Abstract
Atherosclerotic carotid stenosis (ACS) is a major cause of ischemic stroke. Screening for asymptomatic ACS is important to identify the patients who require longitudinal surveillance, medication, or endovascular surgery. The aim of this study was to assess the prevalence and risk factors for ACS and carotid plaque (CP) in Korea using a population-based screening study.
We recruited participants during visits to several community welfare centers in Korea. The baseline characteristics of the study population were collected. All patients underwent duplex ultrasonography to examine their bilateral carotid arteries. ACS was defined as the presence of plaque with ≥50% vessel diameter reduction and peak systolic velocity (PSV) ≥125 cm/s or PSV ratio ≥2.0. CP was defined as the presence of plaque with <50% vessel diameter reduction. The Mann–Whitney test, χ2 test, Fisher exact test, and logistic regression were used in the statistical analysis.
A total of 3030 participants were enrolled in this study (male 43.7% and female 56.3%). The prevalence of ACS and CP was 1.1% and 5.7%, respectively. Significant risk factors for CP included age ≥80 years (odds ratio [OR], 8.11; 95% confidence interval [CI], 3.45–18.93), male sex (OR, 2.16; 95% CI, 1.29–3.61), hypertension (OR, 1.72; 95% CI, 1.21–2.45), and hyperlipidemia (OR, 1.84; 95% CI, 1.30–2.62). The presence of ACS was significantly associated with age (OR, 1.07; 95% CI, 1.03–1.12), hypertension (OR, 3.16; 95% CI, 1.34–7.46), and being an ex-smoker (OR, 6.81; 95% CI, 1.66–27.93) or current smoker (OR, 6.97; 95% CI, 1.78–27.31) after adjusting for confounding factors.
This population-based screening study revealed that ACS was uncommon and had a prevalence of 1.1% in the study population. Age, hypertension, and smoking were risk factors for ACS. Further investigations into the prevalence and risk factors of ACS are required, as are studies on the cost-effectiveness of a national screening program.
Keywords: atherosclerosis, carotid artery plaque, carotid stenosis, risk factor
1. Introduction
Cerebrovascular disease (CVD) is a major cause of death in Korea. More than 80% of strokes are ischemic, with the rest being hemorrhagic, and atherosclerotic stenosis of the extracranial carotid artery accounts for 15% to 20% of ischemic strokes.[1] Given that plaque formation is integral to the development of atherosclerosis, it is evident that the presence of carotid plaque (CP) may predict future cardiovascular events.[2]
Carotid duplex ultrasound (CDUS) is a noninvasive imaging modality that can safely and accurately measure atherosclerotic carotid stenosis (ACS). As such, it is often used in the early detection of atherosclerosis. However, the cost-effectiveness of using CDUS to screen for ACS has long been debated.[3,4] CDUS is not recommended for screening asymptomatic individuals in the general adult population.[5–7] Symptomatic individuals or adults with high risk factors for carotid atherosclerotic disease are recommended to undergo CDUS screening.[5,8]
Screening individuals with asymptomatic but significant ACS is important, so that patients who require longitudinal surveillance, medication, or surgical treatment can be identified. Several studies regarding the prevalence of ACS have been conducted. However, most of these are based on health maintenance examinations in the hospital,[9–12] and the prevalence of ACS in the general population has not been reported. The purpose of this study was to investigate the prevalence of asymptomatic ACS and CP in the general population, as well as to assess the risk factors for these conditions.
2. Materials and methods
Between January 2008 and December 2012, we visited community welfare halls in Seoul, Gyeonggi-do, Ulsan, and Pohang to conduct the ACS screening. Figure 1 presents a flowchart summarizing this study. All participants older than 50 years who consented to CDUS were included in the study. To avoid selection bias, recruitment took place only with the official document of authority, and without any advertisements or rewards. Interviews were used to collect the baseline characteristics of the participants, as well as the presence of any underlying diseases. In this study, hypertension was defined as having a history of diagnosed hypertension or the current use of antihypertensive pharmacological therapy. Diabetes mellitus (DM) was defined as having a history of diabetes or the use of oral hypoglycemic agents to treat diabetes. Hyperlipidemia was defined as having a history of diagnosed hyperlipidemia and/or treatment by a physician. Current smoking was defined as smoking or having stopped smoking cigarettes in the 1 year before the survey took place, and ex-smoking as having stopped smoking cigarettes >1year before the survey. Drinking was defined as the consumption of any type of alcohol.
Figure 1.
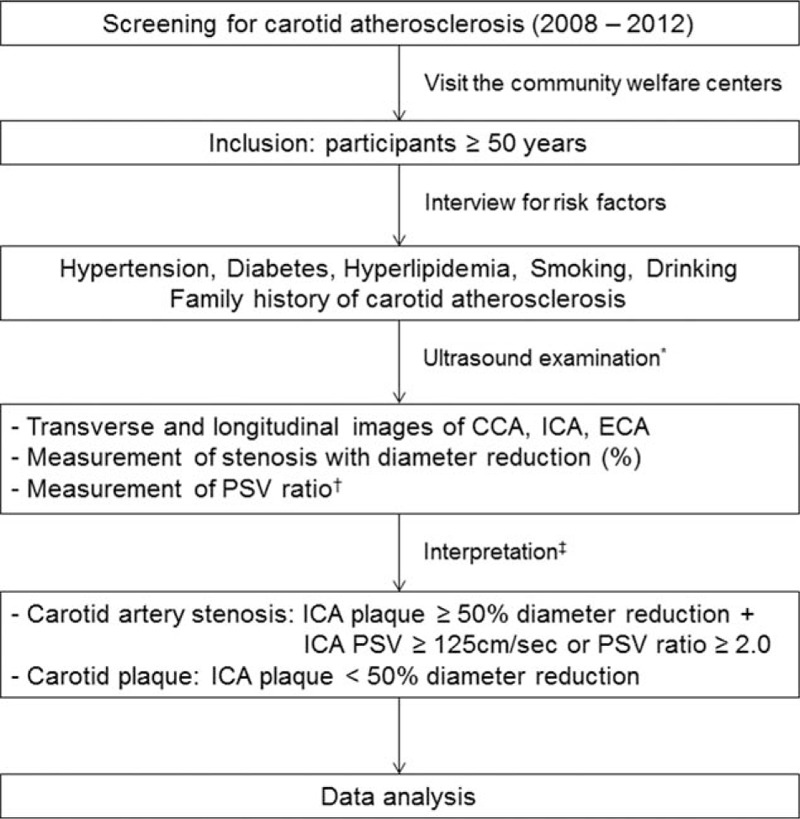
Flowchart of summarizing this study. CCA = common carotid artery, ECA = external carotid artery, ICA = internal carotid artery, PSV = peak systolic velocity. ∗Ultrasound examination was performed by an experienced sonographer who earned the certification of Registered Vascular Technologist. †The PSV ratio was calculated with the PSV of ICA divided by the PSV of CCA obtained at the CCA, 2 cm proximal to the carotid bifurcation. ‡Ultrasound results were interpreted by a vascular surgeon who earned the certification of Registered Physician for Vascular Interpretation.
CDUS was used to examine both of each participant's carotid arteries. We used 2 types of ultrasound equipment—Zonare (Zonare Medical Systems, Mountain View, CA) and HD7 (Philips, Amsterdam, the Netherlands) equipped with a 5 to 12 MHz linear array transducer. CDUS was performed by 2 experienced sonographers who had earned the certification of Registered Vascular Technologist from the American Registry for Diagnostic Medical Sonography (ARDMS). These scans were interpreted by a vascular surgeon who had earned the certification of Registered Physician in Vascular Interpretation from ARDMS. During the scan, the patient was positioned supine with the head resting flat on the bed with a rolled-up towel under the neck. The carotid arteries were imaged in the transverse and longitudinal planes. The common carotid artery (CCA), its bifurcation, and the internal carotid artery (ICA) on each side were examined for the presence of ACS or CP. Caliper measurements were used to estimate the reduction in vessel diameter caused by the plaque. The pulsed Doppler sample volume was swept continuously throughout the length of the vessels to search for areas of increased velocity or flow disturbance in the longitudinal orientation. The peak systolic velocities (PSV) of the CCA and ICA were obtained at the areas of increased velocity. The PSV ratio was calculated with the PSV of the ICA divided by the PSV obtained at the CCA, 2 cm proximal to the carotid bifurcation.
ACS was defined as the presence of plaque with ≥50% vessel diameter reduction and increased PSV ≥125 cm/s or increased PSV ratio ≥2.0. CP was defined as presence of plaque with <50% vessel diameter reduction and a focal thickening that encroached into the lumen by 50% of the surrounding intima-media thickness. Figure 2 showed the typical images of ACS and CP. The baseline characteristics of the participants were compared using the Mann–Whitney test, χ2 test, and Fisher exact test. After each factor had been tested in a simple logistic regression, potential confounders in the univariate models were adjusted for, and a multivariate model was used to examine the association between ACS or CP and underlying disease or demographic factors. The results of the logistic models were presented as odds ratio (OR) and 95% confidence interval (CI). All statistical tests were conducted at the 0.05 level. All statistical analyses were conducted using SPSS software version 21 (SPSS PC version 21.0, SPSS Inc, Chicago, IL). This study was approved by Kyung Hee University Hospital at Gangdong Institutional Review Board, Seoul, Korea.
Figure 2.
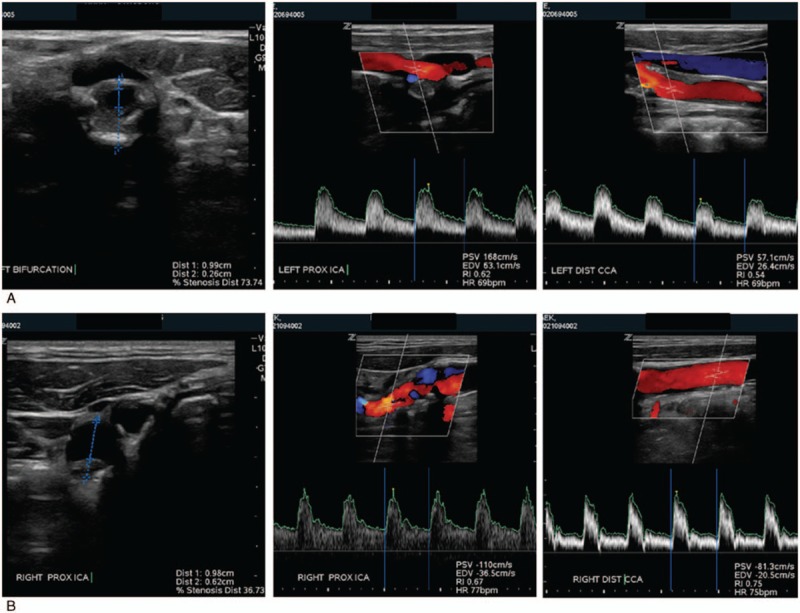
Ultrasound images of carotid artery stenosis and plaque. (A) Atherosclerotic carotid stenosis: diameter reduction 73%, peak systolic velocity of internal carotid artery 168 cm/s, PSV ratio 2.9 (168 cm/s ÷ 57 cm/s). (B) Carotid plaque: diameter reduction 36%, peak systolic velocity of internal carotid artery 110 cm/s, PSV ratio 1.3 (110 cm/s ÷ 81 cm/s).
3. Results
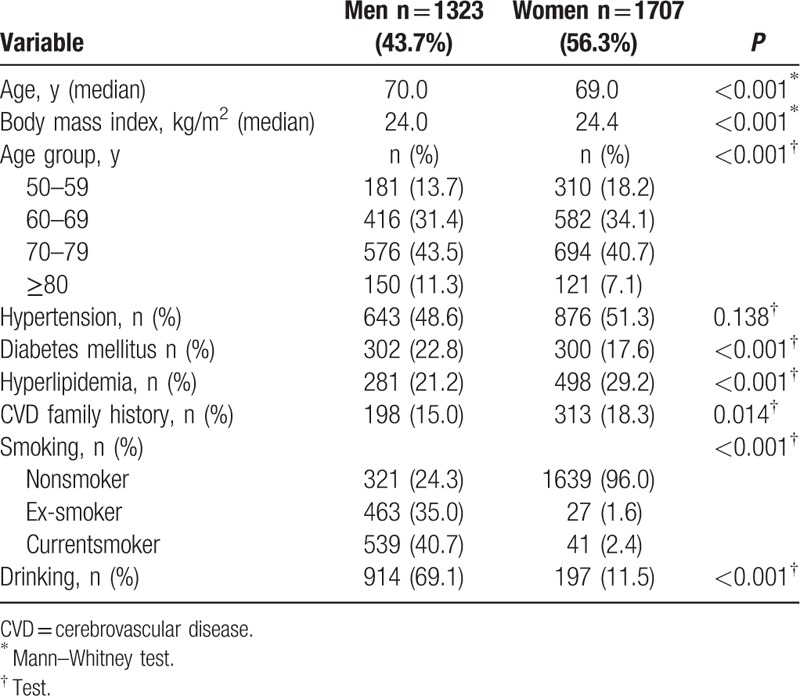
Three thousand and thirty participants were enrolled in this study. This comprised 1323 (43.7%) males and 1707 (56.3%) females with a combined median age of 70.0 years (range, 50–100 years). Table 1 lists the general characteristics of the study population according to sex. The median age was higher in the male participants than in the female participants (P < 0.001). The body mass index (BMI) was higher in the female group (P < 0.001). In both sexes, the highest-frequency age group was the 70- to 79 years’ group. In the male group, the commonest risk factors included diabetes mellitus (DM), smoking (ex-smoker and current smoker), and drinking, and these were all statistically significant.
Table 1.
Characteristics of the study population.
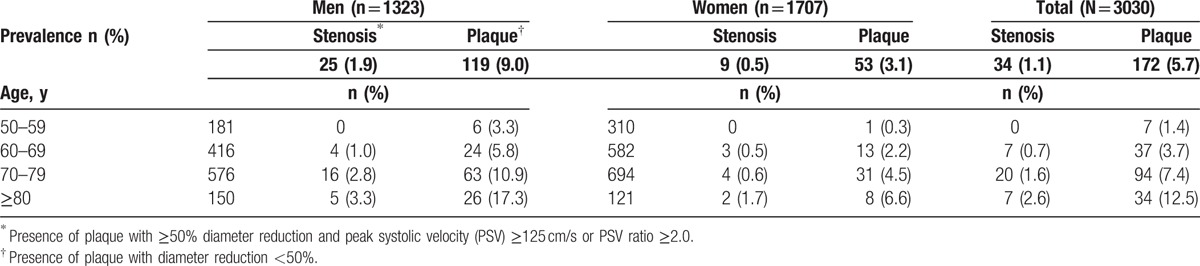
The prevalence of ACS and CP by age and sex is shown in Table 2. The overall prevalence of ACS was 1.1%. The prevalence of ACS in males and females was 1.9% and 0.5%, respectively. In both sexes, the prevalence of ACS increased with age. The overall prevalence of CP was 5.7%, and was higher in males than in females. The prevalence of ACS and CP increased with age.
Table 2.
The prevalence of the atherosclerotic carotid stenosis and plaque by age and sex.
Male sex, increased age, hypertension, DM, hyperlipidemia, smoking, and drinking were significantly associated with the presence of CP (Table 3). Participants with CP had a median age of 74 years. The prevalence of CP was 3 times higher in the male sex than in the female sex, and this was statistically significant (P < 0.001). In the multivariate analysis, risk factors including increased age, male sex, hypertension, and hyperlipidemia were independently associated with CP (Table 4).
Table 3.
Univariate analysis of risk factors for carotid plaque.
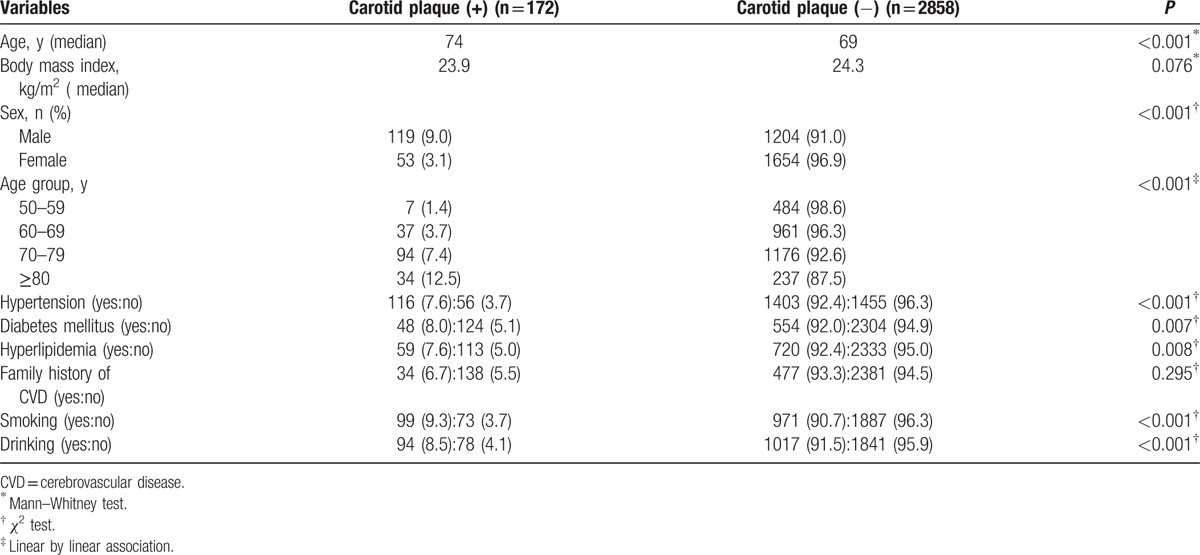
Table 4.
Multivariate analysis of risk factors for carotid plaque.
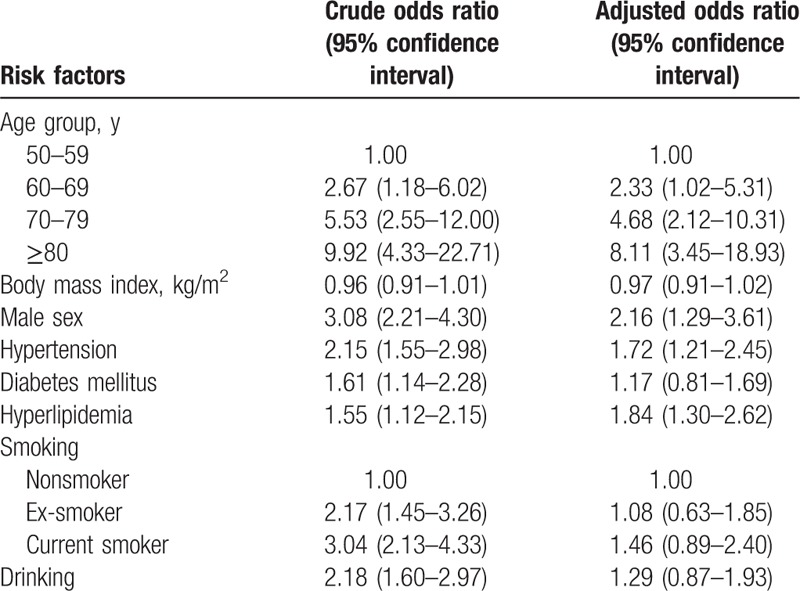
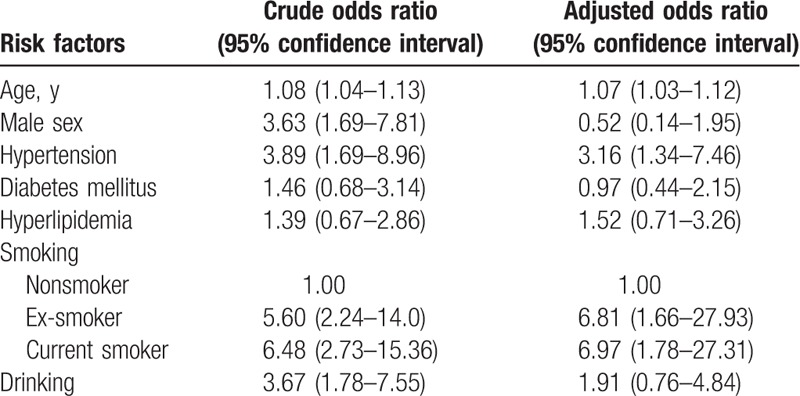
Similarly, in the analysis of variables for ACS, risk factors including male sex, increased age, hypertension, smoking, and drinking were significantly associated with ACS (Table 5). Participants with ACS had a median age of 73 years. The frequency of ACS was 4 times higher in males than in females (P < 0.001). The multivariate analysis showed that increased age, hypertension, and smoking (being an ex-smoker or a current smoker) were independent risk factors for the occurrence of ACS (Table 6).
Table 5.
Univariate analysis of risk factors for atherosclerotic carotid stenosis.
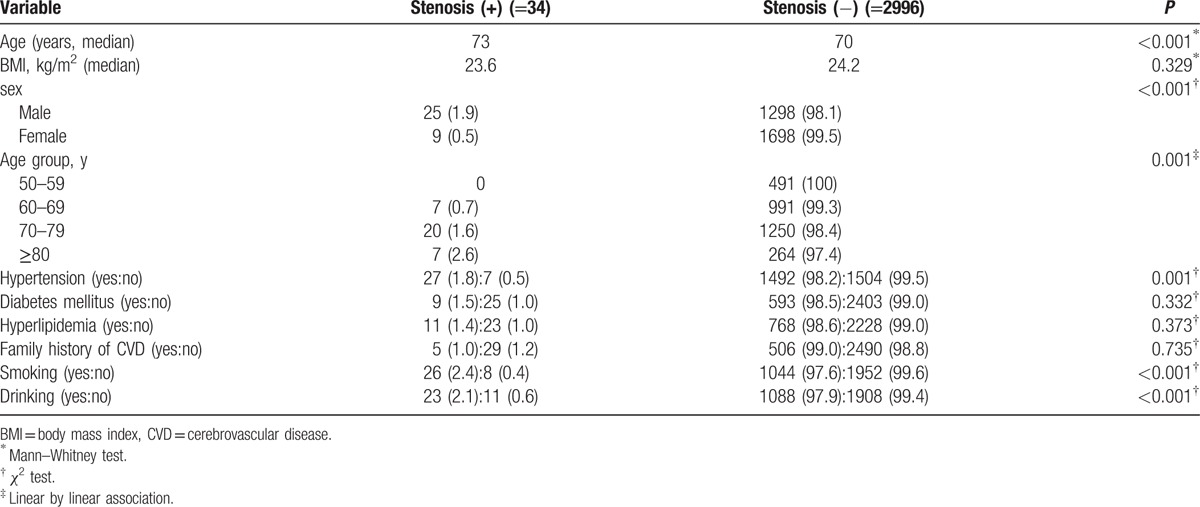
Table 6.
Multivariable analysis of risk factors for atherosclerotic carotid stenosis.
4. Discussion
The aim of this study was to evaluate the prevalence of ACS and CP in a population-based study, as well as to investigate the risk factors associated with these conditions. The overall prevalence of ACS was 1.1%, with a prevalence of 1.9% in males and 0.5% in females. The prevalence of ACS was lower in this study compared to other population-based studies conducted in Asian countries. One population-based study using ultrasound found that the prevalence of ACS was 7.9% in males and 1.3% in females.[13] Another study of 1499 subjects over 60 years of age reported a prevalence of 12.7% in males and 6.2% in females.[14] This difference may stem from the different definitions of ACS used in each study. In the present study, ACS was defined as the presence of plaque with ≥50% vessel diameter reduction and PSV ≥125 cm/s or PSV ratio ≥2.0. In the other 2 studies, ACS was defined as ≥50% vessel diameter reduction without PSV. B-mode can be detected independent of the operator's skills, and so the prevalence of ACS may appear artificially high. Therefore, it is important to use increased PSV parameters to provide a more accurate definition of ACS.[15]
The prevalence of ACS in Western studies was slightly higher than that found in the present study. A population-based study in Italy reported a prevalence of 2.7% in males and 1.5% in females.[16] The Tromso study in Norway reported a prevalence of 3.8% and 2.7% in 3016 males and 3404 females, respectively.[17] A published meta-analysis of 4 population-based studies reported a prevalence of 0% to 3.1%.[18] A large population-based Swedish study of 65-year-old men reported a prevalence of 2%.[19] A possible reason for the higher prevalence of ACS in Western populations is that their average BMI tends to be higher than that of Asian populations. In the present study, the BMI was 24.0 kg/m2 for males and 24.3 kg/m2 for females, which is lower than the BMI of 25.9 to 26.7 kg/m2 reported in the aforementioned meta-analysis.[18] In addition, ethnic differences may also contribute to this discrepancy. Previous studies have shown that the prevalence of ACS varies by race, and tends to be lower in Asian populations.[20,21]
In this study, increased age, hypertension, and smoking were independent risk factors associated with ACS.[22] Increased age was a significant risk factor for ACS in both genders. This is consistent with the findings of many previous studies, which have suggested that the increasing stiffness of blood vessel walls with increasing age may be the underlying mechanism.[16,17,21]
Hypertension was another independent risk factor for ACS, which is also consistent with results of previous studies.[13,16,17,19] High blood pressure leads to the deposition of cholesterol in the arteries, which increases the risk of atherosclerotic plaque rupture and stroke.[23]
It is well known that smoking is a strong risk factor for ACS. Being an ex-smoker or current smoker carries a more than 6-fold risk of ACS than in nonsmokers. Several Western studies have also confirmed this.[24]
Screening for carotid atherosclerosis has been highly debated. Several guidelines do not recommend the screening of general population.[4,6,7,25] But there are recommendations for screening of high-risk population wit cardiovascular risk factors.[8] This study showed that the significant risk factors for carotid artery stenosis were old age, hypertension, and smoker. Therefore, it might be possible to recommend the ultrasound screening for carotid artery stenosis in this high risk group. There are several limitations in this study. The variables for risk factors were obtained from questionnaires. Although the interviews had been conducted by medical professionals, self-reported data may inadvertently include an inherent recall bias. And this study was performed with visiting the welfare centers. Therefore, the selection bias exists because the welfare users can be interested in the health maintenance. In addition, because of the cross-sectional study design, the clinical significance throughout time could not be determined.
In conclusion, the prevalence of ACS and CP in our study was 1.1% and 5.7%, respectively. ACS was observed in 1.9% of males and 0.5% of females included in the study. Age, hypertension, and smoking were independent risk factors for ACS. Further investigations into the cost-effectiveness of a national screening program are required.
Footnotes
Abbreviations: ACS = atherosclerotic carotid stenosis, BMI = body mass index CCA = common carotid artery, CDUS = carotid duplex ultrasound, CI = confidence interval, CP = carotid plaque, CVD = cerebrovascular disease, DM = diabetes mellitus, ECA = external carotid artery, ICA = internal carotid artery, OR = odd ratio, PSV = peak systolic velocity, RPVI = Registered Physician in Vascular Interpretation, RVT = Registered Vascular Technologist.
The authors report no conflicts of interest.
References
- [1].Petty GW, Brown RD, Whisnant JP, et al. Ischemic stroke subtypes: a population-based study of incidence and risk factors. Stroke 1999;30:2513–6. [DOI] [PubMed] [Google Scholar]
- [2].Naqvi TZ, Lee MS. Carotid intima-media thickness and plaque in cardiovascular risk assessment. JACC Cardiovasc Imaging 2014;7:1025–38. [DOI] [PubMed] [Google Scholar]
- [3].Cull DL, Cole T, Miller B, et al. The value of a carotid duplex surveillance program for stroke prevention. Ann Vasc Surg 2011;25:887–94. [DOI] [PubMed] [Google Scholar]
- [4].Jonas DE, Feltner C, Amick HR, et al. Screening for asymptomatic carotid artery stenosis: a systematic review and meta-analysis for the U.S. Preventive Services Task Force. Ann Intern Med 2014;161:336–46. [DOI] [PubMed] [Google Scholar]
- [5].LeFevre ML. Force USPST Screening for asymptomatic carotid artery stenosis: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med 2014;161:356–62. [DOI] [PubMed] [Google Scholar]
- [6].Goldstein LB, Adams R, Alberts MJ, et al. Primary prevention of ischemic stroke: a guideline from the American Heart Association/American Stroke Association Stroke Council: cosponsored by the Atherosclerotic Peripheral Vascular Disease Interdisciplinary Working Group; Cardiovascular Nursing Council; Clinical Cardiology Council; Nutrition, Physical Activity, and Metabolism Council; and the Quality of Care and Outcomes Research Interdisciplinary Working Group. Circulation 2006;113:e873–923. [DOI] [PubMed] [Google Scholar]
- [7].Ricotta JJ, Aburahma A, Ascher E, et al. Updated Society for Vascular Surgery guidelines for management of extracranial carotid disease. J Vasc Surg 2011;54:e1–31. [DOI] [PubMed] [Google Scholar]
- [8].Qureshi AI, Alexandrov AV, Tegeler CH, et al. Guidelines for screening of extracranial carotid artery disease: a statement for healthcare professionals from the multidisciplinary practice guidelines committee of the American Society of Neuroimaging; cosponsored by the Society of Vascular and Interventional Neurology. J Neuroimaging 2007;17:19–47. [DOI] [PubMed] [Google Scholar]
- [9].Yun WS, Rho YN, Park UJ, et al. Prevalence of asymptomatic critical carotid artery stenosis in Korean patients with chronic atherosclerotic lower extremity ischemia: is a screening carotid duplex ultrasonography worthwhile? J Korean Med Sci 2010;25:1167–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Roh YN, Woo SY, Kim N, et al. Prevalence of asymptomatic carotid stenosis in Korea based on health screening population. J Korean Med Sci 2011;26:1173–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Cho DK, Kim SW, Park JI, et al. Risk factors and predictors for the progression of carotid atherosclerotic stenosis in Korean adults. Korean Circ J 2005;35:834–40. [Google Scholar]
- [12].Lee KB, Kim DI, Cho JH, et al. Prevalence and risk factors of asymptomatic carotid stenosis in healthy Korean population. J Korean Surg Soc 2004;66:415–9. [Google Scholar]
- [13].Mannami T, Konishi M, Baba S, et al. Prevalence of asymptomatic carotid atherosclerotic lesions detected by high-resolution ultrasonography and its relation to cardiovascular risk factors in the general population of a Japanese city: the Suita study. Stroke 1997;28:518–25. [DOI] [PubMed] [Google Scholar]
- [14].Liang Y, Yan Z, Sun B, et al. Cardiovascular risk factor profiles for peripheral artery disease and carotid atherosclerosis among Chinese older people: a population-based study. PLoS One 2014;9:e85927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Grant EG, Benson CB, Moneta GL, et al. Carotid artery stenosis: gray-scale and Doppler US diagnosis—Society of Radiologists in Ultrasound Consensus Conference. Radiology 2003;229:340–6. [DOI] [PubMed] [Google Scholar]
- [16].Prati P, Vanuzzo D, Casaroli M, et al. Prevalence and determinants of carotid atherosclerosis in a general population. Stroke 1992;23:1705–11. [DOI] [PubMed] [Google Scholar]
- [17].Mathiesen EB, Joakimsen O, Bonaa KH. Prevalence of and risk factors associated with carotid artery stenosis: the Tromso Study. Cerebrovasc Dis 2001;12:44–51. [DOI] [PubMed] [Google Scholar]
- [18].De Weerd M, Greving JP, Hedblad B, et al. Prevalence of asymptomatic carotid artery stenosis in the general population: an individual participant data meta-analysis. Stroke 2010;41:1294–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Hogberg D, Kragsterman B, Bjorck M, et al. Carotid artery atherosclerosis among 65-year-old Swedish men—a population-based screening study. Eur J Vasc Endovasc Surg 2014;48:5–10. [DOI] [PubMed] [Google Scholar]
- [20].Rockman CB, Hoang H, Guo Y, et al. The prevalence of carotid artery stenosis varies significantly by race. J Vasc Surg 2013;57:327–37. [DOI] [PubMed] [Google Scholar]
- [21].Criqui MH, Vargas V, Denenberg JO, et al. Ethnicity and peripheral arterial disease: the San Diego Population Study. Circulation 2005;112:2703–7. [DOI] [PubMed] [Google Scholar]
- [22].de Weerd M, Greving JP, de Jong AW, et al. Prevalence of asymptomatic carotid artery stenosis according to age and sex: systematic review and metaregression analysis. Stroke 2009;40:1105–13. [DOI] [PubMed] [Google Scholar]
- [23].Sobieszczyk P, Beckman J. Carotid artery disease. Circulation 2006;114:e244–7. [DOI] [PubMed] [Google Scholar]
- [24].Tell GS, Polak JF, Ward BJ, et al. Relation of smoking with carotid artery wall thickness and stenosis in older adults. The Cardiovascular Health Study. The Cardiovascular Health Study (CHS) Collaborative Research Group. Circulation 1994;90:2905–8. [DOI] [PubMed] [Google Scholar]
- [25].U.S. Preventive Services Task Force Screening for carotid artery stenosis: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med 2007;147:854–9. [DOI] [PubMed] [Google Scholar]


