Scholar]


