Abstract
To investigate the influence of resident seniority on supervised clinical practice in the emergency department (ED).
This was a retrospective, 1-year cohort study conducted in 5 EDs within Taiwan largest healthcare system. All adult nontrauma visits presenting to the EDs during the day shift between July 1, 2011 and June 30, 2012 were included in the analysis. Visits were divided into supervised (ie, treated by resident under attending physician's supervision) and attending-alone. Supervised visits were further categorized by resident seniority (junior, intermediate, and senior). The decision-making time (door-to-order and door-to-disposition time), patient dispositions (eg, ED observation and hospital admission), and diagnostic tool use (laboratory examination or computed tomography [CT]) were selected as clinical performance indicators. The differences in clinical performance were determined between supervised visits (ie, resident-seniority groups) and attending-alone visits.
Junior residents were found to have longer median door-to-order and door-to-disposition time than were the other residents for urgent and nonurgent patients. Furthermore, compared with attending-alone visits, supervised visits with junior residents had a greater odds of ED observation (adjusted odds ratio [aOR], 1.1; 95% CI, 1.07–1.20), while supervised visits with all 3 resident-seniority groups had significantly greater odds of laboratory examinations (junior: aOR, 1.1; 95% CI, 1.03–1.16; intermediate: aOR, 1.1; 95% CI, 1.04–1.15; and senior: aOR, 1.1; 95% CI, 1.05–1.15).
As resident seniority increases, less time is needed for decision making in supervised visits. However, compared to attending-alone visits, supervised visits still resulted in greater use of laboratory examinations and delayed patient disposition.
Keywords: emergency, practice, resident, supervised
1. Introduction
High quality patient care can only be provided if physicians are well prepared for this task through residency training.[1] In the emergency department (ED), residents are trained and educated via patient primary care under the supervision of attending physicians, who review histories and physical examinations, adjust treatment options, discuss disposition plans, and assist with procedures.[2] The effect of residency training on clinical practice in the ED setting has been much debated during the past few decades.[3–5] One recent research has noted that resident participation in clinical practice in the ED is associated with greater resource consumption, including greater use of diagnostic tools and increased ED length of stay, which can result in ED congestion.[6] These findings apply to both student- and resident-trainee visits.[7] However, the influence of resident seniority on clinical practice in the ED is still unclear. To realize the clinical practice discrepancy among different seniority residents is important. It is because it could help us to arrange better medical trainee program along with minimal effect on patient's outcome and clinical efficiency. Thus, the aim of the present study is to clarify the influence of resident seniority on supervised practice in ED. Specifically, the authors hypothesized that the clinical practice of senior residents might be more close to attending physicians. As study outcomes, the authors focused on 3 aspects of ED practice: decision-making time, patient disposition, and diagnostic tool use. It is believed that the outcome of the study might also be used to establish the guideline of resident evaluation.
2. Materials and methods
2.1. Study design
This was a retrospective, 1-year cohort study approved by the institutional review board of the Chang Gung Medical Foundation. All patients’ and physicians’ records and information were anonymized and deidentified before analysis.
2.2. Study setting and participants
This study was conducted in 5 EDs within the largest healthcare system in Taiwan, which receives 8% to 10% of the national health insurance budget according to government statistics. The study period was July 1, 2011 to June 30, 2012. The 5 EDs were geographically dispersed nationwide. Two EDs were in tertiary referral medical centers with 80 and 60 ED beds. The other 3 were in secondary regional hospitals with between 15 and 30 ED beds. Other than the smallest ED, all EDs were the largest in their respective counties. All 5 EDs were teaching hospitals and had a cumulative number of mean annual visits of over 480,000.
All adult nontrauma patients who presented to the EDs during the day shift within the study period were included in the analysis. All of the ED visits were classified according to disease acuity according to the Five Level Taiwan Triage and Acuity Scale (TTAS), which is a commonly used triage system formulated by the Department of Health in Taiwan.[8] The TTAS determines patient acuity according to their presenting vital signs (ie, heart rate, blood pressure, respiration rate, and oxygen saturation) and main complaint. For example, a patient who is presenting with dyspnea or chest pain and unstable vital signs would be determined as 2nd level triage patients, or, if immediate resuscitation is needed, even 1st level patients.
The day shift comprised 8 hours corresponding to the duties of the emergency physicians, which was mostly 7:00 to 15:00 (7:30–15:30 in 1 branch). Attending physicians are required to indicate all day-shift patients’ dispositions, including their discharge, hospital admission, and ED observation room admission. Patients who are admitted to the ED observation room would then be handed over to the evening-shift emergency physicians. In one of the EDs (located in a tertiary referral medical center), where 3 attending physicians worked at the same time, patients were assigned to different attending physicians according to their disease acuity (as per the TTAS): 1 physician was in charge of 1st and 2nd level triage patients, 1 was in charge of 3rd level patients, and the remaining physician was in charge of 4th and 5th level patients. In the other tertiary referral medical center (wherein 3 attending physicians also worked at any one time) as well as 2 of the secondary regional hospitals (wherein only 2 attending physicians worked together at any one time), patients were assigned alternatively via computer as they presented to each attending physician in charge. In the remaining secondary regional hospital, only one attending physician was in charge at any time.
As all study sites were teaching medical units, residents assisted in the treatment of ED patients under an attending physician's supervision. All supervised visits were initially evaluated and treated by residents; attending physician consults were usually required. Residents’ independence in clinical practice increased with their seniority. Although senior residents might only consult the attending physician to determine a patient's final disposition or to order particular examinations such as a computed tomography (CT) scan, junior residents more frequently discussed clinical practice with the attending physicians. There was no specific arrangement of duty shift according to the attending physician's and resident's seniority. None of the examinations was prescribed by nursing staff.
Overall, 93 full-time attending physicians were involved in this study; 17 worked only in one tertiary referral medical center, and another 17 worked only in one secondary regional hospital. The other 59 rotated among the other tertiary referral medical center and 2 secondary regional hospitals. All 93 attending physicians were qualified emergency physicians and received the same residency training program, which was developed by the Taiwan Society of Emergency Medicine.
Emergency resident training in Taiwan comprises a 4-year program, followed by a 5th year, which corresponds to a fellowship that takes place after the individual is qualified to be an emergency physician. Residents can also take a postgraduate year, which is a general medicine training course in Taiwan that usually comprises 1 or 2 months of ED training; this is similar to the transitional year residency program in the U.S. Eighty-six resident trainees were involved in this study, including 29 postgraduate year residents, 12 1st-year residents, 11 2nd-year residents, 15 3rd-year residents, 10 4th-year residents, and 9 5th-year residents. Thirty-eight residents (25 postgraduate year, 2 1st-year, 4 2nd-year, 4 3rd-year, 2 4th-year, and 1 5th-year) remained in one of the tertiary referral medical centers, while another 7 (1 1st-year, 2 2nd-year, 2 3rd-year, 0 4th-year, and 2 5th-year) worked only in one secondary regional hospital. The other 41 residents (4 postgraduate year, 9 1st-year, 5 2nd-year, 9 3rd-year, 8 4th-year, and 6 5th-year) rotated among the other tertiary referral medical center and 2 secondary regional hospitals. Residents were grouped according to their seniority, as follows: postgraduate year and 1st-year residents were considered “junior residents”; 2nd- and 3rd-year residents were “intermediate residents”; and 4th- and 5th-year residents were “senior residents.”
2.3. Study protocol
All ED visits were divided into supervised or attending-alone. Supervised visits were defined as visits treated by the resident under the supervision of the attending physician, and the medical record would contain both the resident's and the attending physician's electronic signature, while attending-alone visits were those wherein only the attending physician was involved in treatment with only the attending physician's signature. To keep physician's records anonymized, only the resident seniority and attending physician status were preserved before data analysis. All other physician personal information was removed. The authors’ main analysis involved determining the differences in clinical performance indicators between the supervised visits (broken down by the resident-seniority groups) and the attending-alone visits.
2.4. Measures
Demographic factors (age, sex, disease acuity, and medical setting) of the patients were drawn from the ED administrative database. As noted above, disease acuity was defined according to the TTAS,[8] wherein patients identified as having the 1st and 2nd triage levels should be seen immediately or within 10 minutes, respectively, and are defined as urgent. In contrast, patients assigned the 3rd, 4th, and 5th triage levels should be assessed within 30, 60, or 120 minutes, respectively, and are classified as nonurgent.
To evaluate decision-making time, the authors used the time interval between the patient being assigned to a physician and the physician completing the 1st order prescription (door-to-order time) and patient disposition (door-to-disposition time). The 1st order prescription included medication treatment, laboratory examinations, or image studies. Patient dispositions were classified into discharge, hospital admission (including general ward and intensive care unit), ED observation (admission to ED observation room), and ED mortality.[9]
ED diagnostic tool use was assessed according to the diagnostic investigations ordered by physicians, including laboratory examination (eg, complete blood count, blood chemistry, urine analysis, stool analysis, or influenza screen test) and CT scans. These examinations were selected because the time needed to obtain the results of these examinations and their cost made these investigations suitable to our investigation of ED resources use.
2.5. Data analysis
For continuous variables, the data were summarized as means and standard deviations (SDs). Because the distributions of door-to-order and door-to-disposition times were not normal, we used medians with interquartile ranges and the nonparametric Kruskal–Wallis test to describe and evaluate their associations with emergency physician seniority. The distributions of categorical demographic factors (sex, disease acuity, and medical setting), patient disposition (discharge, admission, ED observation, and ED mortality), and diagnostic tool use (laboratory examination and CT) were described with numbers and percentages, and chi-square tests were used to evaluate the associations between these variables and visit type (including resident seniority). To analyze the associations of clinical practice indicators with visit type (including resident seniority) while adjusting for potential confounding factors (age, sex, disease acuity, and medical setting), multinomial logistic regression was selected for patient disposition, and binomial logistic regression for diagnostic tool use. Effects were estimated in terms of odds ratios (ORs) and the corresponding 95% confidence intervals. Significance testing was 2-sided, and the significance threshold was set at P < 0.05. SPSS version 12.0 (SPSS, Chicago, IL) was used for all statistical analyses.
3. Results
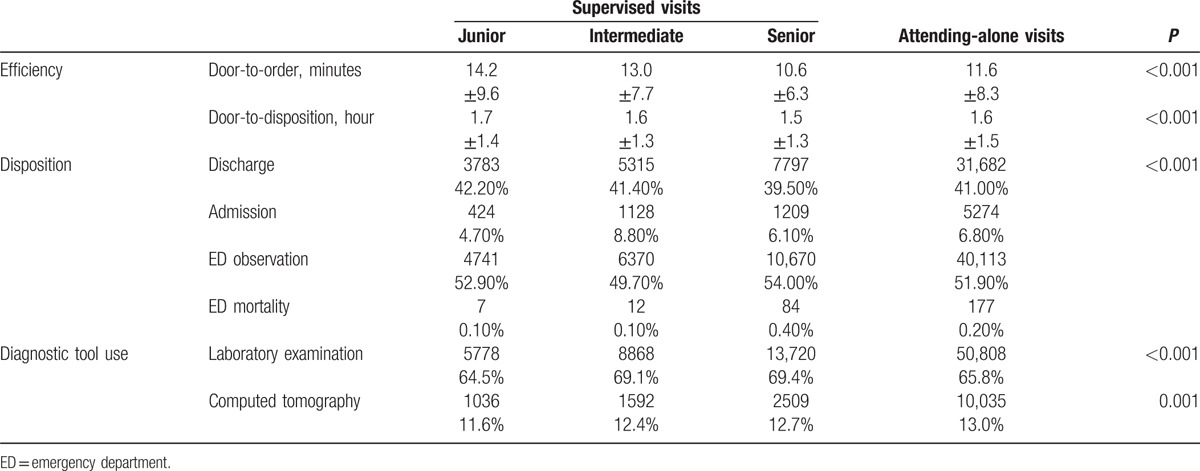
During the 1-year study period, there were 118,802 ED visits. The patients’ relevant demographic factors (patient's age, sex, disease acuity, and medical settings) are shown in Table 1. There were statistically significant differences in patient's age, sex, disease acuity, and patient distribution in medical settings among the 4 study groups. In attending-alone visits and supervised visits with senior residents, there was a greater proportion with urgent disease acuity. Further analysis of the distribution of 1st and 2nd triage levels in these visits revealed that 8.6% of supervised visits with junior residents were at the 1st triage level, followed by 13.9% of intermediate residents, 17.5% of senior residents, and 17.6% of attending-alone visits. The descriptive statistics of the clinical practice indicators (door-to-order and door-to-disposition time, patient disposition, and diagnostic tool use) are shown in Table 2. Statistically significant differences in clinical practice were found between the supervised visits and attending-alone visits.
Table 1.
The patients’ relevant basic demographic factors of supervised visits and attending-alone visits.
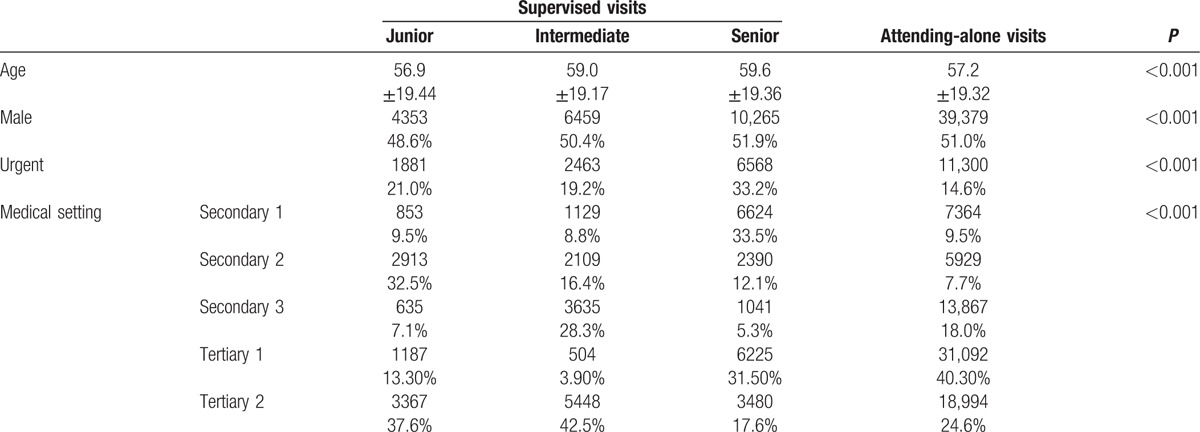
Table 2.
Clinical practice of supervised visit and attending-alone visit.
As shown in Fig. 1A, B, there were statistically significant associations between resident seniority and emergency physician efficiency among urgent and nonurgent patients (P < 0.001 for both door-to-order time and door-to-disposition time, according to a Kruskal–Wallis test). Supervised visits of junior residents (postgraduate year and 1st-year residents) were found to have longer door-to-order (12.9 and 14.5 minutes, respectively) and door-to-disposition (2 and 1.6 hours) times than were other residents for urgent and nonurgent patients (intermediate residents: door-to-order time, 12.1 and 13.2 minutes; door-to-disposition time, 1.9 and 1.5 hours; senior residents: door-to-order time, 9.9 and 11.0 minutes; door-to-disposition time, 1.9 and 1.4 hours; all P < 0.001).
Figure 1.
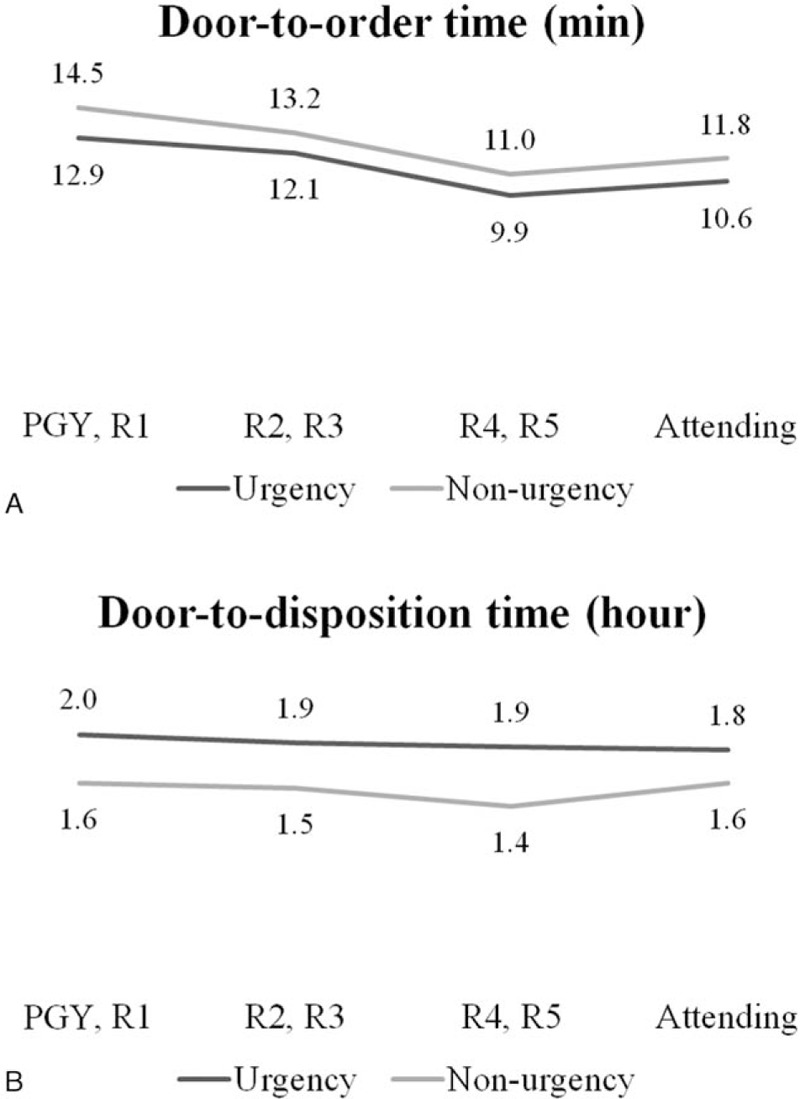
The distribution of door-to-order time (A) and door-to-disposition time (B) clinically made by the emergency physicians among urgent and nonurgent patients. Note: Door-to-order time (minutes) represents the time interval between patient registration and EP prescribing the 1st order, and door-to-disposition time (hours) represents the time interval between patient registration and emergency physician completing disposition order. The 2 types of data were presented as median with IQRs and nonparametric Kruskal–Wallis tests were used to evaluate the differences. Both P < 0.001 for door-to-order time and door-to-disposition time. (Door-to-order time: urgent: PGY, R1: 12.9 [8.1]; R2, R3: 12.1 [7.0]; R4,R5: 9.9 [5.9]; attending: 1.6 [6.7]; nonurgent: PGY, R1: 14.5 [10]; R2, R3: 13.2 [7.8]; R4,R5: 11.0 [6.5]; attending: 11.8 [8.6]; door-to-disposition time: urgent: PGY, R1: 2.0 [1.5]; R2, R3: 1.9 [1.3]; R4, R5: 1.9 [1.4]; attending: 1.8 [1.4]; nonurgent: PGY, R1: 1.6 [1.4]; R2, R3: 1.5 [1.3]; R4, R5: 1.4 [1.3]; attending: 1.6 [1.4]; data are median (IQR)). R1, 1st-year resident; R2, 2nd-year resident; R3, 3rd-year resident; R4, 4th-year resident; and R5, 5th-year resident. IQR = interquartile range, PGY = postgraduate year resident.
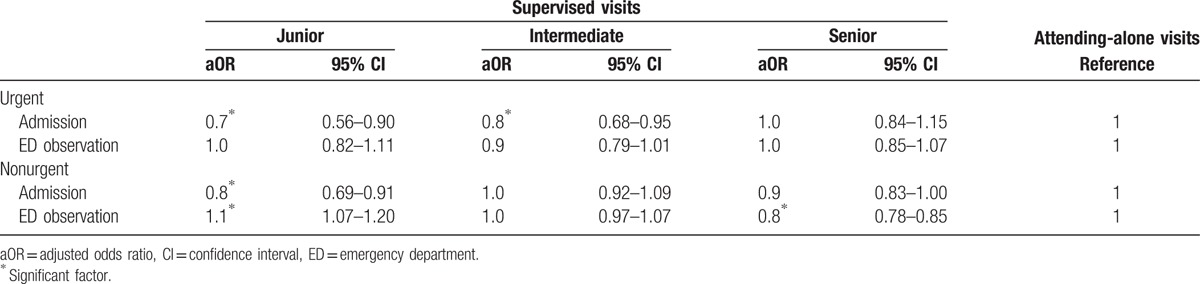
To control for potential confounding factors and analyze the disposition difference between supervised visits and attending-alone visits, multinomial logistic regression was applied with discharge as the reference category and adjusting for patient's age, sex, and medical settings. This analysis was stratified by disease acuity. Compared to attending-alone visits, supervised visits with junior and intermediate residents had lower odds of hospital admission for urgent patients (adjusted odds ratio [aOR]: 0.7 and 0.8, respectively). Similarly, for nonurgent patients, supervised visits with junior residents showed lower odds of hospital admission (aOR: 0.8) but greater odds of ED observation (aOR: 1.1). Supervised visits with senior residents showed lower odds of ED observation among nonurgent patients (aOR: 0.8; Table 3).
Table 3.
Association of patient disposition with supervised visits, adjust for age, sex, and medical setting by multinomial logistic regression with discharge as reference category.
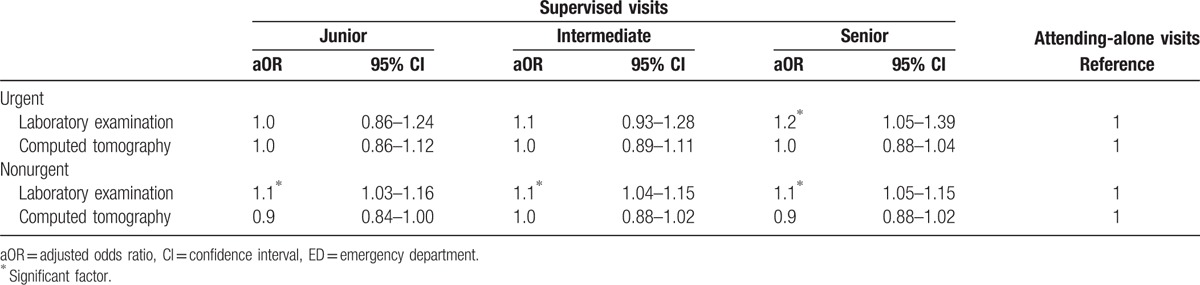
Finally, binomial logistic regression was used to analyze diagnostic tool use while controlling for the confounding factors of patient's age, sex, and medical settings. Again, the analysis was stratified by disease acuity. Compared to attending-alone visits, supervised visits with the 3 resident-seniority groups had greater odds of obtaining laboratory examinations for nonurgent patients; in contrast, the odds of laboratory examinations were greater in supervised visits with senior residents among urgent patients. There were no significant differences in CT scan use between supervised visits and attending-alone visits (Table 4).
Table 4.
Association of ED diagnostic tool use with supervised visits, adjust for age, sex, and medical setting by binomial logistic regression.
4. Discussion
Although recent research has indicated that supervised visits in the ED consume more resources than do attending-alone visits,[6] the influence of residents’ seniority is so far unclear. The few studies that have analyzed the influence of resident seniority on ED performance mainly focused on productivity (ie, patient visits per hour).[10,11] The authors of the present study confirmed that supervised visits consistently consumed greater ED resources, thereby supporting past findings. Importantly, the results also revealed the influence of resident seniority on ED clinical performance. A significant strength of the present study was that the 5 EDs (in 2 tertiary referral medical centers and 3 secondary regional hospitals) studied were geographically well dispersed nationwide, which suggests that the sample was nationally representative of ED visits in Taiwan.
Resident seniority influenced the door-to-order and door-to-disposition times for supervised visits, regardless of whether the patient was urgent or nonurgent. These findings are in line with those of a previous study, wherein supervised visits involving residents were characterized by better productivity (ie, number of patients seen per hour) compared to supervised visits involving medical students.[12] Notably, in supervised visits, senior residents took less time to complete their order prescriptions. Furthermore, a slightly increased door-to-order time was observed for attending alone visits compared to supervised visits of senior residents, which might have been because the attending physician had more duties in the ED, such as resident supervision, during the supervised visits. The increased door-to-order time in supervised visits with junior and intermediate residents might be related to their immature clinical skills and need to repeatedly consult attending physicians. In contrast, senior residents have greater clinical experience and independence in clinical practice, meaning that the door-to-order time would be decreased. Resident seniority had a similar effect on door-to disposition time: namely, the time needed to determine patients’ disposition in supervised visits decreased as resident seniority increased for both urgent and nonurgent patient. This result is compatible with a previous study, wherein the door-to-disposition time for patient discharge was greater among supervised visits, especially the medical student group.[7] Many factors could contribute to this result, including the greater number of examinations in supervised visits and patient re-evaluation by attending physicians.
Previous studies demonstrated that supervised visits were associated with a greater likelihood of hospital admission.[6] However, in this study, supervised visits with junior and intermediate residents resulted in a lower admission rate. This might be due to the myth of patients’ triage level. First, senior residents and attending physicians were responsible for more patients at the 1st triage level (8.6%, 13.9%, 17.5%, and 17.6% among supervised visits with junior, intermediate, senior residents, and among attending-alone visits, respectively). Second, the present study classified patients based on triage at ED presentation to determine the urgency of medical needs. However, clinical conditions among the same triage levels can vary, which can sometimes result in different outcomes.[13] Thus, it was believed that senior residents and attending physicians were responsible for more critical patient care in the ED; therefore, it was not surprizing that there would be lower admission rates among supervised visits with junior and intermediate residents. On the other hand, in supervised visits with junior residents of nonurgent patients, there was a greater likelihood of ED observation. This can be explained by the fact that discharge decisions are more difficult for emergency physicians when patients are initially managed by a resident.[14] Thus, the attending physicians would have had greater difficulty making decisions on patient disposition when patients were initially evaluated by junior residents. In this case, physicians may have been more likely to keep patients for observation in the ED.
Some previous studies discussed the impact of residents on ED diagnostic tool before,[15,16] but most were localized, single-hospital trials. One recent multicenter study by Pitts et al[6] reported increased diagnostic tool use among supervised visits. The present study further analyzed the influence of resident seniority and its interaction with disease acuity on ED diagnostic tool use. Supervised visits among nonurgent patients more often resulted in laboratory examinations compared to attending-alone visits. This is perhaps because residents have less clinical experience than do attending physicians and they therefore order more laboratory examinations to support their clinical decisions on patients with nonurgent presentations. This same scenario was not found for urgent supervised visits with junior and intermediate residents, which instead might be related to the reason for triage level mentioned in relation to patient disposition above. The urgent supervised visits with senior residents also resulted in more laboratory examinations than did attending-alone visits. As such, despite the seniority increase, supervised visits still resulted in increased laboratory examination use. There was no significant difference in CT scan use between the supervised and attending-alone visits. A possible explanation for this was that before ordering high cost examinations such as CT scans, residents discuss with their supervising attending physicians.
5. Limitation
The present study has several limitations. First, the 5 study sites belonged to the same medical system, which may limit generalization of the conclusions to other medical settings with different resident training models. Second, this study did not trace the patients’ outcomes after the end of the day shift, so it could not determine whether patient groups were over-or under-admitted. Third, the administrative data could not supply critical information on many aspects of care, such as the interpersonal quality, technical quality, or appropriateness of care received. Finally, due to the limitations of retrospective studies in general, the authors could not control for all possible confounding factors. As such, it was not possible to conclude that only resident seniority governed the discrepancies in clinical practice observed. Further prospective studies are needed to determine the causality of resident seniority on clinical performance, patient outcomes, and patient and family satisfaction.
6. Conclusion
The present study provides a more comprehensive discussion of supervised practice in the ED by analyzing the influence of resident seniority. With increasing seniority, there was a small decrease in door-to-order and door-to-disposition time. However, all resident groups, even in senior residents, still led to greater laboratory examination use. Supervised visits with junior residents also lead to more patients remaining in the ED for observation. Previous studies reported that supervision is required for emergency medicine residents, and that such supervision should include direct patient interviews and examinations by the attending physician instead of being limited to case discussion or ED record cosignatures.[17,18] The authors recommend that more direct intervention be applied by attending physicians during supervised visits to reduce unnecessary ED resource use and facilitate patient disposition, even when supervising senior residents.
Acknowledgments
The authors thank the Kaohsiung Chang Gung Memorial Hospital for supporting this research by making substantial contributions to acquisition of data
Footnotes
Abbreviations: aOR = adjusted odds ratio, CT = computed tomography, ED = emergency department.
I-MC and Y-JS contributed equally.
C-JL and Y-RL contributed equally.
Funding/support: This study was supported in part by research grants from the Kaohsiung Chang Gung Memorial Hospital (CMRP-G8C0361).
The authors have no conflicts of interest to disclose.
References
- [1].Weiss KB, Bagian JP, Nasca TJ. The clinical learning environment: the foundation of graduate medical education. Jama 2013;309:1687–8. [DOI] [PubMed] [Google Scholar]
- [2].Lammers RL, Roiger M, Rice L, et al. The effect of a new emergency medicine residency program on patient length of stay in a community hospital emergency department. Acad Emerg Med 2003;10:725–30. [DOI] [PubMed] [Google Scholar]
- [3].McGarry J, Krall SP, McLaughlin T. Impact of resident physicians on emergency department throughput. West J Emerg Med 2010;11:333–5. [PMC free article] [PubMed] [Google Scholar]
- [4].Smalley CM, Jacquet GA, Sande MK, et al. Impact of a teaching service on emergency department throughput. West J Emerg Med 2014;15:165–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Ahmed N, Devitt KS, Keshet I, et al. A systematic review of the effects of resident duty hour restrictions in surgery: impact on resident wellness, training, and patient outcomes. Ann Surg 2014;259:1041–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Pitts SR, Morgan SR, Schrager JD, et al. Emergency department resource use by supervised residents vs attending physicians alone. JAMA 2014;312:2394–400. [DOI] [PubMed] [Google Scholar]
- [7].DeLaney M, Zimmerman KD, Strout TD, et al. The effect of medical students and residents on measures of efficiency and timeliness in an academic medical center emergency department. Acad Med 2013;88:1723–31. [DOI] [PubMed] [Google Scholar]
- [8].Ng CJ, Yen ZS, Tsai JC, et al. Validation of the Taiwan triage and acuity scale: a new computerised five-level triage system. Emerg Med J 2011;28:1026–31. [DOI] [PubMed] [Google Scholar]
- [9].Van Leer PE, Lavine EK, Rabrich JS, et al. Resident supervision and patient safety: do different levels of resident supervision affect the rate of morbidity and mortality cases? J Emerg Med 2015;49:944–8. [DOI] [PubMed] [Google Scholar]
- [10].Henning DJ, McGillicuddy DC, Sanchez LD. Evaluating the effect of emergency residency training on productivity in the emergency department. J Emerg Med 2013;45:414–8. [DOI] [PubMed] [Google Scholar]
- [11].Brennan DF, Silvestri S, Sun JY, et al. Progression of emergency medicine resident productivity. Acad Emerg Med 2007;14:790–4. [DOI] [PubMed] [Google Scholar]
- [12].Bhat R, Dubin J, Maloy K. Impact of learners on emergency medicine attending physician productivity. West J Emerg Med 2014;15:41–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Farrohknia N, Castren M, Ehrenberg A, et al. Emergency department triage scales and their components: a systematic review of the scientific evidence. Scand J Trauma Resusc Emerg Med 2011;19:42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Finn KM, Heffner R, Chang Y, et al. Improving the discharge process by embedding a discharge facilitator in a resident team. J Hosp Med 2011;6:494–500. [DOI] [PubMed] [Google Scholar]
- [15].McNamara RM, Kelly JJ. Cost of care in the emergency department: impact of an emergency medicine residency program. Ann Emerg Med 1992;21:956–62. [DOI] [PubMed] [Google Scholar]
- [16].Scholer SJ, Pituch K, Orr DP, et al. Effect of health care system factors on test ordering. Arch Pediatr Adolesc Med 1996;150:1154–9. [DOI] [PubMed] [Google Scholar]
- [17].Sacchetti A, Carraccio C, Harris RH. Resident management of emergency department patients: is closer attending supervision needed? Ann Emerg Med 1992;21:749–52. [DOI] [PubMed] [Google Scholar]
- [18].Sox CM, Burstin HR, Orav EJ, et al. The effect of supervision of residents on quality of care in five university-affiliated emergency departments. Acad Med 1998;73:776–82. [DOI] [PubMed] [Google Scholar]


