Abstract
Considerable research exists documenting the relationship between maternal mood disorders, primarily major depressive disorder (MDD), and a variety of negative child outcomes. By contrast, research exploring the reverse pathway whereby child traits are associated with later maternal mood disorders is much more limited. We examined whether young children’s temperament and psychopathology predicted maternal mood disorders approximately 6 years later. Child temperament and symptoms were assessed at age three using semi-structured diagnostic interviews and parent-report inventories. Maternal psychopathology was assessed with semi-structured interviews when children were three and nine years old. Mothers also reported on their marital satisfaction when children were three and six years old. Child temperamental negative affectivity (NA), depressive symptoms, and externalizing behavior problems significantly predicted maternal mood disorders over and above prior maternal mood, anxiety, and substance disorders. The link between children’s early externalizing symptoms and maternal mood disorders 6 years later was mediated by maternal marital satisfaction 3 years after the initial assessment. These findings suggest that early child temperament and psychopathology contribute to risk for later maternal mood disorders both directly and through their impact on the marital system. Research indicates that effective treatment of maternal depression is associated with positive outcomes for children; however, this study suggests that treating early child problems may mitigate the risk of later maternal psychopathology.
Keywords: Maternal depression, child psychopathology, temperament, maternal mood disorders, risk
Mood disorders represent a serious mental health concern for Americans. Over the course of their lifetimes, approximately 22.9% of women and 13.1% of men suffer from depression in the United States (Eaton et al., 2012). Women with young children are particularly susceptible to mood disorders, and are an important target for research and intervention (Hammen, 2003; Kessler et al., 2003).
A large body of research demonstrates that maternal mood disorders are associated with a wide range of negative child outcomes (Gotlib & Colich, 2014; Lewinsohn, Olino, & Klein, 2005). According to a meta-analysis of 193 studies, maternal depression was significantly related to increased internalizing and externalizing behaviors, general psychopathology, negative affectivity (NA), and decreased positive affectivity (PA) in offspring (Goodman et al., 2011). While the impact of maternal mood disorders on children is well-established, it is probable that the relationship is bi-directional, with child emotional and behavioral problems also influencing mothers’ mental health. However, research exploring the impact of child characteristics on subsequent maternal mood disorders is limited, and much of this work focuses on children with pervasive developmental disorders (Fombonne, Simmons, Ford, Meltzer, Goodman, 2003; Ghodsian, Zajicek, & Wolkind, 1984; Hastings, 2002; Herring et al. 2006; Rao & Beidel, 2009).
A few studies have reported that child externalizing behaviors or breadth of child psychopathology predict subsequent maternal depression. For example, in two studies using cross-lagged panel analyses, Shaw, Gross, and Moilanen (2009) reported that conduct problems in 2–10 year old children, and antisocial behavior in 10–15 year old youth, predicted mothers’ subsequent depressive symptoms. However, these effects were observed for only a minority of the lagged paths. Choe, Sameroff, and McDonough (2013) found that externalizing behavior in 15-month old children predicted mothers’ depressive symptoms 18 months later, but only among the subgroup of children who were poorly regulated at 7 months of age. In another sample, Choe Shaw, Brennan, Dishion, and Wilson (2014) reported that children’s oppositional behavior at age 2 predicted maternal depressive symptoms 1 and 3 years later. Finally, Raposa, Hammen, and Brennan (2011) found that a greater number of youth diagnoses by age 15 conferred increased risk for concurrent and future maternal depressive disorders and number of episodes of maternal depression five years later.
High or low levels of some child temperament traits can also pose significant challenges for parents (Putnam, Sanson, & Rothbart, 2002). Moreover, many investigators view temperament and symptoms as lying on a continuum (Klein, Dyson, Kujawa, & Kotov, 2012). Hence, it is reasonable to hypothesize that child temperament might also predict later maternal depression. However, to our knowledge, this has not been previously examined. Most models of the structure of temperament include concepts related to negative affectivity (NA), surgency, and effortful control (De Pauw & Mervielde, 2010; Rothbart, Ahadi, Hershey, & Fisher, 2001). NA reflects a propensity to experience anger, frustration, sadness, and fear, and is characteristic of both internalizing and externalizing psychopathology (Klein et al., 2012; Laceulle, Ormel, Vollebergh, Aken, & Nederhof, 2014). Surgency is related to high approach, activity, stimulus-seeking, and impulsivity, and is often associated with externalizing psychopathology (Berdan, Keane, & Calkins, 2008; Tackett, Martel, & Kushner, 2012). Low effortful control reflects difficulty in focusing attention and inhibiting prepotent responses, and has been associated with externalizing, and less consistently with internalizing, behavior problems (Eisenberg et al., 2000; Murray & Kochanska, 2002; Laceulle et al., 2014).
There are a number of possible mechanisms by which child symptoms and/or traits could impact later maternal mood disorders. The marital relationship has been proposed as one such mediator of the association of child symptoms and traits with maternal mental health (Befera & Barkley, 1985). This is supported by evidence that the quality of the marital relationship is affected by child behavior (Cui, Donnellan, & Conger, 2007; Johnson & Lobitz, 1974), and that marital problems are a well-established risk factor for depression (Beach & O’Leary, 1993; Whisman, 2013). Thus, it is plausible that at least part of the impact of child symptoms and traits on maternal depression occurs via their effects on the marital relationship.
The Current Study
In this study, we examined the relationship of pre-school aged children’s temperament and symptoms of psychopathology with maternal mood disorder diagnoses 6 years later. We focused on the preschool period because children are still very dependent on their caretakers, and mothers often spend more time with their children prior to the start of formal schooling. Hence, this might amplify the effects of child characteristics on maternal risk. As it is not known what symptom thresholds for early child psychopathology impact mothers, we employed dimensional measures of preschool psychopathology. However, to maximize the clinical and public health relevance of the findings, we focused on clinically significant (i.e., meeting diagnostic criteria) episodes of mood disorder in mothers. We also examined the effects of child temperament on mothers. Finally, to minimize the effects of informant biases and method variance, we used multiple measurement approaches (interviews and self-report questionnaires) and multiple informants (mothers and fathers).
Our primary analyses focused on broad symptom and trait dimensions followed by examining disorder-specific symptoms. We hypothesized that both child internalizing and externalizing symptoms would predict maternal mood disorders 6 years later. At a more specific level, we also expected depression, anxiety, attention deficit hyperactivity disorder (ADHD), and oppositional defiant disorder (ODD) symptoms to predict maternal mood disorders. Finally, we hypothesized that high temperamental NA, high surgency, and low effortful control in children would predict later maternal mood disorders. In these analyses, we included maternal anxiety and substance use disorders as covariates because they often precede, and may contribute to, depression (Mineka, Anand, & Sumner, 2014; Najavits, & Capezza, 2014). This is a conservative approach that should work against our hypotheses. Our second set of analyses tested whether mothers’ marital satisfaction mediates the relationship between child symptoms and traits and later maternal mood disorders.
Method
Participants
The sample consisted of 441 families with a 3-year old child (53.7% male) who completed a baseline assessment and a follow-up assessment 6 years later. Of these families, 362 also completed an interim follow-up 3 years after the initial evaluation. Mothers and children included in this report did not differ from the non-participants on any variables relevant to this study. Families were recruited through commercial mailing lists; those eligible for participation included at least one English-speaking biological parent and a 3-year old child with no significant medical conditions or developmental disabilities. The children were predominantly Caucasian (87.5%), most of the parents were married (88.8% at the initial assessment). About half the parents had graduated from college (55.5% of mothers and 47.6% of fathers). Written informed consent was obtained from all the families following a detailed description of the study. Child assent was also obtained. The families were financially compensated for their participation.
Child Temperament and Psychopathology
In the initial assessment when children were 3 years old, parents completed the Child Behavior Checklist (CBCL; Achenbach, 1991), which assesses internalizing and externalizing behaviors in children (αs = .84 and .90 respectively). Mother and father reports were moderately correlated (r = .38 for internalizing and r = .48 for externalizing). These variables were z-scored and averaged to create composite scores for both parents. If data were available for only one parent, that parent’s ratings were used. An average of the variables was used instead of creating latent variables as latent variables with two indicators with correlated error variances typically result in poor model identification (Bollen & Davis, 2009; Kenny, Kashy, & Bolger, 1998). CBCLs were completed by both parents for 336 children; only mothers’ and only fathers’ reports were available for 99 and 4 children, respectively. There were 439 families with CBCL data.
The Preschool Age Psychiatric Assessment (PAPA; Egger et al., 2006) is a parent-report structured diagnostic interview that assesses Diagnostic and Statistical Manual, 4th edition (American Psychiatric Association, 1994) disorders in preschool-aged children. Data for the PAPA were provided by the primary parent for 441 children. The PAPA uses a structured format and an interviewer-based approach. The interviewer asks all required questions, but also confirms the parent’s understanding of the question, elicits examples, and adheres to guidelines for rating all items. Symptoms are assessed for the three months prior to the interview to maximize recall. For this study, we summed the ratings for anxiety, depression, ADHD, and ODD symptoms to create dimensional scores (αs = .83, .72, .89, and .84, respectively).
Interviews were conducted by advanced graduate students in clinical psychology who received training from a member of the PAPA development team. Interviews were conducted by telephone and generally lasted 1–2 hours. Diagnostic interviews with parents regarding their children have yielded equivalent results when administered by telephone and face-to-face (Lyneham & Rapee, 2005). To examine interrater reliability, a second rater independently rated audiotapes of 21 PAPA interviews. Interrater reliability for anxiety, depression, ADHD, and ODD scores was excellent (intraclass correlations ranged from .98 – 1.00).
To reduce administration time, for the first 60% of the sample the interviewer used the Early Childhood Inventory – 4 (ECI-4) ADHD and ODD scales as a screen to help determine whether to complete the ADHD and ODD sections of the PAPA. The interviewer also confirmed the absence of the key ADHD and ODD symptoms with the parent. If the screener and these queries indicated the child did not show any evidence of ADHD or ODD, then the section(s) was skipped. In the remaining 40% of the sample, the full PAPA ADHD and ODD sections were administered to all caregivers. To account for the missing PAPA values for the 60% of the sample who were administered the ECI-4 as a screener, Full Information Maximum Likelihood (FIML) procedures were used in MPlus 6.0 for all analyses. This approach to missing data is generally acknowledged to be preferable to other methods for dealing with missing data, such as listwise deletion or single imputation, as these latter approaches are more likely to yield severely biased estimates, whereas estimates based on FIML are less biased relative to these other procedures (Little & Rubin, 1989; Muthen, Kaplan, & Hollis, 1987; Schafer, 1997).
The ECI-4 is a parent rating scale used to screen for DSM-IV emotional and behavioral disorders in 3- to 6-year old children (Gadow & Sprafkin, 2000). Parents completed the ADHD and ODD sections of the inventory. The overall correct classification rates for ADHD and ODD with respect to chart diagnoses were 60% and 74%, respectively (Sprafkin, Volpe, Gadow, Nolan, & Kelly, 2002). In the present sample, coefficient alphas for the ECI-4 were .79 (ADHD-Inattention), .82 (ADHD-Hyperactivity/Impulsivity), and .85 (ODD).
Parents also completed the Child Behavior Questionnaire (CBQ; Rothbart et al., 2001), a widely used caregiver report measure of temperament for 3- to 7-year-old children. The CBQ includes 195 items that are rated on a 1–7 scale (extremely untrue – extremely true). For this study, the three CBQ higher order factors, NA, surgency, and effortful control, were used, with alphas of .72, .78, and .71 respectively. Agreement between mother and father reports of NA, surgency, and effortful control were r = .47, .68, and .55 respectively. Mother’s and father’s reports for these variable were z-scored and averaged to create a composite score. The CBQ was completed by both parents for 330 children; data were available from only the mother and only the father for 90 and 7 children, respectively.
Maternal Psychopathology
The Structured Clinical Interview for DSM-IV (SCID; First, Spitzer, Gibbon, & Williams 1996) is a semi-structured diagnostic interview that was used to assess maternal mood, anxiety, and substance disorders at the initial wave, when children were 3. It was re-administered at follow-up six years later to assess mood disorders. SCID data at both time points were available for all 441 mothers included in this report. The SCID is among the most widely used diagnostic interviews, and its interrater reliability and procedural validity have been well documented (Williams et al., 1992). The diagnostic interviews were conducted by masters-level clinicians and advanced graduate students by telephone at the initial assessment and in-person at the third wave. Telephone and face-to-face diagnostic interviews have been shown to yield equivalent results (Rohde, Lewinsohn, & Seeley, 1997). The interviewers were not involved in collecting, and did not have access to, any of the data on the children. We found good interrater reliability when diagnosing lifetime mood disorders at both the initial assessment (Kappa = .93; N = 30), and the six-year follow up (Kappa = .91; N = 74).
Mothers’ Marital satisfaction
The Abbreviated Dyadic Adjustment Scale (ADAS; Sabourin, Valois, & Lissier, 2005) is a 7-item self-report scale measuring marital satisfaction (α = .86) that is comparable to the original 32-item DAS in its ability to predict couple dissolution (Sabourin, Valois, & Lussier, 2005). Mothers completed the questionnaire at the initial assessment and at the three-year follow-up, when children were age 6. 338 mothers completed the ADAS at age 3 and 369 mothers completed the ADAS at age 6.
Procedure
To summarize, the CBCL, PAPA/ECI-4, CBQ, SCID, and ADAS were completed at time point 1 when children were 3 years old. At time 2, three years later, the ADAS was given, and finally, at time 3, when children were age 9, the SCID was re-administered.
Data analyses
Effects of child behavior on maternal mood disorders
Simultaneous logistic regression models were computed using MPlus 6.0 to examine the influence of child temperament and psychopathology at age 3 on maternal mood disorders 6 years later. Maternal history of mood disorders before the initial assessment was entered to control for prior maternal mood disorders. Similarly, maternal anxiety and substance disorders prior to the initial assessment were also entered to control for other disorders that might predispose to later mood disorders. Three models were tested, one each for the 2 CBCL variables, the 4 PAPA variables, and the 3 CBQ variables.
Marital satisfaction as a mediator
Mediation models were tested using cross-lagged path models. By controlling for the effect of time 1 scores (e.g., child externalizing symptoms at age 3) on time 2 scores of the same variable, predictors of that time 2 score are then predicting the residual, or change, in that score from time 1 to time 2. We tested path models only for child symptom and trait variables that predicted maternal mood disorders in the logistic regression analyses.
Mediational analyses were also conducted using MPlus version 6.0. Boostrapping was used to determine confidence intervals around indirect effects. In the current study, we computed a 95% confidence interval with 10,000 draws. Fit indices are not available for mediational models involving categorical outcomes when bootstrapping is used. Instead, we report fit indices without using a bootstrap, whereas effects (i.e., main and indirect regression effects) are bootstrapped. As measures of goodness of fit, we present chi-square, ratio of chi-square to degrees of freedom, comparative fit index (CFI), and root-mean-square error of approximation (RMSEA). As a measure of comparative fit, we used the DIFFTEST option in MPlus, which computes a chi-square test for comparing nested models. Generally, CFI values greater than .90 (Hoyle & Panter, 1995), a χ2/df less than 2 (Carmines & McIver, 1981), and an RMSEA less than .08 (Kline, 1998) indicate acceptable fit. When testing mediational models with a categorical outcome, MPlus uses a Weighted Least Squares estimator, which computes probit regression coefficients.
Participants’ missing data were unrelated to gender, maternal marital satisfaction at age 6, or maternal mood disorders at age 9 (all p’s > .40). However, the mothers of participants with any missing data reported slightly lower marital satisfaction at age 3 (M = 14.09, SD = 5.15) relative to mothers of participants with no missing data (M = 16.12, SD = 3.54), t(335) = 3.35, p < .01. Additionally, mothers of participants with any missing data were somewhat more likely to have had a mood disorder at age 3 relative to mothers of participants with no missing data, χ2 (1) = 5.32, p < .05. However, these two variables were not our primary independent, mediational, or dependent variables, so these patterns of missingness are unlikely to affect results. Data were thus viewed as missing at random for analyses, and so FIML procedures were considered appropriate for modeling missing data.
Results
Correlations among all major study variables can be found in Table 1. The correlations between broad-band inventory-assessed symptoms, narrow-band interview-assessed symptoms, and temperament dimensions were no more than moderate, suggesting that although these domains were related to each other in the expected manner, none were entirely redundant.
Table 1.
Correlations among all major study variables
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Sex (m) | 1 | |||||||||||||||
| 2. PAPA ODD Sxs | −.11* | 1 | ||||||||||||||
| 3. PAPA ADHD Sxs | −.16** | .48** | 1 | |||||||||||||
| 4. PAPA Anxiety Sxs | −.07 | .24** | .15** | 1 | ||||||||||||
| 5. PAPA Depression Sxs | −.05 | .54** | .37** | .47** | 1 | |||||||||||
| 6. CBCL Internalizing Parent Report | −.04 | .30** | .13** | .46** | .41** | 1 | ||||||||||
| 7. CBCL Externalizing Parent Report | −.08 | .62** | .43** | .20** | .44** | .55** | 1 | |||||||||
| 8. CBQ Surgency Parent Report | −.16** | .22** | .37** | −.34** | .01 | −.29** | .26** | 1 | ||||||||
| 9. CBQ NA Parent Report | .14** | .34** | .13** | .36** | .38** | .51** | .43** | −.18** | 1 | |||||||
| 10. CBQ EC Parent Report | .18** | −.32** | −.47** | −.08 | −.21** | −.14** | −.53** | −.29** | −.21** | 1 | ||||||
| 11. Age 3 Mom Mood | .05 | .08 | .10* | .17** | .18** | .16** | .10* | .01 | .13** | .02 | 1 | |||||
| 12. Age 3 Mom Substance Disorder | .07 | .1* | .01 | .12* | .17** | .07 | .04 | −.02 | .10* | −.03 | .19** | 1 | ||||
| 13. Age 3 Mom Anxiety Disorder | −.02 | .15** | .16** | .16** | .20** | .16** | .17** | −.01 | .13** | −.09 | .28** | .17** | 1 | |||
| 14. Age 3 Mother Dyadic Adjust Scale | −.03 | −.06 | −.02 | −.03 | −.05 | −.10* | −.13** | −.01 | −.02 | .04 | −.14** | −.01 | −.10* | 1 | ||
| 15. Age 6 Mother Dydadic Adjust Scale | .01 | −.15** | −.08 | −.10 | −.13* | −.14** | −.19** | .04 | .05 | .09 | −.16** | −.06 | −.13* | .75*** | 1 | |
| 16. Age 9 Mom Mood | −.03 | .24** | .11* | .14** | .26** | .16** | .22** | .07 | .14** | −.07 | .24** | .02 | .20** | −.15 | −.18** | 1 |
| Mean | 7.74 | 3.91 | 6.79 | 1.97 | −0.03 | 0 | 0.04 | −0.02 | 0 | 15.87 | 16.1 | |||||
| Standard Deviation | 6.07 | 6.22 | 6.23 | 2.2 | 0.86 | 0.88 | 0.92 | 0.86 | 0.92 | 6.50 | 3.56 | |||||
| N (%) | 237 (53.7) |
152 (34.5) |
99 (22.4) |
152 (34.5) |
58 (13.2) |
Note: NA = Negative Affect; EC = Effortful Control.
p < .05.
p < .01.
p < .001.
At the first assessment, 2 mothers (0.4%) met criteria for lifetime Bipolar Disorder, 132 (27.8%) for lifetime MDD, and 59 (12.4%) for lifetime dysthymia. During the six-year follow-up period, none of the mothers experienced a manic or hypomanic episode, 54 (9.1%) experienced a full major depressive episode (MDE) at some point in the interval, and 14 (2.4%) met criteria for dysthymic disorder during the interval. At the time of the follow-up assessment, 21 mothers (5.0%) were in a current MDE. Overall, 115 mothers (26.1%) had a mood disorder at or before the initial assessment; 21 (4.8%) had a first onset of a mood disorder between the initial assessment and the 6-year follow-up; 37 (8.4%) had mood disorder episodes both prior to and after the initial assessment; and 268 (60.8%) had no history of mood disorder before the initial assessment and during the 6-year follow-up interval.
At age 3, 34 children (8.0%) exhibited clinically significant externalizing problems, and 26 children (6.1%) exhibited clinically significant internalizing problems on the CBCL (T scores ≥ 64; Achenbach, 1991).
Logistic Regression Analyses
In all three models, prior history of maternal mood and anxiety disorders predicted subsequent maternal mood disorders, but maternal history of substance use disorders was not a significant predictor (see Tables 2–4). We also explored the effects of child sex; this was not a significant predictor and was consequently dropped from the models.
Table 2.
Predicting maternal mood disorders at age 9 assessment from CBCL variables
| DV: Time 3 MMD | B(SE B) | Wald | OR (CI) |
|---|---|---|---|
| Predictor: | |||
| Time 1 MMD | 1.16(.32)*** | 13.47 | 3.19 (1.72 – 5.93) |
| Time 1 Maternal Substance Disorder | −.31(.35) | .78 | .74 (.37 – 1.47) |
| Time 1 Maternal Anxiety Disorder | .73(.31)* | 5.54 | 2.08 (1.11 – 3.88) |
| CBCL Internalizing | .09(.19) | .22 | 1.10 (.76 – 1.59) |
| CBCL Externalizing | .52(.20)** | 6.76 | 1.68 (1.13 – 2.49) |
Note: MMD = Maternal Mood Disorder;
p < .05.
p < .01.
p < .001.
Table 4.
Predicting maternal mood disorders at age 9 assessment from CBQ variables
| DV: Time 3 MMD | B(SE B) | Wald | OR (CI) |
|---|---|---|---|
| Predictor: | |||
| Time 1 MMD | 1.18(.31)*** | 14.65 | 3.24 (1.78 – 5.92) |
| Time 1 Maternal Substance Disorder | −.41(.35) | 1.30 | .67 (.33 – 1.34) |
| Time 1 Maternal Anxiety Disorder | .82(.32)** | 6.54 | 2.28 (1.21 – 4.28) |
| CBQ Surgency | .31(.17)+ | 3.25 | 1.36 (.97 – 1.91) |
| CBQ NA | .51(.22)* | 5.29 | 1.67 (1.08 – 2.59) |
| CBQ Effortful Control | −.06(.19) | .09 | .95 (.65 – 1.38) |
Note: MMD = Maternal Mood Disorder;
p <.10.
p < .05.
p < .01.
p < .001.
The first model (Table 2) focused on child CBCL internalizing and externalizing scores as predictors of maternal mood disorders. There was a significant unique effect for externalizing problems, but the effect for internalizing symptoms was not significant.
In the next model (Table 3), the four PAPA dimensional symptom scores were entered simultaneously. Adjusting for the effects of each of the four symptom scores, only child depression symptoms significantly predicted later maternal mood disorders, although there was also a non-significant trend (p < .10) for child ODD symptoms.
Table 3.
Predicting maternal mood disorders at age 9 assessment from PAPA variables
| DV: Time 3 MMD | B(SE B) | Wald | OR (CI) |
|---|---|---|---|
| Predictor: | |||
| Time 1 MMD | 1.15(.32)*** | 12.90 | 3.16 (1.68 – 5.95) |
| Time 1 Maternal Substance Disorder | −.44(.35) | 1.58 | .64 (.32 – 1.28) |
| Time 1 Maternal Anxiety Disorder | .73(.33)* | 4.89 | 2.07 (1.09 – 3.94) |
| PAPA ODD | .11(.06)+ | 3.36 | 1.12 (.99 – 1.27) |
| PAPA ADHD | −.04(.05) | .64 | .96 (.86 – 1.07) |
| PAPA Depression | .18(.09)* | 4.00 | 1.19 (1.01 – 1.42) |
| PAPA Anxiety | .001(.03) | .001 | 1.00 (.95 – 1.05) |
Note: MMD = Maternal Mood Disorder;
p <.10,
p < .05,
p < .01,
p < .001.
In the last model (Table 4), CBQ NA, surgency, and effortful control were entered into the model. Child NA was the only significant unique predictor of maternal mood disorders 6 years later, although there was also a non-significant trend for greater surgency to be associated with a higher risk of maternal mood disorders.
Mediation Models
Next we tested a series of three mediation models examining whether maternal marital satisfaction at the age 6 assessment mediated the significant associations of age 3 child externalizing problems, depressive symptoms, and NA with maternal mood disorders at the age 9 assessment (see Figures 1 and 2). Given the moderate correlation between child depressive symptoms and externalizing symptoms (r = .44, see Table 1), their indirect effects on maternal mood disorders at age 9 via marital satisfaction at age 6 were examined in separate models, as their effects likely would cancel one another out if examined simultaneously.
Figure 1.
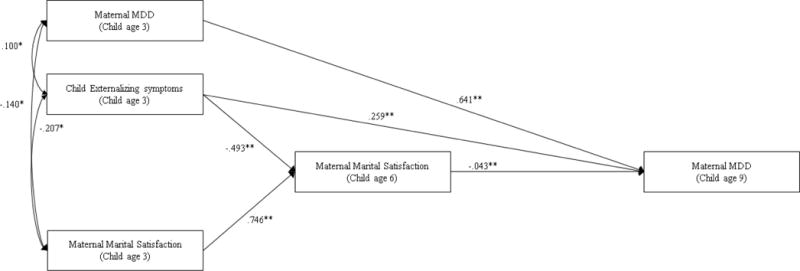
**p < .01, * p < .05. Path model of Maternal Mood Disorder predicted by Child Externalizing symptoms, and Maternal Marital Satisfaction.
Figure 2.
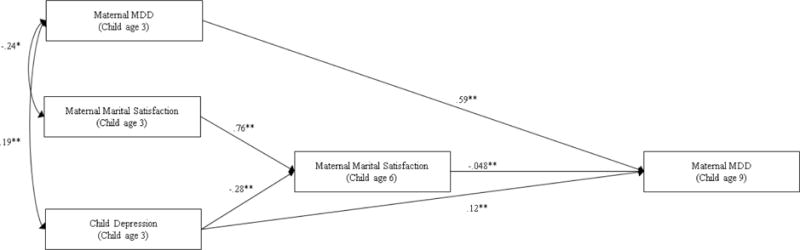
**p < .01, * p < .05. Path model of Maternal mood disorders predicted by Child depression and Maternal Marital Satisfaction.
In our first model (Figure 1), child externalizing symptoms at age 3 was the independent variable, which was initially allowed to predict marital satisfaction assessed at the child age 6 assessment as well as maternal mood disorders at the child age 9 assessment. The effects of maternal marital satisfaction and MDD at child age 3 on marital satisfaction at child age 6 were also controlled for. Finally, the effects of maternal lifetime mood disorders in the initial assessment and maternal marital satisfaction in the second (age 6) assessments on maternal mood disorders when the child was 9 years old were included in the model. All variables in the initial assessment were covaried in order to adjust for their associations.
The second (Figure 2) and third models were identical to the first, the only differences being that child depressive symptoms in one, and child NA in the other, respectively, were the independent variables. All three models were initially fully saturated (i.e., all independent variables were allowed to predict the mediator as well as the dependent variable), with the exception that we did not include a main effect of maternal marital satisfaction in the initial assessment on maternal mood disorders when the child was 9 years old.
Child Externalizing symptoms
The fit of the initial model, in which child externalizing symptoms predicted maternal marital satisfaction, which in turn predicted maternal mood disorders, was excellent: χ2 (1, N = 423) = .331, p = .57, χ2/df = .331, CFI = .100, RMSEA < .001. We trimmed a non-significant path from maternal mood disorders at the initial assessment to marital satisfaction at the age 6 assessment. This model showed an excellent fit to the data: χ2 (2, N = 423) = 2.75, p = .25, χ2/df = 1.375, CFI = .996, RMSEA = .029. There was no significant difference in fit between this model and the initial model with all paths included, χ2 = 2.33 (1), p = .13; the more parsimonious of the two was therefore preferred (Figure 1).
Higher levels of child externalizing symptoms predicted lower levels of marital satisfaction, which in turned predicted an increased probability of the mother experiencing a mood disorder when the child was aged 9. This indirect effect was significant, 95% CI [.001, .05], p < .05.
Child depression
The fit of the initial model, in which child depression predicted marital satisfaction, which in turn predicted maternal mood disorders, was excellent: χ2 (2, N = 423) = 1.122, p = .58, χ2/df = .561, CFI = 1.00, RMSEA < .00. On the basis of Wald chi-square tests (see Fox, 1997), non-significant paths were removed one at a time, and the model was re-estimated. A non-significant covariance between initial maternal marital satisfaction and child depression was trimmed. All other paths were significant. This model had an excellent fit: χ2 (3, N = 423) = 1.845, p = .60, χ2/df = .65, CFI = 1.00, RMSEA < .00. There was no significant difference in fit between this model and the initial model with all paths included, χ2 = 1.60(1), p = .21; the more parsimonious of the two was therefore preferred (Figure 2).
Higher levels of child depression predicted lower levels of maternal marital satisfaction in the age 6 assessment, lower levels of which in turn predicted an increased likelihood of a mood disorder in mothers when the children were age 9. The bootstrapped indirect effect of child depression on maternal mood disorders via marital satisfaction trended towards significance, 92.5% CI [−.001, .027], p = .06. Higher levels of child depression additionally showed a direct effect on maternal mood disorders such that they predicted an increased probability of a maternal mood disorder at the age 9 assessment.
Finally, in a separate model, we examined whether child NA at age 3 predicted maternal mood disorders at the age 9 assessment via maternal marital satisfaction at the age 6 assessment. Child NA was not significantly related to marital satisfaction, and thus did not show an indirect effect on maternal mood disorders via marital satisfaction (p > .24), although its significant direct effect on maternal mood disorders remained, β = .21, p = .02.
Discussion
Many studies have examined the effects of maternal mood disorders on children, but relatively few have evaluated the impact of child characteristics on mothers’ later risk for mood disorders. Furthermore, there are a number of factors that may play a mediating role in the relationship between child traits and later maternal psychopathology. In this study, we examined clinically significant episodes of mood disorders in mothers. In addition, we investigated young children’s symptoms at both the higher-order level of internalizing and externalizing syndromes, and at the more specific level of DSM diagnosis-based symptom dimensions. We also considered children’s temperament, which, while conceptually distinct from psychopathology, may predispose to, or fall on the spectrum of, psychopathology (Klein et al., 2012). Finally, we examined mothers’ reports of their marital satisfaction as a mediator of the subsequent development of maternal mood disorders.
In our initial analyses, we examined the associations of child symptom and temperament dimensions on later maternal mood disorders. After controlling for the effects of prior maternal mood, anxiety, and substance disorders, child externalizing problems, depression symptoms, and temperamental NA at age 3 emerged as significant predictors of maternal mood disorders six years later. These effects may reflect the challenges and burdens of parenting young children with high levels of negative affect, emotion dysregulation, and non-compliance. Alternatively, there may be third variables that are associated with both child and maternal psychopathology (e.g., genes, problematic parenting and family processes, difficult life circumstances), although controlling for prior maternal mood, anxiety, and substance use disorders should account for some of this variance.
These findings highlight the importance of identifying the processes that mediate the relationships between children’s early symptoms and temperament and mothers’ subsequent risk for depression. Raposa and colleagues (2011) found that child-related stress mediated the association between child diagnoses and parental depression. However, child-specific stress is likely not the only contextual variable that is both influenced by child characteristics and increases risk for mood disorders in parents. In our sample, mothers’ marital satisfaction mediated the path between child externalizing problems and later maternal mood disorders. This indicates that, consistent with prior research, child externalizing behaviors negatively impact parents’ marital relationship (Johnson & Lobitz, 1974), and that in turn increases the risk of maternal mood disorders (Beach & O’Leary, 1993; Whisman, 2013). Children who are angry, aggressive, and defiant are challenging to parent and may create conflict within the marital dyad as parents may not agree on how to manage the child’s difficult behavior, blame one another for the child’s acting out, or withdraw or become impatient with one another. However, these relationships are likely reciprocal, as marital turmoil and maternal mood disorders may also increase externalizing behaviors. Future research should continue to address these bidirectional associations.
In the mediation models, the indirect effect for child depressive symptoms on subsequent maternal mood disorders via marital satisfaction, reached only trend level of significance, while externalizing symptoms had direct, in addition to indirect, effects. Moreover, child NA had only a direct effect on maternal mood disorders. These findings suggest the possibility that there are also other mediating processes, such as child-related stressors. Alternatively, they could reflect direct environmental effects or genetic influences shared by the mother and the child. Taken together, the findings from the mediation models suggest that there are multiple direct and indirect paths from child symptoms to later maternal mood disorders, some of which operate through an impact on the marital system.
At the superfactor level, child externalizing problems was a significant predictor of maternal mood disorders, while at the disorder level, child depression, an internalizing condition, was a significant predictor of later maternal mood disorders. This pattern of findings suggests that there may be some features that are shared between child externalizing behavior and depression, such as anger and irritability, which have a particularly powerful effect on mothers’ subsequent risk for depression. It will be important to explore this possibility in future research.
We extended the current literature in several ways. First, while previous studies focused on the effects of child externalizing or pervasive developmental disorders on maternal depression, we also examined the impact of preschooler’s internalizing symptoms and temperament traits. Second, most previous studies of younger children examined effects on mothers’ levels of depressive symptoms over relatively short periods of time. Our findings add to this work by showing that the effects are evident over a number of years and extend to clinically significant mood disturbances in mothers. Finally, we found that mothers’ marital satisfaction mediates the relationship between child externalizing problems and later maternal mood disorders. This extends previous findings showing that, in adolescents, child-related stressors mediated the association between youth psychiatric disorders and maternal MDD (Raposa et al., 2011).
The present study had a number of strengths. First, we used a large unselected community sample, allowing us to circumvent many of the biases associated with clinical samples. Second, the longitudinal design provided the opportunity to predict the development of maternal mood disorders over the course of 6 years, and to preserve the temporal ordering of the independent variables (child psychopathology and temperament), mediator (marital satisfaction), and dependent variable (maternal mood disorder) while covarying for the initial values of the mediator and dependent variables. Finally, we used multiple methods (semistructured interviews and parent-report inventories) to assess child psychopathology, and multiple informants (mothers and fathers) to assess child psychopathology and temperament.
However, several limitations of our study should also be considered. First, we chose to use child symptom scores rather than diagnoses. However, most psychopathology appears to be dimensional (Markon, Chmielewski, & Miller, 2011) and thresholds for defining preschool psychopathology are even less clear than for older youth and adults (Egger & Emde, 2011).
Second, mothers provided some of information on child symptoms and behavior. Mothers who are prone to depression may view their 3 year olds more negatively or as more symptomatic than other mothers (Richters & Pellegrini, 1989). We attempted to mitigate these effects by aggregating both parents’ reports of child psychopathology and temperament on the CBCL and CBQ.
Third, it is possible that mothers’ psychopathology contributed to their children’s symptoms, which then predicted mothers’ mood disorders in a reciprocal manner. However, by controlling for prior maternal mood, anxiety, and substance disorders, it is likely that at least part of the effect does in fact travel from the child to the parent.
Fourth, we examined the association of child psychopathology and temperament with maternal depression over a relatively long period. We do not know the time period over which these effects unfold; hence, the results could be different with either shorter or longer times between assessments. However, with shorter intervals, it would not be possible to accumulate enough cases to examine the onset of clinically significant mood disorder episodes.
Fifth, the sample was largely demographically homogenous, making it challenging to generalize our findings to other demographic groups. Sixth, the number of mothers with a first onset of depression between the initial assessment and the follow up assessment 6 years later was relatively small. Additional cases, and thus more statistical power, would provide greater confidence in the results. Also, consistent with the literature, it can be expected in a community sample such as ours that rates of children who meet criteria for clinically significant symptoms would be low. In our sample, 8.0% and 6.1% of children exhibited clinically significant externalizing and internalizing problems, respectively. While we believe the findings of our study may be generalized to other community samples, they cannot be extrapolated to clinical samples.
Seventh, for a number of children, we used a screener for the ODD and ADHD sections of the PAPA rather than administering the full section, requiring us to impute a substantial amount of data for children with low levels of these symptoms. Eighth, the only outcome we examined was maternal mood disorders; child predictors and contextual mediators might differ for other outcomes.
Ninth, we did not examine the relationship between child characteristics and paternal mood disorders. Unfortunately, we did not have enough new cases of paternal mood disorders to analyze given that rates of mood disorders are much lower in men than women. However, the rationale for focusing on mothers is stronger, as the magnitude of the association between child symptoms and parental depression is much greater for mothers than fathers (Goodman et al., 2011), and the path from marital satisfaction to depression is more strongly established in women than in men (Fincham et al., 1997).
Tenth, most of the effects found were relatively small in size. As such, there are likely additional factors which were unaccounted for in this study which would further explain the occurrence of maternal depressive disorders. Finally, we did not include life stressors or treatment utilization for either the child or the mother in our models – these may have also influenced maternal and/or child psychopathology.
These findings have important implications for treatment and early family interventions. There has long been considerable interest in the impact of maternal depression on children (Barker et al., 2012; Cummings & Davies, 1994; Goodman, Brogan, Lynch, & Fielding, 1993; Hammen et al., 1987), and there is growing evidence that treatment of maternal depression ameliorates offspring psychopathology (Pilowsky et al., 2008; Weissman et al., 2006). However, it may also be important to view treatment of child psychopathology as a means of preventing later maternal mood disorders. Thus targeting child externalizing problems, depressive symptoms, and NA for intervention may not only mitigate the risk of later psychopathology in the child, but also reduce risk to the child’s parents. Further research should also focus on methods of reducing the stress that parents may experience, or increasing parents’ coping resources, when raising a child who has externalizing problems, depression, and/or high NA. Finally, our findings reinforce the importance of considering the impact of child behaviors and traits on parents’ marital and other social relationships and their subsequent impact on maternal mood disorders.
Acknowledgments
This work was supported by NIMH grant RO1 MH 069942.
Contributor Information
Anna E.S. Allmann, Department of Psychology, Stony Brook University, Stony Brook, NY 11794-2500
Daniel C. Kopala-Sibley, Department of Psychology, Stony Brook University, Stony Brook, NY 11794-2500
Daniel N. Klein, Stony Brook University, Stony Brook, NY 11794-2500
References
- Achenbach TM. Integrative guide for the 1991 CBCL/4-18, YSR, and TRF profiles. Burlington, VT: University of Vermont, Department of Psychiatry; 1991. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- Barker ED, Copeland W, Maughan B, Jaffee SR, Uher R. Relative impact of maternal depression and associated risk factors on offspring psychopathology. British Journal of Psychiatry. 2012;200:124–129. doi: 10.1192/bjp.bp.111.092346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beach SR, O’Leary KD. Marital discord and dysphoria: For whom does the marital relationship predict depressive symptomatology? Journal of Social and Personal Relationships. 1993;10:405–420. [Google Scholar]
- Befera MS, Barkley RA. Hyperactive and normal girls and boys: Mother-child interaction, parent psychiatric status and child psychopathology. Journal of Child Psychology and Psychiatry. 1985;26:439–452. doi: 10.1111/j.1469-7610.1985.tb01945.x. [DOI] [PubMed] [Google Scholar]
- Berdan LE, Keane SP, Calkins SD. Temperament and externalizing behavior: Social preference and perceived acceptance as protective factors. Developmental Psychology. 2008;44:957. doi: 10.1037/0012-1649.44.4.957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bollen KA, Davis WR. Causal indicator models: Identification, estimation, and testing. Structural Equation Modeling. 2009;16:498–522. [Google Scholar]
- Carmines EG, McIver JP. Analyzing models with unobserved variables: Analysis of covariance structures. In: Bohrnstedt GW, Borgatta EF, editors. Social measurement: Current issues. Beverly Hills, CA: Sage Publications; 1981. pp. 65–115. [Google Scholar]
- Choe DE, Sameroff AJ, McDonough SC. Infant functional regulatory problems and gender moderate bidirectional effects between externalizing behavior and maternal depressive symptoms. Infant Behavior and Development. 2013;36:307–318. doi: 10.1016/j.infbeh.2013.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choe DE, Shaw DS, Brennan LM, Dishion TJ, Wilson MN. Inhibitory control as a mediator of bidirectional effects between early oppositional behavior and maternal depression. Development and Psychopathology. 2014;26:1129–1147. doi: 10.1017/S0954579414000613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cui M, Donnellan MB, Conger RD. Reciprocal influences between parents’ marital problems and adolescent internalizing and externalizing behavior. Developmental Psychology. 2007;43:1544. doi: 10.1037/0012-1649.43.6.1544. [DOI] [PubMed] [Google Scholar]
- Cummings EM, Davies PT. Maternal depression and child development. Journal of Child Psychology and Psychiatry. 1994;35:73–122. doi: 10.1111/j.1469-7610.1994.tb01133.x. [DOI] [PubMed] [Google Scholar]
- De Pauw SSW, Mervielde I. Temperament, personality and developmental psychopathology: A review based on the conceptual dimensions underlying childhood traits. Child Psychiatry and Human Development. 2010;41:313–329. doi: 10.1007/s10578-009-0171-8. [DOI] [PubMed] [Google Scholar]
- Eaton NR, Keyes KM, Krueger RF, Balsis S, Skodol AE, Markon KE, Hasin DS. An invariant dimensional liability model of gender differences in mental disorder prevalence: Evidence from a national sample. Journal of Abnormal Psychology. 2012 Feb;121:282–288. doi: 10.1037/a0024780. 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Egger HL, Emde RN. Developmentally sensitive diagnostic criteria for mental health disorders in early childhood: The Diagnostic and Statistical Manual of Mental Disorders—IV, the Research Diagnostic Criteria—Preschool age, and the Diagnostic Classification of Mental Health and Developmental Disorders of Infancy and Early Childhood—Revised. American Psychologist. 2011;66:95. doi: 10.1037/a0021026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Egger HL, Erkanli A, Keeler G, Potts E, Walter BK, Angold A. Test-retest reliability of the preschool age psychiatric assessment (PAPA) Journal of the American Academy of Child and Adolescent Psychiatry. 2006;45:538–549. doi: 10.1097/01.chi.0000205705.71194.b8. [DOI] [PubMed] [Google Scholar]
- Eisenberg N, Guthrie IK, Fabes RA, Shepard S, Losoya S, Murphy B, Jones S, Poulin R, Reiser M. Prediction of elementary school children’s externalizing problem behaviors from attentional and behavioral regulation and negative emotionality. Child Development. 2000;71:1367–1382. doi: 10.1111/1467-8624.00233. [DOI] [PubMed] [Google Scholar]
- Fincham FD, Beach SR, Harold GT, Osborne LN. Marital satisfaction and depression: Different causal relationships for men and women? Psychological Science. 1997;8:351–356. [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. User’s guide for the structured interview for DSM-IV axis I disorders—research version (SCID-I, version 2.0) New York: New York State Psychiatric Institute, Biometrics Research; 1996. [Google Scholar]
- Fombonne E, Simmons H, Ford T, Meltzer H, Goodman R. Prevalence of pervasive developmental disorders in the British nationwide survey of child mental health. International Review of Psychiatry. 2003;15:158–165. doi: 10.1080/0954026021000046119. [DOI] [PubMed] [Google Scholar]
- Fox J. Applied regression analysis, linear models, and related methods. Beverly Hills, CA: Sage Publications, Inc; 1997. [Google Scholar]
- Gadow KD, Sprafkin J. Early Childhood Inventory – 4: Screening manual. Stony Brook, NY: Checkmate Plus; 2000. [Google Scholar]
- Ghodsian M, Zajicek E, Wolkind S. A longitudinal study of maternal depression and child behavior problems. Journal of Child Psychology and Psychiatry. 1984;25:91–109. doi: 10.1111/j.1469-7610.1984.tb01721.x. [DOI] [PubMed] [Google Scholar]
- Goodman SH, Brogan D, Lynch ME, Fielding B. Social and emotional competence in children of depressed mothers. Child Development. 1993;64:516–531. doi: 10.1111/j.1467-8624.1993.tb02925.x. [DOI] [PubMed] [Google Scholar]
- Goodman SH, Rouse MH, Connell AM, Broth MR, Hall CM, Heyward D. Maternal depression and child psychopathology: A meta-analytic review. Clinical Child and Family Psychology Review. 2011;14:1–27. doi: 10.1007/s10567-010-0080-1. [DOI] [PubMed] [Google Scholar]
- Gotlib IH, Colich NL. Children of parents with depression. In: Gotlib IH, Hammen CL, editors. Handbook of Depression. 3rd. New York: Guilford Press; 2014. pp. 240–258. [Google Scholar]
- Hammen C. Interpersonal stress and depression in women. Journal of Affective Disorders. 2003;74:49–57. doi: 10.1016/s0165-0327(02)00430-5. [DOI] [PubMed] [Google Scholar]
- Hammen C, Adrian C, Gordon D, Burge D, Jaenicke C, Hiroto D. Children of depressed mothers: maternal strain and symptom predictors of dysfunction. Journal of Abnormal Psychology. 1987;96:190. doi: 10.1037//0021-843x.96.3.190. [DOI] [PubMed] [Google Scholar]
- Hastings RP. Parental stress and behavior problems of children with developmental disability. Journal of Intellectual & Developmental Disability. 2002;27:149–160. [Google Scholar]
- Herring S, Gray K, Taffe J, Tonge B, Sweeney D, Einfeld S. Behavior and emotional problems in toddlers with pervasive developmental disorders and developmental delay: associations with parental mental health and family functioning. Journal of Intellectual Disability Research. 2006;50:874–882. doi: 10.1111/j.1365-2788.2006.00904.x. [DOI] [PubMed] [Google Scholar]
- Hoyle RH, Panter AT. Writing about structural equation models. In: Hoyle FH, editor. Structural equation modeling: concepts, issues, and applications. Thousand Oaks: Sage Publications; 1995. pp. 158–176. [Google Scholar]
- Johnson SM, Lobitz GK. The personal and marital adjustment of parents as related to observed child deviance and parenting behaviors. Journal of Abnormal Child Psychology. 1974;2:193–207. doi: 10.1007/BF00918887. [DOI] [PubMed] [Google Scholar]
- Kenny DA, Kashy DA, Bolger N. Data analysis in social psychology. In: Gilbert D, Fiske S, Lindzey G, editors. Handbook of social psychology. 4th. Vol. 1. New York: McGraw-Hill; 1998. pp. 233–265. [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Koretz D, Merikangas KR, Wang PS. The epidemiology of major depressive disorder. Journal of the American Medical Association. 2003;289:3095–3105. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- Klein DN, Dyson MW, Kujawa AJ, Kotov R. Temperament and internalizing disorders. In: Zentner M, Shiner R, editors. Handbook of Temperament. New York: Guilford Press; 2012. pp. 541–561. [Google Scholar]
- Kline R. Principles and practice of structural equation modeling. New York: Guilford Press; 1998. [Google Scholar]
- Laceulle OM, Ormel J, Vollebergh WA, Aken MA, Nederhof E. A test of the vulnerability model: temperament and temperament change as predictors of future mental disorders–the TRAILS study. Journal of Child Psychology and Psychiatry. 2014;55:227–236. doi: 10.1111/jcpp.12141. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Olino TM, Klein DN. Psychosocial impairments in offspring of depressed parents. Psychological Medicine. 2005;35:1493–1503. doi: 10.1017/S0033291705005350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Little RJ, Rubin DB. The analysis of social science data with missing values. Sociological Methods & Research. 1989;18:292–326. [Google Scholar]
- Lyneham HJ, Rapee RM. Agreement between telephone and in-person delivery of a structured interview for anxiety disorders in children. Journal of the American Academy of Child and Adolescent Psychiatry. 2005;44:274–282. doi: 10.1097/00004583-200503000-00012. [DOI] [PubMed] [Google Scholar]
- Markon KE, Chmielewski M, Miller CJ. The reliability and validity of discrete and continuous measures of psychopathology: a quantitative review. Psychological Bulletin. 2011;137:856. doi: 10.1037/a0023678. [DOI] [PubMed] [Google Scholar]
- Mineka S, Anand D, Sumner J. Generalized anxiety disorder. In: Richards CS, O’Hara MW, editors. The Oxford handbook of depression and comorbidity. Oxford: Oxford University Press; 2014. pp. 129–147. [Google Scholar]
- Murray KT, Kochanska G. Effortful control: Factor structure and relation to externalizing and internalizing behaviors. Journal of Abnormal Child Psychology. 2002;30:503–514. doi: 10.1023/a:1019821031523. [DOI] [PubMed] [Google Scholar]
- Muthen B, Kaplan D, Hollis M. On structural equation modeling with data that are not missing completely at random. Psychometrika. 1987;52:431–462. [Google Scholar]
- Najavits LM, Capezza NM. Depression and alcohol use. In: Richards CS, O’Hara MW, editors. The Oxford handbook of depression and comorbidity. Oxford: Oxford University Press; 2014. pp. 100–110. [Google Scholar]
- Pilowsky D, Wickramaratne P, Talati A, Tang M, Hughes C, Garber J, Weissman MM. Children of depressed mothers 1 year after the initiation of maternal treatment: findings from the STAR* D-Child Study. American Journal of Psychiatry. 2008;165:1136–1147. doi: 10.1176/appi.ajp.2008.07081286. [DOI] [PubMed] [Google Scholar]
- Putnam SP, Sanson AV, Rothbart MK. Child temperament and parenting. In: Bornstein M, editor. Handbook of parenting. Mahwah, NJ: Lawrence Erlbaum; 2002. pp. 255–277. [Google Scholar]
- Rao PA, Beidel DC. The impact of children with high-functioning autism on parental stress, sibling adjustment, and family functioning. Behavior Modification. 2009;33:437–451. doi: 10.1177/0145445509336427. [DOI] [PubMed] [Google Scholar]
- Raposa EB, Hammen CL, Brennan PA. Effects of child psychopathology on maternal depression: The mediating role of child-related acute and chronic stressors. Journal of Abnormal Child Psychology. 2011;39:1177–1186. doi: 10.1007/s10802-011-9536-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richters J, Pellegrini D. Depressed mothers’ judgment about their children: An examination of depression–distortion hypothesis. Child Development. 1989;50:1068–1075. doi: 10.1111/j.1467-8624.1989.tb03537.x. [DOI] [PubMed] [Google Scholar]
- Rohde P, Lewinsohn PM, Seeley JR. Comparability of telephone and face-to-face interviews in assessing axis I and II disorders. American Journal of Psychiatry. 1997;154:1593–1598. doi: 10.1176/ajp.154.11.1593. [DOI] [PubMed] [Google Scholar]
- Rothbart MK, Ahadi SA, Hershey KL, Fisher P. Investigations of temperament at three to seven years: The Children’s Behavior Questionnaire. Child Development. 2001;72:1394–1408. doi: 10.1111/1467-8624.00355. [DOI] [PubMed] [Google Scholar]
- Sabourin, Valois, Lussier Development and validation of a brief version of the Dyadic Adjustment Scale with a nonparametric item analysis model. Psychological Assessment. 2005;17:15–27. doi: 10.1037/1040-3590.17.1.15. [DOI] [PubMed] [Google Scholar]
- Schafer JL. Analysis of incomplete multivariate data. Boca Raton, FL: CRC Press; 1997. [Google Scholar]
- Shaw DS, Gross H, Moilanen K. Developmental transactions between boys’ conduct problems and mothers’ depressive symptoms. In: Sameroff A, editor. Transactional processes in development. Washington D.C.: American Psychological Association; 2009. pp. 77–96. [Google Scholar]
- Sprafkin J, Volpe RJ, Gadow KD, Nolan EE, Kelly K. A DSM-IV-referenced screening instrument for preschool children: The Early Childhood Inventory-4. Journal of the American Academy of Child and Adolescent Psychiatry. 2002;41:604–612. doi: 10.1097/00004583-200205000-00018. [DOI] [PubMed] [Google Scholar]
- Tackett J, Martel M, Kushner S. Temperament, externalizing disorders, and attention-deficit/hyperactivity disorder. In: Zentner M, Shiner R, editors. Handbook of Temperament. New York: Guilford Press; 2012. pp. 562–580. [Google Scholar]
- Weissman MM, Pilowsky DJ, Wickramaratne PJ, Talati A, Wisniewski SR, Fava M, Rush AJ. Remissions in maternal depression and child psychopathology: a STAR* D-child report. Journal of the American Medical Association. 2006;295:1389–1398. doi: 10.1001/jama.295.12.1389. [DOI] [PubMed] [Google Scholar]
- Whisman MA. Relationship discord and the prevalence, incidence, and treatment of psychopathology. Journal of Social and Personal Relationships. 2013;30:163–170. [Google Scholar]
- Williams JB, Gibbon M, First MB, Spitzer RL, Davies M, Borus J, Wittchen HU. The structured clinical interview for DSM-III-R (SCID) II. Multisite test-retest reliability. Archives of General Psychiatry. 1992;49:630. doi: 10.1001/archpsyc.1992.01820080038006. [DOI] [PubMed] [Google Scholar]


