Abstract
Background:
In this article, we attempt to address a persistent question in the health policy literature: Does more public health spending buy better health? This is a difficult question to answer due to unobserved differences in public health across regions as well as the potential for an endogenous relationship between public health spending and public health outcomes.
Methods:
We take advantage of the unique way in which public health is funded in Georgia to avoid this endogeneity problem, using a twelve year panel dataset of Georgia county public health expenditures and outcomes in order to address the “unobservables” problem.
Results:
We find that increases in public health spending lead to increases in mortality by several different causes, including early deaths and heart disease deaths. We also find that increases in such spending leads to increases in morbidity from heart disease.
Conclusions:
Our results suggest that more public health funding may not always lead to improvements in health outcomes at the county level.
Keywords: public health finance, health outcomes, public policy
Introduction
According to Winslow1 the field of public health is concerned with the prevention of disease, prolonging life, and promoting population health through organized community efforts. These community efforts involve sanitation, the control of communicable diseases, health education, and the organization of medical services for the early diagnosis and preventive treatment of disease. In the United States, public health expenditures are supported through a variety of funding sources and financial arrangements that vary across states and communities.2
A recent focus in the literature on public health financing is on return to investment. In other words, does more public health spending lead to better health outcomes? As is discussed in Mays and Smith,3 there is little credible empirical evidence, regarding the extent to which differences in spending contribute to differences in health. A common approach taken in the literature is to use a cross-section of data for various countries to regress spending on public health outcomes. One issue with such an approach is the unobservables problem. There may be unobservable country-specific characteristics that could bias an estimate of spending on outcomes. For example, a country with a stronger “taste” for public health may spend more and have better outcomes than others. There may also be an important endogeneity problem inherent in such an approach. Countries with poor public health outcomes may be compelled to spend more on public health. Such an allocation system could potentially lead to negative estimated effect of per capita public health spending on public health outcomes. Given these 2 concerns, it may not be surprising that Mays and Smith3 conclude that this literature finds no consistent evidence on the health impact of public health spending. Filmer and Pritchett,4 Rivera,5 and Ghobarah et al6 provide further discussion. Only a handful of recent articles attempt to address these challenging issues, with varying degrees of success.
In this article, we take advantage of the unique way in which public health is funded in the state of Georgia to provide new evidence on the relationship between public health spending and public health outcomes. Using a 12-year panel of county-level data in Georgia, we estimate models that include county and year fixed effects in an attempt to address the unobservables problem. We are able to overcome the endogeneity problem inherent in this literature by exploiting the fact that between 1970 and 2011, Georgia counties were allocated public health general grant-in-aid (GGIA) dollars on the basis of their land value and population as measured in 1970. As long as recent county health outcomes are not strongly tied to these 1970 county characteristics, we can make the case that in our analysis county per capita public health spending (as measured by per capita GGIA dollars) is exogenous to county health outcomes. In addition, we allow for public health spending to influence health outcomes both contemporaneously and with multiple lags.
We find that increases in public health spending lead to increases in mortality by several different causes, including early deaths and heart disease deaths. We also find that increases in such spending leads to increases in morbidity from heart disease. We do not find much evidence of the longer run impacts attenuating or amplifying the short-run impact once we control for the endogeneity of lagged public health spending. Additionally, we stratify Georgia counties by income and find that there does not seem to be major overall differences in terms of statistical significance, though we see that for heart disease mortality and morbidity in particular, the impacts are concentrated in middle-income counties. In terms of magnitude, the estimated contemporaneous impact among high-income counties is smaller than for low- or middle-income counties in a majority of the outcomes. This may imply that low- and middle-income counties respond to increases in public health spending with reductions in private health spending (which would be a form of moral hazard). Another possible explanation is that high-income counties are somehow better able to harness increased public health spending to improve their health outcomes in a way that other counties cannot.
The rest of the article is organized as follows: the second section provides a literature review and the third section some background on public health funding in Georgia. the fourth section describes the Georgia county data used in the analysis, the fifth section describes the methods utilized in this article, and the sixth section discusses our main results. The seventh section offers conclusions and policy implications.
Literature Review
We restrict our attention in this review of the large literature on public health spending impacts to the few articles that have used panel data to attempt to address the endogenous relationship between public health spending and public health outcomes or the challenge associated with unobserved regional characteristics correlated with public health spending or both. We present summaries of each article in order of increasing methodological rigor.
Erwin et al7 use national data from 1993 to 2005 to study the impact of changes in local health department (LHD) expenditures on a broad set of health outcomes that include both measures of morbidity (smoking, infectious disease, and obesity prevalence) and mortality (infant, cardiovascular, and premature deaths). The authors use state fixed effects to address the unobservables problem but do not model lagged public health spending or attempt to address the endogeneity problem mentioned previously in order to produce causal estimates. They find that an increase in LHD expenditures is associated with a statistically significant decline in infectious disease and in years of potential life lost.
Brown8 estimates the causal effect of California county public health department expenditures on all-cause mortality rates. Unlike many other articles in the previous literature, he attempts to explicitly model the lagged effect of public health spending by adopting a Koyck distributed lag model. In addition, he uses a Lewbel instrumental variables (IVs) approach to deal with the endogeneity problem mentioned previously. Using data from 2001 to 2008, he estimates that an extra US$10 per capita of public health spending decreases all-cause mortality by 9.1 deaths per 100 000 and that the long-run effect of public health spending on mortality is stronger than the short-run effect. Brown et al9 use the same data set and a similar approach to estimate the causal impact of public health spending in California on self-reported health and find that a US$10 long-term increase in per capita public health expenditures would increase the percentage of the population reporting good, very good, or excellent health by 0.065 percentage points.
Two other studies also use IV estimation strategies to attempt to causally estimate the impact of public health spending. First, Rajkumar and Swaroop10 examine the impact of the interaction of public health spending and governance quality on health outcomes using a sample of 91 developed and developing countries over 3 years. Rajkumar and Swaroop10 use as instruments dummy variables representing different degrees of “state orientation” among each country in their sample. The authors find that ordinary least square (OLS) estimation without an index of governance showed that a 1 percentage point increase in the share of public health expenditure in a country’s gross domestic product is associated with a 0.18% decline in child mortality. However, when an index of governance is included in the model, the estimated coefficient of public health spending becomes positive and statistically insignificant, thus suggesting no impact of spending. Second, Mays and Smith3 use a similar data set as used in Erwin et al7 and employ an IV estimation strategy to estimate the impact of US local public health spending. Mays and Smith3 use measures of local public health decision-making structures as instruments, including whether the public health agency is governed by a local board of health with policy-making authority and whether the agency operates under the centralized administrative control of their respective state government. They find that mortality rates fell between 1.1% and 6.9% for each 10% increase in local public health spending. Two other studies, Bekemeier et al11 and Grembowski et al,12 unsuccessfully attempt IV estimation.
To summarize, only 3 studies in the literature successfully use an IV approach to estimate the causal impact of public health spending on mortality and 1 estimates the impact on self-reported health status. In terms of mortality, 2 find that increases in public health spending lead to mortality reductions, while the other finds a null result. The final study finds that increases in public health spending lead to increases in self-reported health.
Background on Public Health Funding in Georgia
Administrative Structure Overview
The Georgia Department of Public Health (DPH) is a department of the Georgia state government whose commissioner reports directly to the Governor. The mission of the DPH is to prevent disease, injury, and disability; promote health and well-being; and prepare for and respond to disasters. Responsibility for the provision of public health is shared by the DPH and each of the 159 Georgia counties through their County Boards of Health. In this system with over 6000 employees, County Boards of Health exercise local control, while district- and state-level leadership, coordination, and oversight ensure that statewide public health goals are met. Further background is provided in the following sources: Sweeney,13 Parker,14 and Georgia Office of Planning and Budget (OPB).15
General Grant-in-Aid Overview
General grant-in-aid funds were originally established in the late 1930s to provide Georgia county health departments with the opportunity to address public health priorities based on community-level needs. Consequently, GGIA funds are not earmarked for specific programs or services. In this article, we focus on the allocation of GGIA funds to counties and how this allocation impacts county public health outcomes, such as disease-specific mortality and morbidity rates.
The reason for the focus on GGIA funds (rather than earmarked programmatic GIA funds) is because the allocation of GGIA funds to Georgia counties is not tied to the current health status of the citizens of these counties. According to a program evaluation produced by the Governor’s OPB, a funding formula to allocate GGIA dollars to individual Georgia counties was developed in 1966 and first used in 1967. This formula is as follows:
| 1 |
where Tax base share = (County Pop2/Gross Digest)/(Σ County Pop2/Σ Gross Digest); and County Population share = (County Population/State Population).
Thus, GGIA receipt was based on county population and relative wealth. This formula was never completely successful in dealing with issues relating to population growth and disparities relating to county wealth, so 1970 was the last year in which county characteristics served as an input into this funding formula. The decision was made to freeze the proportion of funding going to each county at the 1970 level, subject to some minor year to year modifications.
In other words, if a county had population and relative wealth such that they received 4% of the total state allotment of GGIA dollars in 1970, then they would continue to receive 4% in the future, regardless of any changes in county population or relative wealth. Although the percentage of GGIA dollars going to each county remains constant, the total number of GGIA dollars going to each county varies from year to year, depending on the total state allotment of GGIA dollars. Table 1 lists the total state allotment of GGIA dollars for fiscal years 2000 to 2011 in the first row. The funding formula was finally updated in fiscal year 2012. For this reason, our analysis does not include any post-2011 data.
Table 1.
Descriptive Statistics for Georgia Counties.a
| 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Georgia General grant-in-aid nominal dollars 2000-2011 (in millions) | 70 | 74 | 74 | 71 | 67 | 64 | 64 | 66 | 72 | 80 | 61 | 66 |
| Health outcomes—mortality | ||||||||||||
| # Infant deaths per 1000 | 0.14 | 0.14 | 0.13 | 0.14 | 0.14 | 0.14 | 0.14 | 0.12 | 0.12 | 0.11 | 0.09 | 0.09 |
| # Early deaths (age ≤ 44) per 1000 | 0.79 | 0.80 | 0.81 | 0.82 | 0.78 | 0.72 | 0.71 | 0.90 | 0.80 | 0.78 | 0.72 | 0.69 |
| # Heart disease deaths per 1000 | n/a | 2.74 | 2.76 | 2.66 | 2.54 | 2.42 | 2.37 | 2.32 | n/a | n/a | n/a | n/a |
| # Cancer deaths per 1000 | 2.04 | 2.02 | 2.06 | 2.08 | 2.05 | 2.01 | 1.93 | 2.02 | 1.98 | 2.03 | 1.95 | 2.04 |
| # Diabetes deaths per 1000 | 0.26 | 0.23 | 0.24 | 0.27 | 0.26 | 0.28 | 0.24 | 0.24 | 0.24 | 0.24 | 0.27 | 0.32 |
| # Asthma deaths per 1000 | 0.02 | 0.02 | 0.02 | 0.02 | 0.02 | 0.01 | 0.01 | 0.01 | 0.01 | 0.01 | 0.02 | 0.01 |
| Health outcomes—morbidity | ||||||||||||
| # Cancer cases per 1000 | 2.75 | 3.03 | 2.98 | 2.90 | 2.90 | 2.81 | 2.84 | 2.84 | 2.82 | 2.69 | 2.53 | 2.55 |
| # Heart disease cases per 1000 | 15.18 | 16.39 | 16.34 | 16.12 | 16.18 | 15.84 | 15.54 | 15.21 | 14.88 | 13.99 | 13.84 | 13.50 |
| # Diabetic cases per 1000 | 1.55 | 1.69 | 1.69 | 1.69 | 1.73 | 1.68 | 1.68 | 1.65 | 1.63 | 1.62 | 1.63 | 1.67 |
| # Asthma cases per 1000 | 1.33 | 1.58 | 1.69 | 1.70 | 1.56 | 1.73 | 1.46 | 1.39 | 1.33 | 1.36 | 1.26 | 1.14 |
| Explanatory variables | ||||||||||||
| General grant-in-aid PC (real 2009 $) | 14.37 | 14.70 | 14.37 | 13.41 | 12.18 | 11.23 | 10.81 | 10.63 | 11.29 | 12.40 | 9.34 | 9.92 |
| Income PC (real 2009 $, unit: US$ 1000) | 26.31 | 26.60 | 26.33 | 26.37 | 26.47 | 26.73 | 26.88 | 27.02 | 28.77 | 28.58 | 28.10 | 28.78 |
| County unemployment rate, % | 4.23 | 4.85 | 5.24 | 5.11 | 5.07 | 5.53 | 4.91 | 5.12 | 6.94 | 10.65 | 11.10 | 10.82 |
| # MDs per 1000 | 1.10 | 1.11 | 1.13 | 1.15 | 1.16 | 1.17 | 1.19 | 1.17 | 1.17 | 1.16 | 1.15 | 1.15 |
| # African American residents PC | 0.35 | 0.35 | 0.36 | 0.36 | 0.36 | 0.36 | 0.36 | 0.36 | 0.36 | 0.36 | 0.36 | 0.36 |
| # Residents of Hispanic ethnicity PC | 0.05 | 0.05 | 0.05 | 0.05 | 0.06 | 0.06 | 0.06 | 0.07 | 0.07 | 0.07 | 0.07 | 0.07 |
| # Aged 18-24 PC | 0.11 | 0.11 | 0.12 | 0.11 | 0.11 | 0.11 | 0.11 | 0.11 | 0.11 | 0.11 | 0.11 | 0.11 |
| # Aged 25-34 PC | 0.17 | 0.16 | 0.16 | 0.16 | 0.15 | 0.15 | 0.15 | 0.15 | 0.15 | 0.15 | 0.15 | 0.15 |
| # Aged 35-44 PC | 0.18 | 0.18 | 0.18 | 0.17 | 0.17 | 0.17 | 0.17 | 0.16 | 0.16 | 0.16 | 0.15 | 0.15 |
| # Aged 45-54 PC | 0.15 | 0.15 | 0.16 | 0.16 | 0.16 | 0.16 | 0.16 | 0.16 | 0.16 | 0.16 | 0.16 | 0.16 |
| # Aged 55-64 PC | 0.10 | 0.10 | 0.11 | 0.11 | 0.12 | 0.12 | 0.13 | 0.13 | 0.13 | 0.14 | 0.14 | 0.14 |
| # Aged 65+ PC | 0.13 | 0.13 | 0.13 | 0.13 | 0.13 | 0.13 | 0.14 | 0.14 | 0.14 | 0.15 | 0.15 | 0.15 |
Abbreviations: MD, medical doctor; PC, per capita.
aCounts of infant deaths, early deaths, cancer deaths, diabetes deaths, asthma deaths, racial/ethnic groups, and age groups come from OASIS, the Online Analytical Statistical Information System (http://oasis.state.ga.us/index.asp). Counts of cancer, heart disease, diabetes, and asthma cases come from OASIS as well. Counts of heart disease deaths and county income come from the Georgia County Guide (http://www.georgiastats.uga.edu/oldsets.html). General grant-in-aid dollars come from author calculations based on total general grant-in-aid dollars allocated in each year by the state from the Georgia Department of Community Health.15 The county unemployment rate data come from the Bureau of Labor Statistics (http://www.bls.gov/). The number of physicians in each county comes from the Area Resource File (http://arf.hrsa.gov/).
Data
Data from each of Georgia’s 159 counties were compiled for 12 years (2000-2011) from 2 main sources. Our primary data source is the Georgia Department of Community Health’s Online Analytical Statistical Information System (OASIS).16 The OASIS is a suite of interactive tools used to access Georgia’s standardized health data repository. It includes multiple county-level measures of morbidity and mortality. Our second data source is the Georgia County Guide (GCC), various annual editions. The GCC is a reference source for researchers and policy makers in need of agricultural, economic, and demographic data for the state. Finally, unemployment rate data were taken from the Bureau of Labor Statistics Web site, and other supplemental data were taken from the Area Resource File.
Table 1 also presents descriptive statistics for the Georgia counties in each of the 12 years. As in Mays and Smith,3 we selected mortality outcome measures that were routinely collected, available at the county level, and were expected to potentially be sensitive to public health expenditures. Several of the mortality measures show improvement between 2000 and 2011, with reductions in the number of infant deaths, early deaths, and heart disease deaths per 1000 residents. In addition to the mortality measures, we also analyzed a set of morbidity measures (the number of cancer, heart disease, asthma, and diabetes cases per 1000 residents). We also see decreases in most of these morbidity measures over time.
The key independent variable in our analysis is the level of GGIA dollars (measured in 2009 dollars) allocated to each county according to the funding formula described previously. Table 1 shows that the average amount allocated to a county fell from just over US$14 per person in 2000 to just under US$10 per person in 2011. One concern associated with working our time series data is the presence of unit roots that would lead to spurious correlations between public health spending and health outcomes. In order to test for this, we applied the standard Harris-Tsavalis panel data unit root test for each of our health outcomes and our measure of health spending. We were able to strongly reject the null hypothesis of a unit root in favor of the alternative that all of our health outcome variables and our health spending variable are stationary.
In order to isolate the impact of the GGIA dollars, we also control for changes in real per capita income at the county level, the county unemployment rate, the number of physicians per capita, the county age distribution, and the county racial/ethnic distribution. As will be described in more detail subsequently, we exploit the panel nature of the data to include a full set of county and year fixed effects. These fixed effects will control for time-invariant, county-level unobserved characteristics as well as general temporal trends over the 2000 to 2011 time period.
Methods
As discussed in Erwin et al,7 the literature on the impact of public health spending on health outcomes has primarily relied on cross-sectional or pooled panel data to estimate associations rather than a causal relationship. Equation 2 represents such a regression model, where y represents a typical public health outcome measured at the county level, i is an index of counties, t is an index of time periods, x represents county i public health expenditure at time t, z represents a vector of contemporaneous control variables, such as county income, and u is the error term.
| 2 |
There are multiple issues with such an approach. First, such an approach doesn’t take advantage of the panel nature of the data to include county or time fixed effects, which would control for general temporal trends or unobservable time-invariant county factors that could influence public health outcomes, such as a county’s underlying “taste” for public health. A regression model with time and county fixed effects is given in Equation 3.
| 3 |
Even after including controls for such fixed effects, a second issue still remains. Both Equations 2 and 3 restrict the impact of public health spending on health outcomes to occur contemporaneously. It seems intuitive that current public health spending would have both an immediate and a longer term impact on health outcomes. A final issue involves the potential endogeneity of public health spending. As discussed in the literature review, few previous studies have attempted to address all of these issues.
In order to address all of these issues, in this article, we have built a long panel data set on county public health spending and health outcomes in Georgia and use that to estimate the Koyck distributed-lag model given in equation 4. Gujarati and Porter17 provide more information on this model and, in fact, include as an end of the chapter exercise (Chapter 17, number 5) in their chapter on dynamic econometric models.
| 4 |
where
The big change here relative to Equation 2 or 3 is the inclusion of multiple lags of public health spending (xi). Further, λ denotes the change rate of the distributed lag of public health spending. One benefit of the Koyck distributed lag model is that the data determine the weight (λ) each lag receives in predicting outcomes. Public health spending would only impact public health outcomes contemporaneously if λ = 0, which almost all of the previous literature implicitly assumes. Brown8 and Brown et al9 impose the assumption that λ is positive, which implies that the long-run effect of public health spending always amplifies the short-run effect. We do not impose such an assumption in our analysis, as we allow for the possibility that λ could be negative. This would imply that the long-run effect of public health spending could attenuate the short-run effect.
Under what circumstances could the long-run effect of public health spending attenuate the short-run effect? Suppose an increase in today’s public health spending improves today’s health outcomes, but it also leads to the perhaps unintended consequence of crowding out future private health care spending. This crowd out could potentially attenuate the long-run effect of this public health spending increase. One could think of this as a type of moral hazard problem that we will discuss further subsequently.
In order to derive the regression model, we estimate in this article, we first take Equation 4 and lag it by 1 period. This 1-period lagged model is given in Equation 5:
| 5 |
Next we multiply Equation 5 by λ and subtract this from Equation 4. This gives us Equation 6:
| 6 |
where and .
Here the short-run impact of public health spending (SR) is given by , and, if −1 < λ < 1, the long-run impact of public health spending (LR) is given by , where since Finally, we include a vector z of additional control variables (county income, unemployment rate, and number of physicians per capita), a vector τ of year fixed effects and a vector C of county fixed effects to arrive at Equation 7.
| 7 |
There are 2 sources on endogeneity that could bias estimates of this model. First, it may be the case that public health outcomes may factor into the determination of public health budgets in a given county. For example, a state may provide counties with the worst health outcomes more public health dollars than counties with the best health outcomes. Second, there is a mechanical source of endogeneity inherent in all distributed-lag models due to the relationship between the error term and the lagged dependent variable. This can be formally expressed as follows:
| 8 |
Brown8 and Brown et al9 use the Lewbel IVs approach to addresses these endogeneity problems. This approach is used when standard instruments are weak or not available.18 In our article, we exploit the fact that Georgia counties are allocated GGIA dollars on the basis of their land value and population from the early 1970s. As long as current county health outcomes are not strongly tied to these county characteristics from the early 1970s, we can make the case that in our analysis, county per capita public health spending (as measured by per capita GGIA dollars) is exogenous to county health outcomes. Therefore, we can use a standard 2-stage least squares (2SLSs) estimation approach, with the predicted value of a 1-period lag of our dependent variable serving as our instrument. Gujarati and Porter17 describe how to implement 2SLSs with exogenous independent variables in distributed lag models. First, we regress on and using OLS and get predicted value of , . Next, we replace with in Equation 7, giving us Equation 9, which we then estimate using OLS.
| 9 |
where .
In this equation, we sort and cluster our data by county. Therefore, standard errors will be robust to heteroskedasticity and serial correlation.
Results
We start this section with a description of our primary results in which we estimate 4 different specifications. The first represents the standard cross-sectional approach taken in the literature. Next we add county and time fixed effects and then add lagged expenditures to the model. Finally, we employ a 2SLSs approach to address the inherent endogeneity associated with including lagged spending in the model. Following a discussion of these primary results, we then stratify the sample by county income to test for heterogeneous impacts of public health spending.
Primary Results
Table 2 shows the results for 4 different regressions estimating the impact of public health spending on each of 10 different mortality and morbidity outcomes, using 12 years of county-level data in Georgia. The first column represents estimates of Equation 2, which mimics most of the literature in that it doesn’t include county or year fixed effects and doesn’t allow for public health spending to have a lagged effect on health outcomes. The coefficient estimates suggest a statistically significant and positive relationship between local public health expenditures and almost all the health outcomes being considered. For example, this model predicts that a US$1000 increase in contemporaneous real GGIA per capita leads to an increase of 0.006 early deaths per capita or 6 early deaths per 1000 county residents. These results are perhaps counterintuitive in that we would expect more public health spending to lead to better health outcomes. One could potentially explain this finding if Georgia allocated more public health funding to counties with worse health outcomes, but as we discussed, Georgia has a unique system for allocating its GGIA funds to county health departments that is arguable independent of current health outcomes in each county.
Table 2.
Regressions of OLS, OLS With FE, OLS With FE and Lags, and 2SLS.a
| Impact of an Extra US$1000 GGIA PC on | (1) OLS | (2) OLS With FE | (3) OLS With FE and Lags | (4) Two Stage Least Squares | ||
|---|---|---|---|---|---|---|
| β0 | β0 | β0 | λ | β0 | λ | |
| (SE) | (SE) | (SE) | (SE) | (SE) | (SE) | |
| Infant deaths PC | 0.0017b | 0.0049 | 0.0067 | −0.1285b | 0.0077 | −0.4582 |
| (0.0004) | (0.0043) | (0.0052) | (0.0345) | (0.0054) | (0.3871) | |
| Early deaths PC | 0.0056b | 0.0150c | 0.0231b | −0.0942b | 0.0263b | −0.2949 |
| (0.0012) | (0.0079) | (0.0082) | (0.0206) | (0.0084) | (0.2903) | |
| Heart disease deaths PC | 0.0179b | 0.0904d | 0.1122d | −0.1104b | 0.1315b | −0.5171b |
| (0.0038) | (0.0381) | (0.0443) | (0.0265) | (0.0352) | (0.1283) | |
| cancer deaths PC | 0.0138b | 0.0231 | 0.0260 | −0.0274 | 0.0326 | −0.3912 |
| (0.0021) | (0.0273) | (0.0305) | (0.0368) | (0.0292) | (0.2555) | |
| Diabetes deaths PC | 0.0042b | 0.0068 | 0.0047 | −0.0827 | 0.0065 | −0.5063 |
| (0.0008) | (0.0099) | (0.0108) | (0.0577) | (0.0108) | (0.2976) | |
| Asthma deaths PC | 0.0010b | 0.0012 | 0.0015 | −0.1086b | 0.0017 | −0.7131c |
| (0.0002) | (0.0018) | (0.0019) | (0.0350) | (0.0018) | (0.4101) | |
| Cancer PC | 0.0043 | 0.0181 | 0.0316 | 0.0193 | 0.0353 | −0.2770 |
| (0.0035) | (0.0266) | (0.0272) | (0.0303) | (0.0259) | (0.3689) | |
| Heart disease PC | −0.0827b | 0.3768b | 0.3251b | 0.3586b | 0.3928b | 0.1292 |
| (0.0204) | (0.0779) | (0.0603) | (0.0373) | (0.0953) | (0.1827) | |
| Diabetes PC | 0.0001 | 0.0120 | 0.0120 | 0.1720b | 0.0145 | −0.1361 |
| (0.0027) | (0.0244) | (0.0228) | (0.0545) | (0.0251) | (0.2783) | |
| Asthma PC | −0.0045 | 0.0251 | 0.0375c | 0.2125b | 0.0321 | 0.2621 |
| (0.0036) | (0.0178) | (0.0198) | (0.0383) | (0.0224) | (0.1967) | |
| County FE | No | Yes | Yes | Yes | ||
| Year FE | No | Yes | Yes | Yes | ||
| Lags | No | No | Yes | Yes | ||
| IV | No | No | No | Yes | ||
Abbreviations: FE, fixed effect; GGIA, general grant-in-aid; OLS, ordinary least square; PC, per capita; SE, standard error; 2SLS, 2-stage least square.
aThe data used in this analysis come from Georgia’s 159 counties from 2000 to 2011 (N = 159, T = 12). This represents a sample size of 1908 county-years. Standard errors, clustered by county, are in parentheses. Income per capita, number of medical doctors per 1000, age and racial/ethnic distributions, and unemployment rates are included in each model. The impact of an extra US$1000 GGIA PC on health outcomes is estimated and dollar figures are adjusted for inflation and expressed in constant 2009 dollars. For full results, see http://www2.gsu.edu/˜ecojhm/public_health.html.
bStatistical significance at the 1% level.
cStatistical significance at the 10% level.
dStatistical significance at the 5% level.
Given that unobserved, time-invariant county characteristics or general temporal trends could be driving this result, column 2 reports estimates of Equation 3, which extends the previous model by including county and year fixed effects. The inclusion of these fixed effects in many cases increases the estimated impact of public health spending on our outcomes of interest. The same US$1000 increase in contemporaneous real GGIA per capita is now estimated to lead to an increase in 0.015 early deaths per capita or 15 early deaths per 1000 county residents.
One potential explanation could be that some counties have a stronger “taste” for health than others and estimates of Equation 3 control for that, while estimates of Equation 2 do not. In other words, if we don’t control for a county’s taste for health, it appears as though the hypothetical increase in public health spending leads to 6 additional early deaths per 1000. This is an aggregate of the “pure” negative impact of public health spending on health and the positive impact of the county’s preference for health and general temporal trends. When we control for county health preferences and general temporal trends in Equation 3, we isolate the “pure” impact of public health spending, which is predicted to lead to 15 early deaths per 1000.
As mentioned, few previous studies allow for lagged impacts of public health spending or attempt to address the potential endogeneity of such spending. Column 3 of Table 2 addresses the first issue by presenting the results of estimates of Equation 7, which allows public health spending to have a lagged impact. The left side of column 3 reports estimates of β0, which gives the current or “short-run” impact of public health spending, while the right side reports estimates of λ, which represents the “long run” influence of public health spending over and above the short-run impact. In general, one can think of the contemporaneous effect given in column 2 as the aggregate of the short- and long-run effects reported in column 3. Continuing our discussion of early deaths, column 3 suggests that the short-run impact of a US$1000 per capita increase in public health spending leads to an additional 23 early deaths per 1000 in the short run. The negative estimated value of λ associated with early deaths suggests an attenuation of this short-run effect in the long run. The long-run impact is estimated to be (0.0231)/(1 – −0.0942) = 0.02111 or 21 additional early deaths per 1000.
Although we argued previously that contemporaneous public health spending in Georgia is arguably independent of contemporaneous county health status, and thus exogenous, the inclusion of lagged public health spending in the model presented in column 3 creates a new endogeneity problem because . In other words, the stochastic explanatory variable representing lagged spending (yit-1) is correlated with the error term (vit) in Equation 7 by definition. This implies that estimates of Equation 7 reported in column 3 of Table 2 are biased since we do not address this issue in that specification.
In order to address this particular endogeneity problem, we adopt 2SLSs approach as described in Equation 9 and present the results in column 4 of Table 2. According to column 4, addressing the endogeneity of lagged public health spending leads to short-run coefficient estimates that are mostly somewhat larger in magnitude than those reported in column 3. In addition, the estimates of λ are mostly negative and typically not statistically significant. Thus, correcting for the endogeneity of lagged spending implies the potential for some attenuation but in most cases no statistically significant difference between the short-run and long-run impact of public health spending for many of the health outcomes we consider.
There are a few possible explanations for our perhaps somewhat counterintuitive finding of an adverse effect of public health spending on health outcomes. First, an increase in public health spending could lead to a moral hazard effect in which private health spending is crowded out. Such crowd out could potentially lead to reductions in health status. In Figure 1, we compare annual trends in Pap smear tests and mammograms to total state GGIA spending in Georgia between 2000 and 2011. This figure illustrates that when GGIA spending is high the number of Pap smear tests is lower than when GGIA spending is low. This descriptive evidence is suggestive of GGIA spending potentially crowding out this type of preventive private health spending to some degree. Such a relationship is less clear for mammograms though, as GGIA spending increases between 2006 and 2009, we see a slight contemporaneous reduction in mammograms.
Figure 1.
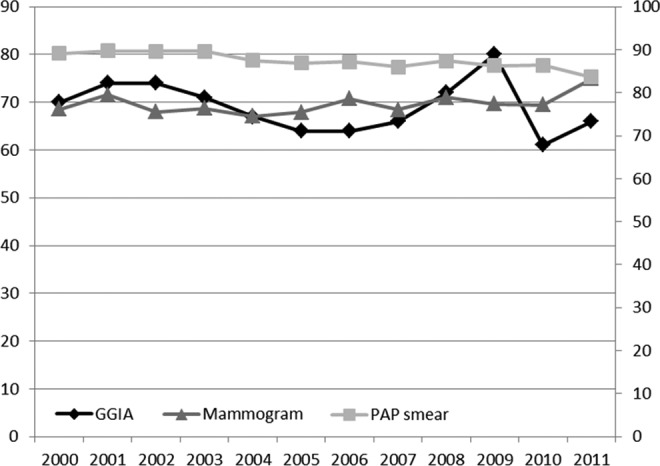
Georgia public health general grant-in-aid spending and prevention activities. Counts of mammograms and PAP smears come from OASIS, the Online Analytical Statistical Information System (http://oasis.state.ga.us/index.asp). General grant-in-aid dollars come from author calculations based on total general grant-in-aid dollars allocated in each year by the state from the Georgia Department of Community Health.15
In a somewhat related example from a different literature, Dave and Kaestner19 investigate the ex-ante moral hazard effect of gaining Medicare coverage and estimate that Medicare coverage leads to reductions in exercise and increases in smoking and drinking among the elderly patients. Another possible explanation found in Rajkumar and Swaroop10 is that inefficient administration of public health dollars could also lead to a failure to improve health. Our results suggest the potential for a negative impact of public health funding.
Although the unique institutional structure regarding the allocation of GGIA in Georgia mitigates concerns about reverse causality, we also employ the Lewbel IV approach with our data as a robustness check. Our motivation for this approach comes from Brown8 and Brown et al,9 2 articles interested in estimating the causal impact of county public health expenditures in California. As mentioned, these articles employ the Lewbel18 IV approach because reverse causality is a major issue in any analysis of California public health spending, as counties with worse health outcomes are explicitly allocated more public health funding. In our case, if reverse causality was driving our results, we would expect the Lewbel IV coefficient estimates to differ widely from our 2SLS coefficient estimates. In fact, they are quite similar (results available upon request). This gives us additional confidence that our results are not being driven by reverse causality or some sort of model misspecification issue in our 2SLSs approach.
Stratification by County Income
In order to investigate whether or not public health spending has differential impacts on counties with different income levels, we follow Bekemeier et al11 and classify Georgia counties into 3 categories based on income. Low-income counties represent those with the lowest, 20% of county income, and high-income counties represent those with the highest, 20% of county income. Middle-income counties represent all others. Table 3 gives the stratified results based on Equation 9, using 2SLSs to account for the endogeneity of lagged public health spending.
Table 3.
Two Stage Least Squares Regressions Stratified by Income.a
| Two Stage Least Squares | Low-Income Counties | Middle-Income Counties | High-Income Counties | |||
|---|---|---|---|---|---|---|
| β0 | λ | β0 | λ | β0 | λ | |
| (SE) | (SE) | (SE) | (SE) | (SE) | (SE) | |
| Infant deaths PC | 0.0251b | −1.5971c | 0.0009 | −0.8420b | 0.0077 | −0.1788 |
| (0.0106) | (0.5581) | (0.0093) | (0.3255) | (0.0062) | (0.3651) | |
| Early deaths PC | 0.0366 | −0.1818 | 0.0218 | −0.3758 | 0.0211 | −0.6339 |
| (0.0267) | (0.5693) | (0.0171) | (0.2585) | (0.0234) | (0.3816) | |
| Heart disease deaths PC | −0.0205 | 0.1109 | 0.0764b | −0.3458c | 0.0986 | −0.2931 |
| (0.0730) | (0.3146) | (0.0365) | (0.1226) | (0.0683) | (0.3066) | |
| Cancer deaths PC | −0.0011 | 0.6634 | 0.0421 | −0.5703c | −0.0181 | 0.1301 |
| (0.0503) | (0.4039) | (0.0502) | (0.1481) | (0.0429) | (0.5442) | |
| Diabetes deaths PC | 0.0159 | −0.6951d | 0.0044 | 0.0415 | 0.0031 | −0.5459d |
| (0.0143) | (0.3703) | (0.0167) | (0.2949) | (0.0114) | (0.3097) | |
| Asthma deaths PC | 0.0043 | −0.1377 | −0.0031 | −1.6468d | 0.0026 | −1.3495b |
| (0.0026) | (0.1842) | (0.0031) | (0.9494) | (0.0030) | (0.5834) | |
| Cancer PC | 0.0452 | 0.8303d | −0.0119 | −0.4864d | 0.0954d | −0.7930 |
| (0.0721) | (0.4249) | (0.0271) | (0.2887) | (0.0568) | (0.5328) | |
| Heart disease PC | 0.2215 | 0.3233d | 0.4989c | −0.1204 | 0.0880 | 0.2569 |
| (0.1982) | (0.1772) | (0.1584) | (0.1661) | (0.1588) | (0.3983) | |
| Diabetes PC | 0.0014 | −0.3853 | 0.0255 | −0.2392 | −0.0162 | −0.1510 |
| (0.0396) | (0.2741) | (0.0337) | (0.2483) | (0.0365) | (0.2619) | |
| Asthma PC | 0.0201 | 0.5048 | 0.0281 | 0.1193 | 0.0181 | 0.3274 |
| (0.0627) | (0.4818) | (0.0232) | (0.2171) | (0.0365) | (0.4777) | |
Abbreviations: FE, fixed effect; GGIA, general grant-in-aid; SE, standard error.
aThe data used in this analysis come from Georgia’s 159 counties from 2000 to 2011 (N = 159, T = 12). This represents a sample size of 1908 county-years. Standard errors, clustered by county, are in parentheses. Income per capita, number of medical doctors per 1000, age and racial/ethnic distributions, and unemployment rates are included in each model. The impact of an extra US$1000 GGIA PC on health outcomes is estimated, and dollar figures are adjusted for inflation and expressed in constant 2009 dollars. All specifications in this table include county and year fixed effects as well as lagged values of public health spending. For full results, see http://www2.gsu.edu/˜ecojhm/public_health.html.
bStatistical significance at the 5% level.
cStatistical significance at the 1% level.
dStatistical significance at the 10% level.
Overall, there does not seem to be major differences in terms of statistical significance, though we see that for heart disease mortality and morbidity in particular, the impacts are concentrated in middle-income counties. In terms of magnitude, the estimated contemporaneous impact among high-income counties is smaller than for low- or middle-income counties in a majority of the outcomes.
A second result of this stratification exercise is that the handful of negative short-run coefficient estimates within each county income category fits more neatly with the conventional wisdom that increases in public health spending lead to improvements in health. These coefficient estimates are not statistically significant, though this could be due in part to sample size limitations.
Conclusion
This article contributes to the literature on the health impacts of public health spending by combining the unique way in which GGIA dollars are allocated to county health departments in Georgia with an empirical strategy that addresses important modeling issues ignored in most of the previous literature. As mentioned, only 3 previous studies have successfully used an IVs approach to estimate the causal impact of public health spending on mortality. One uses data from California,8 another from all United States,3 and the third is a cross-country comparison.10
Unlike much of the previous literature, we find that in Georgia increases in public health spending lead to increases in mortality by several different causes, including early deaths and heart disease deaths. We also find that increases in such spending leads to increases in morbidity associated with heart disease. Although we allow for differences between the short-run and the long-run impact of such spending, we do not find much evidence of the longer run impacts attenuating or amplifying the short-run impact once we control for the endogeneity of lagged public health spending.
Given the unique way in which GGIA dollars are allocated to county health departments in Georgia, we are not concerned that our results are being caused by counties with worse health outcomes getting more GGIA dollars. It is rare to find a naturally occurring situation in which current public health dollars are allocated through a mechanism that is plausibly independent of current health outcomes. That being said, the benefit that comes from exploiting this unique situation comes at the potential cost of external validity. For example, we would not necessarily expect the same results from public health funding streams that were earmarked for specific services (ie, programmatic grant-in-aid), such as HIV prevention.
This suggests the need for more rigorous studies of the impact of public health spending that use data on different types of public health funding mechanisms (such as programmatic grant-in-aid) from other data sources and/or other states. In addition, more work needs to better understand the mechanisms or pathways through which public health spending impacts health outcomes. The fact that our impact estimates conflict with some of the previous literature highlights the need for these additional studies. A final avenue for future research would be to attempt to measure health outcomes at a finer level of geography than at county level, which may mask important within-county heterogeneity in health outcomes. The OASIS Web site documents any measurement issues associated with their mortality and morbidity counts (https://oasis.state.ga.us/oasis/oasis/help/DischargeDataReportingIssues.html).
Acknowledgments
We would like to thank Subha Basu, Patrick Henson, Austin LeVert, Xinxin Lu, Michael Sikivie, and Jamie Turner for their work as research assistants.
Author Biographies
James Marton is an associate professor in the Department of Economics, Andrew Young School of Policy Studies, Georgia State University.
Jaesang Sung is a PhD student in the Department of Economics, Andrew Young School of Policy Studies, Georgia State University.
Peggy Honore’ is the AmeriHealth Mercy Endowed Professor at Louisiana State University Health Sciences Center School of Public Health in New Orleans.
Footnotes
Authors’ Note: The authors are responsible for any errors.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Winslow CEA. The untilled field of public health. Mod Med. 1920;2:183–191. [Google Scholar]
- 2. Bernet PM. Local public health agency funding: money begets money. J Public Health Manag Pract. 2007;13(2):188–193. [DOI] [PubMed] [Google Scholar]
- 3. Mays GP, Smith SA. Evidence links increases in public health spending to declines in preventable deaths. Health Aff. 2011;30(8):1585–1593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Filmer D, Pritchett L. The impact of public spending on health: does money matter? Soc Sci Med. 1999;49(10):1309–1323. [DOI] [PubMed] [Google Scholar]
- 5. Rivera B. The effects of public health spending on self-assessed health status: an ordered probit model. Appl Econ. 2001;33(10):1313–1319. [Google Scholar]
- 6. Ghobarah HA, Huth P, Russett B. Comparative public health: the political economy of human misery and well-being. Int Stud Q. 2004;48(1):73–94. [Google Scholar]
- 7. Erwin PC, Mays GP, Riley WJ. Resources that may matter: the impact of local health department expenditures on health status. Public Health Rep. 2012;127(1):89–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Brown TT. How effective are public health departments at preventing mortality? Econ Hum Biol. 2014;13:34–45. [DOI] [PubMed] [Google Scholar]
- 9. Brown TT, Martinez-Gutierrez MS, Navab B. The impact of changes in county public health expenditures on general health in the population. Health Econ Policy Law. 2014;9(3):251–269. [DOI] [PubMed] [Google Scholar]
- 10. Rajkumar AS, Swaroop V. Public spending and outcomes: does governance matter? J Dev Econ. 2008;86(1):96–111. [Google Scholar]
- 11. Bekemeier B, Yang Y, Dunbar M, Pantazis A, Grembowski D. Targeted health department expenditures benefit birth outcomes at the county level. Am J Prev Med. 2014;46(6):569–577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Grembowski D, Bekemeier B, Conrad D, Kreuter W. Are local health department expenditures related to racial disparities in mortality? Soc Sci Med. 2010;71(12):2057–2065. [DOI] [PubMed] [Google Scholar]
- 13. Sweeney T. Overview of Georgia’s Public Health Budget & Activities. Georgia Budget & Policy Institute, Atlanta, GA; 2009. [Google Scholar]
- 14. Parker C. Funding formula use in Georgia’s public health system: setting the context. Georgia Health Policy Center Working Paper; 2009. [Google Scholar]
- 15. Georgia Office of Planning and Budget. Division of Public Health: Governance and General Grant-in-Aid; 2008. Available at: http://opb.georgia.gov/sites/opb.georgia.gov/files/imported/vgn/images/portal/cit_1210/58/6/162698053public_health_evaluation_4-25-08.pdf. Accessed March 7, 2015.
- 16. Georgia Department of Community Health, Division of Public Health, Office of Health Information and Policy. Web site http://oasis.state.ga.us/. Accessed March 7, 2015.
- 17. Gujarati DN, Porter DC. Basic Econometrics. 5th ed NY: The McGraw-Hill Companies, Inc; 2009. [Google Scholar]
- 18. Lewbel A. Using heteroscedasticity to identify and estimate mismeasured and endogenous regressor models. J Business Econ Stat. 2012;30(1):67–80. [Google Scholar]
- 19. Dave D, Kaestner R. Health insurance and ex ante moral hazard: evidence from Medicare. Int J Health Care Finance Econ. 2009;9(4):367–390. [DOI] [PubMed] [Google Scholar]


