Supplemental Digital Content is available in the text
Keywords: adherence, antihypertensive, cardiovascular diseases, hypertension, Morisky medication adherence scale, nonadherence, uncontrolled blood pressure
Abstract
Background:
Hypertension drives the global burden of cardiovascular disease and its prevalence is estimated to increase by 30% by the year 2025. Nonadherence to chronic medication regimens is common; approximately 43% to 65.5% of patients who fail to adhere to prescribed regimens are hypertensive patients. Nonadherence to medications is a potential contributing factor to the occurrence of concomitant diseases.
Objective:
This systematic review applied a meta-analytic procedure to investigate the medication nonadherence in adult hypertensive patients.
Methods:
Original research studies, conducted on adult hypertensive patients, using the 8-item Morisky medication adherence scale (MMAS-8) to assess the medication adherence between January 2009 and March 2016 were included. Comprehensive search strategies of 3 databases and MeSH keywords were used to locate eligible literature. Study characteristics, participant demographics, and medication adherence outcomes were recorded. Effect sizes for outcomes were calculated as standardized mean differences using random-effect model to estimate overall mean effects.
Results:
A total of 28 studies from 15 countries were identified, in total comprising of 13,688 hypertensive patients, were reviewed. Of 25 studies included in the meta-analysis involving 12,603 subjects, a significant number (45.2%) of the hypertensive patients and one-third (31.2%) of the hypertensive patients with comorbidities were nonadherent to medications. However, a higher proportion (83.7%) of medication nonadherence was noticed in uncontrolled blood pressure (BP) patients. Although a higher percentage (54%) of nonadherence to antihypertensive medications was noticed in females (P < 0.001), the risk of nonadherence was 1.3 times higher in males, with a relative risk of 0.883. Overall, nearly two-thirds (62.5%) of the medication nonadherence was noticed in Africans and Asians (43.5%).
Conclusion:
Nonadherence to antihypertensive medications was noticed in 45% of the subjects studied and a higher proportion of uncontrolled BP (83.7%) was nonadherent to medication. Intervention models aiming to improve adherence should be emphasized.
1. Introduction
Hypertension is prevalent and remains one of the most significant causes of mortality worldwide. Elevated blood pressure (BP) is a major risk factor for coronary artery disease and its complications, heart failure, stroke, renal insufficiency, and blindness in diabetic patients. The Global Burden of Disease study estimated that hypertension is now the leading risk factor for disability-adjusted life years worldwide.[1] The risk of developing hypertension can be reduced by effective medication therapy management and significant lifestyle modifications. Adherence to antihypertensive medications is the cornerstone for achieving hypertension control.
Nonadherence to medication is a growing concern and is associated with adverse outcomes. Maintaining medication adherence to multiple medications is a complex issue in patients with chronic diseases, particularly cardiovascular diseases (CVDs). The influence of nonadherence to antihypertensive medications is the most important cause of uncontrolled BP. Consequently, because of nonadherence, most (nearly 3-quarters) of the hypertensive patients do not achieve optimal BP control.[2]
Several approaches were tried to investigate the medication-taking behavior and the traditional methods such as pill counts, clinical reports, prescription refills and patient-reported measures are some of the cheap and acceptable ones to provide medication adherence information. However, self-reported questionnaires were often used to assess the medication adherence in chronic disease patients. Several self-reported validated questionnaires were developed to monitor medication adherence in chronic disease patients including hypertension patients. Some of the scales suitable for measuring adherence in hypertension patients include Morisky medication adherence scale-8 (MMAS-8),[3] Brief Medication Questionnaire by Svarstad et al,[4] the Hill-Bone Compliance scale,[5] and the most recent Adherence scale by Culig et al.[6] Of these, MMAS-8 remains the best known and most widely used scale for investigating medication adherence in hypertensive patients. To date, there has been no systematic review or meta-analysis conducted to estimate the nonadherence status in hypertensive patients using any of the above-mentioned self-reported scales. Therefore, a better understanding of these issues could help to tailor effective interventions and strategies to improve the medication adherence in hypertensive patients. In order to gather the data from all the available literature that evaluated the adherence to antihypertensive medications using MMAS-8, we aimed to perform a systematic review and meta-analysis to synthesize medication nonadherence in hypertensive patients.
2. Materials and methods
2.1. Search strategies
A computerized systematic search of the PubMed, Scopus, and Google Scholar using the Cochrane guidelines to conduct the meta-analysis following PRISMA (Preferred Reporting Items for Systematic review and Meta-Analysis) statement was used (Appendix 1, https://figshare.com/s/5c111733cd4185c2362a). Published studies related to antihypertensive medications adherence using MMAS-8 and using MeSH terms: medication adherence∗ AND Morisky medication adherence scale∗ OR MMAS-8∗ AND adherence∗ OR compliance∗ AND antihypertensive∗ AND hypertension∗ AND using patients self-reported questionnaire. All the papers that were published in the English language between January 2009 and March 2016 were included. The review was limited to self-reported studies that were conducted using MMAS-8 validated questionnaire administered to the hypertensive patients using antihypertensive medications.
2.2. Inclusion criteria
We included studies that met the following inclusion criteria: Study used the MMAS-8 questionnaire on hypertensive patients to assess the adherence levels to antihypertensive medications; the study was an original article; and studies conducted on hypertensive patients.
2.3. Exclusion criteria
We excluded studies that used the MMAS-8 scale on other than hypertensive patients using antihypertensive medications, the subjects included other CVDs and diabetic patients and the studies using MMAS-4 scale.
2.4. Review process
All records that were identified from searches of the electronic databases were loaded into the ENDNOTE software version X5 (Thomson Reuters, Toronto, Ontario, Canada) and duplicates were removed. Two researchers (TMA and ASB) independently screened the titles and abstracts to identify the potentially eligible studies. Studies that were potentially eligible were selected for full-text review (Flow of information). Disagreement was resolved by mutual consent after discussion.
2.5. Data extraction
Information on the year of the execution of the study, the geographic location, the sample size, the way of administration of the questionnaire, and data about the nonadherence toward antihypertensive medication were retrieved. In particular, MMAS-8 statements that grouped answers that were scored <6 were considered as nonadherence outcomes for the meta-analysis.
2.6. Statistical analysis
The meta-analysis was performed using StatsDirect statistical software version 3.0 (Cheshire, UK). The Cochrane Q and the I2 were used to evaluate heterogeneity of studies. Random-effects model was used to combine studies showing heterogeneity of Cochrane Q P < 0.10 and I2 > 50.[7] Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) scale was used to assess the quality of the studies by categorizing into high quality (≥75% of the STROBE checklist) and low quality (<75% of the STROBE checklist).[8] We performed subgroup analysis by gender and studies carried out in different continents. Moreover, Egger and Begg tests representing funnel plots were used to assess the publication bias.
2.7. Ethical statement
This study was carried out in strict accordance with the recommendations in the STROBE and PRISMA guidelines. Ethics committee or institutional review board permission is not required for conducting systematic review and meta-analysis.
3. Results
A total of 912 articles were screened from the 3 scientific databases (PubMed = 380, Scopus = 312, and Google Scholar = 220). After screening the abstracts and titles, 852 were excluded because of irrelevance and duplicates. Sixty articles were assessed for full-text review and 32 articles were excluded with reasons (Suppl 2). Finally, 28 articles were included in the systematic review[9–36] and 25 of these were included in the meta-analysis.[9,11–25,27–31,33–36]
3.1. Characteristics of studies assessed
In total, 13,688 subjects were included in the analyzed studies. Nine of the studies were conducted in the United States,[11,12,15,26,29,30,32,33,35] and 2 each in China,[11,17] Nigeria,[16,22] Hong Kong,[21,25] and Iran.[10,18] Countries such as Uganda, Lebanon, Kenya, Republic of Korea, Peru, Ethiopia, Ghana, Malaysia, Palestine, Brazil, and Italy were represented with a single study.[9,13,19,20,23,24,27,28,31,34,36] These studies were conducted on hypertensive patients to assess medication adherence using MMAS-8 between January 2009 and March 2016. Twenty-four studies were cross-sectional[9–27] and others were cohort,[35] observational,[36] and interventional studies.[32] Only 1 randomized controlled trial (RCT) was found.[29] The sample size of studies ranged from 25[32] to 2445[21] subjects. Eleven studies assessed adherence through face-to-face interviews,[10,14,18,20,22–24,26,29–31] while 8 studies used self-administered questionnaires,[13,17,21,25,32–34,36] and only 1 study was administered through a telephone interview.[35] However, 8 studies did not specify the type of MMAS-8 questionnaire administered.[9,11,12,15,16,19,27,28] Except 1 study,[22] all the included studies met the quality criteria and showed high quality (>75%).[9–27,29–36]
3.2. Baseline characteristics of study subjects
The baseline characteristics of 28 studies are presented in Table 1. Among these hypertensive patients, the majority were females (n = 7859, 57.4%); 34% had comorbidities (n = 4661) and/or uncontrolled hypertension (n = 2606, 19%).
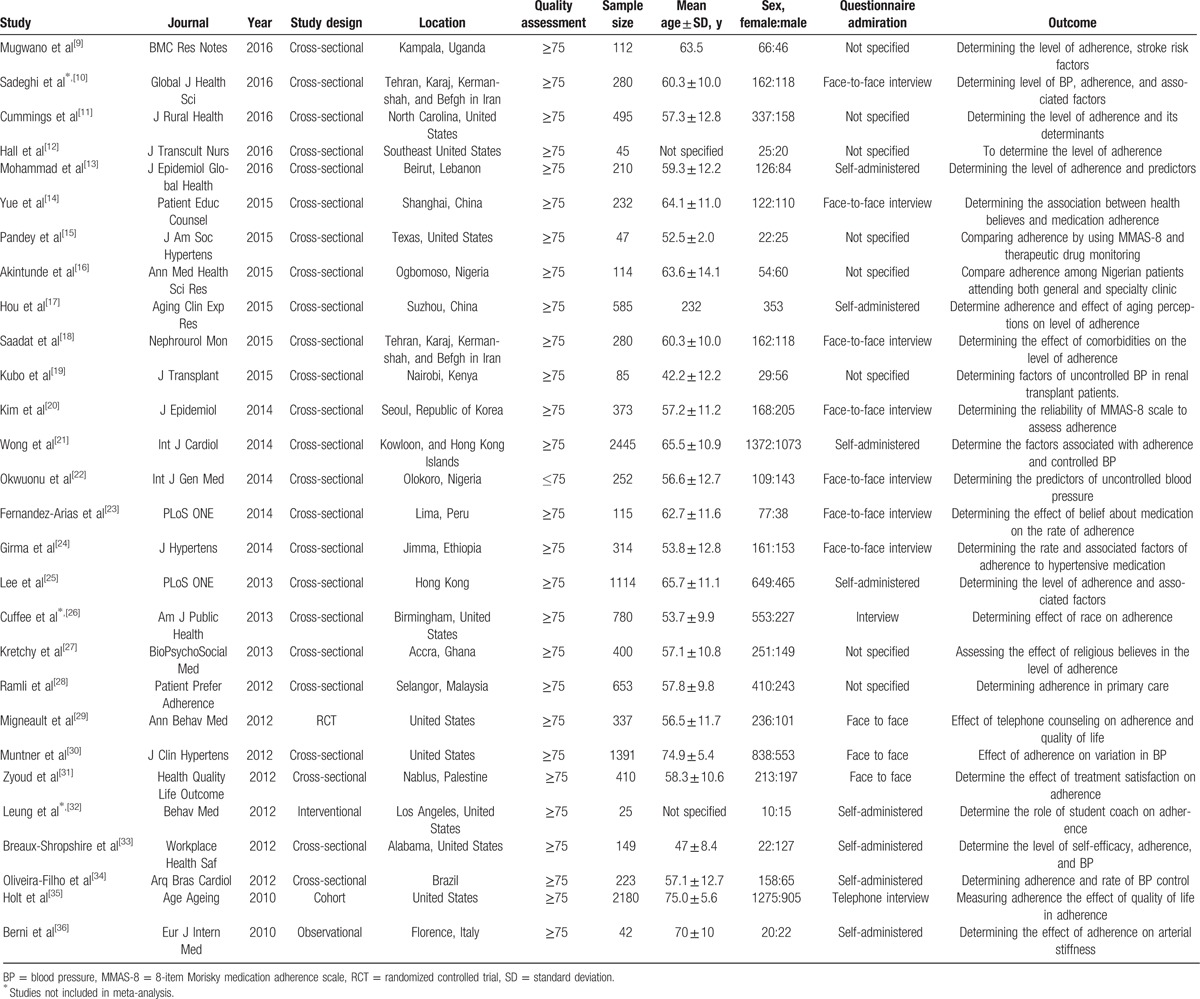
Table 1.
Overview of studies included in systematic review and meta-analysis (N = 13,688).
3.3. Nonadherence to antihypertensive medications
We identified a total of 25 studies (n = 12,628) that used MMAS-8 to assess the medication adherence in hypertensive patients. Overall, nonadherence to antihypertensive medications was 45.2% (95% confidence interval [CI] = 34.4–56.1, P < 0.001) (Fig. 1).
Figure 1.
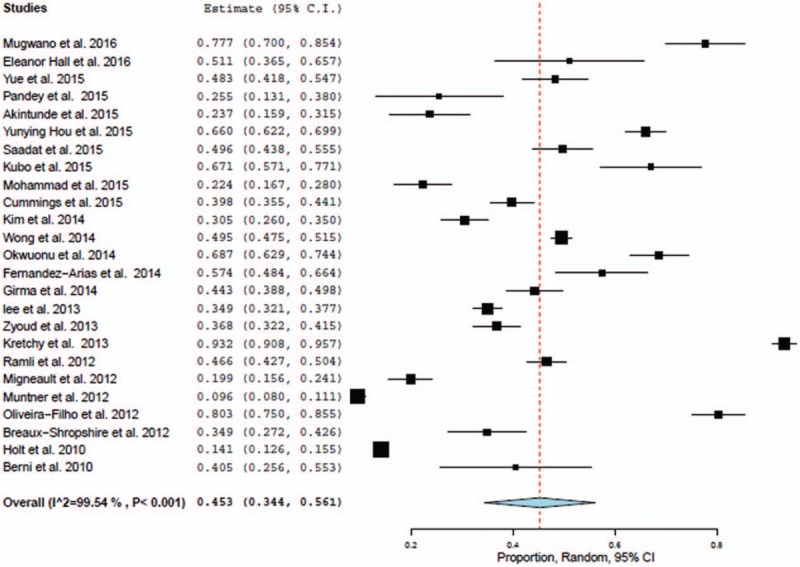
Nonadherence in hypertensive patients.
3.4. Nonadherence in hypertensive patients with comorbidities
Ten studies, with a total of 6836 subjects, reported the medication adherence levels in hypertensive patients with comorbidities. Overall, the nonadherence to antihypertensive medications was significant in hypertensive patients with comorbidities: 31.6% (95% CI = 10.2–97.5), P = 0.045; heterogeneity I2 = 99.1% (Fig. 2).
Figure 2.
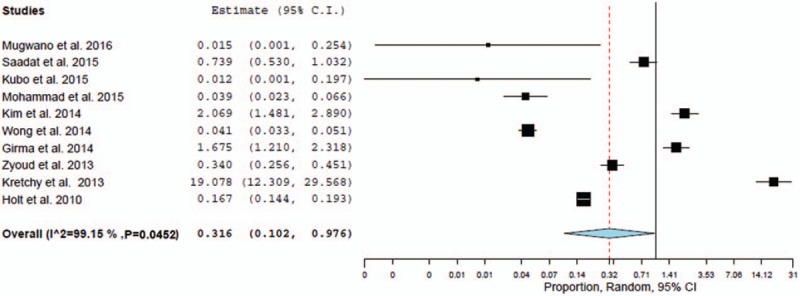
Nonadherence in hypertensive patients with comorbidities.
3.5. Nonadherence in uncontrolled hypertension patients
We identified 10 studies (n = 4574) that reported the medication adherence levels in uncontrolled and controlled hypertension patients. Compared to controlled hypertensive patients (n = 1973) (59.7% [95% CI = 37.7–81.7]), nonadherence in uncontrolled hypertensive patients (n = 2606) was 83.7% (95% CI = 59.9–117.0), but no statistical significance was noticed (P = 0.2991); heterogeneity I2 = 86.2% (Fig. 3).
Figure 3.
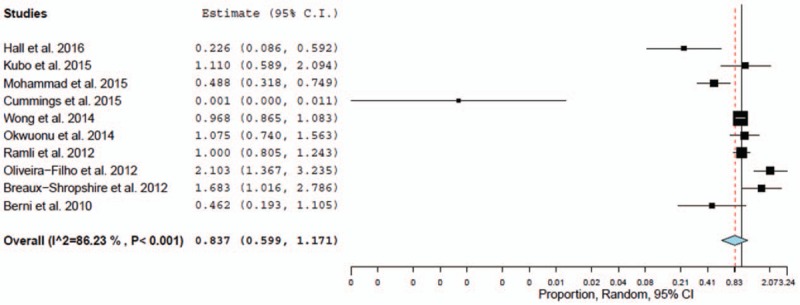
Nonadherence in uncontrolled hypertension patients.
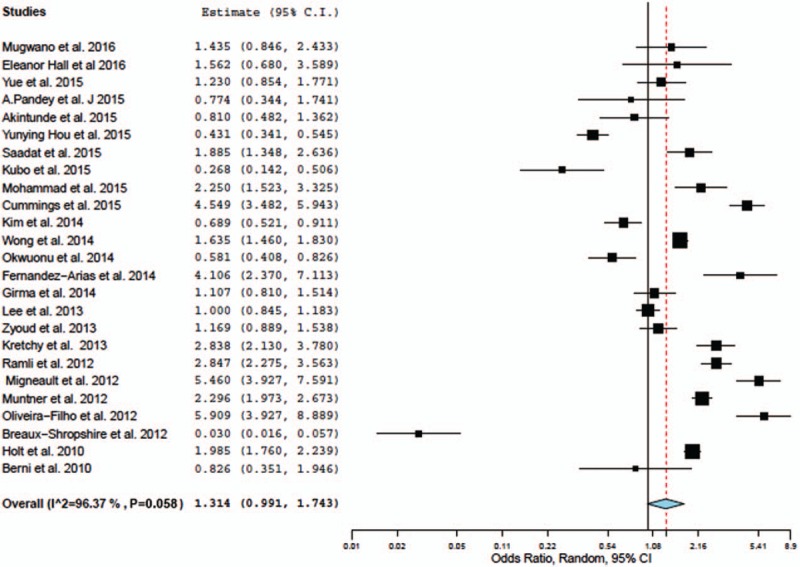
3.6. Subgroup analysis
To investigate the potential discrepancy, the results of 25 studies were stratified by gender with regard to nonadherence to antihypertensive medications using a random model. Overall, the risk of nonadherence to antihypertensive medications was 1.3 times (95% CI = 0.99–1.74, P = 0.058) higher in male hypertensive patients than females (odds ratio = 0.73, 95% CI = 0.56–0.93) with a relative risk of 0.883 (95% CI = 0.76–1.02), P = 0.104 (Fig. 4). Indeed, in the subgroup analysis, the percentage of nonadherence to antihypertensive medications was higher in females: 53.9% (95% CI = 49.7–57.9), P < 0.001 than males: 46.2% (95% CI = 42.2–50.2), P = 0.020.
Figure 4.
Nonadherence in females and males.
3.7. Sensitivity analysis stratified for different continents
Sensitivity analysis was carried out where the studies were conducted in different continents. Studies carried out in Africa (6 studies; n = 1277) (62.5% [95% CI = 39.9–85.0]; P < 0.001) and Asia (8 studies; n = 5917) (43.5% [95% CI = 35.0–53.0]; P < 0.001) showed a higher proportion of nonadherence to antihypertensive medications than American studies (9 studies; n = 4982) (36.6% [95% CI = 24.4–48.8], P < 0.001)and European studies (2 studies; n = 452) (37.1% [95% CI = 32.7–41.6], P < 0.001).
3.8. Publication bias
Publication bias was not highlighted in all the analysis and confirmed by the Egger and Begg tests showed funnel plots.
4. Discussion
Several epidemiological studies about medication adherence in hypertensive patients using MMAS-8 were conducted in recent years, making it possible to obtain direct evidence of the nonadherence situation of hypertensive patients. Based on the strict inclusion criteria, we reviewed 28 studies that assessed the antihypertensive medication adherence, we included 25 articles in this meta-analysis including 12,603 subjects, covering 15 countries and different provinces, thus the large population guaranteed the reliability of this study.
Using a systematic review, we aimed to gather different studies published between January 2009 and March 2016 that assessed medication adherence in hypertensive patients using MMAS-8. To our knowledge, this is the first systematic review on this topic. Previous reviews were focused on beliefs and hypertension treatment,[37] nonadherence in resistant hypertension patients,[38] and medication compliance in resistant hypertension patients.[39]
4.1. Strengths and limitations
The strengths of this paper consisted of execution of nonadherence to antihypertensive medications by including 25 studies in meta-analysis. This has helped us gather and strengthen the combination of each study findings to obtain pooled prevalence provided stronger evidence about medication nonadherence in hypertensive patients. In addition, the analysis conducted on 5 different outcomes showed interesting results. However, our search strategy was comprehensive, included research articles using MMAS-8 questionnaire, conducted on hypertensive patients and studies published in English language.
4.2. Summary of study findings
Through this study, we identified that a significant number (45.2%) of the hypertensive patients are nonadherent to antihypertensive medications and nearly one-third (31.2%) of hypertensive patients with various comorbidities showed nonadherence to medications. Interestingly, a higher proportion (83.7%) of uncontrolled hypertensive patients was nonadherent to medications. Although a higher percentage (54%) of nonadherence to antihypertensive medications was noticed in females (P < 0.001), the risk of nonadherence was 1.3 times higher in males, with a relative risk of 0.883. Overall, nearly two-thirds (62.5%) of the medication nonadherence was noticed in Africans and Asians (43.5%).
The findings of our review pointed out that the lack of medication adherence in hypertensive patients is a significant concern. “For instance, nearly half (45%) of the hypertensive population studied are nonadherent to antihypertensive medications.” This is comparably similar with Carrea et al study findings (57%) assessed the antihypertensive medication adherence using MMAS-8 items and urine fluorescence in resistant hypertensive patients.[40] Nonadherence to pharmacological agents in hypertensive patients has a negative impact and increases the risk of cardiovascular events and stroke. Medication nonadherence is multifactorial, several studies have demonstrated the association between nonadherence and patients’ beliefs, socioeconomic status, health literacy, race/ethnicity, and others.[37,41–45] Early identification of patients’ barriers by sharing the concerns with health professionals can help improve adherence, reduce costs, optimize drug therapy, and achieve BP control. However, several interventions were extensively tried to improve the adherence, it is notable that these interventions focused only on implementation of medication adherence for BP control. Future investigations should explore the potential benefits of tailoring patient-specific interventions, implementation adherence versus persistence outcomes, and the preferences for interventional delivery (e.g., face-to-face vs technology-mediated). These interventions were also confirmed by Conn et al review.[46]
BP lowering in hypertensive patients with comorbidities is significantly important in reducing vascular risk such as CVDs, coronary heart disease (CHD), stroke, diabetes, heart failure, and chronic kidney disease. However, a few studies identified hypertensive patients with comorbidities and the number of medications prescribed are the 2 significant factors associated with poor adherence.[45,47,48] In contrast, our findings showed that only one-third (31.2%) of hypertensive patients with comorbidities showed nonadherence to antihypertensive medications and was not strongly associated for nonadherence (P = 0.045). Evidence from the recent meta-analysis suggests that a 10 mm Hg reduction in systolic BP in hypertensive patients reduces the risk of major CVD events by 20%, CHDs by 17%, stroke by 27%, heart failure by 28%, and all-cause mortality by 13%.[49] This highlights the protective effects of pharmacologically induced BP reduction in hypertensive patients with comorbidities. Despite this, identifying best approach to reduce BP in hypertensive patients with comorbidities remains controversial.[50]
Uncontrolled systolic and diastolic BPs are important risk factors for increased cerebrovascular events, cardiovascular events, and all-cause mortality. Studies estimated that more than 50% of the uncontrolled hypertensive patients have suboptimal adherence.[51] Through our investigation we identified an alarming levels of nonadherence to antihypertensive medications in uncontrolled BP patients (83.7% [95% CI = 59.9–117.0]) than controlled BP patients (59.7% [95% CI = 37.7–81.7]). These results were comparably much higher than de Oliveira-Filho et al study assessed the medication adherence using MMAS-8 showed nearly two-thirds (62.4%) of the uncontrolled BP patients are nonadherent to antihypertensive medications.[52] In order to improve their medication adherence, practitioners need to focus on treatment targets and pharmacists should spend more time to adequately counsel about treatment and comprehensively discuss the advantages of lifestyle modifications in uncontrolled BP patients (but also controlled BP patients).
Antihypertensive medication adherence can vary substantially between individuals, identification of sex differences for nonadherence could assist the healthcare providers to customize an effective intervention. Through a subgroup analysis, our investigation showed nonadherence to antihypertensive medications is 1.3 times higher in male than in female patients, with a relative risk of 0.883 (95% CI = 0.76–1.02), P = 0.104. However, the percentage of nonadherence was noticeably higher in females than in males (53.9% vs 46.2%). These results were much higher than Holt et al study conducted on older adult hypertensive patients using MMAS-8, where a higher percentage of women had low adherence scores compared to men (15% vs 13.1%).[53] In accordance with previous studies, no differences in low medication adherence was noticed between men and women in CoSMO study.[54] Further research is needed to better understand the underlying and modified risk factors associated with nonadherence between the sexes.
The sensitivity analysis stratified for different continents showed a significant nonadherence levels in hypertensive patients. In particular, studies carried out in Africa showed a higher percentage of nonadherence levels (62.4%) than Asians (43.5%), Europeans (36.6%), and Americans (36.6%). These findings were consistent with studies conducted in African countries such as Ivory Coast (87.5%), Togo (83.7%), Congo (78.8%), and Tunisia (63.4%).[55–58]These oceanic discrepancies may be due to differences in the populations studied, ethnic/race differences, samples seize, difference in the questionnaire administered, or patients’ beliefs.
4.3. Limitations
The overall quality of the included studies was high, especially given that more than 90% of the studies were assessed as low risk of sampling bias. High level of heterogeneity was noticed across the included studies was one of the limitations of our study. A substantial proportion of the heterogeneity across studies could be due to differences in the population characteristics, sociocultural variations, and study methodologies. In addition, we used only validated and commonly used MMAS-8 questionnaire administered to hypertensive patients in all studies to prevent selection bias. Quality assessment and stratification of the quality and geographic criteria have allowed the evaluation of the presence of potential bias and confounders. Further, we may have missed some potentially relevant studies; however, this systematic review arguably constitutes the largest study on nonadherence to antihypertensive medications comprising >13,000 participants.
5. Conclusion
This comprehensive meta-analysis of nonadherence to antihypertensive medication documented a significantly higher proportion (45.2%) of medication nonadherence was noticed among hypertensive patients, particularly uncontrolled BP patients (83.7%). There is a need for tailoring interventions by linking adherence behavior with daily habits, developing patient-specific interventions, providing motivational interviews, and actively engaging family members to improve the antihypertensive medication adherence. Future research should explore alternative techniques to assess and monitor the medication adherence program particularly for older adult hypertensive patients.
Acknowledgments
The authors like express our sincere gratitude to Prof. Shiri Diskin, Israel for reviewing and editing the manuscript.
Supplementary Material
Footnotes
Abbreviations: BP = blood pressure, CHD = coronary heart disease, CVD = cardiovascular disease, MMAS = Morisky medication adherence scale, PRISMA = Preferred Reporting Items for Systematic review and Meta-Analysis, STROBE = Strengthening the Reporting of Observational Studies in Epidemiology.
TMA and AS conceived the study design, study protocol, literature review, data collection, data interpretation, and data analysis. EAG, ASB, and AAE: data interpretation, data analysis, statistical interpretation, and manuscript review. All the authors read and approved the final manuscript for submission.
The authors have no funding and conflicts of interest to disclose.
Supplemental Digital Content is available for this article.
References
- [1].Lim SS, Vos T, Flaxman AD, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012;380:2224–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Burnier M. Drug adherence in hypertension. Pathophysiology and Pharmacotherapy of Cardiovascular Disease 2015;Switzerland:Springer International Publishing, 919–933. [Google Scholar]
- [3].Morisky DE, Ang A, Krousel-Wood M, et al. Predictive validity of a medication adherence for hypertension control. J Hypertens 2008;10:348–54. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- [4].Svarstad BL, Chewning BA, Sleath BL, et al. The Brief Medication Questionnaire: a tool for screening patient adherence and barriers to adherence. Patient Educ Counsel 1999;37:113–24. [DOI] [PubMed] [Google Scholar]
- [5].Kim MT, Hill MN, Bone LR, et al. Development and testing of the Hill-Bone Compliance to high blood pressure therapy scale. Progress Cardiovasc Nurs 2000;15:90–6. [DOI] [PubMed] [Google Scholar]
- [6].Culig J, Leppee M, Boskovic J, et al. Determining the difference in medication compliance between general patient population and patients receiving antihypertensive therapy: a case study. Arch Pharm Res 2011;34:1143–52. [DOI] [PubMed] [Google Scholar]
- [7].Haidich AB. Meta-analysis in medical research. Hippokratia 2010;14(suppl 1):29–37. [PMC free article] [PubMed] [Google Scholar]
- [8].Von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol 2008;61:344–9. [DOI] [PubMed] [Google Scholar]
- [9].Mugwano I, Kaddumukasa M, Mubenyi L, et al. Poor drug adherence and lack of awareness of hypertension among hypertensive stroke patients in Kampala, Uganda: a cross-sectional study. BMC Res Notes 2016;9:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Sadeghi E, Behnood-Rod A, Aerab-Sheibani H, et al. Controlled blood pressure in Iranian patients: a multi-center report. Global J Health Sci 2016;8:188–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Cummings DM, Wu J, Cene C, et al. Perceived social standing, medication nonadherence, and systolic blood pressure in the rural south. J Rural Health 2016;32:156–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Hall E, Lee S, Clark PC, et al. Social ecology of adherence to hypertension treatment in Latino migrant and seasonal farmworkers. J Trascult Nurs 2016;27:33–41. [DOI] [PubMed] [Google Scholar]
- [13].Mohammad Y, Amal A, Sanaa A, et al. Evaluation of medication adherence in Lebanese hypertensive patients. J Epidemiol Global Health 2016;6:157–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Yue Z, Li C, Weilin Q, et al. Application of the health belief model to improve the understanding of antihypertensive medication adherence among Chinese patients. Patient Educ Counsel 2015;98:669–73. [DOI] [PubMed] [Google Scholar]
- [15].Pandey A, Raza F, Velasco A, et al. Comparison of Morisky medication adherence scale with therapeutic drug monitoring in apparent treatment-resistant hypertension. J Am Soc Hypertens 2015;9:420–6. [DOI] [PubMed] [Google Scholar]
- [16].Akintunde AA, Akintunde TS. Antihypertensive medications adherence among Nigerian hypertensive subjects in a specialist clinic compared to a general outpatient clinic. Ann Med Health Sci Res 2015;5:173–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Hou Y, Zhang D, Gu J, et al. The association between self-perceptions of aging and antihypertensive medication adherence in older Chinese adults. Aging Clin Exp Res 2015;28:1113–20. [DOI] [PubMed] [Google Scholar]
- [18].Saadat Z, Nikdoust F, Aerab-Sheibani H, et al. Adherence to antihypertensives in patients with comorbid conditions. Nephr Urol Mon 2015;7:e299863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Kubo MN, Kayima JK, Were AJ, et al. Factors associated with uncontrolled hypertension among renal transplant recipients attending nephrology clinics in Nairobi, Kenya. J Transplant 2015;2015:746563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Kim J, Lee W, Hong Y, et al. Psychometric properties of a short self-reported measure of medication adherence among patients with hypertension treated in a busy clinic setting in Korea. J Epidemiol 2014;24:132–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Li WTL, Kang CD, Tsang PPM, et al. Determinants of medication adherence and blood pressure control among hypertensive patients in Hong Kong: a cross-sectional study. Int J Cardiol 2015;182:250–7. [DOI] [PubMed] [Google Scholar]
- [22].Okwuonu CG, Ojimadu NE, Okaka EI, et al. Patient-reported barriers to hypertension control in a Nigerian population. Int J Gen Med 2014;7:345–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Fernandez-Arias M, Acuna-Villaorduna A, Miranda JJ, et al. Adherence to pharmacotherapy and medication-related beliefs in patients with hypertension in Lima, Peru. PLoS ONE 2014;9:e112875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Girma F, Emishaw S, Alemseged F, et al. Compliance with anti-hypertensive treatment and associated factors among hypertensive patients on follow-up in Jimma University specialized hospital, Jimma, south west Ethiopia: a quantitative cross-sectional study. J Hypertens 2014;3:174. [Google Scholar]
- [25].Lee GKY, Wang HHX, Liu KQL, et al. Determinants of medication adherence to antihypertensive medications among a Chinese population using Morisky medication adherence scale. PLoS ONE 2013;8:e62775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Cuffee YL, Hargraves JL, Briesacher BA, et al. Reported racial discrimination, trust in physicians, and medication adherence among inner-city African Americans with hypertension. Am J Public Health 2013;103:e55–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Kretchy I, Owusu-Daaku F, Danquah S. Spiritual and religious beliefs: do they matter in the medication adherence behavior of hypertensive patients? BioPsychoSocial Med 2013;7:15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Ramli A, Ahmad NS, Paridathathu T. Medication adherence among hypertensive patients of primary health clinics in Malaysia. Patient Prefer Adherence 2012;6:613–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Migneault JP, Dedier JJ, Wright JA, et al. A culturally adapted telecommunication system to improve physical activity, diet quality, and medication adherence among hypertensive African-Americans: a randomized controlled trial. Ann Behav Med 2012;43:62–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Muntner P, Levitan EB, Joyce C, et al. Association between antihypertensive medication adherence and visit-to-visit variability of blood pressure. J Clin Hypertens 2013;15:112–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Zyoud SH, Al-Jabi S, Swelleh WM, et al. Relationship of treatment satisfaction to medication adherence: findings from a cross-sectional survey among hypertensive patients in Palestine. Health Quality Life Outcome 2013;11:191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Leung LB, Busch AM, Nottage SL, et al. Approach to antihypertensive adherence: a feasibility study on the use of students health coaches for uninsured hypertensive adults. Behav Med 2012;38:19–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Breaux-Shropshire TL, Brown KC, Pryor ER, et al. Relationship of blood pressure self-monitoring, medication adherence, self-efficacy, stage of change, and blood pressure control among municipal workers with hypertension. Workplace Health Saf 2012;60:303–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Oliveira-Filho AD, Barreto-Filho JA, Neves SJ, et al. Association between the 8-item Morisky medication adherence scale (MMAS-8) and blood pressure control. Arq Bras Cardiol 2012;99:649–58. [DOI] [PubMed] [Google Scholar]
- [35].Holt EW, Muntner P, Joyce CJ, et al. Health-related quality of life and antihypertensive medication adherence among older adults. Age Ageing 2010;39:481–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Berni A, Ciani E, Cecioni I, et al. Adherence to antihypertensive therapy affects ambulatory atrial stiffness index. Eur J Int Med 2011;22:93–8. [DOI] [PubMed] [Google Scholar]
- [37].Buckley L, Labonville S, Barr J. A systematic review of beliefs about hypertension and its treatment among African Americans. Curr Hypertens Rep 2016;18:52. [DOI] [PubMed] [Google Scholar]
- [38].Hyman DJ, Pavlik V. Medication adherence and resistant hypertension. J Hum Hypertens 2015;29:213–8. [DOI] [PubMed] [Google Scholar]
- [39].Waeber W, Feihi F. Assessment of drug compliance in patients with high blood pressure resistant to antihypertensive therapy. EuroIntervention 2013;9(suppl):R29–34. [DOI] [PubMed] [Google Scholar]
- [40].Carrea NB, Paula de Faria A, Ritter AVM, et al. A practical approach for measurement of antihypertensive medication adherence in patients with resistant hypertension. J Am Soc Hypertens 2016;10:510–6.e1. [DOI] [PubMed] [Google Scholar]
- [41].Lewis LM. Factors associated with medication adherence in hypertensive blacks: a review of the literature. J Cardiovasc Nurs 2012;27:208–19. [DOI] [PubMed] [Google Scholar]
- [42].De Geest S, Ruppar T, Berben L, et al. Medication non-adherence as a critical factor in the management of presumed resistant hypertension: a narrative review. EuroIntervention 2014;9:1102–9. [DOI] [PubMed] [Google Scholar]
- [43].Pladevall M, Brotons C, Gabriel R, et al. Multicenter cluster-randomized trial of a multifactorial intervention to improve antihypertensive medication adherence and blood pressure control among patients at high cardiovascular risk (the COM99 study). Circulation 2010;122:1183–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Conn VS, Enriquez M, Ruppar TM, et al. Meta-analysis of theory use in medication adherence intervention research. Am J Health Behav 2016;40:155–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Ghembaza MA, Senoussaoui Y, Tani MK, et al. Impact of patient knowledge of hypertension complications on adherence to antihypertensive therapy. Curr Hypertens Rev 2014;10:41–8. [DOI] [PubMed] [Google Scholar]
- [46].Conn VS, Rupper TM, Chase JD, et al. Interventions to improve medication adherence in hypertensive patients: systematic review and meta-analysis. Curr Hypertens Rep 2015;17:94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47].Holmes HM, Luo R, Hanlon JT, et al. Ethnic disparities in adherence to antihypertensive medications of Medicare part D beneficiaries. J Am Geriatr Soc 2012;60:1298–303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [48].Wong MC, Jiang JY, Griffiths SM. Antihypertensive drug adherence among 6408 Chinese patients on angiotensin-converting enzyme inhibitors in Hong Kong: a cohort study. J Clin Pharmacol 2010;50:598–605. [DOI] [PubMed] [Google Scholar]
- [49].Ettehad D, Emdin CA, Kiran A, et al. Blood pressure lowering for prevention of cardiovascular diseases and death: a systematic review and meta-analysis. Lancet 2016;387:957–67. [DOI] [PubMed] [Google Scholar]
- [50].James P, Oparil S, Carter B, et al. 2014 Evidence-based guideline for the management of high blood pressure in adults report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA 2014;311:507–20. [DOI] [PubMed] [Google Scholar]
- [51].Egan BM. Treatment resistant hypertension. Ethn Dis 2015;25:495–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [52].de Oliveira-Filho AD, Costa FA, Neves SJ, et al. Pseudoresistant hypertension due to poor medication adherence. Int J Cardiol 2014;172:e309–10. [DOI] [PubMed] [Google Scholar]
- [53].Holt E, Joyce C, Dornelles A, et al. Sex differences in barriers to antihypertensive medication adherence: findings from the cohort study of medication adherence among older adults. J Am Geriatr Soc 2013;61:558–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [54].Coons SJ, Sheahan SL, Martin SS, et al. Predictors of medication noncompliance in a sample of older adults. Clin Ther 1994;16:110–7. [PubMed] [Google Scholar]
- [55].Konin C, Adoh M, Coulibaly I, et al. Black Africans’ compliance to antihypertensive treatment. J Hypertens 2007;25:A11. [PubMed] [Google Scholar]
- [56].Pio M, Baragou S, Afassinou Y, et al. Adherence to hypertension and its determinants in the cardiology department of the university hospital of Lome Tokoin. Pan African Med J 2012;14:48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [57].Ikama MS, Nsitou BM, Loumouamou M, et al. Drug compliance and its factors in a group of hypertensive Congolese. Pan African Med J 2013;15:121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [58].Ghozzi H, Kassis M, Hakim A, et al. Medication adherence of a sample of hypertensive patients in the region of Sfax (Tunisia). Ann Cardiol Angeiol 2010;59:131–7. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


