Highlights
-
•
Pancreatitis, panniculitis and polyarthritis syndrome is a very rare manifestation of pancreatitis with panniculitis and polyarthritis with intraosseous fat necrosis.
-
•
A rare differential diagnosis of unclear polyarthritis, panniculitis or osteonecrosis.
-
•
Surgical treatment, if possible can lead to complete remission.
Keywords: Pancreatitis, Arthritis, Fat tissue necrosis, Pancreatic pseudocyst, Lipase, Osteonecrosis
Abstract
Introduction
Pancreatitis, panniculitis and polyarthritis syndrome is a very rare extra-pancreatic complication of pancreatic diseases.
Presentation of case
While in most cases this syndrome is caused by acute or chronic pancreatitis, we report a case of a 62-year-old man presenting with extensive intraosseous fat necrosis, polyarthritis and panniculitis caused by a post-pancreatitis pseudocyst with a fistula to the superior mesenteric vein and extremely high blood levels of lipase. This became symptomatic 2.5 years after an episode of acute pancreatitis and as in most cases abdominal symptoms were absent. Treatment by surgical resection of the pancreatic head with the pseudocyst and mesenteric fistula led to complete remission of all symptoms.
Discussion
A review of the literature revealed that all publications are limited to case reports. Most authors hypothesize that an unspecific damage can cause a secretion of pancreatic enzymes to the bloodstream leading to a systemic lipolysis and fat tissue necrosis, especially of subcutaneous tissue, bone marrow, inducing panniculitis, polyarthritis and osteonecrosis. Even if caused by an acute pancreatitis abdominal symptoms are often mild or absent in most cases leading to misdiagnosis and poor prognosis.
Conclusion
While symptomatic treatment with NSAR and cortisone showed poor to moderate response, causal treatment can be successful depending on the underlying pancreatic disease.
1. Introduction
Pancreatitis, panniculitis and polyarthritis syndrome (PPP-syndrome) is a very rare symptom complex of extra pancreatic manifestations of pancreatitis with lobular panniculitis and (poly-) arthritis with intraosseous fat necrosis. Although the pancreatic pathology with exceptional high blood levels of pancreatic enzymes (in particular lipase) is widely considered causative, abdominal symptoms are often mild or absent. This leads to misdiagnosis, delay of appropriate therapy and worsening of prognosis [1]. Here we report a case of PPP-syndrome with extensive intraosseous fat necrosis in multiple bones and polyarthritis. Outstanding in this case was the extremely high blood level of up to 600-fold elevated lipase caused by a pancreatic pseudocyst with contact and fistula to the superior mesenteric vein. While in most cases acute or chronic pancreatitis were present at the onset of the PPP-syndrome, this patient became clinically apparent 2.5 years after an acute pancreatitis and was successfully treated by surgical resection of the pancreatic head with the pseudocyst and mesenteric fistula. Furthermore, we review the literature and summarize the characteristics of this syndrome. This report is in line with the SCARE guideline [2].
2. Case report
A 62-year-old Caucasian male with a history of alcohol abuse and acute pancreatitis 3 years ago, was admitted to University Hospital because of progressive, spreading joint and bone pain for 3–4 weeks. He reported that initially both cubital joints, then both ankle joints, finger joints and wrists on both hands were affected. The patient also mentioned a heavily painful and reddened swelling of his left wrist. Previously the patient was treated under the suspicion of reactive arthritis based on positive titer for chlamydia pneumoniae IgA and IgG and absent signs of a systemic rheumatologic disease with 20 mg/d prednisolone and antibiotics (doxycycline). In addition, there was a high level of lipase noticed, but in absence of signs of pancreatitis in clinical symptoms, computed tomography and ultrasound it was not related with the other symptoms. By this treatment, the elevated lipase levels and CRP-values were normalized, but joint pain was only partially reduced. After 2 weeks, the patient was readmitted with heavy pain in his left knee joint with distinct swelling and reddening. In minor extent, he suffered also from pain in the left shoulder, wrists, cubital and both ankle joints. He added that 9 months ago, he suffered from similar symptoms with multiple joint pain. The patient had a history of acute, necrotizing head-pancreatitis caused by heavy alcohol abuse 3 years ago, but now he clearly negated any abdominal symptoms and was plausibly abstinent of alcohol. A cystic lesion of the uncinate process of the pancreas with constant size was described in imaging for 3 years.
On physical examination, the left knee joint showed clear signs of inflammation with reddening, massive pressure pain and swelling. Abdominal status was inconspicuous. There were no signs of skin lesions typical for psoriasis, but “sausage toes” on the fifth left toe and third and fifth right toe were noticed.
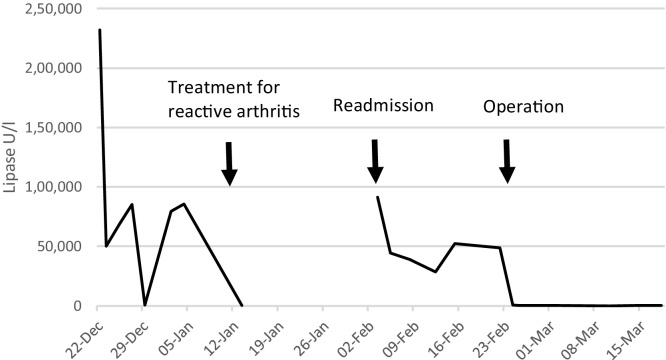
Laboratory tests showed extremely high levels of plasma lipase up to 232.000 U/l (normal: 73–383 U/l) and alpha-amylase up to 11920 U/l (normal: 25–115 U/l) (Fig. 1). C-reactive protein was 147 mg/l (normal: 0–5 mg/l). Further laboratory tests were negative for rheumatoid factor (RF), antibodies to citrullinated protein antigens (ACPAs), anti-neutrophil cytoplasmic antibodies (ANCAs), antinuclear antibodies (ANAs), immunoglobulin G1-4, complement factor C3/C4, protein electrophoresis, procalcitonin, differential blood count, LDH, ACE, sIL2, HIV and screening for hepatitis B and C. The puncture of a pretibial fluid accumulation revealed a sterile, bloody material.
Fig. 1.
Development of lipase levels. Normal: 73–393 U/l. Treatment for reactive arthritis was 20 mg prednisolone + doxycycline. Operation: Surgical resection of pancreatic pseudocyst.
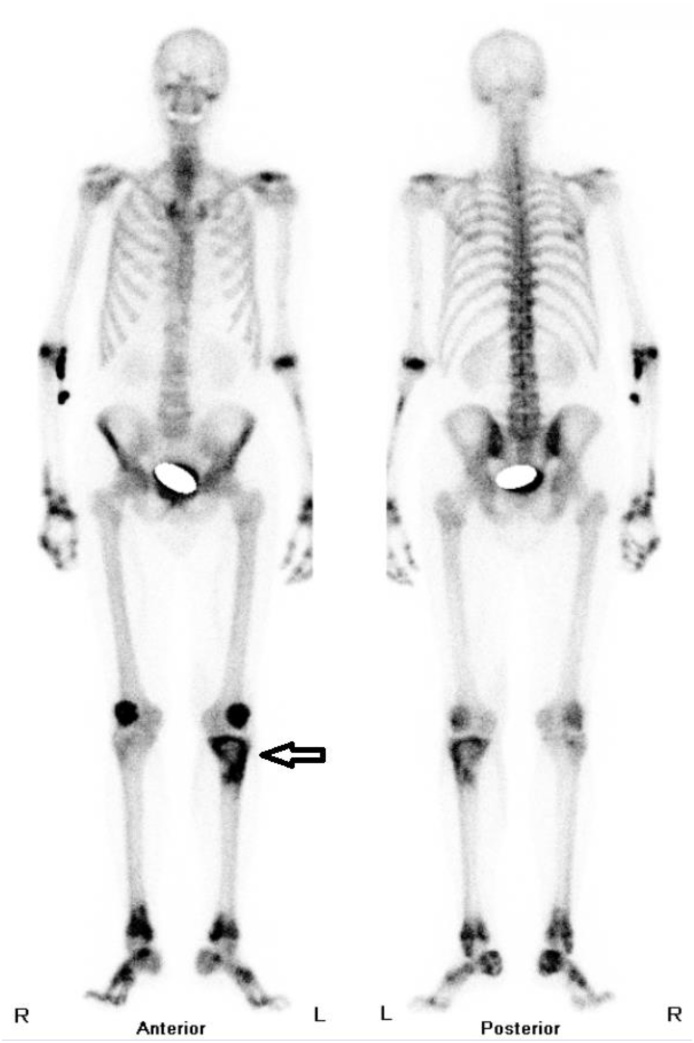
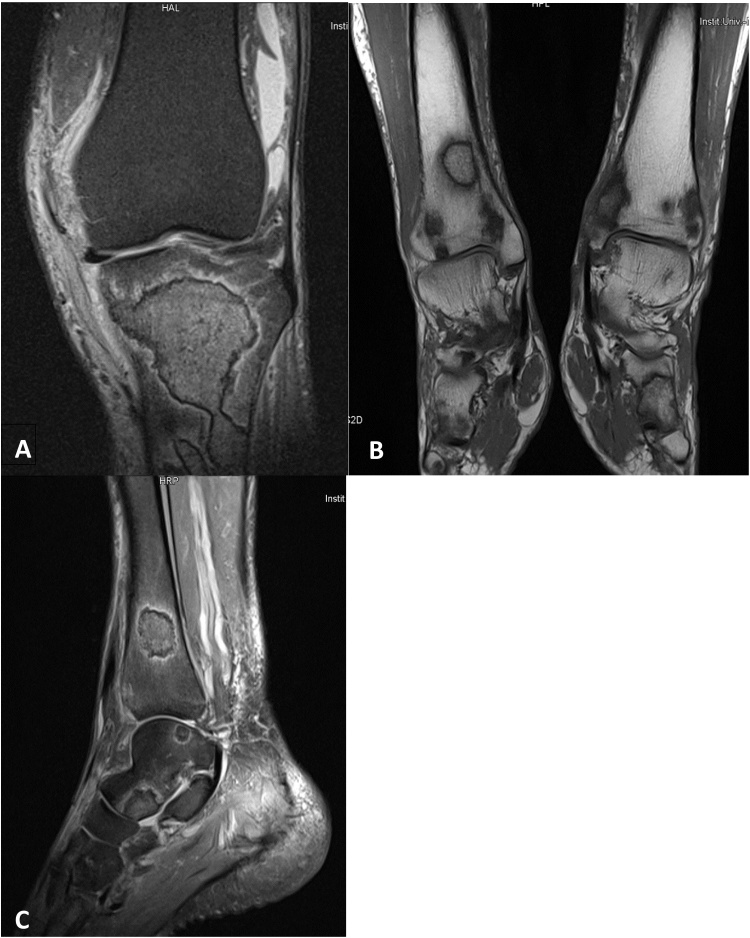
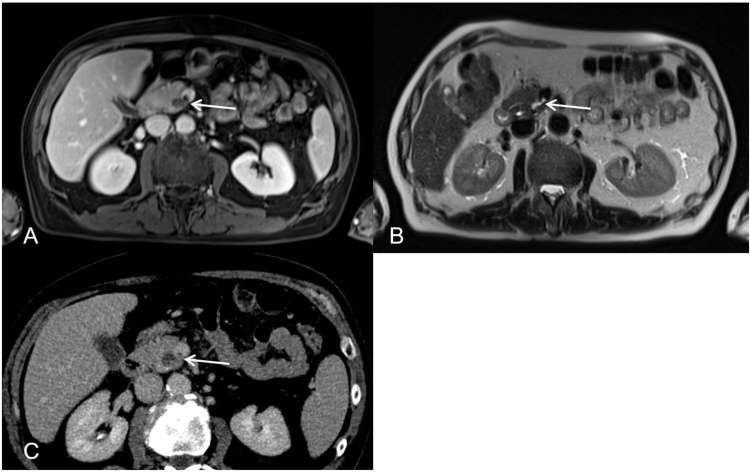
2-phase bone scintigraphy showed symmetric polyarthritis with pathological nuclide uptake of left proximal tibia, both patellae, cubital joints, wrists, ankle joints and metatarsus as well as calcaneus and all the interphalangeal joints of hands and feet. There was also a striking intense uptake in the clinically highly affected left proximal tibia with a central gap (mark in Fig. 2) which is not typical for arthritis. Magnetic resonance imaging revealed multiple necrotic bone lesions in proximal tibia and both patellae with circumscribed, garland-like T1-hypointense, T2-hyperintense lesions with marginal contrast agent uptake. Further examination showed similar lesions in both distal tibiae, calcaneus, talus and all tarsal bones (Fig. 3). In addition, there was an articular effusion in the left knee with contrast agent uptake of the synovia. A malignant process was excluded by CT-guided puncture. Histology showed unspecific bone necrosis consistent with fat tissue necrosis. Magnetic resonance and computed tomography of pancreas and biliary tract showed a cystic lesion in the pancreas head with a diameter of 1.3 cm and a partial thrombosis of the superior mesenteric vein adjacent to the cyst (Fig. 4).
Fig. 2.
2-phase bone scintigraphy (late phase). Symmetric polyarthritis of the extremity skeleton, but atypical intense uptake in the left proximal tibia (arrow).
Fig. 3.
MR-Imaging of knee and ankles demonstrated multiple ‘infarct like’ bone necrosis near joints of prox. and distal tibia, calcaneus, talus and all tarsal bones. Diffuse contrast agent uptake of surrounding soft tissue.
Fig. 4.
Abdominal MRI (A, B) depicted a pseudocyst of the uncinate process of the pancreas. The cystic lesion shows a direct connection to the superior mesenteric vein on the contrast enhanced T1 weighted images (A) as well as on the T2 weighted images (B) (arrow in A and B). The connection between the cyst and the superior mesenteric vein was also detectable on a contrast enhanced CT study which was performed one week prior to the MRI examination.
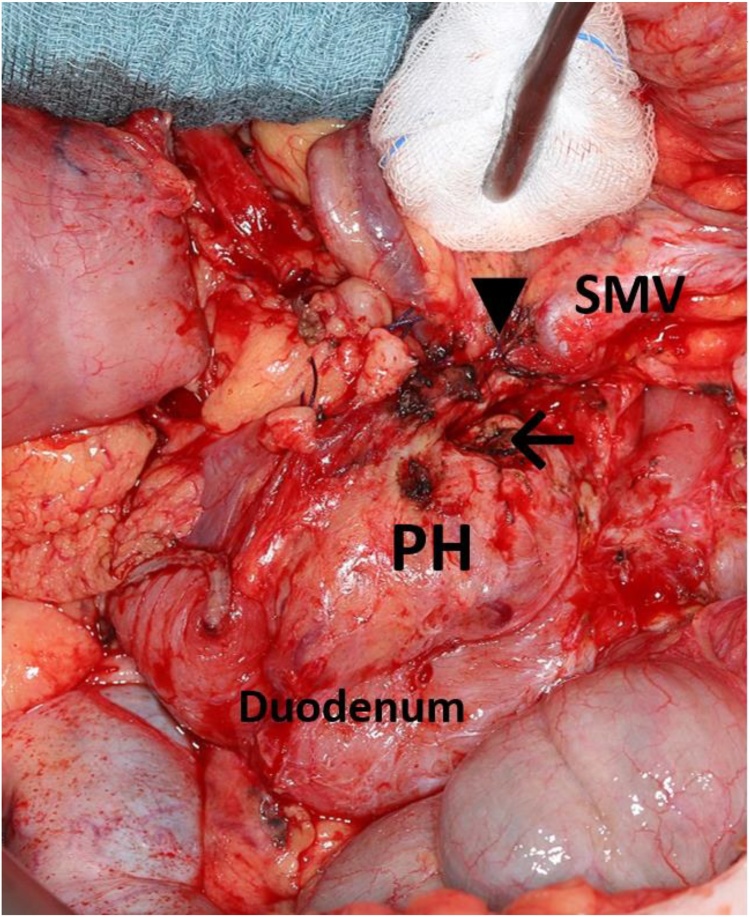
Diagnosis of pancreatitis, panniculitis and polyarthritis syndrome due to a post pancreatitis pseudocyst with pseudocysto-mesenteric fistula was made. On surgical exploration, the pancreas presented with heavy post-inflammatory alterations of the uncinate process with a pseudocyst adjacent to the superior mesenteric vein (Fig. 5). We performed a pylorus-preserving partial pancreaticoduodenectomy with resection of the mesenteric fistula, removal of the mesenteric thrombus and reconstruction of the vein by direct suture. Postoperative plasma levels of lipase dropped immediately and permanently to normal levels, which confirmed the diagnosis (Fig. 1). In the further course no more signs of inflammation or active disease were detectable, but the patient still suffered from pain and mobility restriction due to the distinct bone necrosis for some weeks. Afterwards he was completely free of symptoms. Follow-up computed tomography of tibia head showed bone densification, but no osteolysis or fractures.
Fig. 5.
Operative findings showed the opened pseudocyst of the uncinated process (arrow) close to the superior mesenteric vein (SMV). ▼marks the altered segment of SMV with thrombosis. PH = pancreatic head.
3. Literature review and discussion
Pancreatic panniculitis can occur in 2–3 % of patients with pancreatitis, first described by Chiari in 1883 [3], [4]. Much rarer the triad of pancreatitis, subcutaneous tissue inflammation (panniculitis) and polyarthritis, often referred to as “Pancreatitis-Panniculitis-Polyarthritis-Syndrome” or “PPP-syndrome” could be observed. In addition to our case we found 32 well-documented cases in current literature [1], [5], [6], [7], [8], [9], [10], [11]. Reports are limited to case-reports and speculations about pathogenesis. The pathogenesis is unknown, but most authors consider that direct secretion of pancreatic enzymes to the bloodstream causes systemic fat necrosis especially in subcutaneous fat tissue, bones and joints [10]. In all cases an exceptional high level of lipase was found though other pancreatic enzymes such as amylase, phosphorylase and trypsin may play a role [3]. Notably, in all cases lipase was considerably elevated, but in two amylase was not [11], [12], [13]. Additionally elevated amylase alone cannot cause panniculitis [11]. Also while the level of lipase does not indicate the severity of acute pancreatitis, it seems to correspond with the extent of extra pancreatic fat tissue necrosis in PPP-syndrome [1], [14], [15]. Some authors hypothesize that arthritis is caused by free fatty acids that are released into the joint, after the lipolytic pancreatic enzymes have hydrolyzed triglycerides in the joint near bone marrow [1], [16].
PPP-syndrome can occur at any age (range: 6–88), although the typical patient is a middle-aged male with a history of heavy alcohol abuse (past or present) [1], [7], [11], [17]. It can precede (1/3), coincide or succeed the pancreatic disease [1]. In all cases the authors saw an underlying pancreatic pathology as the main etiological factor, which can be acute or chronic pancreatitis, pancreatic carcinoma, neuroendocrine carcinoma, insulinoma, ischemic pancreatic disease, abdominal trauma or pancreatic duct stenosis [5], [6], [7], [11], [18], [19], [20], [21]. Some authors described the presence of a pseudocyst, others detected a fistula between the pseudocyst and the superior mesenteric vein [8]. While the usually tiny fistulas are difficult to visualize in preoperative imaging, presence of mesenteric vein thrombosis can be an indirect sign and should always lead to surgical exploration. It is important to emphasize that in most cases abdominal symptoms were mild or absent, despite high levels of lipase [1].
The panniculitis presents with sometimes painful, erythematous red-brown nodules (0.5–5 cm), which are typically located on the lower extremities, but can spread to the entire body if the disease progresses. The cutaneous manifestation can precede the pancreatic disease several weeks [12]. Spontaneous rupture of the skin lesions can occur and secretion of a sterile “oily, brown, viscous” material is described [7], [11]. In the beginning these lesions can be confounded with erythema nodosum, vasculitic lesions, sweet-syndrome, a1-antitrypsin deficiency or infection [11]. Histology usually shows lobular panniculitis without vasculitis and a surrounding inflammation. A pathognomonic finding are “ghost-adipocytes”, which have lost their nuclei and have thick shadowy walls due to coagulative necrosis by pancreatic enzymes [7], [11], [22].
Arthritis is much rarer and can occur as severe monoarthritis, but more often as symmetric polyarthritis of the ankle, knees, wrists, metacarpal joints, elbows and tarsal joints, following the distribution of the cutaneous manifestations. Analysis of synovial liquid usually shows a sterile, thick, yellow material with high count of neutrophil leukocytes [1], [6], [22], while unspecific signs of chronic inflammation can be found in biopsy of synovia [9]. Other manifestations of PPP-syndrome include chondronecrosis, necrosis of intramedullary bones and gastrointestinal submucosa [10], [23]. Like in polyarthritis the lower distal extremity is affected more often. Common localizations are distal and proximal ends of the long bones and small bones of hand and feet such as tibia, fibula, calcaneus, talus, malleolus, distal radius, scaphoid and carpal bones [1], [5], [6], [8], [10]. If the disease progresses pathological fractures can occur [5]. MR imaging is the method of choice to show intramedullary fat necrosis, bone marrow edema, synovitis and surrounding inflammation of periarticular soft tissue, while computed tomography is best for detecting secondary bone damage.
Causative treatment depends on the underlying pancreatic disease and involves handling of acute or chronic pancreatitis, pancreatic duct stenosis, EUS-guided cyst-gastrostomy and surgical resection of pseudocysts [1], [6], [7], [9], [22], [24]. Of particular relevance are the surgical dissection or even segmental resection and reconstruction of the mesenteric or portal veins in order to reliably remove the fistula, which drains the pancreatic juice into the portal blood stream. As shown in this case the right treatment if possible can lead to remission, but in most cases, as in our case too, the pancreatic disease was misdiagnosed in the beginning leading to a delay in treatment and high mortality especially among patients with pancreatitis or carcinomas [1]. Francombe et al. [22] used plasmapheresis in addition to intensive care and operative treatment of severe pancreatitis with persistent elevated amylase levels. They also showed an effective reduction of amylase level, however the patient died before the effect on PPP-syndrome could be evaluated [22]. Panniculitis and polyarthritis are usually treated with NSAID and corticosteroids. Although we have seen some temporary effect on arthritis and bone pain in this case most reports describe poor to moderate response. There is no evidence that NSAID and corticosteroids can improve prognosis and they are considered as a purely symptomatic therapy [1], [5], [6], [10], [11]. Attempts with octreotide (somatostatin analogue) showed response in one case of pancreatic carcinoma, but did not in 4 others [11], [25].
In the review of Narváez et al., 24% patients died due to complications of pancreatitis or metastatic carcinomas. In about half the patients who recovered from pancreatic disease peripheral joint and skin lesions healed without sequelae while the rest developed chronic arthritis which was independent of the pancreatic disease and sustained even after pancreatic enzymes were normalized. Secondly intraosseous fat necrosis can lead to consequential bone damage with fragmentation and subsequent subarticular bone collapse [1].
In conclusion, we present a rare case of PPP-syndrome with extremely high levels of lipase up to 600-fold of normal levels and osteonecrosis as the predominant clinical symptom accompanied by polyarthritis and only minimal signs of panniculitis. Causative was a fistula between a post-pancreatic pseudocyst and the superior mesenteric vein, which became clinically apparent 2.5 years after acute pancreatitis. A key learning point is the high value of mesenteric vein thrombosis as an indirect radiological sign of tiny fistulas. This case supports the hypothesis that an unspecific damage of pancreas tissue can lead to a direct release of lipase to the bloodstream and subsequent systemic extra pancreatic fat tissue necrosis as the important pathogenic step of this syndrome. A PPP-syndrome has to be taken into consideration if the origin of any osteonecrosis, polyarthritis or panniculitis remains unclear, considering the high morbidity and mortality. Absent abdominal symptoms can delay the diagnosis of the underlying pancreatic disease [7], [9]. Measuring of lipase, skin or bone biopsies, which show pathognomonic features, and if appropriate surgical exploration are the most important diagnostic procedures. Depending on the kind of the underlying pancreatic disease correct treatment can be successful and lead to complete remission.
Conflicts of interest
None (all authors).
Funding
None (all authors).
Ethical approval
Ethics board approval was not required in accordance with our institution policy.
Consent
The patients consent was obtained to publish the information and pictures of this case report.
Author contribution
WD diagnosed the syndrome and did the research for this case report and review. JD did the follow up examination and further treatment of the patient. TH analysed the CT and MR images. AS was involved as senior gastroenterologist in decision-making for the best treatment. FR and TW were involved in decision-making for the best treatment and did the surgical treatment, BK was senior physician and diagnosed the syndrom and treated the patient. All authors read and approved the final manuscript.
Registration of research studies
None.
Guarantor
Wulf Dieker.
Bernd Krüger.
Contributor Information
Wulf Dieker, Email: wulf.dieker@umm.de.
Johannes Derer, Email: Johannes.Derer@umm.de.
Thomas Henzler, Email: Thomas.Henzler@umm.de.
Alexander Schneider, Email: Alexander.Schneider@umm.de.
Felix Rückert, Email: Felix.Rueckert@umm.de.
Torsten J. Wilhelm, Email: Torsten.Wilhelm@umm.de.
Bernd Krüger, Email: Bernd.Krueger@umm.de.
References
- 1.Narvaez J., Bianchi M.M., Santo P., de la Fuente D., Rios-Rodriguez V., Bolao F. Pancreatitis, panniculitis, and polyarthritis. Semin. Arthritis Rheum. 2010;39:417–423. doi: 10.1016/j.semarthrit.2008.10.001. [DOI] [PubMed] [Google Scholar]
- 2.Agha R.A., Fowler A.J., Saeta A., Barai I., Rajmohan S., Orgill D.P. The SCARE statement: consensus-based surgical case report guidelines. Int. J. Surg. 2016;34:180–186. doi: 10.1016/j.ijsu.2016.08.014. [DOI] [PubMed] [Google Scholar]
- 3.Laureano A., Mestre T., Ricardo L., Rodrigues A.M., Cardoso J. Pancreatic panniculitis – a cutaneous manifestation of acute pancreatitis. J. Dermatol. Case Rep. 2014;8:35–37. doi: 10.3315/jdcr.2014.1167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chiari H. Über die sogenannte fettnekrose. Prag. Med. Wochenschr. 1883;8:255–256. [Google Scholar]
- 5.Azar L., Chatterjee S., Schils J. Pancreatitis, polyarthritis and panniculitis syndrome. Joint Bone Spine revue du rhumatisme. 2014;81:184. doi: 10.1016/j.jbspin.2013.08.003. [DOI] [PubMed] [Google Scholar]
- 6.Fraisse T., Boutet O., Tron A.M., Prieur E. Pancreatitis, panniculitis, polyarthritis syndrome: an unusual cause of destructive polyarthritis. Joint Bone Spine revue du rhumatisme. 2010;77:617–618. doi: 10.1016/j.jbspin.2010.05.005. [DOI] [PubMed] [Google Scholar]
- 7.Harris M.D., Bucobo J.C., Buscaglia J.M. Pancreatitis, panniculitis, polyarthritis syndrome successfully treated with EUS-guided cyst-gastrostomy. Gastrointest. Endosc. 2010;72:456–458. doi: 10.1016/j.gie.2009.11.040. [DOI] [PubMed] [Google Scholar]
- 8.Kuwatani M., Kawakami H., Yamada Y. Osteonecrosis and panniculitis as life-threatening signs. Clin. Gastroenterol. Hepatol. 2010;8:e52–53. doi: 10.1016/j.cgh.2009.12.026. [DOI] [PubMed] [Google Scholar]
- 9.Menon P., Kulshreshta R. Pancreatitis with panniculitis and arthritis: a rare association. Pediatr. Surg. Int. 2004;20:161–162. doi: 10.1007/s00383-003-1041-2. [DOI] [PubMed] [Google Scholar]
- 10.Mustafa K.N., Hadidy A., Shoumaf M., Razzuki S.A. Polyarthritis with chondronecrosis associated with osteonecrosis, panniculitis and pancreatitis. Rheumatol. Int. 2010;30:1239–1242. doi: 10.1007/s00296-009-1046-9. [DOI] [PubMed] [Google Scholar]
- 11.Preiss J.C., Faiss S., Loddenkemper C., Zeitz M., Duchmann R. Pancreatic panniculitis in an 88-year-old man with neuroendocrine carcinoma. Digestion. 2002;66:193–196. doi: 10.1159/000066758. [DOI] [PubMed] [Google Scholar]
- 12.Durden F.M., Variyam E., Chren M.M. Fat necrosis with features of erythema nodosum in a patient with metastatic pancreatic carcinoma. Int. J. Dermatol. 1996;35:39–41. doi: 10.1111/j.1365-4362.1996.tb01614.x. [DOI] [PubMed] [Google Scholar]
- 13.Feuer J., Spiera H., Phelps R.G., Shim H. Panniculitis of pancreatic disease masquerading as systemic lupus erythematosus panniculitis. J. Rheumatol. 1995;22:2170–2172. [PubMed] [Google Scholar]
- 14.Price-Forbes A.N., Filer A., Udeshi U.L., Rai A. Progression of imaging in pancreatitis panniculitis polyarthritis (PPP) syndrome. Scand. J. Rheumatol. 2006;35:72–74. doi: 10.1080/03009740500228073. [DOI] [PubMed] [Google Scholar]
- 15.Simkin P.A., Brunzell J.D., Wisner D., Fiechtner J.J., Carlin J.S., Willkens R.F. Free fatty acids in the pancreatitic arthritis syndrome. Arthritis Rheum. 1983;26:127–132. doi: 10.1002/art.1780260202. [DOI] [PubMed] [Google Scholar]
- 16.Ferrari R., Wendelboe M., Ford P.M., Corbett W.E., Anastassiades T.P. Pancreatitis arthritis with periarticular fat necrosis. J. Rheumatol. 1993;20:1436–1437. [PubMed] [Google Scholar]
- 17.Loverdos I., Swan M.C., Shekherdimian S., Al-Rasheed A.A., Schneider R., Fish J.S. A case of pancreatitis, panniculitis and polyarthritis syndrome: elucidating the pathophysiologic mechanisms of a rare condition. J. Pediatr. Surg. Case Rep. 2015;3:223–226. doi: 10.1016/j.epsc.2015.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Radin D.R., Colletti P.M., Forrester D.M., Tang W.W. Pancreatic acinar cell carcinoma with subcutaneous and intraosseous fat necrosis. Radiology. 1986;158:67–68. doi: 10.1148/radiology.158.1.3940400. [DOI] [PubMed] [Google Scholar]
- 19.Schwartz R.A., Fleishman J.S. Association of insulinoma with subcutaneous nodular fat necrosis. J. Surg. Oncol. 1981;16:305–311. doi: 10.1002/jso.2930160402. [DOI] [PubMed] [Google Scholar]
- 20.Smukler N.M., Schumacher H.R., Pascual E., Brown S., Ryan W.E., Sadeghian M.R. Synovial fat necrosis associated with ischemic pancreatic disease. Arthritis Rheum. 1979;22:547–553. doi: 10.1002/art.1780220517. [DOI] [PubMed] [Google Scholar]
- 21.Tannenbaum H., Anderson L.G., Schur P.H. Association of polyarthritis, subcutaneous nodules, and pancreatic disease. J. Rheumatol. 1975;2:15–20. [PubMed] [Google Scholar]
- 22.Francombe J., Kingsnorth A.N., Tunn E. Panniculitis, arthritis and pancreatitis. Br. J. Rheumatol. 1995;34:680–683. doi: 10.1093/rheumatology/34.7.680. [DOI] [PubMed] [Google Scholar]
- 23.Dahl P.R., Su W.P., Cullimore K.C., Dicken C.H. Pancreatic panniculitis. J. Am. Acad. Dermatol. 1995;33:413–417. doi: 10.1016/0190-9622(95)91385-8. [DOI] [PubMed] [Google Scholar]
- 24.Jose T., Biju I.K., Kumar A., Anver P.C., Kuruvila R., Kuruvila S. ‘Pancreatitis, polyarthritis, panniculitis syndrome’ (PPP syndrome) plus prolonged pyrexia-a rare presentation of chronic pancreatitis. Indian J. Gastroenterol. 2009;28:186–188. doi: 10.1007/s12664-009-0072-6. [DOI] [PubMed] [Google Scholar]
- 25.Hudson-Peacock M.J., Regnard C.F., Farr P.M. Liquefying panniculitis associated with acinous carcinoma of the pancreas responding to octreotide. J. R. Soc. Med. 1994;87:361–362. doi: 10.1177/014107689408700620. [DOI] [PMC free article] [PubMed] [Google Scholar]