Abstract
World Health Organization recommends a target for the male circumcision prevalence rate of 80%. This rate will have a substantial impact on the human immunodeficiency virus-acquired immunodeficiency syndrome epidemic in Eastern and Southern Africa. The objective of the study was to assess whether an innovative intervention can lead to an increased voluntary male medical circumcision (VMMC) uptake among adults in a short time. This prospective observational study of a demand generation intervention was conducted in the township of Orange Farm (South Africa) in August to November 2015. In this community male circumcision prevalence rate among adults was stable between 2010 and 2015 at 55% and 57%, despite regular VMMC campaigns at community level and the presence of a VMMC clinic that offered free VMMC. The intervention took place in a random sample of 981 households where 522 men aged 18 to 49 years accepted to participate in the study. Among the 226 uncircumcised men, 212 accepted to be enrolled in the intervention study. A personal male circumcision adviser trained in interpersonal communication skills was assigned to each uncircumcised participant. The male circumcision advisers were trained to explain the risks and benefits of VMMC, and to discuss 24 possible reasons given by men for not being circumcised. Participants were then followed for 9 weeks. Each participant had a maximum of 3 motivational interviews at home. Participants who decided to be circumcised received financial compensation for their time equivalent to 2.5 days of work at the minimum South African salary rate. Among the 212 uncircumcised men enrolled in the intervention, 69.8% (148/212; 95% confidence interval [CI]; 63.4%–75.7%) agreed to be circumcised, which defines the uptake of the intervention. The male circumcision prevalence rate of the sample increased from 56.7% (296/522) to 81.4% (425/522; 77.9%–84.6%), P < 0.001, corresponding to a relative increase of 43.6% (95% CI: 35.4%–53.7%). The reported reasons for accepting circumcision were motivational interviews with the male circumcision adviser (83.1%), and time compensation (39.4%).
Increased uptake of VMMC uptake can be obtained in a short time among adult males but requires an intense intervention centered on uncircumcised men at an individual level and time compensation.
Keywords: Africa, demand creation, HIV, male circumcision, prevention, public health, uptake
1. Introduction
Following 3 randomized controlled trials conducted in Africa,[1–3] World Health Organization (WHO) and Joint United Nations Program on HIV/AIDS recommended in 2007 the use of voluntary medical male circumcision (VMMC) to fight the human immunodeficiency virus-acquired immunodeficiency syndrome (HIV-AIDS) epidemic in countries with a low male circumcision prevalence rate and a high HIV prevalence rate.[4] Since 2009, a roll-out of VMMC mainly funded by The United States President's Emergency Plan for AIDS Relief started in 14 priority countries from Eastern and Southern Africa. The aim of this ongoing roll-out is to reach a male circumcision prevalence rate of 80% among adults, which is the target recommended by WHO.[5,6] Such a level will have a substantial impact on the HIV-AIDS epidemic in Eastern and Southern Africa.[7]
Over time, the male circumcision prevalence rate, which is often called the male circumcision coverage, increased in these countries. However, current rate varies substantially between countries. As of December 2014, while Ethiopia, Kenya, and Tanzania have already reached 80% male circumcision coverage targets, Lesotho, Malawi, Namibia, Rwanda, and Zimbabwe have low male circumcision coverage, ranging from 6% to 26%.[8] Despite this remarkable success in some countries, it is uncertain whether an 80% male circumcision prevalence rate will be reached in all priority countries.
The first roll-out of VMMC in Africa was conducted in the township of Orange Farm located in South Africa (French National Agency for Research on Aids and Viral Hepatitis-12126 project), one of the priority countries. In this typical township, an intensive roll-out took place between 2008 and 2010 and led to an increase in adult male circumcision prevalence rate from 12% in 2008 to 53% in 2011.[9] Since 2011, a VMMC demand creation was organized, similar to that in many other countries in Africa, entailing school talks, street advertisement, local radio slots, and episodic door-to-door distribution of flyers. Despite these efforts, the male circumcision prevalence rate among adults remained relatively constant between 2010 and 2015.[10] This situation may prefigure what will happen in some of the priority countries.
The objective of the study was to assess whether an innovative intervention can lead to an increased VMMC uptake among adults in a short time.
2. Methods
This study was a prospective intervention study described in detail below. In summary, a random sample of men was taken from the township and willing, uncircumcised men of the sample were enrolled in an intervention aiming to motivate them to undergo circumcision in the 9-week period following enrolment.
2.1. Study setting
This study was conducted in the South African township of Orange Farm where the adult population (18–49 years) is estimated to be 110,000. The study was conducted in 2015 between mid August and early November, a period not considered as the male circumcision season in South Africa. The township is located approximately 40 km from Johannesburg, in Gauteng province which has experienced one of the most severe HIV epidemics in the world, with a HIV prevalence rate estimated at 28.6% among antenatal women in 2013.[11] In this township, a free-for-service VMMC clinic has been running since 2008. It provides VMMC to males from the age of 10 years.
2.2. Sampling
A random sample of 30 clusters was selected among the 346 clusters of Orange Farm obtained from Statistics South Africa. A systematic sample of 20% of the households was then selected in the 30 clusters. All men who stayed at least 2 nights in the selected households in the past 7 days and spoke English or 1 of the 2 main local languages (Sesotho and IsiZulu) were eligible. The households were not visited at specific hours. Contact was established with 870 households among the 981 eligible households, which corresponds to a household response rate of 88.5%. In these 870 households, 696 men were eligible and 522 men accepted to participate in the study, which corresponds to an individual response rate of 75.0%. Participants underwent a clinical examination performed by a trained male nurse during which their clinical male circumcision status (presence or absence of foreskin) was assessed. Following this assessment, all men underwent HIV risk reduction counseling, with the offer of free HIV testing. The intervention was then proposed to all those uncircumcised among the 522 men.
2.3. Intervention at household level
The intervention combined a household intervention with an individual intervention. The household intervention consisted of the distribution of a flyer entitled “What men and women should know about male circumcision” and engagement in discussion with all the members of the household about male circumcision. The aim of this first level intervention was to facilitate future discussion about male circumcision between the uncircumcised adults of the household and the other members, which may include parents, children, partners, and friends.
2.4. Intervention at individual level
Intervention at an individual level consisted of combining motivational interviews with the offer of financial compensation in cases where participants decided to undergo circumcision. Following informed consent, a first motivational interview was given by a “male circumcision adviser.” This motivational interview was a face-to-face private discussion that took place either in a room of the house or in a vehicle parked in front of the house. For this intervention, we used 2 male circumcision advisers trained in interpersonal communication skills. They were female. Each participant was followed by the same adviser to establish a personal relationship based on respect and trust. These advisers recorded the initial willingness of participants to become circumcised and their reason for not being circumcised. Then, they presented the risks and benefits of medical male circumcision and discussed the reasons given by participants for not being circumcised. A list of 24 possible reasons with answers was established in advance from our experience, and the male circumcision advisers were trained to explain these answers.
Following the first motivational interview, the male circumcision adviser made an appointment with the participant for a second motivational interview approximately 3 weeks after the first motivational interview. A third and last motivational interview was organized approximately 3 weeks following the second motivational interview. Participants willing to become circumcised in the 9-week period after recruitment were welcomed at the VMMC clinic of Orange Farm, where they were circumcised. In the case of this study, the VMMC procedures differed in 2 ways from the usual procedure: the pre male circumcision counseling did not include information about male circumcision as this information was already delivered by the male circumcision adviser, and the participants were prioritized for the circumcision procedure before the other men, mainly youths, waiting for circumcision. For the participants coming for circumcision after the first or second motivational interviews, the subsequent motivational interviews were canceled. The motivational interviews were given between August 17 and November 4.
The participants came for VMMC between August 22 and November 5. After circumcisions were performed either at the VMMC clinic of Orange Farm but within the 9-week period following recruitment, men received financial compensation of R250 (US$17) corresponding to 2.5 days of work for a domestic worker paid at minimum wage. This time corresponds to 1 day for the surgery, 1 day to rest after surgery when it is difficult to work and 0.5 days for the postoperative checkup that takes place 1 week after surgery.
2.5. Data collection
Before the first motivational interview, a face-to-face questionnaire with close-ended questions provided an opportunity to record the participant's background characteristics and his knowledge and attitudes towards male circumcision. After circumcision, a face-to-face questionnaire permitted the recording of the perception of the intervention by each participant. To assess the effect on VMMC uptake of other concurrency factors than those forming the intervention, such as TV shows or male circumcision campaigns in the township, we also recorded the level of VMMC performed on adult men living in Orange Farm during the course of the study and not recruited in the intervention study.
2.6. Statistical analysis
“Uptake of the intervention” was defined here as the proportion of uncircumcised men who came for medical male circumcision in the 9-week period following recruitment, even if the surgery could not be done because of a medical contraindication. Similarly, “Uptake of male circumcision” was defined as the proportion of men who were circumcised in the same 9-week period.
Quantitative data are presented with mean, median, and interquartile range. For qualitative data, we used frequency distribution and relative frequency. 95% confidence interval (CI) of proportions were calculated using the Clopper–Pearson interval by calculating quantiles from the beta distribution.[12] We used the binomial test to compare the observed male circumcision prevalence rate with the value of 80%. We used the bootstrap technique with 5000 replications to compare the proportion of circumcised men before and after the intervention. A P value less than 0.05 was considered statistically significant, and all tests were 2-sided. The sample size of uncircumcised men was calculated to be 84 assuming an uptake of 30% and 95% CI of 20% to 40%.
We analyzed the association of background characteristics with the uptake of the intervention by estimating prevalence rate ratios (PRRs) using univariate and adjusted PRRs multivariate general linear models (Poisson regression). The covariates with an univariate P value <0.2 were included in the multivariate analysis.
Analyses were computed using the R statistical package (version 3.2.5) (Vienna, Austria).[13] All data are within the paper.
2.7. Ethics approval and consent to participate
The Human Research Ethics Committee (Medical) of the University of the Witwatersand, Johannesburg, South Africa, granted ethical clearance for the study on the January 19, 2015 (M140946). All men provided written informed consent before inclusion in the study.
3. Results
3.1. Characteristics of the sample
Among the 522 men, we found 296 circumcised men and 226 uncircumcised men. Among these 226 uncircumcised men, 212 (93.8%) accepted to participate in the intervention. Table 1 describes the characteristics of these men. Most (76.4%) knew that they could be circumcised for free in Orange Farm. To the question “Are you willing to become circumcised in the future?” asked before being exposed to the intervention, 186/212 (87.7%; 95% CI: 82.8%–91.6%) chose the answer “Yes, definitely”, 21/212 (9.9%; 95% CI: 6.4%–14.5%) chose the answer “Maybe”, and 5/212 (2.4%; 95% CI: 0.9%–5.1%) chose “Unlikely” or “Definitely not”.
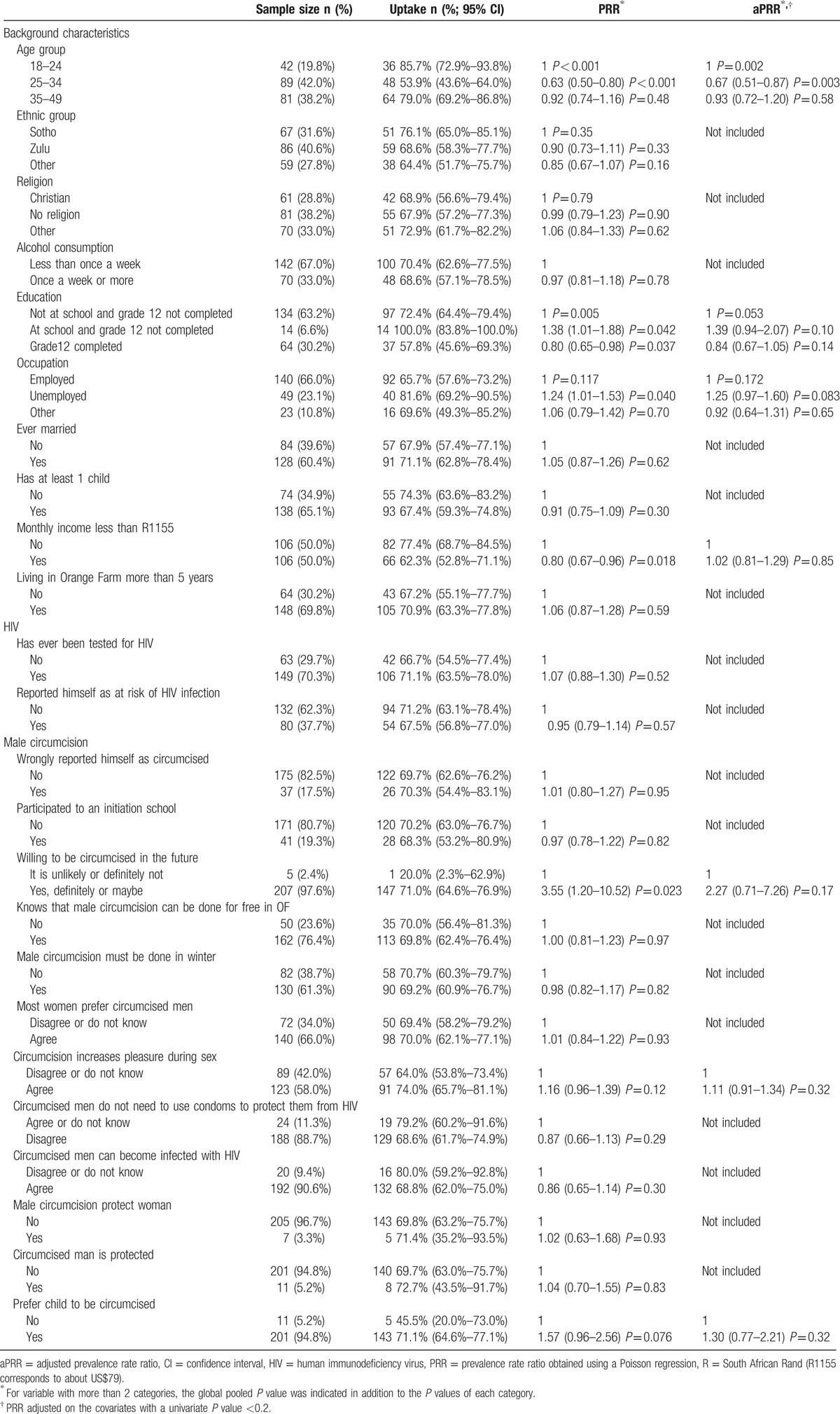
Table 1.
Characteristics of the uncircumcised men and association with the uptake of the intervention.
3.2. Uptake of the intervention and of male circumcision
Figure 1 describes the study flow of the intervention. This figure reveals that among the 212 men who were exposed to the intervention, the uptake of the intervention was 148/212 (69.8%; 95% CI: 63.4%–75.7%). A general practitioner practicing in Orange Farm circumcised 1 participant. Among the 148 men who came for circumcision, 112 (75.7%) came in the 3 weeks following the first motivational interview. However, 1 participant was willing to be circumcised after the first motivational talk but effectively came only 3 months later.
Figure 1.
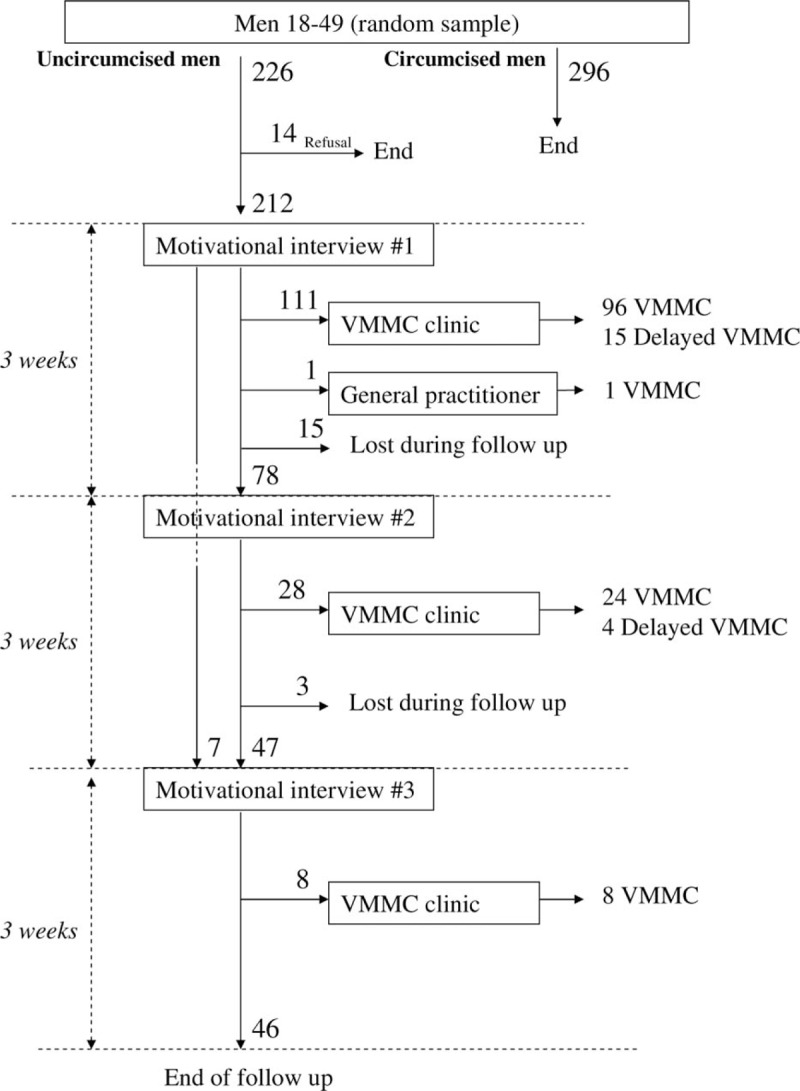
Study flow of the intervention. Among the 226 uncircumcised men, 212 were exposed to the intervention and 148 (112 + 28 + 8) came for circumcision. Among them, 19 (15 + 4) could not be circumcised during the 9-week follow-up of the study due to medical reasons. VMMC = voluntary male medical circumcision.
In the sample of 522 men, 296 were already circumcised, 148 came for circumcision and 129 underwent circumcision. A total of 19 could not be circumcised during their follow-up because of medical reasons such as symptomatic sexually transmitted infection or a CD4 count lower than 200 cells/mm3, following the policy of the VMMC clinic. Thus, the male circumcision prevalence rate increased from 296/522 (56.7%; 95% CI: 52.4%–60.9%) to (296 + 129)/522 (81.4%; 95% CI: 77.9%–84.6%), P < 0.001. The relative increase was 43.6% (95% CI: 35.4%–53.7%). The initial male circumcision prevalence rate was significantly different from 80% (P < 0.001), which was not the case for the final male circumcision prevalence rate (P = 0.44). If no VMMC had been delayed because of medical reasons, we would have observed a final male circumcision prevalence rate of (296 + 148)/522 (85.1%; 95% CI: 81.8%–87.9%).
Figure 2 presents the distribution of male circumcision prevalence by age group before and after the intervention if no VMMC had been delayed because of medical reasons. Among the age groups 18 to 24, 25 to 29, 30 to 39, and 40 to 49, the uptake of the intervention was respectively 36/42 (85.7%; 95% CI: 72.9%–93.8%), 26/49 (53.1%; 95% CI: 39.2%–66.5%), 43/67 (64.2%; 95% CI: 52.3%–74.9%), and 43/54 (79.6%; 95% CI: 67.5%–88.7%). This shows that the uptake of male circumcision was distributed throughout all age groups. Among the 148 men who came for circumcision, 31 (20.9%; 95% CI: 15.0%–28.0%) were tested for HIV for the first time at the VMMC clinic.
Figure 2.

Male circumcision prevalence rate before and after the intervention by age group. The dotted lines represent the overall male circumcision prevalence rate before and after the intervention. The male circumcision prevalence rate after the intervention in this figure is the prevalence rate that would have been observed if no voluntary medical male circumcision had been delayed due to medical reasons (see text).
3.3. Factors associated with the uptake of the intervention
The factors associated with the uptake of the intervention are described in Table 1. Among those not willing to become circumcised before the intervention, 1/5 (20%) came for circumcision. Among the remaining participants answering either “Maybe” or “Yes definitely” when asked of their willingness to be circumcised before the intervention, 147/207 (71.0%) came for circumcision (P = 0.023). The multivariate analysis revealed that age was a highly significant factor and that the significance of education level was borderline. Ethnic group and the fact of living in Orange Farm for more than 5 years were not associated with the uptake rate of the intervention.
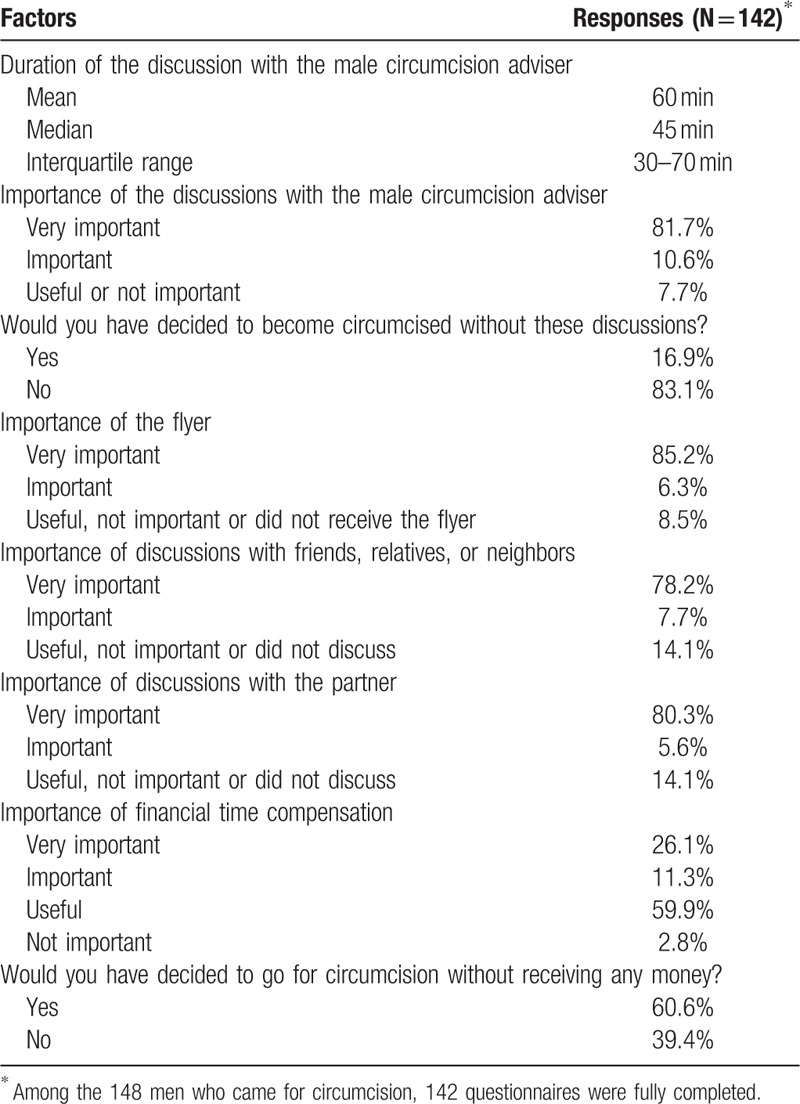
3.4. Analysis of the acceptance of the intervention
Table 2 presents the perception of the components of the intervention reported by those who came for circumcision. This table shows that the components of the intervention: discussion with the male circumcision advisers, distribution of flyers and discussion with friends, relatives and partners as well as financial time compensation were important. Financial compensation was reported as important or very important by 37.4% (53/142), which is consistent with the fact that almost 40% (56/142) reported that they would not have undergone circumcision without this compensation element (P = 0.023). Among those who opted for circumcision, 124/142 (87.3%; 95% CI: 81.1%–92.0%) reported that they would not have been circumcised without the discussions with male circumcision advisers together with the financial compensation.
Table 2.
Perception of the components of the intervention reported by those who came for VMMC.
3.5. Effect of other factors on the uptake
We counted an average of 18.6 of VMMCs per week performed on adult men living in Orange Farm during the course of the study and not recruited in the intervention study. Knowing that the sample was 1.2% of the corresponding population of Orange Farm, this implies that approximately 2.1 VMMCs would have been observed during a 9-week period in the sample without the intervention. This complementary analysis indicates that when taking the Orange Farm population as a control group, the intervention leads to a final male circumcision prevalence rate attributable to the intervention of (296 + 129 − 2)/522 (81.0%; 95% CI: 77.5%–84.2%).
4. Discussion
4.1. Main results
In this study, we first designed an innovative intervention to promote VMMC among adults. Second, we tested this intervention in a prospective experiment that demonstrated that the uptake of the intervention reached almost 70% and a male circumcision prevalence rate of 80% could be obtained among a random sample of adults in a setting where this rate had been stable over a certain period at a lower level. Moreover, this increase prevalence rate was obtained in just 9 weeks.
4.2. Limitations
The main limitation of this study is that we used an evaluation method in which the male circumcision prevalence rate after the intervention was compared with the value before the intervention. Therefore, the observed increase of male circumcision prevalence rate may be attributable to other concurrency factors than those forming the intervention, such as TV shows or male circumcision campaigns in the township. To assess this possibility, we carefully recorded the level of VMMC performed on adult men living in Orange Farm during the course of the study and not recruited in the intervention study. The result was that we can consider that most of the 129 VMMCs performed in this study are confidently attributable to the intervention. Another important argument in favor of a causal interpretation of our study is that most of men (87.3%) of this study who came for circumcision reported that they would not have come without the motivational interviews and the financial compensation, which were key components of the intervention.
Another limitation of this study is the response rate, even if the rates obtained are acceptable for such a study. From reports provided by fieldworkers having conducted the preliminary discussion in the selected households before inclusion, about 45% of the men who refused to participate were men not willing to have a genital examination. Because the intervention study was proposed only to men who accepted the genital examination, there is no reason to think that such a refusal is linked to the male circumcision status of those who refused to participate. However, we cannot determine what would have been the result of the study without including a genital examination.
4.3. Intervention
In this study, we used an innovative intervention. Although this intervention is new in the field of VMMC, it is composed of classical elements such as motivational interviews.[14,15] This intervention was designed using communication means untried by the current VMMC demand creation techniques among adults in Eastern and Southern Africa. Current recruitment is based on communication means such as street advertisement, street animation, and flyer distribution in various places including households. School talks are also widely used for recruiting younger men but also some adults who remain in school beyond the age of 17. An important component of the ongoing demand creation method is talks conducted at the VMMC clinics for those interested in VMMC. The results presented here suggest that activities such as school talks, street animation with flyer distribution, and local frequency modulation radio slots, which were ongoing throughout the township during the study, played a minor role in recruiting adult men of the study for VMMC. This is consistent with the stable male circumcision prevalence rate observed in this community in the past years. However, these activities were very important in motivating the men already circumcised.[16]
We designed our intervention based on the following principles: the men have to make minimum effort; the intervention should focus on repeated motivational interviews that allow for private discussion in a respectful manner of the reasons given by each man for not being circumcised; discussion with friends, relatives, and partners are important in the decision making process; and financial compensation for time encourages those who may not be able to afford to take time off work to undergo VMMC. As a result, we designed an intervention that took place in the home, in which a personal relationship was established between each male circumcision adviser and participants. The intervention combined these motivational interviews with a financial compensation element and discussions with all members of the household. In 2/3 of the cases, only 1 motivational interview was enough to motivate the uncircumcised men to go for circumcision. These discussions were introduced using flyer distribution and aimed to facilitate future exchanges on the topic of VMMC between participants and other house members, and friends.
4.4. Interpretation of the success of the intervention
The success of this study was not predictable in view of the campaigns conducted in Orange Farm. The fact that the rate of VMMC uptake had remained constant at approximately 53% following a successful intensive campaign in the township between 2008 and 2010,[9] increasing the rate from 12% suggested that perhaps a saturation level of circumcision uptake had been reached and that this new intervention would not significantly increase the prevalence. Previous studies suggest that most men are favorable to male circumcision[16,17] and therefore we postulated that it was more a question of convincing men to come for VMMC than to convince men of the benefits of VMMC. In a sense, our study simply aimed to create an attractive opportunity for men to come for VMMC. The fact that this opportunity was offered for a limited period may also have played an important role. The role played by the discussion with the male circumcision advisers appeared as “very important,” as it was reported by the participants. The financial incentives appeared also clearly important, though to a lesser extent. This latter finding is consistent with a recent study conducted in Kenya[18] where compensation in the form of food vouchers resulted in a modest increase in the prevalence of circumcision after 2 months. The Kenyan study concluded that “the effects of more intense promotion require further investigation.” This is what this study has achieved in Orange Farm. However, the precise role of financial incentives and its nature should be studied in a randomized controlled trial due to its potential importance and programing implications. Broadly, we believe that any intervention devoted to convincing adult men to undergo circumcision will need to be of a multifaceted nature in order to be successful, as has already been shown for VMMC uptake by adolescents.[19]
4.5. Reproducibility
An important question is whether this intervention is replicable elsewhere with similar results. There is no doubt that the intervention is replicable elsewhere as it is based on easily repeatable methods such as motivational interviews with male circumcision advisers, flyer distribution, discussion in households, and financial incentives. In addition, the male circumcision advisers in Orange Farm were ordinary fieldworkers with some experience in interpersonal communication. They were selected among fieldworkers used in Orange Farm in previous male circumcision surveys to interview participants. One has been trained to work in a call center, and the other has studied psychology for 2 years at university. They were trained for 1 week to learn the risks, benefits, and possible answers to reply to arguments given by men for not being circumcised. These reasons and answers may easily be adapted to another context than that of South Africa.
5. Conclusion
The conclusion of this study is that innovative methods of VMMC demand creation can be elaborated and can be tested locally and rapidly among a small random sample of uncircumcised men. Such methods can lead to an increased male circumcision prevalence rate among adults in a short period. These methods should be encouraged in order to increase the male circumcision prevalence rate to 80% as recommended by WHO in severely HIV affected countries, and thus to decrease HIV incidence. Another important conclusion is that financial incentives should be used when required as their role is shown to be significant. Finally, the Orange Farm demand creation method should be scaled up in Orange Farm and would likely lead to a significantly increased male circumcision prevalence rate, which would, in turn, lead to a strong impact on the HIV epidemic.[9,20,21]
Acknowledgments
We would like to thank the entire research team of Progressus Research and Development and specifically Agenda Gumbo for organizing the data entry of this study. We would like to thank the CHAPS Orange Farm clinic team for the support in getting study participants circumcised and prioritizing study participants, as well as Gaph Phatedi, Genevieve Dean and Audrey Mkwanazi for support. We are also grateful to Kévin Jean for comments on the first version of the proposal. We would like to thank the community of Orange Farm and specifically the Community Advisory Board of Orange Farm chaired by Portia Ntshangase.
Footnotes
Abbreviations: AIDS = acquired immunodeficiency syndrome, CI = confidence interval, HIV = human immunodeficiency virus, PRR = prevalence rate ratio, VMMC = voluntary medical male circumcision, WHO = World Health Organization.
Availability of data: The dataset supporting the conclusions of this article is included within the article.
Authors’ contributions: BA, RR-T, and AP developed the hypothesis and secured funding. BA and EM carried out statistical analyses. EM and BA wrote the first draft of the paper. The remaining authors contributed to the data collection and the management of the study. All authors critically commented on and approved the final submitted version of the paper.
Funding/support: The present study was funded by a grant (award number 12285) from the ANRS (France) supplemented by funds from the National Institute For Communicable Diseases (South Africa).
The authors have no conflicts of interest to disclose.
References
- [1].Auvert B, Taljaard D, Lagarde E, et al. Randomized, controlled intervention trial of male circumcision for reduction of HIV infection risk: the ANRS 1265 Trial. PLoS Med 2005;2:e298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Bailey RC, Moses S, Parker CB, et al. Male circumcision for HIV prevention in young men in Kisumu, Kenya: a randomised controlled trial. Lancet Lond Engl 2007;369:643–56. [DOI] [PubMed] [Google Scholar]
- [3].Gray RH, Kigozi G, Serwadda D, et al. Male circumcision for HIV prevention in men in Rakai, Uganda: a randomised trial. Lancet Lond Engl 2007;369:657–66. [DOI] [PubMed] [Google Scholar]
- [4].WHO-UNAIDS. Technical consultation on male circumcision and HIV prevention: research implications for policy and programming. New Data Male Circumcision HIV Prev Policy Programme Implic. 2007. http://www.who.int/hiv/mediacentre/MCrecommendations_en.pdf [Accessed September 30, 2016] in press. [Google Scholar]
- [5].WHO-UNAIDS Joint Strategic Action Framework to Accelerate the Scale-Up of Voluntary Medical Male Circumcision for HIV Prevention in Eastern and Southern Africa 2012–2016. 2011;Geneva:WHO-UNAIDS, http://www.who.int/hiv/pub/strategic_action2012_2016/en/http://www.who.int/hiv/pub/strategic_action2012_2016/en/. [Accessed September 30, 2016]. [Google Scholar]
- [6].Njeuhmeli E, Forsythe S, Reed J, et al. Voluntary medical male circumcision: modeling the impact and cost of expanding male circumcision for HIV prevention in eastern and southern Africa. PLoS Med 2011;8:e1001132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Williams BG, Lloyd-Smith JO, Gouws E, et al. The potential impact of male circumcision on HIV in Sub-Saharan Africa. PLoS Med 2006;3:e262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].WHO-UNAIDS UNAIDS World AIDS Day Report. 2015;Geneva:WHO-UNAIDS, http://www.unaids.org/sites/default/files/media_asset/WAD2015_report_en_part01.pdfhttp://www.unaids.org/sites/default/files/media_asset/WAD2015_report_en_part01.pdf. [Accessed September 30, 2016]. [Google Scholar]
- [9].Auvert B, Taljaard D, Rech D, et al. Association of the ANRS-12126 male circumcision project with HIV levels among men in a South African township: evaluation of effectiveness using cross-sectional surveys. PLoS Med 2013;10:e1001509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Marshall E, Rain-Taljaard R, Tsepe M, et al. Sequential cross-sectional surveys in Orange Farm, a township of South Africa, revealed a constant low voluntary medical male circumcision uptake among adults despite demand creation campaigns and high acceptability. PLoS One 2016;11:e0158675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].National Department of Health (South Africa) The 2013 National Antenatal Sentinel HIV Prevalence Survey South Africa. 2015;https://www.health-e.org.za/wp-content/uploads/2016/03/Dept-Health-HIV-High-Res-7102015.pdfhttps://www.health-e.org.za/wp-content/uploads/2016/03/Dept-Health-HIV-High-Res-7102015.pdf. [Accessed September 30, 2016]. [Google Scholar]
- [12].Clopper C, Pearson ES. The use of confidence or fiducial limits illustrated in the case of the binomial. Biometrika 1934;26:404–13. [Google Scholar]
- [13].R Development Core Team R: A Language and Environment for Statistical Computing. Vienna, Austria:R Foundation for Statistical Computing; 2005. [Google Scholar]
- [14].Miller WR, Rose GS. Toward a theory of motivational interviewing. Am Psychol 2009;64:527–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Lundahl B, Burke BL. The effectiveness and applicability of motivational interviewing: a practice-friendly review of four meta-analyses. J Clin Psychol 2009;65:1232–45. [DOI] [PubMed] [Google Scholar]
- [16].Lissouba P, Taljaard D, Rech D, et al. A model for the roll-out of comprehensive adult male circumcision services in African low-income settings of high HIV incidence: the ANRS 12126 Bophelo Pele Project. PLoS Med 2010;7:e1000309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Westercamp N, Bailey RC. Acceptability of male circumcision for prevention of HIV/AIDS in sub-Saharan Africa: a review. AIDS Behav 2007;11:341–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Thirumurthy H, Masters SH, Rao S, et al. Effect of providing conditional economic compensation on uptake of voluntary medical male circumcision in Kenya: a randomized clinical trial. JAMA 2014;312:703–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Kaufman MR, Smelyanskaya M, Van Lith LM, et al. Adolescent sexual and reproductive health services and implications for the provision of voluntary medical male circumcision: results of a systematic literature review. PLoS One 2016;11:e0149892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Williams BG, Lloyd-Smith JO, Gouws E, et al. The potential impact of male circumcision on HIV in sub-Saharan Africa. PLoS Med 2006;3:e262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Orroth KK, Freeman EE, Bakker R, et al. Understanding the differences between contrasting HIV epidemics in east and west Africa: results from a simulation model of the Four Cities Study. Sex Transm Infect 2007;83(suppl 1):i5–16. [DOI] [PubMed] [Google Scholar]


