Abstract
Insights into the pathogenesis of inflammatory bowel diseases (IBD) have provided important information for the development of therapeutics. Levels of interleukin 23 (IL23) and T-helper (Th) 17 cell pathway molecules are elevated in inflamed intestinal tissues of patients with IBD. Loss of function variants of the interleukin 23 receptor gene (IL23R) protect against IBD, and in animals, blocking IL23 reduces severity of colitis. These findings indicated that the IL23 and Th17 cell pathways might be promising targets for treatment of IBD. Clinical trials have investigated the effects of agents designed to target distinct levels of the IL23 and Th17 cell pathways, and the results are providing insights into IBD pathogenesis and additional strategies for modulating these pathways. Strategies to reduce levels of proinflammatory cytokines more broadly and increase anti-inflammatory mechanisms are also emerging for treatment of IBD. The results from trials targeting these immune system pathways have provided important lessons for future trials. Findings indicate the importance of improving approaches to integrate patient features and biomarkers of response with selection of therapeutics.
Keywords: Crohn’s disease, ulcerative colitis, therapy, intestine
The intestinal lamina propria contains a complex population of immune cells that balance the need to maintain tolerance to the luminal microbiota with the need for protection against pathogens or entry of excessive resident microbes. Inflammatory bowel diseases (IBD) are characterized by expansion and/or infiltration of intestinal tissues with innate and adaptive inflammatory cells, including neutrophils, macrophages, dendritic cells, natural killer T cells, innate lymphoid cells (ILCs), and B and T cells. Increased numbers and activation of these cells increase levels of cytokines in the intestinal mucosa, such as tumor necrosis factor (TNF), interferon gamma (IFNγ), interleukin 1 beta (IL1β), IL6, and IL23, as well as T-helper (Th) 17 cell pathway cytokines. An overall imbalance between proinflammatory and anti-inflammatory cytokines promotes the inflammatory process observed in patients with IBD.
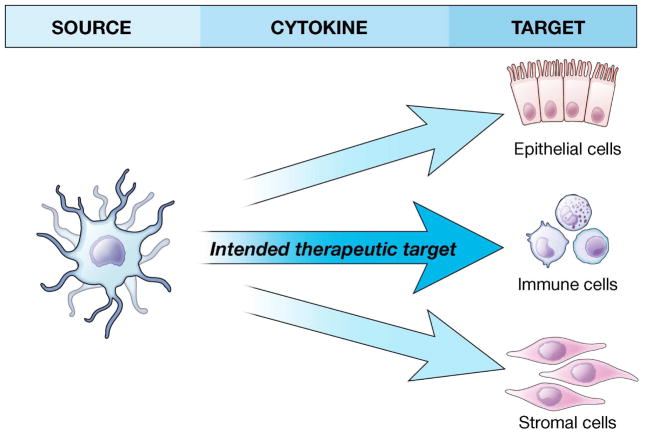
Many strategies have been developed to alter levels of cytokines for treatment of IBD; antagonists of TNF provide a prototype for this approach. However, only one-third of patients treated with TNF-antagonists remain in clinical remission after 1 year of therapy, and the off-target effects of TNF-antagonists can produce serious or life-threatening events1–3. Additional therapeutic options are therefore needed. In designing therapies to target cytokines, it is important to consider the cells that produce and respond to those cytokines. Although the intent of targeting a given cytokine is generally to affect its regulation of select immune cells and prevent inappropriate immune responses, this approach can have unintended consequences, due to the roles of the cytokine in those same immune cells or in other immune and non-immune cells (e.g. epithelial cells, stromal cells, or endothelial cells), within the intestinal tissues and systemically (Figure 1). These unintended consequences can limit therapeutic efficacy or produce unexpected adverse events. We discuss these outcomes, along with advances that have provided a foundation for evaluating newer therapeutic agents for IBD. We review the successes and failures in these agents, what they tell us about IBD pathogenesis, and how they could change patient management.
Figure 1. Considerations of Cytokine Sources and Targets.
Important considerations in designing therapies targeting cytokines include both the sources of and the responders to the targeted cytokine. Intestinal tissues contain a repertoire of immune cells and non-immune cells. Although the intent of targeting a given cytokine is generally to impact on its regulation of select immune cells (e.g. T cells) contributing to inappropriate immune responses, unintended consequences may occur due to cytokine-dependent essential roles in other immune and non-immune cells (e.g. epithelial cells, stromal cells, endothelial cells) within intestinal tissues and systemically. These unintended consequences may limit the efficacy of the therapy or result in unexpected adverse events.
IL23 and Th17 Cell Pathways
Subsets of T cells distributed throughout gut-associated lymphoid tissues must be carefully regulated to maintain intestinal immune homeostasis4. These T cells are characterized by the transcription factors they express and the cytokines they secrete. CD4+ T cells are comprised of effector Th cells, which promote activation of the immune system, and regulatory T cells (e.g. Foxp3+), which suppress activation of the immune system. Effector T cell subsets such as Th1, Th2, Th9, and Th17 cells are critical for mediating defenses against pathogens and limiting excessive entry of luminal microbiota. However, expansion and over activity of these effector T cells relative to regulatory T cells can lead to intestinal inflammation4. Intestinal tissues from patients with IBD have increased levels of cytokines produced by Th17 cells (IL17, IL21, IL22, and IL265,6), Th1 cells (IFNγ and TNF), Th2 cells (IL4, IL5, IL13), and Th9 cells (IL9 and IL21)4,7. The importance of the IL23 and Th17 cell pathways in intestinal inflammation has been a particular area of focus in recent years.
IL23 and Th17 cell pathways in mice
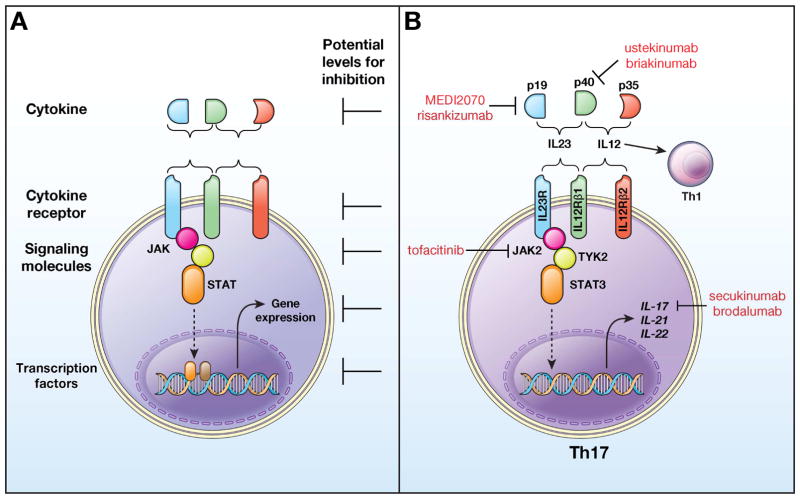
IL23 is a heterodimeric cytokine (comprising IL23p19 and IL12p40) that signals through a heterodimeric IL23 receptor (comprising IL23R and IL12Rβ1) (Figure 2). This engagement activates the janus-associated kinase (JAK) and signal transducer and activator of transcription (STAT) pathways, which regulates transcription of downstream genes (Figure 2). IL23 signaling is required for maintenance of Th17 cells and their specific phenotype, as well as for regulation of additional cell subsets, including innate lymphoid cells (ILC3s) and colonic isolated lymphoid follicles8–10. IL23 is required for optimal regulation of responses to resident and pathogenic microbes8,9,11,12.
Figure 2. IL23 and Th17 Cell Pathways.
(A) Cytokines can be made up of multiple subunits. Some subunits are specific to 1 cytokine while others are shared by 2 or more cytokines. When a cytokine interacts with its receptor, which is also frequently composed of subunits (some shared), signals are initiated which induce gene expression patterns. Many cytokine receptors activate the JAK-STAT signaling pathway. In designing therapeutic agents, is important to consider whether to target the shared vs unique components of cytokines, cytokine receptors, signaling molecules, transcription factors or downstream regulated genes, because each can produce different outcomes. It also is important is to design therapeutic agents that reduce inflammatory effects while retaining immune regulatory effects. (B) IL23 signaling is mediated by the engagement of the heterodimeric IL23 cytokine (comprising IL23p19 and IL12p40) with its heterodimeric receptor (comprising IL23R and IL12Rβ1). This engagement activates the JAK-STAT signaling pathway, which in turn, regulates transcription of genes including IL17, IL21, and IL22. IL23 is important for maintenance of Th17 cells and for the generation of the more ‘pathogenic’ Th17 cells that contribute to intestinal inflammation. IL23 and its receptor share subunits with IL12 (IL12p40) and the IL12 receptor (IL12RB1), respectively. IL12 contributes to the differentiation of Th1 cells. Therefore, agents that target the IL12p40 subunit affect IL12 and IL23 signaling, and therefore, Th1 and Th17 cells. In contrast, agents that target IL23p19 disrupt only IL23 signaling and therefore the IL23-dependent regulation of Th17 cells, as well as other cells regulated by IL23. The figure shows agents targeting molecules at distinct levels in the pathway.
IL23 is constitutively expressed in the terminal ileum11. Sources of IL23 include macrophages, dendritic cells, neutrophils, and epithelial cells8,9,13,14. Cells that produce IL17 (generally referring to IL17A, with 6 members in the family described) are also highly enriched in mucosal tissues11. Sources of IL17 include Th17 cells, γδ T cells, innate lymphoid cells (e.g. ILC3s), natural killer T cells, and intestinal epithelial cells (Supplementary Figure 1)8,9,15. Numbers of IL17-producing T cells in the intestine can be altered by environmental factors, such as intestinal microbiota (e.g. segmental filamentous bacteria), secreted microbial factors (e.g. ATP), dietary factors (e.g sodium chloride, fat), and substances that bind to the aryl hydrocarbon receptor8,9,11,16–20. Most of this information was obtained from studies of mice—the factors that regulate IL17 production in humans are incompletely defined, although select bacteria isolated from healthy individuals and patients with ulcerative colitis (UC) can induce IL17-producing cells when transferred into mice21.
IL17 contributes to microbial defenses but also chronic inflammation, through recruitment and activation of neutrophils, macrophages and dendritic cells, and production of an array of inflammatory mediators11. Although IL23 and Th17 cell pathway cytokines are constitutively expressed in intestinal tissues, mice with colitis have increased intestinal expression of IL23, and Th17 lineage cytokines and transcription factors, such as RAR related orphan receptor C (RORC)11. Transgenic expression of IL23p19 in mice results in severe systemic inflammation, as well as inflammation of the small and large intestine22. Studies have reported reduced intestinal inflammation upon induction of colitis in IL23-deficient mice or in mice given neutralizing antibodies against IL23p1923–25. The intestinal tissue injury mediated by IL23 can also be observed in the absence of IL1726 and in the absence of T cells, indicating IL17- and T-cell–independent effects of IL2327.
In addition to promoting tissue-mediated inflammation, the IL23 and Th17 cell pathways contribute to downregulation of inflammation11. The IL23-Th17 and IL12-Th1 pathways can cross-regulate each other, such that an increase in the IL23-Th17 pathway can decrease Th1 pathway activation28. In addition, Th17 and ILC3 populations secrete immune regulatory cytokines such as IL22. IL22 contributes to epithelial barrier restitution, mucus-producing goblet cells, and anti-microbial protein production11; these functions contribute to homeostasis at mucosal surfaces. Consistently, IL22 can attenuate inflammation in some models of colitis in mice29–31. Importantly, sustained expression of IL22 increases risk of colonic dysplasia and cancer due to ongoing epithelial cell proliferation31,32. Given the immune regulatory roles for IL23, blocking or loss of IL23 or IL23R might worsen colitis under certain conditions33. Therefore, Th17 cells are heterogeneous and the cytokines they produce can defend against microbes at mucosal surfaces while simultaneously downregulating inflammation and restoring injured tissues.
IL23 and Th17 cell pathways in human beings
Levels of IL23 and Th17 cell cytokines are increased in the intestinal mucosa, plasma, and serum of patients with IBD11,34,35. Variants in several genes in the IL23 and Th17 cell pathways are associated with risk for IBD, including IL23R, IL12B, JAK2, TYK2, STAT3, RORC, and CCR6.36,37 The most significant of these associations is a variant of IL23R that encodes an amino acid change from an arginine to a glutamine at position 381 and reduces risk of IBD38 and other immune-mediated diseases, such as ankylosing spondylitis and psoriasis4. This protective variant results in a loss-of-function of IL23R, with decreased STAT3 signaling and Th17 cell responses upon exposure to IL2339–41. Therefore, the convergence of data in human studies demonstrating elevated IL23 and Th17 cell pathway molecules in inflamed intestinal tissues and IL23R loss-of-function genetic variants leading to IBD protection, and in animal studies demonstrating efficacy in blocking IL23, positioned the IL23 and Th17 cell pathways as promising targets in IBD.
Targeting the IL23 and Th17 cell pathways
What is the optimal level and optimal approach for targeting the IL23 and Th17 cell pathways in patients with IBD? Despite the recent focus on the IL23 pathway in mediating intestinal inflammation, there is significant evidence for Th1 cell-mediated inflammation, as well as for the combined effects of Th1 cell and IL23–Th17 cell pathways in intestinal inflammation11. Therefore, there might be advantages to targeting the shared IL12p40 subunit, which regulates both Th1 and Th17 cells. However, IL23 might contribute more specifically to mucosal inflammation, with IL12 mediating more systemic effects,27,42 so selective targeting of IL23, via the unique IL23p19 subunit, might be more effective. This hypothesis is supported by a recent trial in patients with psoriasis—selective blockade of IL23p19 was more effective than blockade of IL12p4043. Targeting the cytokines and/or molecules downstream in the IL23–Th17 cell pathway, which are thought to mediate inflammatory effects, might avoid the adverse consequences of inhibiting immune regulatory cytokines in this pathway, such as IL22 and IL10. Trials targeting multiple levels in the IL23 and Th17 cell pathways have been conducted and provide interesting results (Figure 2).
Trial results
Several therapeutic agents designed to disrupt the IL23 and Th17 cell pathways have been studied (Table 1, Supplementary Table 1). One of the earliest therapeutic agents in this class was briakinumab, a monoclonal immunoglobulin (Ig)G1 that disrupts the interactions of IL12 and IL23 with their receptors by blocking the IL12p40 subunit.44 A phase 2 trial found that a significantly larger proportion of patients with Crohn’s disease had a response by week 7 to weekly weight-based subcutaneous briakinumab (75%) than placebo (25%). Patients given briakinumab also had improvements in histologic disease activity, and ex vivo stimulated colonic lamina propria T cells from briakinumab-treated patients produced lower levels of IL12, IFNγ, and TNF.44
Table 1.
Findings From Clinical Trials of Patients With IBD
| Key Outcomes and Observations | Insights and Lessons Learned | |
|---|---|---|
| IL23/Th17 pathway | ||
| Mannon44, 2004 Phase 2A, briakinumab Crohn’s disease |
- Significant increase in response rates
with weekly SQ weight-based dosing - Accompanied by improvement in histologic activity and cytokine response - Higher rate of injection site reaction with intervention vs placebo - Presence of ADA prior to initiation of therapy |
- Dose response: weekly SQ treatment at
higher dose associated with best response and efficacy - Possibly related to immunogenicity and improved drug concentration with higher dose |
| Panaccione48, 2015 Phase 2B, briakinumab Crohn’s disease |
- Failed to meet primary end-point
(clinical remission at week 6) - Week 12 rates of remission and response higher in some active intervention groups but no consistent demonstrable efficacy and considered a negative study - Higher rate of infusion reactions with intervention (switched to different formulation compared to phase 2A trial) |
- Immunogenicity may have impacted
outcomes - Clinical remission too strict as primary outcome for phase 2 if used early (i.e. week 6) - May have time dependency efficacy which impacts optimal time point of assessment and re-randomization design |
| Sandborn45, 2008 Phase 2A, ustekinumab Crohn’s disease |
- Failed to meet primary end-point
(clinical response at week 8), although there was a significant increase
in week 4 and 6 response rates and there was a measurable reduction in
inflammation for intervention arm but not placebo - Efficacy influenced by prior anti-TNF therapy with improved efficacy demonstrated in anti-TNF failures - Efficacy influenced by use of 100-point CDAI response as end-point - Enhanced efficacy with IV vs SQ formulation of drug |
- 100-point CDAI response and shorter
follow-up interval to assess primary end-point - Enrich future trials with anti-TNF failures - Switch to IV weight-based dosing regimens |
| Sandborn46, 2012 Phase 2B, ustekinumb Crohn’s disease |
- Met its primary end-point (clinical
response at week 6) for highest weight-based dose (6 mg/kg) - Among responders, use of SQ maintenance therapy associated with higher response, remission, and steroid-free remission rates - Efficacy again influenced by prior anti-TNF therapy with improved efficacy demonstrated in anti-TNF failures |
- Study anti-TNF failures and non-failures
or those naïve to anti-TNF therapy separately - IV weight-based induction with SQ fixed-dose maintenance feasible and associated with treatment efficacy |
| Feagan47, 2016 Phase 3, ustekinumab Crohn’s disease |
- Met its primary end-point (clinical
response at week 6) for fixed-dose and weight-based IV induction
regimen - Association between drug concentrations and treatment outcomes, with weight-based regimen achieving therapeutic concentrations more often - Difference between intervention and placebo similar for both anti-TNF naïve and anti-TNF failure, with trend towards improved outcomes for anti-TNF naive - Demonstrable efficacy for IV induction with SQ maintenance |
- Pharmacokinetics likely similar to that
of anti-TNF therapy with regards to drug concentration and treatment
efficacy association and dosing - Rapid treatment onset and effect - Prior signals for enhanced efficacy in anti-TNF failures not clearly shown |
| Sands56, 2015 Phase 2, MEDI2070 Crohn’s disease |
- Higher rate of clinical effect (clinical remission OR clinical response) and clinical effect + > 50% reduction in CRP or FC, but rates of remission specifically not significantly higher in active treatment arm vs placebo at week 8 | - IL23p19 inhibition at least
equally efficacious as compared IL12p40 inhibition - Week 12 may be ideal assessment point - Consider enrichment with biomarkers or endoscopic evaluation of inflammation |
| Feagan55, 2016 Phase 2, Risankizumab Crohn’s disease |
- Higher rate of clinical remission, endoscopic response, and endoscopic remission at week 12 as compared to placebo | |
| Hueber57, 2012 Phase 2A, Secukinumab Crohn’s disease |
- Study stopped due to futility given
higher response rate in placebo group vs active treatment group - Genetic polymorphisms identified to be associated with response and/or worsening of disease activity with drug exposure - Increased frequency of infectious complications, with specific increase in fungal infections |
- These class of agents have been abandoned
in IBD - Potential for genetic enrichment of trials |
| Th1 Pathway | ||
| Reinisch52, 2006 Phase 2, fontolizumab Crohn’s disease |
- No clear dose-dependent safety signal or
intolerability - Dose-dependent signal of efficacy and response to therapy. However, the placebo group had high rates of response and no statistical significance - Treatment effect more prominent when stratifying by CRP |
- anti-IFNG biologics are tolerable and
there may be a signal of efficacy at higher doses - High placebo rates possibly driven by lack of active inflammation and improved treatment effect size when stratifying by CRP |
| Hommes51, 2006 Phase 2, fontolizumab Crohn’s disease |
- Failed to meet primary end-point
(response on day 28 after single dose) - Statistically significant rates of response with follow-up dosing at day 56 with trend towards significance for clinical remission - Treatment effect again more prominent when stratifying by CRP with accompanying reduction in placebo response rates - Pharmacodynamic effects were observed by immunohistochemistry |
- Multiple doses are needed to demonstrate
the potential efficacy of this agent - Placebo rates and CRP again impacted results and consideration for baseline assessment of inflammation |
| Reinisch53, 2010 Phase 2, fontolizumab Crohn’s disease |
- Failed to meet its primary end-point
(response on day 29) - Again observed increased response over time - Higher rate of adverse events and ADA antibodies (study switched to using SQ formulation of drug after first IV based dose) |
- Primary end-point should be beyond 28
days - Unclear pharmacokinetics of SQ formulation |
| Th2 Pathway | ||
| Danese102, 2015 Phase 2, Tralokinumab UC |
- Higher rate of clinical remission but not clinical response or mucosal healing at week 8 as compared to placebo | - Add on therapy with anti-cytokine agents targeting IL-13 in UC is not efficacious |
| Reinisch103, 2015 Phase 2, Anrukinzumab UC |
- Failed to meet its primary end-point with a high dropout rate due to lack of efficacy | |
| Other Cytokines | ||
| Ito105, 2004 Phase 2, MRA (anti-L6R) Crohn’s disease |
- Higher rates of response and clinical remission at week 8 and 12 as compared to placebo, but no difference in endoscopic or histologic response | - Targeting IL-6 may be a therapeutic option |
| Danese106, 2016 Phase 2, anti-IL6 Crohn’s disease |
- Met its primary end-point for clinical
response (CDAI score of 70) at weeks 8 and 12 - Higher rate of clinical remission with 50mg dosing regimen - Concerns surrounding safety, with majority of events with high dose (200mg) |
- Anti-IL6 therapies are efficacious but may be associated with increased rates of adverse events |
| JAK Pathway | ||
| Sandborn110, 2012 Phase 2A, Tofacitinib UC |
- Met its primary end-point (clinical
response) along with key secondary outcomes (clinical and endoscopic
remission) - Dose dependent increase in cholesterol and potentially neutropenia |
- Efficacious treatment option
for UC - 10mg twice daily optimal dosing strategy - Rapid onset of treatment efficacy - Equally efficacious in anti-TNF naïve and exposed individuals |
| Sandborn111, 2016 Phase 3, Tofacitinib UC |
- Again demonstrated a significant increase
in response, remission, and mucosal healing outcomes with active
treatment arm as compared to placebo - Rapid treatment onset (within 2 weeks of therapy) and outcomes similar in anti-TNF naïve and anti-TNF exposed |
|
| Sandborn112, 2014 Phase 2A, Tofacitinib Crohn’s disease |
- No improvement in clinical efficacy for
any of the dosing regimens at week 4, although highest dose did result
in reductions in systemic inflammation - Dose dependent increase in cholesterol |
- High placebo rates may be due to lack of
disease activity assessment prior to enrollment - May have slower onset of action in CD as compared to UC, and may require longer follow-up to assess treatment efficacy |
| Panes113, 2016 Phase 2B, Tofacitinib Crohn’s disease |
- Again failed to meet primary end-point now at week 8, but did demonstrate reduction in systemic inflammation (CRP and FC) | - Non-selective inhibition of JAK pathway may not be an efficacious treatment option in CD |
| Vermeire114, 2016 Phase 2, Filgotinib Crohn’s disease |
- Significantly higher rate of response and remission at week 4 | - Selective JAK1 inhibition may be a more effective approach for targeting the JAK pathway in CD |
ADA: antidrug antibodies; IV: intravenous; SQ: subcutaneous; CRP: C-reactive protein, FC: fecal calprotectin; CD: Crohn’s disease
Shortly thereafter, the effects of ustekinumab, another monoclonal IgGI (fully human) against IL12p40, were studied in a phase 2 trial. A significantly higher proportion of patients with Crohn’s disease given ustekinumab had a response at week 4 (53% vs 30% in patients given placebo) and week 6 (53% vs 30% in patients given placebo)45. Although there was no statistically significant difference in the proportion of patients who achieved the primary endpoint of clinical response at week 8 (49% of the ustekinumab group vs 40% of the placebo group), 2 key observations were made. First, outcomes were associated with prior exposure to TNF antagonists; among patients with previous exposure to TNF antagonists, 59% of those given ustekinumab had a response at week 8 compared with 26% of those given placebo which was statistically significant. Second, the authors observed slightly higher rates of response and remission with weight-based dosing compared to fixed-dose subcutaneous administration. It is unclear if these observations were true differences in efficacy or simply variations in placebo response rates and the effect of small sample sizes.
Based on findings from the phase 2A trial of ustekinumab, several notable changes were made to the phase 2B study design.46 First, the authors chose a shorter follow-up time point (week 6) and used intravenous weight-based dosing. Second, they used a decrease in Crohn’s Disease Activity Scores (CDAI) scores of 100 points as the primary endpoint, given the higher difference between groups observed in the phase 2A trial with this outcome. Finally, the authors limited the study to patients with Crohn’s disease who had not responded to previous TNF antagonist therapy, and during randomization they stratified patients based on the reason for TNF antagonist failure. The phase 2B trial met its primary end point: 40% of patients given ustekinumab had a significant response at week 6 vs 24% of patients given placebo. Furthermore, among individuals with an initial response to therapy, at week 22 a significantly higher proportion of patients receiving subcutaneous fixed-dose maintenance ustekinumab had a response (70% vs 43% given placebo), entered remission (42% vs 27% given placebo), and had steroid-free remission (31% vs 18% given placebo).
The Phase 2B ustekinumab trial design was carried forward into phase 3 studies, which also reported that a significantly higher percentage of patients with Crohn’s disease had a response to ustekinumab than placebo.47 Efficacy was observed as early as week 3, a positive association was demonstrated between ustekinumab drug concentrations and treatment outcomes, and the weight-based dosing group more often achieved ustekinumab concentrations associated with improved efficacy.47 Importantly, efficacy was demonstrated in individuals who had and had not been exposed to TNF antagonists, with similar differences between groups in proportions responding to drug vs placebo. Among responders to ustekinumab induction therapy who were re-randomized to groups given subcutaneous ustekinumab maintenance every 8 or 12 weeks or placebo (IM-UNITI study), the rates of clinical remission, steroid-free remission, and durable clinical response were significantly higher in both ustekinumab maintenance groups, compared to the placebo group, but generally greater in the 8-week group. Notably, higher proportions of patients who were naïve to TNF antagonists achieved clinical remission (65% of patients receiving ustekinumab every 8 weeks, 57% receiving it every 12 weeks, and 49% of patients receiving placebo) compared to patients who had previously failed TNF antagonist therapy (41% of patients receiving ustekinumab every 8 weeks, 39% receiving it every 12 weeks, and 26% receiving placebo). This is in contrast to phase 2 studies, which reported consistent efficacy only among patients who failed treatment with TNF antagonists.
The phase 2B trial of briakinumab in patients with Crohn’s disease failed to meet its primary endpoint of inducing clinical remission by week 6,48 although a significantly higher proportion of patients receiving intravenous briakinumab (400 mg) achieved remission by week 12 (29%) compared with placebo (11%). Significantly higher proportions of patients given 700 mg briakinumab had responses at week 6 (37% vs 17% of patients given placebo) and week 12 (40% vs 20% of patients given placebo).
There are several potential reasons for the lack of observed efficacy for briakinumab compared with ustekinumab. Clinical remission may not be an ideal early endpoint for studies of agents that block IL12p40. Furthermore, the study used a re-randomization of responders enrichment strategy to assess maintenance therapy. The interval between re-randomization and repeat assessment was only 12 weeks, which may have resulted in a higher response to placebo, due to a lack of drug washout. Finally, the authors did not assess immunogenicity or drug concentrations for the intravenous formulation of this drug, which replaced the subcutaneous formulation used in the phase 2A trial; this could have resulted in increased immunogenicity, reducing drug concentrations. Consistent with this possibility, infusion reactions (a potential consequence of immunogenicity) occurred in a greater percentage of patients given briakinumab than placebo. These results highlight the value of targeting a given pathway with multiple drugs, and using different trial designs.
Fontolizumab is a monoclonal antibody against IFNγ; IFNγ is an effector molecule in the IL12-Th1 cell pathway. Levels of IFNγ are increased in the lamina propria of patients with Crohn’s disease49,50. Although a signal of efficacy was observed in fontolizumab trials in Crohn’s disease patients, the magnitude of fontolizumab’s effect was less than that of agents that target IL12p40 (ustekinumab).51–53 This was likely in part due to a large placebo effect and variations in trial designs, time-point assessments, transition to subcutaneous formulation without pharmacokinetic analyses, and unclear dosing strategy. Furthermore, IFNγ has additional activities, such as contributing to inhibition of intestinal inflammation by downregulating IL2354, and additional Th1 cytokines cooperate to mediate intestinal inflammation. In aggregate, these trial design and biological factors may have contributed to the trial outcomes.
Risankizumab and MEDI2070 (brazikumab) were developed to target the IL23p19 subunit of IL23 (also called IL23A). Risankizumab, a fully human monoclonal IgG1 against IL23p19, has been examined in a phase 2 trial of patients with Crohn’s disease. At week 12, a significantly higher proportion of patients given 600 mg risankizumab (37%) achieved clinical remission (the primary endpoint) than of patients given placebo (15%).55 Furthermore, significantly greater proportions of patients receiving 600 mg risankizumab achieved endoscopic remission (20% vs 3% of patients given placebo) or had an endoscopic response (37% vs 13% of patients given placebo).
Similarly, results from a phase 2 study of MEDI2070 (brazikumab) in patients with Crohn’s disease were promising. A significantly greater proportion of patients receiving MEDI2070 (brazikumab) (49%) achieved clinical remission or had clinical response than of patients receiving placebo (27%).56 However, the proportions of patients who achieved clinical remission specifically did not differ significantly between groups (27% for MEDI2070 vs 15% for placebo). We cannot directly compare the efficacies of risankizumab or MEDI2070 (brazikumab) with ustekinumab or briakinumab, due to differences in trial design, enrollment criteria, concomitant medications, prior treatment failures, and follow-up intervals. However, the data indicate that selectively blocking IL23 through IL23p19 inhibition is at least equally efficacious as compared to ustekinumab which inhibits both IL23 and IL12 through blocking IL12p40.
In contrast to the positive results from trials of agents that block combined IL12 and IL23 or selectively block IL23, which are upstream in the IL23-Th17 pathway, strategies to target IL17 which was hypothesized to be mediating the inflammatory consequences of the pathway, were ineffective. Secukinumab, a monoclonal antibody against IL17A, was examined in a small phase 2 trial of 59 patients with Crohn’s disease.57 The trial was stopped early, due to futility, and this agent is no longer being investigated for treatment of Crohn’s disease. Although several trial design issues could be implicated in the lack of efficacy, it was notable that among individuals with active inflammation at baseline (based on levels of C-reactive protein or fecal calprotectin), the placebo group had a greater reduction in disease activity at the end of the study period than the secukinumab group. However, among patients with no active inflammation at baseline, the reduction in disease activity was similar between groups. This finding indicates that in individuals with truly active Crohn’s disease, secukinumab was not associated with improvement, compared to placebo, and might actually worsen disease activity. Furthermore, a monoclonal antibody against the IL17 receptor, brodalumab, did not show efficacy in a phase 2 trial, so the trial was terminated early.58
Why were Outcomes Different when Targeting IL23 vs IL17?
The contrasting outcomes of targeting IL23 or combined IL12 and IL23 vs targeting IL17 or its receptor in patients with Crohn’s disease has led to much discussion about the functions of these pathways, how they might contribute to IBD pathogenesis, and where to direct research on therapeutic agents.
Targeting IL17 or its receptor had mixed results in mouse models. With IL17 deficiency or blockade, some studies in experimental mouse models (e.g. transfer of CD45RBhi CD4+ T cells into RAG-deficient mice, dextran sodium sulfate (DSS)-induced colitis) demonstrated increased intestinal inflammation28,59, whereas other studies reported decreased inflammation60. The increased inflammation with IL17 deficiency or blockade occurred in the context of a compensatory increase in Th1 cells28,61. Recent studies in Abcb1a−/− mice and with DSS-induced colitis recapitulated the dichotomy of reduced intestinal inflammation upon blockade of IL23 or combined IL12 and IL23 vs increased inflammation upon blockade of IL17 or its receptor61,62. These studies found that with defects in IL17 or IL17R signaling during inflammation, there was impaired intestinal epithelial barrier function and decreased intestinal expression of anti-microbial proteins61,62. Therefore, given the multiple targets of IL17 (Supplementary Figure 1), the adverse effects of IL17 deficiency outweighed the benefits of blocking its contribution to intestinal inflammation. Interestingly, a population of lamina propria γδ T cells produced IL17 in an IL23-independent manner, such that select IL17 production could persist despite IL23 deficiency or blockade62. Importantly, in contrast to its effects in patients with IBD, IL17 blockade is highly effective in patients with psoriasis63, highlighting the different roles of IL17 in distinct tissues.
Another consequence of blocking IL17 in patients with Crohn’s disease was a reported increase in fungal infections57. In humans and mice, the IL23-Th17 cell pathway protects against fungal infections and intracellular bacteria—particularly at mucosal surfaces11. Patients with mutations in genes encoding members of the IL17 family or their receptors (IL17F or IL17RA), adaptors required for IL17R-initiated signaling (ACT1), or proteins that signal IL17 production (IL23, IL12B, IL12RB1, STAT1, STAT3, TYK2, CARD9 and DECTIN1), are at increased risk of fungal infections and/or chronic mucocutaneous candidiasis9. Patients with these genetic variants are also at increased risk for infection with mycobacteria, Salmonella, and Staphylococcus. Risk for these infections should be considered with treatments targeting the IL23 and Th17 cell pathways in patients with IBD.
The observed IL17-independent efficacy of targeting upstream in the IL23 signaling pathway (IL23 or combined IL12 and IL23) are likely multifold. IL23 can increase the pathogenic behavior of non-Th178,9,64 and Th17 cell subsets, thereby contributing to intestinal inflammation19,65–70. Th17 cells have a spectrum of phenotypes and demonstrate plasticity. Th17 cells are influenced by factors in the local environment, such as cytokines, and their position on the longitudinal axis of the intestine8,9,71–75, thereby enabling Th17 cells to adapt to ongoing conditions. Cells that express IL10 or FOXP3 in addition to IL17 can protect against inflammation 73,74,76. In contrast, cells that produce IFNγ and/or colony stimulating factor 2 (CSF2, also called GMCSF) can promote inflammation, and their numbers are increased at sites of inflammation, including in intestinal tissues of patients with IBD42,75,77–84. Importantly, IL23 directs these pathogenic, inflammation-promoting Th17 cells in mice and humans.11,17,18,81,85,86 Th17 cells can be identified based on surface markers and transcription factors associated with their differentiation (such as RORC, STAT3, IRF4, and BATF8,9), as well as their unique transcriptional signatures, relative to other CD4+ T cell subsets. Furthermore, Th17 cells that protect against inflammation vs those that contribute to it have different gene expression profiles.11,17,18,81,85–92 Given the importance of these factors in regulating IL23 and Th17 cell pathways, additional strategies to inhibit these pathways in patients with IBD include inhibition of lineage-specific transcription factors (such as RORC93,94; inhibitors are being tested in clinical trials), factors that amplify Th17 cells (such as IL21), and factors that regulate the inflammatory effects of Th17 cells.
Inhibiting Additional Cytokine Pathways
IL13 is produced by Th2 cells and its levels were reported to be increased in intestinal tissues of patients with UC in some,49,95,96 but not all studies97. IL13 can contribute to cytotoxicity towards intestinal epithelial cells, epithelial barrier dysfunction, and fibrosis.98–100 Further, IL13 blockade can reduce intestinal inflammation and fibrosis in mice with colitis.100,101 However, 2 trials examining anti-IL13 biologic agents failed to meet their primary end points,102,103 although there appeared to be a signal of efficacy in some patients with UC (Table 1, Supplementary Table 1). Variations in patient populations and mucosal levels of IL13, trial size, and compensatory effects of other cytokines may have contributed to the lack of efficacy.
IL6 has pleiotropic activity in the innate and adaptive immune responses. Levels of IL6 and its receptor (allows for trans-signaling) are increased in patients with IBD and are associated with increased disease severity104; disrupting IL6 signaling reduced colitis in mice104. The first clinical trial with a monoclonal antibody against the IL6 receptor, in 36 patients with Crohn’s disease, reported a clinical response in 80% of patients given the agent vs 31% of patients given placebo. Clinical remission was achieved by 20% of the patients given the agent vs none of the patients given placebo, at week 12 (Table 1, Supplementary Table 1).105
A phase 2 trial of an anti-IL6 biologic agent has produced conflicting results. This study met its primary end-point of clinical response at week 8 and week 12 among patients given 50 mg of the agent, and there was a significant difference in the proportion of patients in clinical remission after receiving 50 mg of the agent vs placebo (difference, 17%). However, there was a troubling number of adverse events, including 1 death, 2 perforations, and 4 serous gastrointestinal abscesses in the group given the anti-IL6 antibody.106 Of note, cases of gastrointestinal perforation and increased incidence of infection were also described in patients with rheumatoid arthritis receiving therapy targeting the IL6 pathway107. IL6 plays a critical role on multiple cell targets, including on epithelial cells, where it contributes to intestinal epithelial proliferation and restitution during injury104,108. Therefore, despite the ability of IL6 pathway targeting to induce remission in patients with IBD, the essential role for IL6 on various cell subsets appears to result in side effects that outweigh its benefits in IBD patients.
Signaling pathways that regulate multiple cytokines
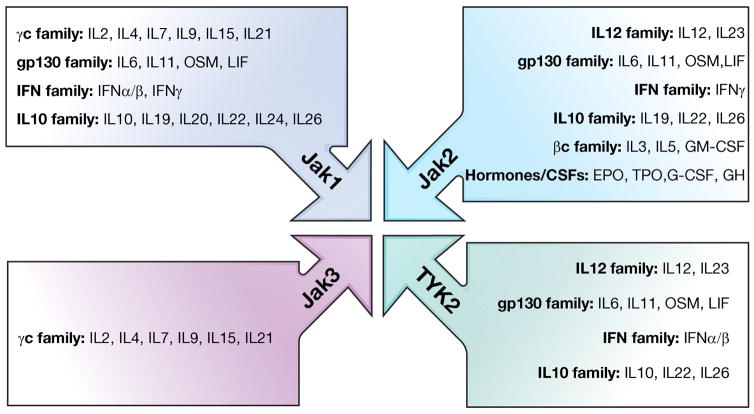
Most of the therapeutic agents designed to date to target cytokines in IBD patients have acted on a specific cytokine or cytokine receptor, generally through the use of monoclonal antibodies. Another approach involves targeting signaling pathways used by multiple cytokines contributing to intestinal inflammation in IBD. Recent trials have focused on the JAK family of proteins, non-receptor tyrosine kinases comprising 4 members: JAK1, JAK2, JAK3 and TYK2. JAK family members, in cooperation with STAT family members, are critical for interacting with and initiating signaling downstream of a wide array of cytokine receptors109 (Figure 3). In addition, JAK2 initiates signaling from various colony-stimulating factors (e.g. GMCSF, erythropoietin) and hormones.
Figure 3. Cytokines That Signal via JAK Proteins.
The JAK family of proteins are receptor tyrosine kinases comprising 4 members: JAK1, JAK2, JAK3, and TYK2. The different JAK family members, in cooperation with STAT family members, interact with and initiate signaling from a number of cytokine receptors. The figure shows select cytokines that signal through individual JAK members109,145. It is important to note that JAK2 also mediates signaling from various growth factors and hormones.
Variants in genes that activate JAK signaling, or in JAK2 or TYK2 themselves, are associated with IBD11. The wide range of receptors regulated by JAK signaling ultimately leads to effects on many immune and non-immune cells. Given the important role of T cells in IBD pathogenesis, and the many cytokines that signal through JAKs to regulate T cell functions, small molecules inhibitors have been developed to inhibit JAKs (JAKINIBs) and thereby reduce T cell activation and differentiation.109 Distinct JAK inhibitors with differing specificities are under investigation for many immune-mediated diseases; tofacitinib has been approved by the Food and Drug Administration for treatment of rheumatoid arthritis109. Tofacitinib is the best studied of the inhibitors for IBD (Table 1, Supplementary Table 1). It is an oral small molecule inhibitor and competitively binds to the ATP-binding site of JAK1, JAK2, and JAK3 to inhibit kinase activity.
JAK pathway trial results
Tofacitinib demonstrated promising results in phase 2 and 3 trials of patients with UC. In the phase 2 study, twice-daily tofacitinib produced statistically significant increases in rates of clinical response, clinical remission, endoscopic response, and endoscopic remission at week 8, compared to placebo.110 The 10 mg dose was subsequently chosen for the phase 3 trials, which were recently completed.111 Within the 2 identical phase 3 induction trials (Oral Clinical Trials for tofAcitinib in ulceratiVE colitis [OCTAVE] 1 and 2), tofacitinib resulted in a statistically significant increase in rates of clinical response, clinical remission, and mucosal healing at 8 weeks, compared to placebo. In both induction trials, there was a significant difference between tofacitinib and placebo in producing a clinical response as early as week 2, and rates of clinical remission and mucosal healing were similar in anti-TNF naïve and anti-TNF exposed individuals.
In contrast to trials of patients with UC, trial of tofacitinib in patients with Crohn’s disease have produced disappointing results. In the phase 2A trial rates of clinical response and remission were not significantly higher in any of the tofacitinib groups compared to placebo.112 However, the placebo response and remission rates were quite high, and in some instances higher than the tofacitinib groups. Given the measurable effects of tofacitinib on reducing systemic inflammation (based on levels of C-reactive protein and calprotectin) in these patients, this high placebo response was proposed to account for some of the lack of demonstrable efficacy with tofacitinib. Disease extent and presence was confirmed by endoscopy or imaging within the preceding 24 months of enrollment, which may have allowed for some misclassification of true mucosal inflammatory disease activity at the time of randomization. Furthermore, the study used the week 4 time point for assessment, which may have been too short to allow for treatment separation.
In the phase 2B trial, mucosal inflammation (ulceration) was therefore confirmed by colonoscopy within the 6 weeks before randomization, although the results were not read centrally.113 Despite this, the study failed to meet its primary end point (remission at week 8) and the response was still small, albeit statistically significant. This study also associated tofacitinib with a significant reduction in systemic inflammation (based on measurement C-reactive protein and calprotectin), but this did not translate into meaningful disease activity changes.
A phase 2 trial of the selective JAK1 inhibitor filgotinib was recently completed and reported promising results for patients with Crohn’s disease.114 Filgotinib produced a statistically significant increase in rates of remission (primary endpoint, in 47% vs 23% in the placebo groups) and response (in 59% vs 41% in the placebo group) at week 10. This would suggest that selective JAK inhibition may be more effective in inducing responses and remission in patients with Crohn’s disease; additional selective inhibitors of JAK1 and JAK1/2 are under evaluation (such as ABT-494 and baricitinib).
Why might tofacitinib be less effective in patients with Crohn’s disease than UC? The different outcomes observed could be due to technical aspects in trial design, to differences in disease pathogenesis, or a combination of these. The trial of patients with Crohn’s disease had a high rate of remission in the placebo group (36%) compared to other trials (18%), which may be a contributing factor. In considering differences in disease pathogenesis, the JAK family is expressed in a wide array of cells and essential not only for mediating the effects of proinflammatory cytokines, but also for immune regulatory cytokines (Figure 3). This raises the possibility of potential unintended consequences of JAK inhibition on other cells, such as epithelial cells or innate immune cells, which can restore homeostasis during intestinal inflammation.
JAK3 is required in intestinal epithelial cells for optimal epithelial proliferation in vitro115, and for proper enterocytic and secretory epithelial lineage differentiation in vivo116. Consistently, compared to mice without deletion of JAK3, mice with JAK3 deletion develop more severe colitis following administration of DSS, with associated decreased barrier function116. Complete deletion and epithelial-specific deletion in mice of yet another JAK family member, TYK2, can also increase the severity of DSS- and citrobacter-induced colitis; TYK2 deficiency leads to impaired epithelial proliferation and anti-microbial protein production in response to IL22, as well as alterations in intestinal microbial composition117. Other factors that control epithelial cell proliferation108,115,118,119 also signal through JAK proteins.
JAK inhibition also affects the function of innate immune cells. Most120–123, but not all124, studies that inhibited JAKs in myeloid cells during microbial product stimulation reported reduced production of anti-inflammatory cytokines and increased production of proinflammatory cytokines; this pattern would likely not be helpful to patients with IBD, because myeloid cells in intestinal tissues are continuously exposed to microbial products. The increased production of proinflammatory cytokines has been attributed to the impaired autocrine and paracrine anti-inflammatory cytokine signaling pathways required to reduce expression of proinflammatory cytokines. In human myeloid cells, reduced production of anti-inflammatory cytokines and increased production of pro-inflammatory cytokines are observed specifically once the level of JAK signaling falls below a specific threshold (~25%)123, indicating that outcomes can differ in innate immune cells based on levels of JAK inhibitor. Variants in the JAK2 gene associated with IBD lead to altered regulation of JAK2 expression123, so it might be beneficial to analyze genotypes of JAK2 or of IBD-associated genes that regulate other JAK family members before JAK inhibitors are given to patients. As innate immune signaling pathways are particularly important in Crohn’s disease patients, the effects of JAK inhibition on myeloid cells, as well as on epithelial cell restitution, may counteract beneficial effects of JAK inhibition on T cells. This may be more pronounced when multiple JAK family members are inhibited simultaneously. Ultimately, the balance in inflammatory (lymphocyte activation and differentiation) and regulatory (epithelial restitution, select innate immune cell functions) immune responses may differ based on the specific JAKs inhibited and the threshold of signaling that remains, as well as on the pathogenic mechanisms mediating UC versus Crohn’s disease.
Sphingosine-1-phosphate pathways
Another approach to reducing the activities of multiple cytokines simultaneously is to decrease immune cell trafficking into intestinal tissues. Recent reviews have discussed targeting of adhesion molecules and chemokine pathways (see125,126). Researchers have recently investigated strategies to target the sphingosine-1-phosphate pathway, which reduces circulating lymphocytes by sequestering them in secondary lymphoid organs.127 In a phase 2 trial of patients with UC, once daily ozanimod (1 mg) resulted in statistically significant increases in clinical remission and mucosal healing at week 8 compared with placebo.128 An important observation from this trial was that the rates of histologic remission (22%) were lower than the rates of mucosal healing at week 8 (34%) with ozanimod, but by week 32 these rates were more comparable (31% vs 33%). This would suggest that efficacy increases with time with this agent similar to other anti-trafficking agents, thereby highlighting the need for extended duration studies.
Increasing Anti-Inflammatory Pathways: The TGFβ Pathway
Cytokines such as IL10 and TGFβ and immune cells such as T-regulatory cells downregulate immune responses in intestinal tissues, where immune cells are continuously exposed to microbial products. TGFβ has many functions, and is produced by and acts on many different cells, including specialized intestinal populations129–132. Mice with disruption of Tgbf1 develop lethal levels of inflammation, indicating the importance of TGFβ1 in controlling the immune response in mice.133,134. Mice with disruption of Tgfbr2 specifically in T cells also develop severe and diffuse tissue inflammation, including in intestinal tissues135.
There are 3 isoforms of TGFβ: TGFβ1 (predominantly expressed in the immune system), TGFβ2, and TGFβ3. TGFβ signals through 2 trans-membrane receptors, TGFβR1 and TGFβR2. Upon activation, the serine-kinase receptor TGFβR1 directly phosphorylates SMAD2 and SMAD3, leading to association of these proteins with SMAD4, and subsequent translocation of the complex to the nucleus, where it regulates target genes. There are also inhibitory Smad proteins (SMAD6 and SMAD7). SMAD7 interacts with TGFβR1 to interfere with phosphorylation of SMAD2 and SMAD3 upon TGFβ1 exposure; this prevents optimal TGFβR signaling in target cells.
Although levels of TGFβ1 are increased in intestinal tissues of mice with colitis136,137 and in patients with IBD138, levels of TGFβ have been insufficient to inhibit the inflammation observed. One mechanism identified for this insufficient inhibition has been the inability of TGFβ to mediate optimal inhibitory effects on target populations. Consistently, levels of SMAD7 are increased in intestinal lamina propria cells (T cells and non-T cells) from mice with colitis and patients with UC and Crohn’s disease136,137. Consistent with the upregulated SMAD7, intestinal lamina propria cells from inflamed intestine have reduced levels of TGFβ1-induced SMAD3 phosphorylation compared with non-inflamed control tissues136,137,139. Further, engineered overexpression of SMAD7 in CD4+ T cells makes them less susceptible to suppression by T-regulatory cells (an important source of TGFβ) in vitro and in vivo during intestinal inflammation in mice139. In contrast, reducing expression of SMAD7 with an antisense oligonucleotide increases responsivity of lamina propria cells from patients with IBD to TGFβ1 ex vivo and attenuates inflammation in mice with colitis136,137. Findings from these studies have provided the foundation for clinical trials to reduce the upregulated SMAD7 observed in patients with IBD.
SMAD7 pathway trial results
Mongersen is an anti-sense oligonucleotide that hybridizes with human Smad7 RNA to reduce levels of SMAD7 protein. A pH-dependent release tablet allows for the drug to become active in only the terminal ileum and right colon, making it optimal for treatment of ileocolonic Crohn’s disease. In a phase 2 trial, rates of clinical remission (proportions of patients achieving remission at day 15 and maintaining it through day 28) were significantly higher in the 160 mg (65%) and 40 mg (55%) groups than the placebo group (10%).140 The rates of clinical response at days 15 and 28 were also significantly higher in groups given 160 mg or 40 mg compared with placebo. Interestingly, when analysis was limited to individuals with increased levels of C-reactive protein at baseline, similar proportions of patients normalized their level of C-reactive protein, for all doses (160 mg, 18%; 40 mg, 18%; and 10 mg, 22% vs placebo, 4%). However, none of the groups given mongersen had statistically significant reductions in level of C-reactive protein. This disconnect may indicate a gut selectivity of this agent or may be related to a disconnect between symptomatic disease activity and mucosal inflammation in patients with Crohn’s disease.141 Nevertheless, these results are promising and this study achieved one of the highest treatment effect sizes observed in trials of patients with Crohn’s disease. Further studies using composite end points of clinical and mucosal outcomes will be important to ensure accurate disease classification and response to therapy.
It is important to note that TGFβ is also an activator of fibroblasts, myofibroblasts, and smooth muscle cells; these cells contribute to the increased collagen production, and ultimately strictures, observed in patients with IBD142. Myofibroblasts from mucosa overlaying strictures in patients with Crohn’s disease patients have increased activation of SMAD2 and SMAD3 in response to TGFβ1, decreased expression of SMAD7, and increased collagen production143. Therefore, the dysregulation and increased responsivity to TGFβ of myofibroblasts in patients with IBD necessitates ongoing monitoring for fibrosis and strictures in patients given mongersen. Another factor to consider when increasing TGFβ responsivity is the potential for increased colon cancer risk.144
Future Directions
The increased insight into IBD pathogenesis has provided tremendous opportunities for therapeutic advances. Challenges in designing therapies for implicated IBD pathways have included trial design considerations (Table 2), and identifying the optimal pathway level (e.g. IL12 and IL23 vs IL17) and specificity (e.g. IL23p19 vs IL12p40) for intervening. As we refine our understanding of the cells that are affected by these agents, we would aim to block the pathways in cells that contribute to inflammation but not disrupt these same pathways in cells that downregulate inflammation or promote tissue healing (e.g. epithelial cells), through cell-specific targeting approaches. Intestinal-specific delivery systems may reduce adverse systemic events and achieve higher local drug concentrations, although they may be less effective in modulating dysregulated systemic immune mechanisms and treating extra-intestinal manifestations. It is also important to consider fine-tuning the threshold of immunomodulation. As opposed to the complete inhibition of dysregulated but essential pathways, simulating the levels of function in these pathways observed in protective, ‘loss-of-function’ genetic variants associated with IBD may provide a threshold of pathway function that balances reducing inflammation with minimizing adverse consequences. Finally, with the variety of emerging new therapies, it will be critical to examine immune responses pre- and post-therapy and to determine how to best integrate therapeutic decisions based on disease and patient phenotypes.
Table 2.
Insights From Clinical Trials of Patients With IBD
| Topic | Insights | Future Work |
|---|---|---|
| Patient selection | - Importance of baseline inflammation (biomarkers or endoscopic assessment of mucosal activity) and prior exposure to anti-TNF therapy for pathways | - Specific impact of prior anti-TNF
exposure (and of emerging immunological therapies) on various pathways
and implications for selection - Genetic and pathway expression enrichment in trial recruitment |
| Dose and Route selection | - Importance of assessing immunogenicity
and drug concentration/exposure with various regimens prior to
initiating phase 2 clinical trials - Small molecule inhibitors may help overcome issues with immunogenicity and pharmacokinetics |
- New drug delivery mechanisms that selectively target inflammatory pathways in specific areas of the gut (gut and site specific selectivity) and to specific cell subsets |
| Clinical End Point and Outcomes | - Timing of assessment important and
dependent on pathway involved - Clinical response more ideal for phase 2 trials - Consideration for composite end-points that accurately account for mucosal inflammation (i.e. CRP, fecal calprotectin, or endoscopic assessment) |
- Pathway specific end-points (e.g. reductions or alterations in pathway specific markers of inflammation to ensure high degree of on-target inhibition with minimal off-target effects, outcome stratification based on genetic variants) |
| Safety | - Off-target effects provide insight into molecular effects and pathway mechanisms | - Pre-defined safety concerns based on
known range of activity for pathway targeted to help better understand
safety monitoring parameters - More refined measures of immunological parameters |
CRP: C-reactive protein,
Supplementary Material
Sources of and Targets for IL17. A variety of cells within intestinal tissues can secrete IL17, including intraepithelial and lamina propria γδ T cells, Th17 cells and innate lymphoid cells. In mice IL17 production from lamina propria γδ T cells can occur independently of IL23, and therefore can persist despite IL23 blockade. IL17, in turn, acts on a number of targets, including epithelial cells, fibroblasts and neutrophils, to mediate protection against intestinal microbes. Importantly, despite the contribution of IL17 to intestinal inflammation through the regulation of such cells as neutrophils, blocking IL17 during intestinal inflammation actually leads to worsening of the inflammation. The essential role for IL17 on epithelial function during inflammatory conditions appears to be one reason accounting for the adverse outcomes with IL17 blockade.
Supplementary Table 1: Findings From Clinical Trials of Patients with IBD
Abbreviations
- DSS
Dextran sodium sulfate
- ILCs
innate lymphoid cells
- JAK
Janus-associated kinase
- STAT
signal transducer and activator of transcription
- Th
T helper
Footnotes
Disclosures: CA and PSD have no financial conflicts. CA is supported by DK099097 and DK062422 from the National Institutes of Health and the Crohn’s and Colitis Foundation of America. PSD is supported by a grant through the National Institutes of Health T32DK007202. SV has received consulting fees from AbbVie, MSD, Takeda, Ferring, Genentech/Roche, Shire, Pfizer Inc, Galapagos, Mundipharma, Hospira, Celgene, Second Genome, Eli Lilly and Janssen; research grants from AbbVie, MSD and Takeda; and speaker fees from AbbVie, MSD, Takeda, Ferring, Dr Falk Pharma, Hospira and Tillot. WJS reports personal fees from Kyowa Hakko Kirin, Millennium Pharmaceuticals, Celgene Cellular Therapeutics, Santarus, Salix Pharmaceuticals, Catabasis Pharmaceuticals, Vertex Pharmaceuticals, Warner Chilcott, Cosmo Pharmaceuticals, Ferring Pharmaceuticals, Sigmoid Biotechnologies, Tillotts Pharma, Am Pharma BV, Dr. August Wolff, Avaxia Biologics, Zyngenia, Ironwood Pharmaceuticals, Index Pharmaceuticals, Nestle, Lexicon Pharmaceuticals, UCB Pharma, Orexigen, Luitpold Pharmaceuticals, Baxter Healthcare, Ferring Research Institute, Novo Nordisk, Mesoblast Inc., Shire, Ardelyx Inc., Actavis, Seattle Genetics, MedImmune (AstraZeneca), Actogenix NV, Lipid Therapeutics Gmbh, Eisai, Qu Biologics, Toray Industries Inc,, Teva Pharmaceuticals, Eli Lilly, Chiasma, TiGenix, Adherion Therapeutics, Immune Pharmaceuticals, Celgene, Arena Pharmaceuticals, personal fees from Ambrx Inc., Akros Pharma, Vascular Biogenics, Theradiag, Forward Pharma, Regeneron, Galapagos, Seres Health, Ritter Pharmaceuticals, Theravance, Palatin, Biogen, University of Western Ontario (owner of Robarts Clinical Trials); grants and personal fees from Prometheus Laboratories, AbbVie, Gilead Sciences, Boehringer Ingelheim, Amgen, Takeda, Atlantic Pharmaceuticals, Bristol-Myers Squibb Genentech, GlaxoSmithKline, Pfizer, Nutrition Science Partners, Receptos, Amgen; grants, personal fees and non-financial support from Janssen; grants from Broad Foundation, American College of Gastroenterology, Exact Sciences, outside the submitted work. In addition, WJS has a patent Use of topical azathioprine to treat inflammatory bowel disorders (US 5,691,343) issued, a patent Topical formulations of azathioprine to treat inflammatory bowel disorders (US 5,905,081) issued, a patent Colonic delivery of nicotine to treat inflammatory bowel disease (South African patent 97/1020; US 5,846,983, 5,889,028, and 6,166,044; Mexico patent 209636; Europe patents 0954337 and 893998; Hong Kong patent HK1019043; China patent ZL97192177; Czech patent 293616; Canada patent 2,246,235) issued, a patent Use of azathioprine to treat Crohn’s disease (US 5,733,915) issued, a patent Azathioprine compositions for colonic administration (New Zealand patent 306062; Singapore patent 45647; Australia patent 707168; Czech patent 290428) issued, a patent Intestinal absorption of nicotine to treat nicotine responsive conditions (Australia patent 718052; US 6,238,689) issued, a patent Use of topical azathioprine and thioguanine to treat colorectal adenomas (US 6,166,024) issued, a patent Enema and enterically-coated oral dosage forms of azathioprine (US 6,432,967) issued, a patent Pharmaceutical composition for the treatment of inflammatory bowel disease (US 7341741) issued, a patent Intestinal absorption of nicotine to treat nicotine responsive conditions (Canada patent 2,260,909) issued, and a patent Obesity treatment and device (US 7,803,195 B2) issued.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Dulai PS, Siegel CA. The risk of malignancy associated with the use of biological agents in patients with inflammatory bowel disease. Gastroenterol Clin North Am. 2014;43:525–41. doi: 10.1016/j.gtc.2014.05.010. [DOI] [PubMed] [Google Scholar]
- 2.Dulai PS, Thompson KD, Blunt HB, et al. Risks of serious infection or lymphoma with anti-tumor necrosis factor therapy for pediatric inflammatory bowel disease: a systematic review. Clin Gastroenterol Hepatol. 2014;12:1443–51. doi: 10.1016/j.cgh.2014.01.021. [DOI] [PubMed] [Google Scholar]
- 3.Ding NS, Hart A, De Cruz P. Systematic review: predicting and optimising response to anti-TNF therapy in Crohn’s disease - algorithm for practical management. Aliment Pharmacol Ther. 2016;43:30–51. doi: 10.1111/apt.13445. [DOI] [PubMed] [Google Scholar]
- 4.Abraham C, Cho JH. Inflammatory bowel disease. N Engl J Med. 2009;361:2066–78. doi: 10.1056/NEJMra0804647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dambacher J, Beigel F, Zitzmann K, et al. The role of the novel Th17 cytokine IL-26 in intestinal inflammation. Gut. 2009;58:1207–17. doi: 10.1136/gut.2007.130112. [DOI] [PubMed] [Google Scholar]
- 6.Meller S, Di Domizio J, Voo KS, et al. T(H)17 cells promote microbial killing and innate immune sensing of DNA via interleukin 26. Nat Immunol. 2015;16:970–9. doi: 10.1038/ni.3211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gerlach K, Hwang Y, Nikolaev A, et al. TH9 cells that express the transcription factor PU. 1 drive T cell-mediated colitis via IL-9 receptor signaling in intestinal epithelial cells. Nat Immunol. 2014;15:676–86. doi: 10.1038/ni.2920. [DOI] [PubMed] [Google Scholar]
- 8.Gaffen SL, Jain R, Garg AV, et al. The IL-23-IL-17 immune axis: from mechanisms to therapeutic testing. Nat Rev Immunol. 2014;14:585–600. doi: 10.1038/nri3707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Patel DD, Kuchroo VK. Th17 Cell Pathway in Human Immunity: Lessons from Genetics and Therapeutic Interventions. Immunity. 2015;43:1040–51. doi: 10.1016/j.immuni.2015.12.003. [DOI] [PubMed] [Google Scholar]
- 10.Donaldson DS, Bradford BM, Artis D, et al. Reciprocal regulation of lymphoid tissue development in the large intestine by IL-25 and IL-23. Mucosal Immunol. 2015;8:582–95. doi: 10.1038/mi.2014.90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Abraham C, Cho J. Interleukin-23/Th17 pathways and inflammatory bowel disease. Inflamm Bowel Dis. 2009;15:1090–1100. doi: 10.1002/ibd.20894. [DOI] [PubMed] [Google Scholar]
- 12.Shih VF, Cox J, Kljavin NM, et al. Homeostatic IL-23 receptor signaling limits Th17 response through IL-22-mediated containment of commensal microbiota. Proc Natl Acad Sci U S A. 2014;111:13942–7. doi: 10.1073/pnas.1323852111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Macho-Fernandez E, Koroleva EP, Spencer CM, et al. Lymphotoxin beta receptor signaling limits mucosal damage through driving IL-23 production by epithelial cells. Mucosal Immunol. 2015;8:403–13. doi: 10.1038/mi.2014.78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kvedaraite E, Lourda M, Idestrom M, et al. Tissue-infiltrating neutrophils represent the main source of IL-23 in the colon of patients with IBD. Gut. 2016;65:1632–1641. doi: 10.1136/gutjnl-2014-309014. [DOI] [PubMed] [Google Scholar]
- 15.Friedrich M, Diegelmann J, Schauber J, et al. Intestinal neuroendocrine cells and goblet cells are mediators of IL-17A-amplified epithelial IL-17C production in human inflammatory bowel disease. Mucosal Immunol. 2015;8:943–58. doi: 10.1038/mi.2014.124. [DOI] [PubMed] [Google Scholar]
- 16.Yang Y, Torchinsky MB, Gobert M, et al. Focused specificity of intestinal TH17 cells towards commensal bacterial antigens. Nature. 2014;510:152–6. doi: 10.1038/nature13279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kleinewietfeld M, Manzel A, Titze J, et al. Sodium chloride drives autoimmune disease by the induction of pathogenic TH17 cells. Nature. 2013;496:518–22. doi: 10.1038/nature11868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wu C, Yosef N, Thalhamer T, et al. Induction of pathogenic TH17 cells by inducible salt-sensing kinase SGK1. Nature. 2013;496:513–7. doi: 10.1038/nature11984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Qiu J, Heller JJ, Guo X, et al. The aryl hydrocarbon receptor regulates gut immunity through modulation of innate lymphoid cells. Immunity. 2012;36:92–104. doi: 10.1016/j.immuni.2011.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Veldhoen M, Hirota K, Westendorf AM, et al. The aryl hydrocarbon receptor links TH17-cell-mediated autoimmunity to environmental toxins. Nature. 2008;453:106–9. doi: 10.1038/nature06881. [DOI] [PubMed] [Google Scholar]
- 21.Atarashi K, Tanoue T, Ando M, et al. Th17 Cell Induction by Adhesion of Microbes to Intestinal Epithelial Cells. Cell. 2015;163:367–80. doi: 10.1016/j.cell.2015.08.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wiekowski MT, Leach MW, Evans EW, et al. Ubiquitous transgenic expression of the IL-23 subunit p19 induces multiorgan inflammation, runting, infertility, and premature death. J Immunol. 2001;166:7563–70. doi: 10.4049/jimmunol.166.12.7563. [DOI] [PubMed] [Google Scholar]
- 23.Elson CO, Cong Y, Weaver CT, et al. Monoclonal anti-interleukin 23 reverses active colitis in a T cell-mediated model in mice. Gastroenterology. 2007;132:2359–70. doi: 10.1053/j.gastro.2007.03.104. [DOI] [PubMed] [Google Scholar]
- 24.Yen D, Cheung J, Scheerens H, et al. IL-23 is essential for T cell-mediated colitis and promotes inflammation via IL-17 and IL-6. J Clin Invest. 2006;116:1310–6. doi: 10.1172/JCI21404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kullberg MC, Jankovic D, Feng CG, et al. IL-23 plays a key role in Helicobacter hepaticus-induced T cell-dependent colitis. J Exp Med. 2006;203:2485–94. doi: 10.1084/jem.20061082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Izcue A, Hue S, Buonocore S, et al. Interleukin-23 restrains regulatory T cell activity to drive T cell-dependent colitis. Immunity. 2008;28:559–70. doi: 10.1016/j.immuni.2008.02.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Uhlig HH, McKenzie BS, Hue S, et al. Differential activity of IL-12 and IL-23 in mucosal and systemic innate immune pathology. Immunity. 2006;25:309–18. doi: 10.1016/j.immuni.2006.05.017. [DOI] [PubMed] [Google Scholar]
- 28.O’Connor W, Jr, Kamanaka M, Booth CJ, et al. A protective function for interleukin 17A in T cell-mediated intestinal inflammation. Nat Immunol. 2009;10:603–9. doi: 10.1038/ni.1736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sugimoto K, Ogawa A, Mizoguchi E, et al. IL-22 ameliorates intestinal inflammation in a mouse model of ulcerative colitis. J Clin Invest. 2008;118:534–44. doi: 10.1172/JCI33194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zenewicz LA, Yancopoulos GD, Valenzuela DM, et al. Innate and adaptive interleukin-22 protects mice from inflammatory bowel disease. Immunity. 2008;29:947–57. doi: 10.1016/j.immuni.2008.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Huber S, Gagliani N, Zenewicz LA, et al. The IL-22—IL-22BP axis is regulated by the inflammasome and modulates tumorigenesis in the intestine. Nature. 2012;491:259–263. doi: 10.1038/nature11535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Eken A, Singh AK, Treuting PM, et al. IL-23R+ innate lymphoid cells induce colitis via interleukin-22-dependent mechanism. Mucosal Immunol. 2014;7:143–54. doi: 10.1038/mi.2013.33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cox JH, Kljavin NM, Ota N, et al. Opposing consequences of IL-23 signaling mediated by innate and adaptive cells in chemically induced colitis in mice. Mucosal Immunol. 2012;5:99–109. doi: 10.1038/mi.2011.54. [DOI] [PubMed] [Google Scholar]
- 34.Geremia A, Arancibia-Carcamo CV, Fleming MP, et al. IL-23-responsive innate lymphoid cells are increased in inflammatory bowel disease. J Exp Med. 2011;208:1127–33. doi: 10.1084/jem.20101712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kleinschek MA, Boniface K, Sadekova S, et al. Circulating and gut-resident human Th17 cells express CD161 and promote intestinal inflammation. J Exp Med. 2009;206:525–34. doi: 10.1084/jem.20081712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Barrett JC, Hansoul S, Nicolae DL, et al. Genome-wide association defines more than 30 distinct susceptibility loci for Crohn’s disease. Nat Genet. 2008;40:955–962. doi: 10.1038/NG.175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Jostins L, Ripke S, Weersma RK, et al. Host-microbe interactions have shaped the genetic architecture of inflammatory bowel disease. Nature. 2012;491:119–24. doi: 10.1038/nature11582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Duerr RH, Taylor KD, Brant SR, et al. A Genome-Wide Association Study Identifies IL23R as an Inflammatory Bowel Disease Gene. Science. 2006;314:1461–1463. doi: 10.1126/science.1135245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sarin R, Wu X, Abraham C. Inflammatory disease protective R381Q IL23 receptor polymorphism results in decreased primary CD4+ and CD8+ human T-cell functional responses. Proceedings of the National Academy of Sciences. 2011;108:9560–9565. doi: 10.1073/pnas.1017854108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Pidasheva S, Trifari S, Phillips A, et al. Functional studies on the IBD susceptibility gene IL23R implicate reduced receptor function in the protective genetic variant R381Q. PLoS One. 2011;6:e25038. doi: 10.1371/journal.pone.0025038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Di Meglio P, Di Cesare A, Laggner U, et al. The IL23R R381Q gene variant protects against immune-mediated diseases by impairing IL-23-induced Th17 effector response in humans. PLoS One. 2011;6:e17160. doi: 10.1371/journal.pone.0017160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ahern PP, Schiering C, Buonocore S, et al. Interleukin-23 Drives Intestinal Inflammation through Direct Activity on T Cells. Immunity. 2010;33:279–288. doi: 10.1016/j.immuni.2010.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Papp KA, Menter A, Sofen H, et al. Efficacy and Safety of Different Dose Regimens of a Selective IL-23p19 Inhibitor (BI 655066) Compared with Ustekinumab in Patients with Moderate-to-Severe Plaque Psoriasis with and without Psoriatic Arthritis [abstract #2144] Arthritis Rheumatol. 2015;67(suppl 10) [Google Scholar]
- 44.Mannon PJ, Fuss IJ, Mayer L, et al. Anti-interleukin-12 antibody for active Crohn’s disease. N Engl J Med. 2004;351:2069–79. doi: 10.1056/NEJMoa033402. [DOI] [PubMed] [Google Scholar]
- 45.Sandborn WJ, Feagan BG, Fedorak RN, et al. A randomized trial of Ustekinumab, a human interleukin-12/23 monoclonal antibody, in patients with moderate-to-severe Crohn’s disease. Gastroenterology. 2008;135:1130–41. doi: 10.1053/j.gastro.2008.07.014. [DOI] [PubMed] [Google Scholar]
- 46.Sandborn WJ, Gasink C, Gao LL, et al. Ustekinumab induction and maintenance therapy in refractory Crohn’s disease. N Engl J Med. 2012;367:1519–28. doi: 10.1056/NEJMoa1203572. [DOI] [PubMed] [Google Scholar]
- 47.Feagan BG, Sandborn WJ, Gasink C, et al. Ustekinumab as Induction and Maintenance Therapy for Crohn’s Disease. N Engl J Med. 2016;375:1946–1960. doi: 10.1056/NEJMoa1602773. [DOI] [PubMed] [Google Scholar]
- 48.Panaccione R, Sandborn WJ, Gordon GL, et al. Briakinumab for treatment of Crohn’s disease: results of a randomized trial. Inflamm Bowel Dis. 2015;21:1329–40. doi: 10.1097/MIB.0000000000000366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Fuss IJ, Neurath M, Boirivant M, et al. Disparate CD4+ lamina propria (LP) lymphokine secretion profiles in inflammatory bowel disease. Crohn’s disease LP cells manifest increased secretion of IFN-gamma, whereas ulcerative colitis LP cells manifest increased secretion of IL-5. J Immunol. 1996;157:1261–70. [PubMed] [Google Scholar]
- 50.Fais S, Capobianchi MR, Silvestri M, et al. Interferon expression in Crohn’s disease patients: increased interferon-gamma and -alpha mRNA in the intestinal lamina propria mononuclear cells. J Interferon Res. 1994;14:235–8. doi: 10.1089/jir.1994.14.235. [DOI] [PubMed] [Google Scholar]
- 51.Hommes DW, Mikhajlova TL, Stoinov S, et al. Fontolizumab, a humanised anti-interferon gamma antibody, demonstrates safety and clinical activity in patients with moderate to severe Crohn’s disease. Gut. 2006;55:1131–7. doi: 10.1136/gut.2005.079392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Reinisch W, Hommes DW, Van Assche G, et al. A dose escalating, placebo controlled, double blind, single dose and multidose, safety and tolerability study of fontolizumab, a humanised anti-interferon gamma antibody, in patients with moderate to severe Crohn’s disease. Gut. 2006;55:1138–44. doi: 10.1136/gut.2005.079434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Reinisch W, de Villiers W, Bene L, et al. Fontolizumab in moderate to severe Crohn’s disease: a phase 2, randomized, double-blind, placebo-controlled, multiple-dose study. Inflamm Bowel Dis. 2010;16:233–42. doi: 10.1002/ibd.21038. [DOI] [PubMed] [Google Scholar]
- 54.Sheikh SZ, Matsuoka K, Kobayashi T, et al. Cutting edge: IFN-gamma is a negative regulator of IL-23 in murine macrophages and experimental colitis. J Immunol. 2010;184:4069–73. doi: 10.4049/jimmunol.0903600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Feagan BG, Sandborn W, Panés J, et al. Efficacy and Safety of Induction Therapy With the Selective IL-23 Inhibitor BI 655066, in Patients With Moderate-to-Severe Crohn’s Disease: Results of a Randomized, Double-Blind, Placebo-Controlled Phase II Study. Gastroenterology. 2016;150:S1266. [Google Scholar]
- 56.Sands BE, Chen J, Penney M, et al. Initial Evaluation of MEDI2070 (Specific Anti-IL-23 Antibody) in Patients With Active Crohn’s Disease Who Have Failed Anti-TNF Antibody Therapy: A Randomized, Double-Blind Placebo-Controlled Phase 2A Induction Study. Gastroenterology. 2015;148:S163–S164. [Google Scholar]
- 57.Hueber W, Sands BE, Lewitzky S, et al. Secukinumab, a human anti-IL-17A monoclonal antibody, for moderate to severe Crohn’s disease: unexpected results of a randomised, double-blind placebo-controlled trial. Gut. 2012;61:1693–700. doi: 10.1136/gutjnl-2011-301668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Mozaffari S, Nikfar S, Abdollahi M. Inflammatory bowel disease therapies discontinued between 2009 and 2014. Expert Opin Investig Drugs. 2015;24:949–56. doi: 10.1517/13543784.2015.1035432. [DOI] [PubMed] [Google Scholar]
- 59.Ogawa A, Andoh A, Araki Y, et al. Neutralization of interleukin-17 aggravates dextran sulfate sodium-induced colitis in mice. Clin Immunol. 2004;110:55–62. doi: 10.1016/j.clim.2003.09.013. [DOI] [PubMed] [Google Scholar]
- 60.Zhang Z, Zheng M, Bindas J, et al. Critical role of IL-17 receptor signaling in acute TNBS-induced colitis. Inflamm Bowel Dis. 2006;12:382–8. doi: 10.1097/01.MIB.0000218764.06959.91. [DOI] [PubMed] [Google Scholar]
- 61.Maxwell JR, Zhang Y, Brown WA, et al. Differential Roles for Interleukin-23 and Interleukin-17 in Intestinal Immunoregulation. Immunity. 2015;43:739–50. doi: 10.1016/j.immuni.2015.08.019. [DOI] [PubMed] [Google Scholar]
- 62.Lee JS, Tato CM, Joyce-Shaikh B, et al. Interleukin-23-Independent IL-17 Production Regulates Intestinal Epithelial Permeability. Immunity. 2015;43:727–38. doi: 10.1016/j.immuni.2015.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.McInnes IB, Mease PJ, Kirkham B, et al. Secukinumab, a human anti-interleukin-17A monoclonal antibody, in patients with psoriatic arthritis (FUTURE 2): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet. 2015;386:1137–46. doi: 10.1016/S0140-6736(15)61134-5. [DOI] [PubMed] [Google Scholar]
- 64.Sherlock JP, Joyce-Shaikh B, Turner SP, et al. IL-23 induces spondyloarthropathy by acting on ROR-gammat+ CD3+CD4−CD8− entheseal resident T cells. Nat Med. 2012;18:1069–76. doi: 10.1038/nm.2817. [DOI] [PubMed] [Google Scholar]
- 65.Ota N, Wong K, Valdez PA, et al. IL-22 bridges the lymphotoxin pathway with the maintenance of colonic lymphoid structures during infection with Citrobacter rodentium. Nat Immunol. 2011;12:941–8. doi: 10.1038/ni.2089. [DOI] [PubMed] [Google Scholar]
- 66.Tumanov AV, Koroleva EP, Guo X, et al. Lymphotoxin controls the IL-22 protection pathway in gut innate lymphoid cells during mucosal pathogen challenge. Cell Host Microbe. 2011;10:44–53. doi: 10.1016/j.chom.2011.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Wang Y, Koroleva EP, Kruglov AA, et al. Lymphotoxin beta receptor signaling in intestinal epithelial cells orchestrates innate immune responses against mucosal bacterial infection. Immunity. 2010;32:403–13. doi: 10.1016/j.immuni.2010.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Mizuno S, Mikami Y, Kamada N, et al. Cross-talk between RORgammat+ innate lymphoid cells and intestinal macrophages induces mucosal IL-22 production in Crohn’s disease. Inflamm Bowel Dis. 2014;20:1426–34. doi: 10.1097/MIB.0000000000000105. [DOI] [PubMed] [Google Scholar]
- 69.Pearson C, Thornton EE, McKenzie B, et al. ILC3 GM-CSF production and mobilisation orchestrate acute intestinal inflammation. Elife. 2016;5:e10066. doi: 10.7554/eLife.10066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Buonocore S, Ahern PP, Uhlig HH, et al. Innate lymphoid cells drive interleukin-23-dependent innate intestinal pathology. Nature. 2010;464:1371–5. doi: 10.1038/nature08949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Mukasa R, Balasubramani A, Lee YK, et al. Epigenetic instability of cytokine and transcription factor gene loci underlies plasticity of the T helper 17 cell lineage. Immunity. 2010;32:616–27. doi: 10.1016/j.immuni.2010.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Lee YK, Turner H, Maynard CL, et al. Late developmental plasticity in the T helper 17 lineage. Immunity. 2009;30:92–107. doi: 10.1016/j.immuni.2008.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Esplugues E, Huber S, Gagliani N, et al. Control of TH17 cells occurs in the small intestine. Nature. 2011;475:514–8. doi: 10.1038/nature10228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Gagliani N, Amezcua Vesely MC, Iseppon A, et al. Th17 cells transdifferentiate into regulatory T cells during resolution of inflammation. Nature. 2015;523:221–5. doi: 10.1038/nature14452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Harbour SN, Maynard CL, Zindl CL, et al. Th17 cells give rise to Th1 cells that are required for the pathogenesis of colitis. Proc Natl Acad Sci U S A. 2015;112:7061–6. doi: 10.1073/pnas.1415675112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.McGeachy MJ, Bak-Jensen KS, Chen Y, et al. TGF-beta and IL-6 drive the production of IL-17 and IL-10 by T cells and restrain T(H)-17 cell-mediated pathology. Nat Immunol. 2007;8:1390–7. doi: 10.1038/ni1539. [DOI] [PubMed] [Google Scholar]
- 77.Cohen CJ, Crome SQ, MacDonald KG, et al. Human Th1 and Th17 cells exhibit epigenetic stability at signature cytokine and transcription factor loci. J Immunol. 2011;187:5615–26. doi: 10.4049/jimmunol.1101058. [DOI] [PubMed] [Google Scholar]
- 78.Nistala K, Adams S, Cambrook H, et al. Th17 plasticity in human autoimmune arthritis is driven by the inflammatory environment. Proc Natl Acad Sci U S A. 2010;107:14751–6. doi: 10.1073/pnas.1003852107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Hirota K, Duarte JH, Veldhoen M, et al. Fate mapping of IL-17-producing T cells in inflammatory responses. Nat Immunol. 2011;12:255–63. doi: 10.1038/ni.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Ghoreschi K, Laurence A, Yang XP, et al. Generation of pathogenic T(H)17 cells in the absence of TGF-beta signalling. Nature. 2010;467:967–71. doi: 10.1038/nature09447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Lee Y, Awasthi A, Yosef N, et al. Induction and molecular signature of pathogenic TH17 cells. Nat Immunol. 2012;13:991–9. doi: 10.1038/ni.2416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Codarri L, Gyulveszi G, Tosevski V, et al. RORgammat drives production of the cytokine GM-CSF in helper T cells, which is essential for the effector phase of autoimmune neuroinflammation. Nat Immunol. 2011;12:560–7. doi: 10.1038/ni.2027. [DOI] [PubMed] [Google Scholar]
- 83.Ramesh R, Kozhaya L, McKevitt K, et al. Pro-inflammatory human Th17 cells selectively express P-glycoprotein and are refractory to glucocorticoids. J Exp Med. 2014;211:89–104. doi: 10.1084/jem.20130301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Griseri T, Arnold IC, Pearson C, et al. Granulocyte Macrophage Colony-Stimulating Factor-Activated Eosinophils Promote Interleukin-23 Driven Chronic Colitis. Immunity. 2015;43:187–99. doi: 10.1016/j.immuni.2015.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Yosef N, Shalek AK, Gaublomme JT, et al. Dynamic regulatory network controlling TH17 cell differentiation. Nature. 2013;496:461–8. doi: 10.1038/nature11981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Gaublomme JT, Yosef N, Lee Y, et al. Single-Cell Genomics Unveils Critical Regulators of Th17 Cell Pathogenicity. Cell. 2015;163:1400–12. doi: 10.1016/j.cell.2015.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Ciofani M, Madar A, Galan C, et al. A validated regulatory network for Th17 cell specification. Cell. 2012;151:289–303. doi: 10.1016/j.cell.2012.09.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Huang W, Thomas B, Flynn RA, et al. DDX5 and its associated lncRNA Rmrp modulate TH17 cell effector functions. Nature. 2015;528:517–22. doi: 10.1038/nature16193. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 89.Krausgruber T, Schiering C, Adelmann K, et al. T-bet is a key modulator of IL-23-driven pathogenic CD4(+) T cell responses in the intestine. Nat Commun. 2016;7:11627. doi: 10.1038/ncomms11627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Wang C, Yosef N, Gaublomme J, et al. CD5L/AIM Regulates Lipid Biosynthesis and Restrains Th17 Cell Pathogenicity. Cell. 2015;163:1413–27. doi: 10.1016/j.cell.2015.10.068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Jain R, Chen Y, Kanno Y, et al. Interleukin-23-Induced Transcription Factor Blimp-1 Promotes Pathogenicity of T Helper 17 Cells. Immunity. 2016;44:131–42. doi: 10.1016/j.immuni.2015.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Wang Y, Godec J, Ben-Aissa K, et al. The transcription factors T-bet and Runx are required for the ontogeny of pathogenic interferon-gamma-producing T helper 17 cells. Immunity. 2014;40:355–66. doi: 10.1016/j.immuni.2014.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Withers DR, Hepworth MR, Wang X, et al. Transient inhibition of ROR-gammat therapeutically limits intestinal inflammation by reducing TH17 cells and preserving group 3 innate lymphoid cells. Nat Med. 2016;22:319–23. doi: 10.1038/nm.4046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Leppkes M, Becker C, Ivanov II, et al. RORgamma-expressing Th17 cells induce murine chronic intestinal inflammation via redundant effects of IL-17A and IL-17F. Gastroenterology. 2009;136:257–67. doi: 10.1053/j.gastro.2008.10.018. [DOI] [PubMed] [Google Scholar]
- 95.Inoue S, Matsumoto T, Iida M, et al. Characterization of cytokine expression in the rectal mucosa of ulcerative colitis: correlation with disease activity. Am J Gastroenterol. 1999;94:2441–6. doi: 10.1111/j.1572-0241.1999.01372.x. [DOI] [PubMed] [Google Scholar]
- 96.Mannon P, Reinisch W. Interleukin 13 and its role in gut defence and inflammation. Gut. 2012;61:1765–73. doi: 10.1136/gutjnl-2012-303461. [DOI] [PubMed] [Google Scholar]
- 97.Biancheri P, Di Sabatino A, Ammoscato F, et al. Absence of a role for interleukin-13 in inflammatory bowel disease. Eur J Immunol. 2014;44:370–85. doi: 10.1002/eji.201343524. [DOI] [PubMed] [Google Scholar]
- 98.Fuss IJ, Heller F, Boirivant M, et al. Nonclassical CD1d-restricted NK T cells that produce IL-13 characterize an atypical Th2 response in ulcerative colitis. J Clin Invest. 2004;113:1490–7. doi: 10.1172/JCI19836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Heller F, Florian P, Bojarski C, et al. Interleukin-13 is the key effector Th2 cytokine in ulcerative colitis that affects epithelial tight junctions, apoptosis, and cell restitution. Gastroenterology. 2005;129:550–64. doi: 10.1016/j.gastro.2005.05.002. [DOI] [PubMed] [Google Scholar]
- 100.Fichtner-Feigl S, Fuss IJ, Young CA, et al. Induction of IL-13 triggers TGF-beta1-dependent tissue fibrosis in chronic 2,4,6-trinitrobenzene sulfonic acid colitis. J Immunol. 2007;178:5859–70. doi: 10.4049/jimmunol.178.9.5859. [DOI] [PubMed] [Google Scholar]
- 101.Heller F, Fuss IJ, Nieuwenhuis EE, et al. Oxazolone colitis, a Th2 colitis model resembling ulcerative colitis, is mediated by IL-13-producing NK-T cells. Immunity. 2002;17:629–38. doi: 10.1016/s1074-7613(02)00453-3. [DOI] [PubMed] [Google Scholar]
- 102.Danese S, Rudzinski J, Brandt W, et al. Tralokinumab for moderate-to-severe UC: a randomised, double-blind, placebo-controlled, phase IIa study. Gut. 2015;64:243–9. doi: 10.1136/gutjnl-2014-308004. [DOI] [PubMed] [Google Scholar]
- 103.Reinisch W, Panes J, Khurana S, et al. Anrukinzumab, an anti-interleukin 13 monoclonal antibody, in active UC: efficacy and safety from a phase IIa randomised multicentre study. Gut. 2015;64:894–900. doi: 10.1136/gutjnl-2014-308337. [DOI] [PubMed] [Google Scholar]
- 104.Waldner MJ, Neurath MF. Master regulator of intestinal disease: IL-6 in chronic inflammation and cancer development. Semin Immunol. 2014;26:75–9. doi: 10.1016/j.smim.2013.12.003. [DOI] [PubMed] [Google Scholar]
- 105.Ito H, Takazoe M, Fukuda Y, et al. A pilot randomized trial of a human anti-interleukin-6 receptor monoclonal antibody in active Crohn’s disease. Gastroenterology. 2004;126:989–96. doi: 10.1053/j.gastro.2004.01.012. [DOI] [PubMed] [Google Scholar]
- 106.Danese S, Vermeire S, Hellstern P, et al. Results of Andante, a Randomized Clinical Study With an Anti-IL6 Antibody (PF-04236921) in Subjects With Crohn’s Disease Who Are Anti-TNF Inadequate Responders. Gastroenterology. 2016;150:S155. [Google Scholar]
- 107.Smolen JS, Schoels MM, Nishimoto N, et al. Consensus statement on blocking the effects of interleukin-6 and in particular by interleukin-6 receptor inhibition in rheumatoid arthritis and other inflammatory conditions. Ann Rheum Dis. 2013;72:482–92. doi: 10.1136/annrheumdis-2012-202469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Kuhn KA, Manieri NA, Liu TC, et al. IL-6 stimulates intestinal epithelial proliferation and repair after injury. PLoS One. 2014;9:e114195. doi: 10.1371/journal.pone.0114195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.O’Shea JJ, Schwartz DM, Villarino AV, et al. The JAK-STAT pathway: impact on human disease and therapeutic intervention. Annu Rev Med. 2015;66:311–28. doi: 10.1146/annurev-med-051113-024537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Sandborn WJ, Ghosh S, Panes J, et al. Tofacitinib, an oral Janus kinase inhibitor, in active ulcerative colitis. N Engl J Med. 2012;367:616–24. doi: 10.1056/NEJMoa1112168. [DOI] [PubMed] [Google Scholar]
- 111.Sandborn W, Sands BE, D’Haens GR, et al. Efficacy and Safety of Oral Tofacitinib As Induction Therapy in Patients With Moderate to Severe Ulcerative Colitis: Results From Two Phase 3 Randomized Controlled Trials. Gastroenterology. 2016;150:S157. [Google Scholar]
- 112.Sandborn WJ, Ghosh S, Panes J, et al. A Phase 2 Study of Tofacitinib, an Oral Janus Kinase Inhibitor, in Patients With Crohn’s Disease. Clin Gastroenterol Hepatol. 2014;12:1485–1493. doi: 10.1016/j.cgh.2014.01.029. [DOI] [PubMed] [Google Scholar]
- 113.Panés J, Sandborn W, Schreiber S, et al. Efficacy and Safety of Tofacitinib for Oral Induction Therapy in Patients With Moderate to Severe Crohn’s Disease: Results of a Phase 2B Randomized Placebo-Controlled Trial. Gastroenterology. 2016;150:S182–S183. [Google Scholar]
- 114.Vermeire S, Schreiber S, Petryka R, et al. Filgotinib (GLPG0634), an Oral JAK1 Selective Inhibitor, Induces Clinical Remission in Patients With Moderate-to-Severe Crohn’s Disease: Results From the Phase 2 FITZROY Study Interim Analysis. Gastroenterology. 2016;150:S1267. [Google Scholar]
- 115.Kumar N, Mishra J, Narang VS, et al. Janus kinase 3 regulates interleukin 2-induced mucosal wound repair through tyrosine phosphorylation of villin. J Biol Chem. 2007;282:30341–5. doi: 10.1074/jbc.C600319200. [DOI] [PubMed] [Google Scholar]
- 116.Mishra J, Verma RK, Alpini G, et al. Role of Janus kinase 3 in mucosal differentiation and predisposition to colitis. J Biol Chem. 2013;288:31795–806. doi: 10.1074/jbc.M113.504126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Hainzl E, Stockinger S, Rauch I, et al. Intestinal Epithelial Cell Tyrosine Kinase 2 Transduces IL-22 Signals To Protect from Acute Colitis. J Immunol. 2015;195:5011–24. doi: 10.4049/jimmunol.1402565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Koon HW, Zhao D, Zhan Y, et al. Substance P stimulates cyclooxygenase-2 and prostaglandin E2 expression through JAK-STAT activation in human colonic epithelial cells. J Immunol. 2006;176:5050–9. doi: 10.4049/jimmunol.176.8.5050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Yamaoka T, Yan F, Cao H, et al. Transactivation of EGF receptor and ErbB2 protects intestinal epithelial cells from TNF-induced apoptosis. Proc Natl Acad Sci U S A. 2008;105:11772–7. doi: 10.1073/pnas.0801463105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Kim HJ, Hart J, Knatz N, et al. Janus kinase 3 down-regulates lipopolysaccharide-induced IL-1 beta-converting enzyme activation by autocrine IL-10. J Immunol. 2004;172:4948–55. doi: 10.4049/jimmunol.172.8.4948. [DOI] [PubMed] [Google Scholar]
- 121.Pattison MJ, Mackenzie KF, Arthur JS. Inhibition of JAKs in macrophages increases lipopolysaccharide-induced cytokine production by blocking IL-10-mediated feedback. J Immunol. 2012;189:2784–92. doi: 10.4049/jimmunol.1200310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Wang H, Brown J, Gao S, et al. The role of JAK-3 in regulating TLR-mediated inflammatory cytokine production in innate immune cells. J Immunol. 2013;191:1164–74. doi: 10.4049/jimmunol.1203084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Hedl M, Proctor DD, Abraham C. JAK2 Disease-Risk Variants are Gain of Function and JAK Signaling Threshold Determines Innate Receptor-induced Proinflammatory Cytokine Secretion in Macrophages. Journal of Immunology. 2016;197:3695–3704. doi: 10.4049/jimmunol.1600845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Yarilina A, Xu K, Chan C, et al. Regulation of inflammatory responses in tumor necrosis factor-activated and rheumatoid arthritis synovial macrophages by JAK inhibitors. Arthritis Rheum. 2012;64:3856–66. doi: 10.1002/art.37691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Ley K, Rivera-Nieves J, Sandborn WJ, et al. Integrin-based therapeutics: biological basis, clinical use and new drugs. Nat Rev Drug Discov. 2016;15:173–83. doi: 10.1038/nrd.2015.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Rivera-Nieves J. Strategies that target leukocyte traffic in inflammatory bowel diseases: recent developments. Curr Opin Gastroenterol. 2015;31:441–8. doi: 10.1097/MOG.0000000000000218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Baeyens A, Fang V, Chen C, et al. Exit Strategies: S1P Signaling and T Cell Migration. Trends Immunol. 2015;36:778–87. doi: 10.1016/j.it.2015.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Sandborn WJ, Feagan BG, Wolf DC, et al. Ozanimod Induction and Maintenance Treatment for Ulcerative Colitis. N Engl J Med. 2016;374:1754–62. doi: 10.1056/NEJMoa1513248. [DOI] [PubMed] [Google Scholar]
- 129.Travis MA, Sheppard D. TGF-beta activation and function in immunity. Annu Rev Immunol. 2014;32:51–82. doi: 10.1146/annurev-immunol-032713-120257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Konkel JE, Maruyama T, Carpenter AC, et al. Control of the development of CD8alphaalpha+ intestinal intraepithelial lymphocytes by TGF-beta. Nat Immunol. 2011;12:312–9. doi: 10.1038/ni.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Cortez VS, Cervantes-Barragan L, Robinette ML, et al. Transforming Growth Factor-beta Signaling Guides the Differentiation of Innate Lymphoid Cells in Salivary Glands. Immunity. 2016;44:1127–39. doi: 10.1016/j.immuni.2016.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Reis BS, Rogoz A, Costa-Pinto FA, et al. Mutual expression of the transcription factors Runx3 and ThPOK regulates intestinal CD4(+) T cell immunity. Nat Immunol. 2013;14:271–80. doi: 10.1038/ni.2518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Shull MM, Ormsby I, Kier AB, et al. Targeted disruption of the mouse transforming growth factor-β1 gene results in multifocal inflammatory disease. Nature. 1992;359:693–699. doi: 10.1038/359693a0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Kulkarni AB, Huh C-G, Becker D, et al. Transforming growth factor β1 null mutation in mice causes excessive inflammatory response and early death. Proceedings of the National Academy of Sciences. 1993;90:770–774. doi: 10.1073/pnas.90.2.770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Li MO, Sanjabi S, Flavell RA. Transforming growth factor-beta controls development, homeostasis, and tolerance of T cells by regulatory T cell-dependent and -independent mechanisms. Immunity. 2006;25:455–71. doi: 10.1016/j.immuni.2006.07.011. [DOI] [PubMed] [Google Scholar]
- 136.Monteleone G, Kumberova A, Croft NM, et al. Blocking Smad7 restores TGF-beta1 signaling in chronic inflammatory bowel disease. J Clin Invest. 2001;108:601–9. doi: 10.1172/JCI12821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Boirivant M, Pallone F, Di Giacinto C, et al. Inhibition of Smad7 with a specific antisense oligonucleotide facilitates TGF-beta1-mediated suppression of colitis. Gastroenterology. 2006;131:1786–98. doi: 10.1053/j.gastro.2006.09.016. [DOI] [PubMed] [Google Scholar]
- 138.Babyatsky MW, Rossiter G, Podolsky DK. Expression of transforming growth factors alpha and beta in colonic mucosa in inflammatory bowel disease. Gastroenterology. 1996;110:975–84. doi: 10.1053/gast.1996.v110.pm8613031. [DOI] [PubMed] [Google Scholar]
- 139.Fantini MC, Rizzo A, Fina D, et al. Smad7 controls resistance of colitogenic T cells to regulatory T cell-mediated suppression. Gastroenterology. 2009;136:1308–16. doi: 10.1053/j.gastro.2008.12.053. [DOI] [PubMed] [Google Scholar]
- 140.Monteleone G, Neurath MF, Ardizzone S, et al. Mongersen, an oral SMAD7 antisense oligonucleotide, and Crohn’s disease. N Engl J Med. 2015;372:1104–13. doi: 10.1056/NEJMoa1407250. [DOI] [PubMed] [Google Scholar]
- 141.Peyrin-Biroulet L, Reinisch W, Colombel JF, et al. Clinical disease activity, C-reactive protein normalisation and mucosal healing in Crohn’s disease in the SONIC trial. Gut. 2014;63:88–95. doi: 10.1136/gutjnl-2013-304984. [DOI] [PubMed] [Google Scholar]
- 142.Li C, Kuemmerle JF. Mechanisms that mediate the development of fibrosis in patients with Crohn’s disease. Inflamm Bowel Dis. 2014;20:1250–8. doi: 10.1097/MIB.0000000000000043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Di Sabatino A, Jackson CL, Pickard KM, et al. Transforming growth factor beta signalling and matrix metalloproteinases in the mucosa overlying Crohn’s disease strictures. Gut. 2009;58:777–89. doi: 10.1136/gut.2008.149096. [DOI] [PubMed] [Google Scholar]
- 144.Feagins LA. Role of transforming growth factor-beta in inflammatory bowel disease and colitis-associated colon cancer. Inflamm Bowel Dis. 2010;16:1963–8. doi: 10.1002/ibd.21281. [DOI] [PubMed] [Google Scholar]
- 145.Dudakov JA, Hanash AM, van den Brink MR. Interleukin-22: immunobiology and pathology. Annu Rev Immunol. 2015;33:747–85. doi: 10.1146/annurev-immunol-032414-112123. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Sources of and Targets for IL17. A variety of cells within intestinal tissues can secrete IL17, including intraepithelial and lamina propria γδ T cells, Th17 cells and innate lymphoid cells. In mice IL17 production from lamina propria γδ T cells can occur independently of IL23, and therefore can persist despite IL23 blockade. IL17, in turn, acts on a number of targets, including epithelial cells, fibroblasts and neutrophils, to mediate protection against intestinal microbes. Importantly, despite the contribution of IL17 to intestinal inflammation through the regulation of such cells as neutrophils, blocking IL17 during intestinal inflammation actually leads to worsening of the inflammation. The essential role for IL17 on epithelial function during inflammatory conditions appears to be one reason accounting for the adverse outcomes with IL17 blockade.
Supplementary Table 1: Findings From Clinical Trials of Patients with IBD