Abstract
Background:
Osteonecrosis is an incapacitating disorder with high morbidity. Though extracorporeal shockwave therapy (ESWT) provides a noninvasive treatment option, controversial subjects still exist about its effectiveness, indications, and mechanism of action.
Methods:
An electronic databases search was performed using PubMed, Embase, and the Cochrane library to collect clinical trials, case reports, and cases series on this topic and then useful data were extracted and appraised by experienced clinicians. We evaluated the quality of included evidences by using the Oxford Centre for evidence-based medicine (EBM) Levels of Evidence.
Results:
A total of 17 articles including 2 case reports, 9 open label trials, 2 cohorts, and 6 randomized controlled trials were considered to be eligible for this systematic review. Visual analog scale (VAS), Harris hip scores, and the imaging results were the frequently-used outcome estimates of included studies.
Conclusion:
By systematically analyzing these evidences, we could conclude that ESWT could act as a safe and effective method to improve the motor function and relieve the pain of patients with osteonecrosis of femoral hip, especially those at early stage. Imaging revealed that bone marrow edema was significantly relieved, but the necrotic bone could not be reversed after ESWT. This technique could slow or even block the progression of ONFH and therefore reduce the demand for surgery. Collaboration with other conservative modalities would not improve the curative benefits of ESWT. Meanwhile, ONFH with various risk factors showed similar reaction to this noninvasive treatment method. However, these conclusions should be interpreted carefully for the low-quality of included publications and further studies are requisite to validate the effect of ESWT in ONFH.
Keywords: extracorporeal shockwave therapy, osteonecrosis of femoral head, systematic review
1. Introduction
As is well-known, osteonecrosis of femoral head (ONFH) is a debilitating disorder with a considerably high incidence in the young and middle-aged (from the 20s to age 50), and consequently brings huge economic burden around the world.[1,2] Approximately 20,000 patients were estimated to develop ONFH in America every year and another survey showed that the annul morbidity of ONFH in Japan was about 2.51/10,000.[3,4] It is histologically characterized by insufficient supply of blood, death of osteocytes and bone marrow cells, and progressive structure damage of involved bones. Although osteonecrosis only affects the femoral head in most cases, osteonecrosis of other sites, for example, joints of knee, shoulder, wrist, elbow, and ankle also could be seen on clinic. The etiology of osteonecrosis is of various risk factors such as trauma, surgery of hip, corticosteroids, alcoholism, systemic lupus erythematosus, sickle-cell disease, and coagulopathy;[5] however, usually osteonecrotic lesions possess similar pathophysiological alteration.
Multiple options are available for treating ONFH. Surgical treatment methods include core decompression (CD), conversion osteotomy, bone transplants with or without vascular pedicles, total hip arthroplasty (THA) and so on; however, modalities such as weight bearing restriction, alendronate, anticoagulant drugs, lipid-lowering agents and extracorporeal shockwave therapy (ESWT) are employed as noninvasive and biophysical alternatives to solve this challenging disease.[6–9] ESWT was introduced into the medical field after World War II, targeted at managing urinary calculus first and subsequently incidental phenomena that pelvic bone density increased during lithotripsy intrigued orthopedists to apply extracorporeal shockwave to treat musculoskeletal disorders.[10] A amount of studies investigated the effect of ESWT in the treatment of ONFH but high-quality evidence about its mechanism and effectiveness is still urgently needed. CD with/without bone grafting remains the gold standard for hip-salvage treatment.
One systematic review (SR) published in 2009 collected related clinical researches in this field and drew a favorable result. However, this SR only included 5 studies, one of which was case report and another 4 were presented by same medical center.[11] Besides, more literatures on this topic were published in recent years, in which the clinical effect of ESWT was assessed from a more comprehensive perspective and compared with other therapeutic methods. In order to further elucidate this issue and provide reference for clinicians, we included existing clinical evidences so far and made this updated systematic review about the effect of extracorporeal shockwave therapy in the treatment of osteonecrosis of femoral head.
2. Methods
2.1. Search process
For the purpose of collecting potentially eligible publications, we made a computerized search in PubMed, Embase, and Cochrane library using the following terms: (shock wave OR shockwave OR ESWT) and (osteonecrosis OR avascular necrosis OR aseptic necrosis) by 2 investigators (Zhang QY and Liu LH) independently. No time limitations were imposed and the last search was performed on July 31, 2016. Reference lists of relevant articles were also screened manually to retrieve any additionally possible records.
2.2. Inclusion and exclusion criteria
Studies eligible for this systematic review need to meet following criteria: (1) patients diagnosed with ONFH, (2) ESWT was applied to at least part of patients, (3) adequate data were provided to assess the therapeutic effect (e.g., visual analog scores, Harris score, ARCO stage), and (4) the types of included studies contained prospective or retrospective cohort, open label trial, randomized controlled trial, case-control study and case report. If data overlapped in different articles, we only included the most comprehensive or most recent one. Using these predesigned criteria, apparently ineligible articles were first excluded by screening titles and abstracts. The remainders were downloaded and then assessed by scrutinizing the full texts.
2.3. Data extraction and evidence quality appraisal
Requisite data extracted from original articles and then recorded to standardized excel files included: surname of first author, publication year, number and age and gender of participants, number of affected hips, ARCO stage, technological details of ESWT, evaluation indicators and inclusion period. Quality of included studies was appraised by using Oxford Centre for evidence-based medicine (EBM) Levels of Evidence, in which clinical evidences could be grossly divided to 5 levels ranging from I to V and each level could be subdivided. Ia represents the highest-quality evidence and V is the lowest.[12] Any disagreement was resolved through discussion and consensus of investigators.
Because all data in this article were retrieved from published studies, neither ethical approval nor patient consent was required.
3. Results
Through a computerized search using 3 electronic databases, altogether 42 potentially eligible records were retrieved and at the same time 5 additional ones were obtained by screening the reference lists of relevant articles. However, 13 apparently unqualified ones were first removed by evaluating the titles and abstracts. Subsequently another 17 literatures were excluded by screening full texts of remaining records. The article search process as well as reasons for inclusion and exclusion was listed in Fig. 1 in detail.
Figure 1.
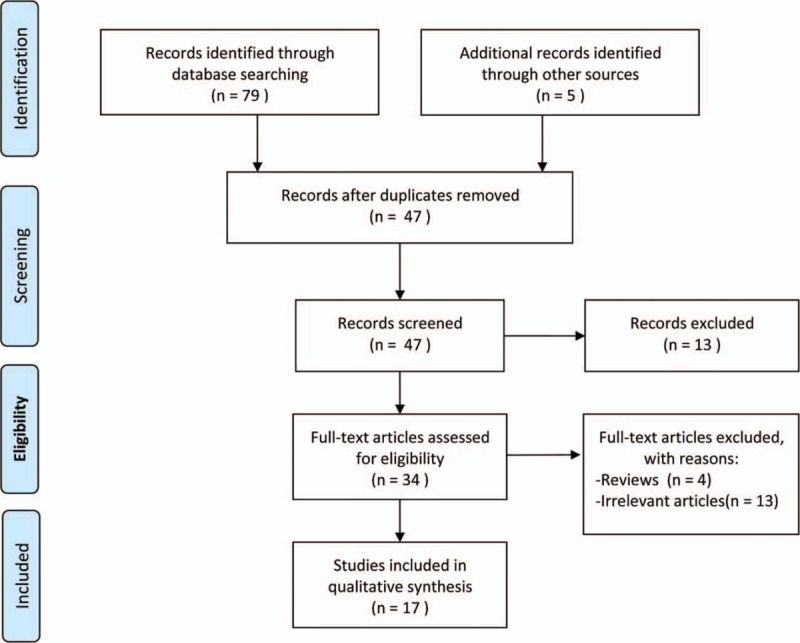
Selection process for eligible studies included in the systematic review.
Eventually, 17[13–29] studies were considered to be eligible for this systematic review, 16[13–21,23–29] of which were published in English and only 1[22] was published in Chinese. Next, we extracted 3 types of useful data from included studies and imported them into different tables: basic information of included publications (Table 1); technological details of extracorporeal shockwave therapy (Table 2) and therapeutic effect assessment indexes of included studies (Table 3).
Table 1.
Basic information of included publications.
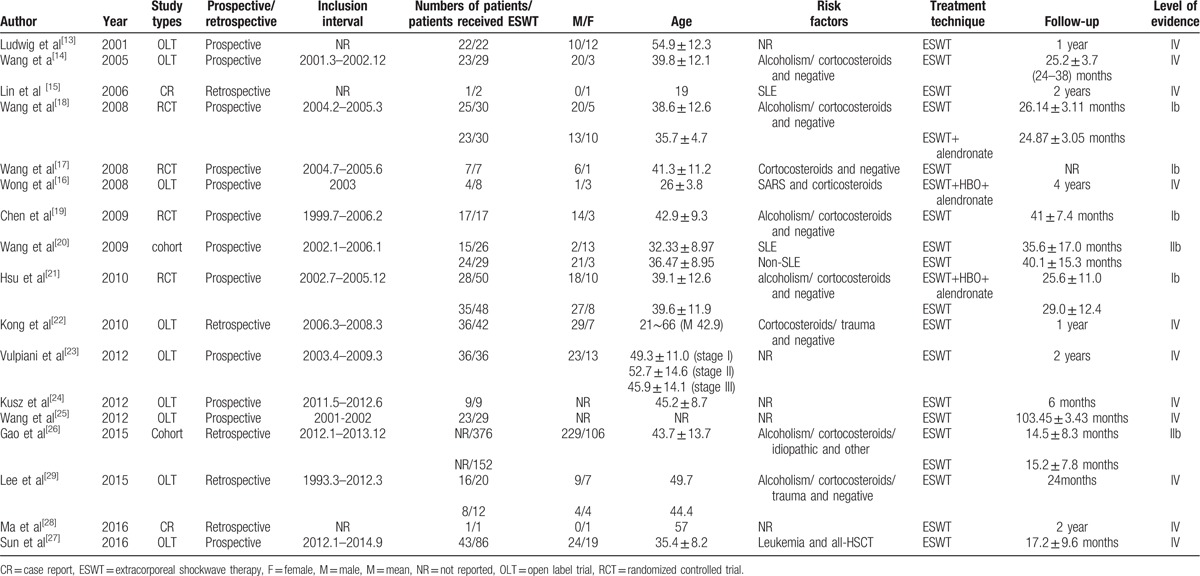
Table 2.
Technological details of extracorporeal shockwave therapy.
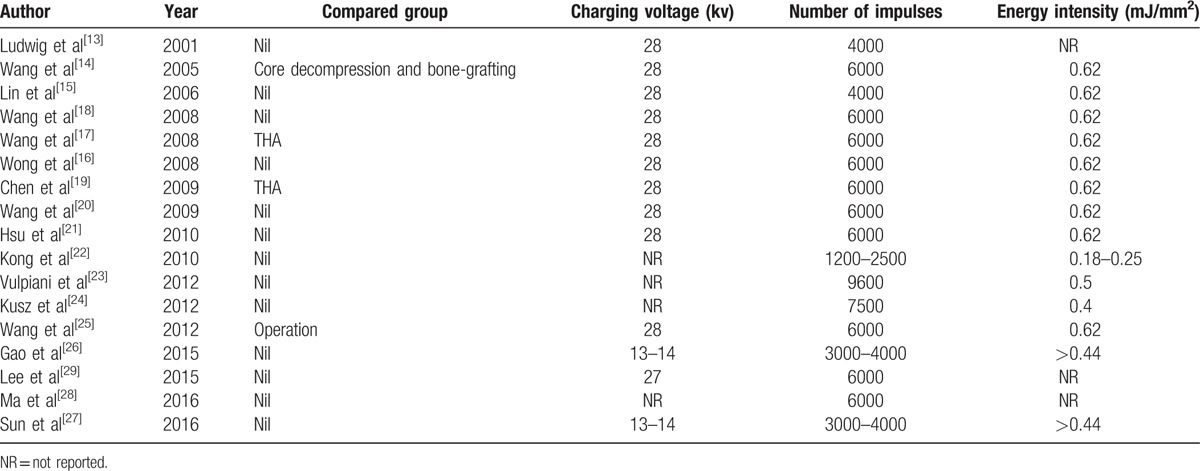
Table 3.
Therapeutic effect assessment indexes of included studies.
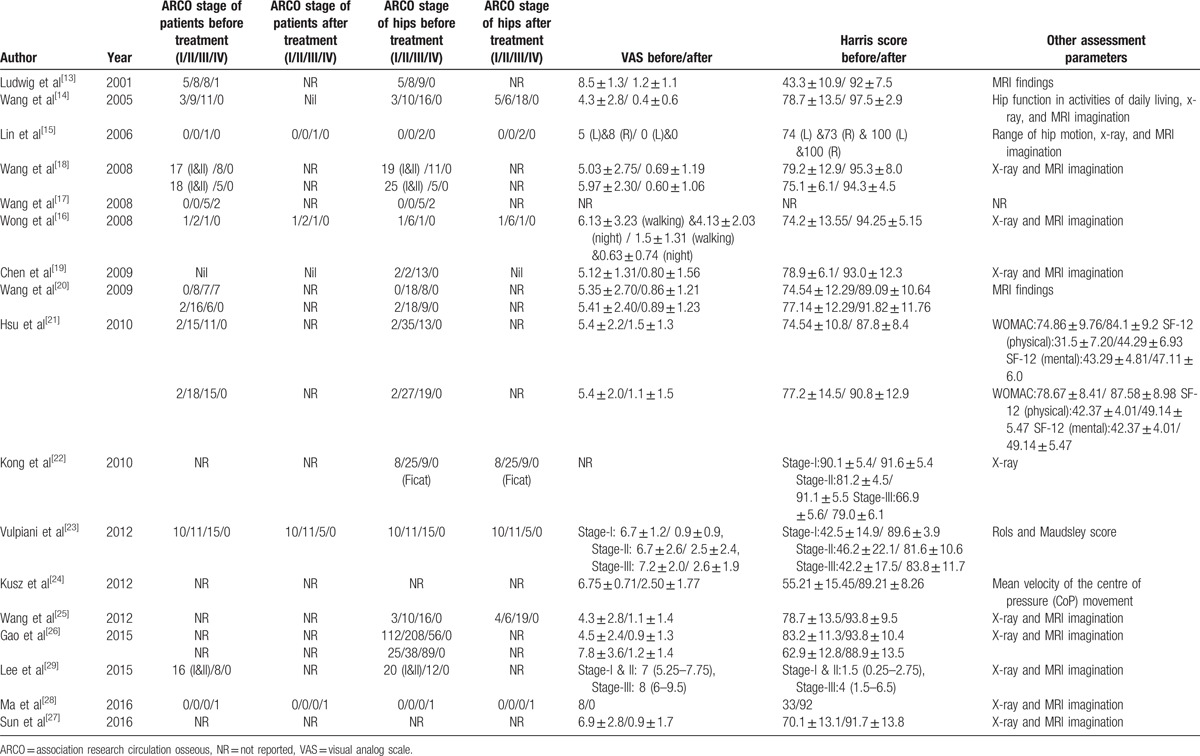
As for the study design, 2[15,28] were case reports, 9[13,14,16,22–25,27,29] were open label trials, 2[20,26] were cohorts, and 4[17–19,24] were randomized controlled trials (RCTs). Twelve[13,14,16–21,23–25,27] studies were prospective ones and 5[15,22,26,28,29] were retrospective ones. All patients were diagnosed with ONFH. Fourteen[14–27] articles provided the energy intensity of ESWT, all of which exceeded 0.18 mj/mm2 and 9 were 0.62 mj/mm2. The patient population of these studies ranged from 1 to 335. Eleven[13,15,16,20,22–24,26–29] studies only investigated the effect of extracorporeal shockwave, 4[14,17,19,25] compared the performance of ESWT with operations (joint-preserving surgeries or endoprosthetic replacement of joint) and 2[18,21] compared the effect of ESWT with cocktail therapy (ESWT combined with other noninvasive modalities). Sixteen[13–16,18–29] studies presented the visual analog scale (VAS) and/or Harris hip score before and after the treatment as evaluation indicators. Other outcome assessment indexes provided by these literatures included the Western Ontario and McMaster Universities Arthritis Index (WOMAC), the 12-item Short Form (SF-12) Survey, magnetic resonance imaging manifestation, the need for surgical intervention as well as numbers of patients with improved, stable and deteriorating conditions.
3.1. Therapeutic effect of ESWT for ONFH
In 2001, Ludwig and his coauthors[13] first suggested that high-energy extracorporeal shockwave might provide a noninvasive alternative for treating ONFH. In this study, a total of 22 patients with ONFH of ARCO I–III stage received 1 (or 2 if necessary) session of ESWT and were followed up for 1 year. The results revealed obvious therapeutic success in 14 patients, in which group patients scored statistically differently at ARCO scale and showed slightly heterogeneous (though not statistically significant) age distribution compared with those resistant to ESWT. Meanwhile, 4 cases of complete healing were observed on MRI. Kong et al[22] supported this conclusion. In their study, 36 ONFH patients involving 42 hips were enrolled and at 1-year follow-up, they declared that cure was observed in 6 hips, marked effect in 13 hips, effectiveness in 16 hips, and ineffectiveness in 7 hips. It must be pointed out that in this study they did not undertake MRI examination and the definition of cure was disappearance of clinical symptoms. In 2012, Vulpiani et al[23] performed a further study by including 36 patients with unilateral ONFH and grouping them according to the ARCO scale. At the same time, the follow-up was extended to 24 months. This study demonstrated that the therapeutic results achieved by ESWT were significantly associated with ARCO stage of patients. ONFH of ARCO stage III responded poorly to ESWT and 10 of the 15 patients had to receive THA during the follow-up. Meanwhile, though clinical symptoms of certain patients were improved, no or only minimal improvement of lesions was observed on plain films or MRIs at all follow-up points. Lee et al's study[29] also divided patients on the basis of ARCO stage and obtained similar results. Kusz et al[24] demonstrated considerable enhancement of quality of life in ONFH patients after ESWT; however, they only followed up patients for 6 weeks. In the study reported by Gao et al,[26] they presented the largest patient population on this topic. A total of 335 patients involving 528 hips were divided into 2 groups according to whether the lateral pillar of femoral head was preserved and both groups showed amelioration of pain, increase of Harris hip scores and slowing of disease progression. They pointed out that the improvement of Harris hip scores was mainly due to the reduction of pains and the lesion decrease on MRI after ESWT was not statistically significant (at the same time, a significant reduction of bone marrow edema was indeed observed). Above-mentioned studies used focused shockwave while in 2016, Ma et al[28] described a case of advanced ONFH opt not to THA and treated with radial ESWT, in which a satisfactory result was obtained. Larger-scale clinical trials are needed to confirm this conclusion.
3.2. Therapeutic effect of ESWT in ONFH with different risk factors
Two studies including a case reported by Lin et al[15] in 2006 and a case series presented by Wang et al[20] in 2009 investigated the use of ESWT in ONFH patients with systemic lupus erythematosus (SLE) and receiving corticosteroids therapy. In Lin et al's article,[15] at 3-year follow-up after ESWT, pain and motor function of bilateral hips of the young ONFH patient were improved and no further progression was observed on MRI. Wang et al's study[20] recruited 1 group of ONFH patients with SLE and another group without SLE, both receiving 6000 impulses of ESWT and then followed up for 3 years. The results revealed that therapeutic effects of 2 groups had no significant difference (P = 0.802, 0.467 and 0.194 for THR, pain scores and function scores, respectively).
Wong et al treated 4 ONFH patients involving 8 hips with cocktail therapy consisting of ESWT, hyperbaric oxygen therapy (HBO) and alendronate.[16] All participants were healthcare workers suffering from severe acute respiratory syndrome (SARS) and had been treated with corticosteroids. At 4-year follow-up, 4 patients returned to work without the need for THA. No improvement or progression of ARCO stage was observed during follow-up.
The therapy of leukemia and allogeneic hematopoietic stem cell transplantation (allo-HSCT) are accompanied with a markedly elevated risk of ONFH. Sun et al[27] recruited 43 ONFH patients with leukemia and justified similar therapeutic effect of ESWT in these patients compared with other ONFH patients. Only 2 hips showed progressive femoral head collapse and accepted THA eventually.
3.3. Comparison with surgery or other alternatives in the treatment of ONFH
In Wang et al's study,[14] 48 ONFH patients with 57 hips were randomized to receive either ESWT or joint-preserving surgery (core decompression and bone-grafting). Participants from 2 groups possessed homogeneous characteristics as well as VAS and Harris hip scores at baseline. At about 2-year follow-up, the ESWT group yielded better outcome in pain relief, Harris scores, hip function in activities of daily living and imaging manifestations. In 2012, Wang et al[25] published a further investigation comparing curative effect of ESWT with core decompression plus autogenous cancellous bone and allogenous fibular graft, and in this study they extended the follow-up to 8- or 9-year. At the last follow-up point, the ratios of good/poor response to treatment were 76/24 and 21/79 in ESWT group and CD group, respectively; meanwhile, THA was applied to 24% and 64% patients in ESWT group and CD group, respectively. Chen and his coworkers included 17 patients with bilateral ONFH, and then treated 17 hips with THA for late disease and other hips with ESWT for early disease.[19] According to the subjective evaluation after treatment, ESWT was valued more highly than THA in 13 patients and believed to be similar to THA in 4 cases. This result indicated that early detection of ONFH was crucial for its management.
Whether a synergistic effect of ESWT and other conservative treatments exists was investigated in 2 literatures. In the study published by Wang et al in 2008, they randomly divided 48 patients to 2 groups, receiving ESWT with and without alendronate, respectively.[18] Eventually, the overall clinical outcomes of 2 curative groups were comparable. The differences of pain and functional enhancement between 2 groups were not statistically significant (P = 0.400 and 0.313, respectively). Hsu et al[21] further combined ESWT, alendronate and HBO to treat early ONFH, and this time, a better result of cocktail therapy than ESWT alone was still not testified. Eventually, 10% patients in the cocktail group and 10.4% patients in the ESWT group had to receive THR (P = 0.946).
3.4. Physiological effect of ESWT
In 2008, Wang et al[17] published a article included 14 patients involving 14 diseased hips graded as ARCO stage III or IV, all of which underwent THA. 7 cases also received ESWT before surgery and others were regarded as control group. ESWT group revealed more live bone and less necrotic bone as well as higher cell concentration and activity compared with control group. Factors for angiogenesis such as von Willebrand factor (vWF), CD31, vascular cell adhesion molecule (VCAM) as well as for bone remodeling and regeneration such as Winless 3a (Wnt 3), Dickkopf-1 (DKK1) and proliferation cell nuclear antigen (PCNA) also had significant differences between ESWT group and control group. These findings prompted the regeneration effects of ESWT to ONFH.
4. Discussion
Total hip arthroplasty has become a mature and reliable operation to remove clinical symptoms of advanced osteonecrosis of femoral head. However, constant need for joint-preserving treatment modalities yielding satisfactory result is still imperative, especially for patients with early ONFH. Until now, the efficacy of most nonsurgical therapeutic methods for ONFH remains disputable, which made them not ready for widely recommendation. In recent several decades, ESWT has been applied to various kinds of musculoskeletal disorders including proximal plantar fascitis, lateral epicondylitis of the elbow, nonunion and delayed union of long bone fracture and so on.[33] As a common disabling disorder, ONFH was also investigated for the effect of ESWT by multiple studies.
We made this SR for the purpose of providing a higher quality evidence to physicians interested in this topic. Eventually, a total of 17 studies were retrieved and remarkable benefits of extracorporeal shockwave for treating ONFH were found to be consistent in included articles. Meanwhile, most included studies only investigated ONFH of ARCO stage I–III; therefore caution should be taken in applying these results and choosing appropriate indications.
As previously mentioned, multiple risk factors could be the etiology of ONFH. In our systematic review, there were 4 studies which investigated the effect of ESWT in ONFH patients with SLE, SARS and leukemia after allo-HSCT.[15,16,20,27] At last, similar effectiveness of ESWT in these certain groups of patients with those indiscriminately recruiting various kinds of ONFH patients was observed. This finding indicated that ESWT could be conducted without considering the risk factors of ONFH.
The exact mechanism of ESWT in the treatment of ONFH is still controversial. High-energy extracorporeal shockwave travels through soft tissue and the change of impedance between soft tissue and bone interface results in energy deposition. This energy deposition of high acoustic waves may explain part of the therapeutic effect of extracorporeal shockwave. Meanwhile, extracorporeal shockwave has the ability to propagate through necrotic femoral hips and at the depth of 10 mm of bone, a pressure loss of 50% of shockwave was observed.[30] One hypothesis is that ESWT could induce microfracture to accelerate bone healing and increase pain threshold.[10] Higher expression level of bone morphogenic protein (BMP)-2, vessel endothelial growth factor (VEGF), alkaline phosphatase, Runt-related transcription factor 2 (RUNX2) and osteocalcin mRNA in marrow stromal cells as well as more mature mineralized nodules were demonstrated in ESWT group compared with control group, in which nitric oxide acted as the mediator.[31] One study showed increased osteogenesis and angiogenesis as well as bone remodeling of diseased hips after ESWT, indicating a regeneration effect.[17,32,33] In experiments with rabbit model, the expression of VEGF, BMP-2 and corresponding mRNA in subchondral bone of necrotic femoral heads was significantly up-regulated, which was consistent with the results in human samples.[34,35]
Durst et al reported that a woman with calcific tendinitis received high-energy extracorporeal shockwave lithotripsy, and about 3 and a half years later she was diagnosed with osteonecrosis of humeral head.[36] Liu et al[37] presented another similar case report in which the onset of osteonecrosis of humeral head occurred only 3 months after ESWT. It is supposed that the high dose of extracorporeal shockwave and relatively small diameter of anterior humeral circumflex in 2 case reports might explain these complications. Though no evident complications of ESWT for treating ONFH was revealed, deterioration of lesions did be observed in some cases. Therefore, before starting ESWT, important arteries and nerves ought to be located with ultrasonography to avoid any possible damage. It is believed that radial ESWT has no need for location in advance but collection of high-quality data is necessary to testify this assumption.
There were several limitations existing in our research. First, the evidence quality of our included studies was various. Only 4 studies were classified as Ib evidence according to Oxford Centre for EBM Levels of Evidence. Second, this is a systematic review and we could only discuss issues based on existing clinical evidences. Third, due to limited number of studies, quantitative analysis (meta-analysis) of extracted data is impossible. Finally, populations of most included studies were very small.
This SR also reminds us of several research directions in the future. Persisting histopathological or even genetic experiments are indispensable to further clarify the mechanism of ESWT in the treatment of ONFH. Meanwhile, charging voltage, energy intensity, focus size, number of session and impulse of extracorporeal shockwave adopted by included studies were heterogeneous; therefore, a standardized therapeutic schedule of ESWT for ONFH needs to be determined. Last but not least, it is urgent for clinicians to discover other effective conservative modalities which could be applied to ONFH alone or enhance the benefits of ESWT.
In a word, extracorporeal shockwave therapy provides a conservative modality to improve the motor function and relieve the pain of patients with osteonecrosis of femoral head. It possesses advantages such as non-invasiveness, safety, convenience to conduct and economy. Imaging revealed that bone marrow edema was significantly relieved but the necrotic bone or femoral head collapse could not be reversed after ESWT. This technique could slow or even block the progression of ONFH and therefore reduce the demand for surgery. ESWT brings more benefits than core decompression with/without bone grafting for early-stage ONFH and there is no evidence revealing that collaboration with other conservative methods could improve the curative effects of ESWT. Meanwhile, ONFH with various risk factors showed similar reaction to this noninvasive treatment method. Nevertheless, these results should be interpreted carefully due to the low quality of included publications and further studies are requisite to validate the effect of ESWT in ONFH.
Footnotes
Abbreviations: allo-HSCT = allogeneic hematopoietic stem cell transplantation, ARCO = association research circulation osseous, BMP = bone morphogenic protein, CD = core decompression, EBM = evidence-based medicine, ESWT = extracorporeal shockwave therapy, ESWT = extracorporeal shockwave therapy, HBO = hyperbaric oxygen therapy, ONFH = osteonecrosis of femoral head, RUNX2 = Runt-related transcription factor 2, SARS = severe acute respiratory syndrome, SF-12 = 12-item Short Form, SLE = systemic lupus erythematosus, SR = systematic review, THA = total hip arthroplasty, VAS = visual analog scale, VEGF = vessel endothelial growth factor, WOMAC = Western Ontario and McMaster Universities Arthritis Index.
QZ and LL contributed equally to this work.
Funding: This study was supported by the National Natural Science Foundation of China (81372013, 81672236) and China-Japan Friendship Hospital Youth Science and Technology Excellence Project (2014-QNYC-A-06).
The authors have no conflicts of interest to disclose.
References
- [1].Aldridge JR, Urbaniak JR. Avascular necrosis of the femoral head: etiology, pathophysiology, classification, and current treatment guidelines. Am J Orthop (Belle Mead, NJ) 2004;33:327–32. [PubMed] [Google Scholar]
- [2].Ma J, Sun W, Gao F, et al. Porous tantalum implant in treating osteonecrosis of the femoral head: still a viable option? Sci Rep 2016;6:28227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Yamaguchi R, Yamamoto T, Motomura G, et al. Incidence of nontraumatic osteonecrosis of the femoral head in the Japanese population. Arthritis Rheum 2011;63:3169–73. [DOI] [PubMed] [Google Scholar]
- [4].Hong YC, Luo RB, Lin T, et al. Efficacy of alendronate for preventing collapse of femoral head in adult patients with nontraumatic osteonecrosis. Biomed Res Int 2014;2014:716538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Malizos KN, Karantanas AH, Varitimidis SE, et al. Osteonecrosis of the femoral head: etiology, imaging and treatment. Eur J Radiol 2007;63:16–28. [DOI] [PubMed] [Google Scholar]
- [6].van der Jagt D, Mokete L, Pietrzak J, et al. Osteonecrosis of the femoral head: evaluation and treatment. J Am Acad Orthop Surg 2015;23:69–70. [DOI] [PubMed] [Google Scholar]
- [7].Zalavras CG, Lieberman JR. Osteonecrosis of the femoral head: evaluation and treatment. J Am Acad Orthop Surg 2014;22:455–64. [DOI] [PubMed] [Google Scholar]
- [8].Unal MB, Cansu E, Parmaksizoglu F, et al. Treatment of osteonecrosis of the femoral head with free vascularized fibular grafting: results of 7.6-year follow-up. Acta Orthop Traumatol Turc 2016;50:323–9. [DOI] [PubMed] [Google Scholar]
- [9].Fessel J. There are many potential medical therapies for atraumatic osteonecrosis. Rheumatology (Oxford) 2013;52:235–41. [DOI] [PubMed] [Google Scholar]
- [10].Wang CJ. Extracorporeal shockwave therapy in musculoskeletal disorders. J Orthop Surg Res 2012;7:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Alves EM, Angrisani AT, Santiago MB. The use of extracorporeal shock waves in the treatment of osteonecrosis of the femoral head: a systematic review. Clin Rheumatol 2009;28:1247–51. [DOI] [PubMed] [Google Scholar]
- [12].Atkins D, Eccles M, Flottorp S, et al. Systems for grading the quality of evidence and the strength of recommendations I: critical appraisal of existing approaches The GRADE Working Group. BMC Health Serv Res 2004;4:38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Ludwig J, Lauber S, Lauber HJ, et al. High-energy shock wave treatment of femoral head necrosis in adults. Clin Orthop Relat Res 2001;387:119–26. [DOI] [PubMed] [Google Scholar]
- [14].Wang CJ, Wang FS, Huang CC, et al. Treatment for osteonecrosis of the femoral head: comparison of extracorporeal shock waves with core decompression and bone-grafting. J Bone Joint Surg Am 2005;87:2380–7. [DOI] [PubMed] [Google Scholar]
- [15].Lin PC, Wang CJ, Yang KD, et al. Extracorporeal shockwave treatment of osteonecrosis of the femoral head in systemic lupus erythematosis. J Arthroplasty 2006;21:911–5. [DOI] [PubMed] [Google Scholar]
- [16].Wong T, Wang CJ, Hsu SL, et al. Cocktail therapy for hip necrosis in SARS patients. Chang Gung Med J 2008;31:546–53. [PubMed] [Google Scholar]
- [17].Wang CJ, Wang FS, Ko JY, et al. Extracorporeal shockwave therapy shows regeneration in hip necrosis. Rheumatology (Oxford) 2008;47:542–6. [DOI] [PubMed] [Google Scholar]
- [18].Wang CJ, Wang FS, Yang KD, et al. Treatment of osteonecrosis of the hip: comparison of extracorporeal shockwave with shockwave and alendronate. Arch Orthop Trauma Surg 2008;128:901–8. [DOI] [PubMed] [Google Scholar]
- [19].Chen JM, Hsu SL, Wong T, et al. Functional outcomes of bilateral hip necrosis: total hip arthroplasty versus extracorporeal shockwave. Arch Orthop Trauma Surg 2009;129:837–41. [DOI] [PubMed] [Google Scholar]
- [20].Wang CJ, Ko JY, Chan YS, et al. Extracorporeal shockwave for hip necrosis in systemic lupus erythematosus. Lupus 2009;18:1082–6. [DOI] [PubMed] [Google Scholar]
- [21].Hsu SL, Wang CJ, Lee MS, et al. Cocktail therapy for femoral head necrosis of the hip. Arch Orthop Trauma Surg 2010;130:23–9. [DOI] [PubMed] [Google Scholar]
- [22].Kong FR, Liang YJ, Qin SG, et al. Clinical application of extracorporeal shock wave to repair and reconstruct osseous tissue framework in the treatment of avascular necrosis of the femoral head (ANFH) (article in Chinese). Zhongguo Gu Shang 2010;23:12–5. [PubMed] [Google Scholar]
- [23].Vulpiani MC, Vetrano M, Trischitta D, et al. Extracorporeal shock wave therapy in early osteonecrosis of the femoral head: prospective clinical study with long-term follow-up. Arch Orthop Trauma Surg 2012;132:499–508. [DOI] [PubMed] [Google Scholar]
- [24].Kusz D, Franek A, Wilk R, et al. The effects of treatment the avascular necrosis of the femoral head with extracorporeal focused shockwave therapy. Ortop Traumatol Rehabil 2012;14:435–42. [DOI] [PubMed] [Google Scholar]
- [25].Wang CJ, Huang CC, Wang JW, et al. Long-term results of extracorporeal shockwave therapy and core decompression in osteonecrosis of the femoral head with eight- to nine-year follow-up. Biomed J 2012;35:481–5. [DOI] [PubMed] [Google Scholar]
- [26].Gao F, Sun W, Li Z, et al. High-energy extracorporeal shock wave for early stage osteonecrosis of the femoral head: a single-center case series. Evid Based Complement Alternat Med 2015;2015:468090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Sun W, Gao F, Guo W, et al. Focused extracorporeal shock wave for osteonecrosis of the femoral head with leukemia after allo-HSCT: a case series. Bone Marrow Transplant 2016;51:1507–9. [DOI] [PubMed] [Google Scholar]
- [28].Ma YW, Jiang DL, Zhang D, et al. Radial extracorporeal shock wave therapy in a person with advanced osteonecrosis of the femoral head: a case report. Am J Phys Med Rehabil 2016;95:e133–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Lee JY, Kwon JW, Park JS, et al. Osteonecrosis of femoral head treated with extracorporeal shock wave therapy: analysis of short-term clinical outcomes of treatment with radiologic staging. Hip Pelvis 2015;27:250–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Hausdorf J, Lutz A, Rohrig H, et al. Extracorporeal shock wave therapy and femur head necrosis--pressure measurements in the femur head. Z Orthop Ihre Grenzgeb 2004;142:122–6. [PubMed] [Google Scholar]
- [31].Yin TC, Wang CJ, Yang KD, et al. Shockwaves enhance the osteogenetic gene expression in marrow stromal cells from hips with osteonecrosis. Chang Gung Med J 2011;34:367–74. [PubMed] [Google Scholar]
- [32].Wang CJ, Wang FS, Yang KD, et al. Shock wave therapy induces neovascularization at the tendon-bone junction. A study in rabbits. J Orthop Res 2003;21:984–9. [DOI] [PubMed] [Google Scholar]
- [33].Ioppolo F, Rompe JD, Furia JP, et al. Clinical application of shock wave therapy (SWT) in musculoskeletal disorders. Eur J Phys Rehabil Med 2014;50:217–30. [PubMed] [Google Scholar]
- [34].Ma HZ, Zeng BF, Li XL. Upregulation of VEGF in subchondral bone of necrotic femoral heads in rabbits with use of extracorporeal shock waves. Calcif Tissue Int 2007;81:124–31. [DOI] [PubMed] [Google Scholar]
- [35].Ma HZ, Zeng BF, Li XL, et al. Temporal and spatial expression of BMP-2 in sub-chondral bone of necrotic femoral heads in rabbits by use of extracorporeal shock waves. Acta Orthop 2008;79:98–105. [DOI] [PubMed] [Google Scholar]
- [36].Durst HB, Blatter G, Kuster MS. Osteonecrosis of the humeral head after extracorporeal shock-wave lithotripsy. J Bone Joint Surg Br 2002;84:744–6. [DOI] [PubMed] [Google Scholar]
- [37].Liu HM, Chao CM, Hsieh JY, et al. Humeral head osteonecrosis after extracorporeal shock-wave treatment for rotator cuff tendinopathy. A case report. J Bone Joint Surg Am 2006;88:1353–6. [DOI] [PubMed] [Google Scholar]


