Abstract
Objectives:
Adherence with diet and prescribed purgative is essential for proper cleansing with low-volume bowel preparations. The aim of this work was to assess the effect of a customized mobile application (App) on adherence and quality of bowel preparation.
Methods:
One hundred and sixty (160) eligible patients scheduled for elective colonoscopy were randomly assigned to paper (control) or App-based instructions. The preparation consisted of low-fiber diet for 2 days, clear fluids for one day and split-dose sodium picosulfate/magnesium citrate (SPS). Before colonoscopy, information was collected regarding adherence with, and utility of the provided instructions. The colonoscopists, blinded to assignment, graded bowel preparation using the Aronchick, Ottawa, and Chicago preparation scales. The primary endpoint was adherence with instructions. Quality of preparation was a secondary endpoint.
Results:
No difference in overall adherence or bowel cleanliness was observed between the study arms. Adherence was reported in 82.4% of App vs. 73.4% of controls (P=0.40). An adequate bowel preparation on the Aronchick scale was noted in 77.2 vs. 82.5%, respectively (P=0.68). Mean scores on the Ottawa and Chicago scales were also similar. Gender, age, time of colonoscopy, and BMI did not influence preparation or adherence. Compliance with the clear fluid diet component was noted in 94% of patients with BMI<30 vs. 77% with BMI≥30 (P<0.01). SPS was well tolerated by 81.9% of patients. The App was user-friendly and received higher overall rating in this respect than paper instructions (P<0.01).
Conclusions:
SPS is well tolerated and effective for bowel cleansing regardless of instruction method. Customized smartphone applications are effective, well-accepted and could replace standard paper instructions for bowel preparation.
ClinicalTrials.gov: NCT02410720
Introduction
Colonoscopy is the preferred procedure for investigating diseases of the colon and terminal ileum and is the current gold standard for colorectal cancer screening due to its high diagnostic sensitivity and specificity for detecting precancerous lesions. For optimal performance and visualization of mucosal details, an adequate bowel preparation is essential. Inadequate bowel preparation occurs surprisingly often and in as many as 25% of patients.1 Inadequate bowel preparation is associated with prolonged procedure time, incomplete examination, increased cost, and missed pathology.2 Predictors of an inadequate bowel preparation include medical factors like chronic constipation, use of opioids and tricyclic antidepressants, diabetes mellitus, and obesity as well as other patient-related factors such as education, health literacy, and motivation.3 Adherence with the prescribed laxative regimen is an essential step to an effective bowel preparation. However, more than 20% of patients describe important negative experiences with bowel preparations particularly relating to volume and taste of the solution, as well as associated hunger and sleep disturbances.4 Low volume bowel preparations are an effective alternative in normal-transit healthy individuals but usually necessitate adherence to dietary modifications, the duration of which ranges from 1–3 days before the scheduled examination date.5, 6, 7
Providing clear and easy to follow instructions can positively influence the quality of bowel preparation solutions8, 9, 10 and has become common practice in modern settings. The advent of mobile technology and wide spread use of smartphones and smartphone applications is increasingly permitting the delivery of medical information to patients at the touch of a button. Text messaging (SMS) and mobile applications are being employed by both health care professionals and patients in order to improve communication, patient medication adherence, and disease outcome in different medical subspecialties.11, 12, 13, 14 Recent studies have investigated the role of SMS reminders as well as mobile applications in improving the quality of bowel preparation as well as colonoscopy outcome using different bowel preparation regimens15, 16, 17 but literature remains limited. In this study, using a randomized single blind trial design, we investigate the effect of a customized mobile application that delivers push notifications to notify users of new messages or events even when users are not actively using the application, timely reminders, dietary recommendations, and clear bowel preparation instructions prior to colonoscopy.
Methods
Consecutive adult patients presenting for elective colonoscopy and who owned a personal smartphone with internet access were recruited during office visits to their gastroenterologist who assessed their eligibility for inclusion in the study. Exclusion criteria included: age<18, pregnant or lactating females, known inflammatory bowel disease, significant gastroparesis, gastric outlet obstruction, psychiatric disease, known or suspected poor compliance, severe chronic kidney disease (creatinine clearance <30 ml/min), severe congestive heart failure (New York Heart Association class III or IV), chronic laxative use or dependence, chronic constipation (<3 spontaneous bowel movements per week), uncontrolled hypertension (systolic blood pressure ≥170 mm Hg, diastolic blood pressure ≥100 mm Hg), and prior segmental colon resection. It is to note that patients who had previously undergone colonoscopy were not excluded, however, most (80%) of our sample population consisted of patients having their first colonoscopy. After written informed consent, patients were randomized using a computer-generated, pre-set randomization list to receive paper instructions vs. paper and smartphone application (App) instructions. Patients randomized to the smartphone App were asked to review the paper instructions for quality assessment and instructed to rely exclusively on the smartphone App instructions except in case of App dysfunction or loss of their smartphone. All elective colonoscopies were scheduled between 10 AM and 4 PM, and were performed by two experienced endoscopists who were unaware of group allocation. An independent investigator performed randomization, provided instructions (paper and App downloading and training), and collected the data before and after colonoscopy. The study was approved by the Institutional Review Board of the American University of Beirut Medical Center and registered at ClinicalTrials.gov (identifier: NCT02410720).
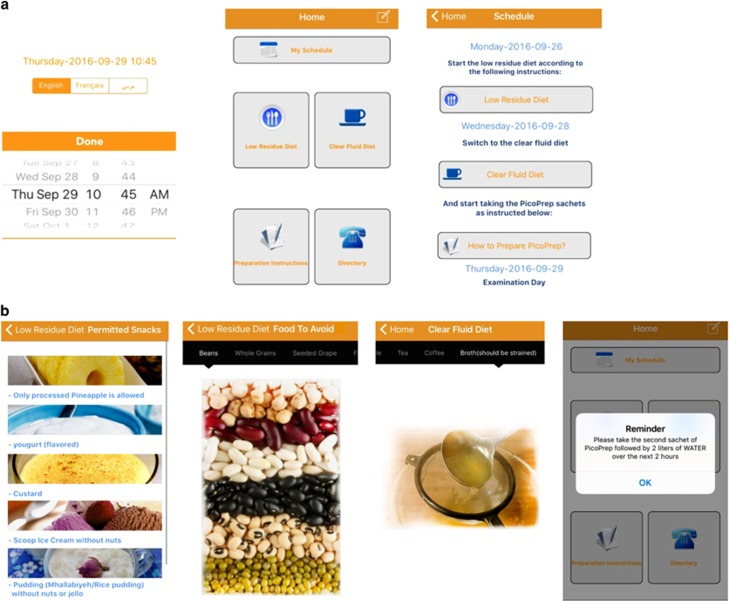
Bowel preparation instructions
Right after their office visit, eligible patients were seen by the post-doctoral research fellow who obtained the informed consent and instructed the patients on the use of the bowel preparation, presenting the information thoroughly in form of paper instructions or via the App. A brief overview of the App was given after downloading it onto the patient's smartphone. All patients were instructed to follow a 3-day diet consisting of a low-fiber diet for the first 2 days (D−3 and D−2) followed by a clear fluid diet on the last day (D−1) prior to the day of colonoscopy (D0). Patients in both groups received a list of foods to avoid during the low-fiber diet period, a list of permitted clear fluids on D−1, and instructions on how to prepare and when to consume the bowel preparation. Patients in the App group also received a free downloadable application on their iOS or Android device that included the same instructions as above. The App was custom developed solely for the purpose of this study and designed to provide the same information as the written instructions regarding diet and preparation steps of the purgative solution. It also provided examples and photographs of low-fiber meals and of allowed clear fluids, as well as daily push notifications on when to start the appropriate diet and bowel preparation solution (D−3, D−2, D−1, D0) and a verification feature to track patient progress (Figure 1). The application had 3 languages included (Arabic, English, and French), all consisting of simple vocabulary understandable to lay people. The use of medical terms was minimized to reduce confusion and allow good understanding of the instructions. The preparation consisted of sodium picosulfate/magnesium citrate (SPS, Picoprep, Ferring, Saint-Prex, Switzerland) prepared according to the manufacturer's instructions and given in split doses with the first dose taken in the evening prior to colonoscopy at 6:00 PM and the second dose 4 h before colonoscopy.
Figure 1.
Representative images from the smartphone app. (a) Choice of language and schedule details and (b) dietary tips and recommendations, push notification, and verification feature.
Data collection
Patients were interviewed immediately prior to their colonoscopies by an independent investigator. The demographic data, including age, gender, and body mass index (BMI) were collected. All subjects completed a questionnaire to assess correct use of the preparation, defined as the use of the full preparation doses at the recommended times with the required hydration as prescribed. Additionally, compliance with the first low-fiber dietary change (100%, 75%, ≤50% of meals) and duration of use of the clear liquid diet (all day, half-day, less than half-day) were assessed in the questionnaire. Patient attitude and acceptability of the mobile application, satisfaction with paper instructions and mobile app instructions, ease of use of the application, and willingness to re-take the same preparation in the future were also evaluated. The two colonoscopists, blinded to assignment, were asked to evaluate bowel cleanliness using three scales: the modified Aronchick scale, the Ottawa Bowel Preparation Scale, and the Chicago Bowel Preparation Scale. An adequate bowel preparation using the modified Aronchick Scale was defined as either an excellent or good preparation.
Sample size calculation and statistical analysis
Sample size was based on previous literature on improvement in adherence with SMS or mobile application intervention in other health-related fields, which ranged between 60 and 85% vs. 42 and 77%.11, 12, 13, 18 We hypothesized that the mobile App group would lead to a 20% overall improvement in adherence compared with the control group and as a result to a secondary improvement in bowel preparation quality. Using a 70% adherence in the control group vs. 90% in the App group and a study power of 0.08 and alpha-error of 0.05, the sample size was estimated at 78 patients per group. We aimed to enroll a minimum of 160 patients to account for possible study withdrawals before scheduled appointment. Statistical analysis was performed using IBM SPSS Statistics version 20.0 (SPSS, Chicago, Illinois, USA). Student's t-test was used to evaluate continuous variables, reported as means±s.d. χ2 test was used to evaluate categorical variables. A P-value<0.05 was considered statistically significant.
Results
During the study period, 200 consecutive patients presenting to the private clinics at the American University of Beirut Medical Center and scheduled for elective outpatient colonoscopy were approached. 22 (11%) did not possess a personal smartphone. A total of 178 consecutive patients with personal smartphones were enrolled: 18 patients were excluded for loss of follow-up (n=11), intolerance to bowel preparation (n=3), aborted procedures (n=2), and study withdrawal (n=2). The remaining 160 patients were equally split between the study arms: 80 patients received only paper instructions (control group) and 80 patients received paper as well as the mobile App instructions (App group). Indications for colonoscopy were screening for colorectal cancer and surveillance of colon polyps in >90% of patients. The mean age was 53.8 years±12.9 (range 20–79), 55.6% of patients were males, and 27.5% of patients had a BMI of ≥30. Patient demographics were similar in the two groups except for gender where males were more represented in the App group (Table 1). All enrolled patients had high school degree education or higher.
Table 1. Patient demographics and value assessment of instruction method.
| Paper group N=80 | Application group N=80 | P-value | |
|---|---|---|---|
| Age, mean±s.d. | 55±12 | 52±13 | NS |
| Male, % | 46.3 | 65.0 | 0.02 |
| BMI≥30, n (%) | 19 (23.8%) | 25 (31.3%) | NS |
| Paper instructions rating VAS, 0–10 | 8.9±1.1 (N=80) | 7.7±2.8 (N=68) | <0.001 |
| Application instructions rating VAS, 0–10 | N/A | 8.7±1.7* (N=78) | N/A |
N/A, not applicable; NS, not significant; VAS, visual analog scale.
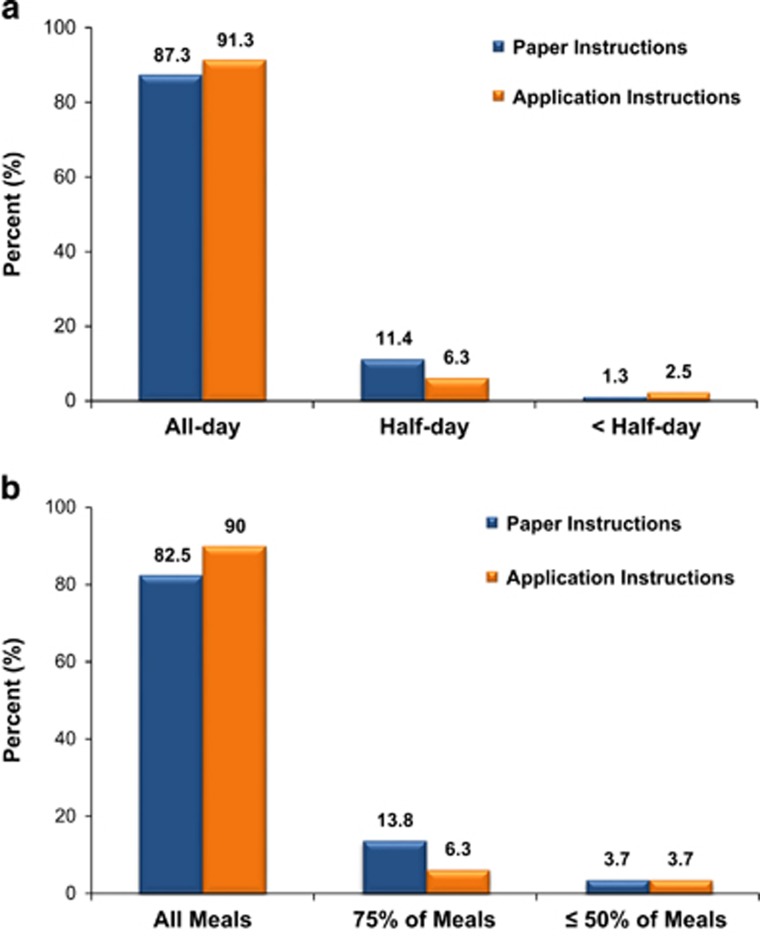
The SPS preparation was very well tolerated by 81.9% of patients as evidenced by their willingness to use it again in the future. No significant difference was observed in patient overall compliance and bowel cleanliness between both arms as measured by the three bowel preparation scales. Complete adherence with instructions (defined as full compliance with the 2-day low-fiber diet, the 1 day clear fluids, and the split-dose SPS) was reported in 73.4% of controls vs. 82.4% of App patients (P=0.40). Figure 2 shows compliance with the diet according to the patients. In the App group, 90.0% reported full compliance with the 2-day low-fiber diet as compared with 82.5% in the control group (P=NS). Full compliance with the clear fluid diet (on the day before the scheduled colonoscopy) was reported by 91.3 vs. 87.3% of patients in the App vs. control group, respectively (P=NS). Of interest, full compliance with the clear fluid diet was noted in 94% of patients with BMI<30 vs. 77% of those with BMI≥30 (P<0.01). Split-dose SPS was used correctly in 97.5 and 96.2% of patients in the App and control group, respectively.
Figure 2.
Adherence with the prescribed diet: (a) Low-fiber diet on days −3 and −2; (b) Clear fluid diet on day −1.
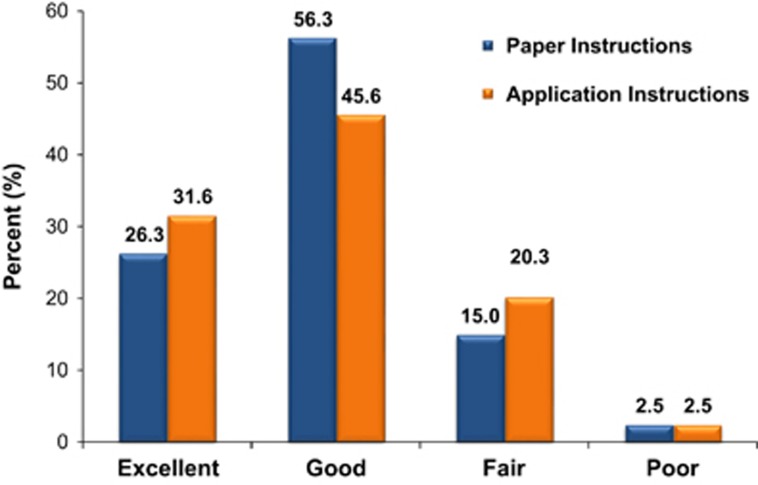
An adequate bowel preparation, defined as either excellent or good on the Aronchick scale, was noted in 82.5 and 77.2% of control vs. App group, respectively (P=0.68) (Figure 3). The mean scores on the Ottawa (6.43±1.84 vs. 6.40±1.95; P=0.93) and the Chicago Bowel Preparation Scales (32.61±3.59 vs. 32.08±4.97) were not significantly different between the control vs. App group, respectively (P=NS for both). Gender, age, BMI, and time of colonoscopy (morning or afternoon) did not influence bowel cleanliness or overall patient compliance.
Figure 3.
Bowel preparation quality on the Aronchick scale.
All patients assigned to the App group reviewed the paper instructions but reported relying exclusively on the App during the period immediately before, and leading to the examination date. The App was deemed user-friendly and helpful or indispensable by 96.2 and 87.3% of patients in the App group, respectively. On a scale of 0–10 of a visual analog scale, the 80 patients in the control group gave a rating of 8.9±1.1 for the paper instructions. The App group, recipient of both forms of instructions (paper and App), gave a rating of 7.7±2.8 for paper instructions (68 of 80 patients responding) vs. 8.7±1.7 for App instructions (78 of 80 patients responding) (P<0.01) (Table 1).
Discussion
An inadequate bowel preparation is associated with longer procedure time, reduced detection of small and large adenomas, and increased cost.1, 19 One study estimated that the cost of colonoscopy increases by 1% for every 1% of exams requiring earlier repeat as a result of unsatisfactory preparation.20 Despite the above information and the importance of bowel preparation as an important quality indicator in colonoscopy, around 20–25% of modern bowel preparations in clinical practice remain inadequate. Risk factors associated with inadequate bowel preparation include obesity, chronic constipation, and treatment with neuroleptics or antidepressants.1, 21 Health literacy22, 23, 24 and patient education9, 25 are additional, and potentially modifiable factors that can impact the quality of bowel preparation. With the advent of mobile technology into medical practice, many medical subspecialties have been turning towards mobile applications and SMS messages to improve medication adherence and intervention outcomes.15, 16, 26, 27 Few studies have investigated the effect of SMS and mobile applications on quality of bowel preparations for colonoscopy. Park et al.15 evaluated the effect of short messaging service (SMS) on bowel preparation quality and preparation-to-colonoscopy interval. There was a significant improvement in median total score of the Ottawa scale in patients who received an SMS reminding them to consume their second split dose of the preparation solution (4L PEG) on the day of scheduled colonoscopy. The SMS group had a satisfactory Ottawa score (arbitrarily set as a score ≤5) in 79.4% of patients vs. 57.8% of controls. However, the reported impact of such a simple intervention is difficult to explain, considering that although patients who consume the evening dose of PEG may be intolerant of/or unable to complete-the morning dose, they rarely require a reminder to consume it.
Lorenzo et al.16 investigated the use of a smartphone application with visual aids and timed alerts in patients receiving same day bowel preparation. In that study, a full 100% of patients (108/108) using the App achieved an adequate preparation compared with 96.1% (146/152) of recipients of the written version that included visual aids and timing notifications of commencement of intake. While same day procedures can be highly effective, such unprecedented rates of adequate bowel preparation are unusual in practice and even in clinical trials. The study investigators did not report a predetermined sample size calculation, making it unclear why this particular number of patients were enrolled. Moreover, the randomization scheme resulted in an uneven distribution (152 controls vs. 108 app), raising concern about possible selection bias. Finally, the pertinent information about diet is confusing: in the methods section, the authors state that a low-fiber diet was limited to the day before colonoscopy, however, a caption of the App specification reads (in Spanish): “During the 3 days of preparation for the colonoscopy, you should follow a low residue diet “. A difference in duration of the low-fiber diet is an important confounder and may explain the improved preparation in the app group.
A recent large study from China involving 770 patients investigated the effect of delivery of instructions via a social media (SM) App.27 An adequate bowel preparation was seen in 82.2 vs. 69.5% of controls (P<0.001). A higher adenoma detection rate (ADR) was also noted (18.6 vs. 12.0% in controls, P=0.012). No specific information was provided regarding the health literacy of the study subjects, but 44.7% of eligible patients were excluded because they had no access to social media delivering information, raising concern about a potential selection bias. The indications for colonoscopy and the study population were unrestricted (age range 18–80), making the ADR un-interpretable. Importantly, unlike the control group, the SM App group received “unrestricted access to an investigator who answered all the questions raised on the SM platform”. Although this particular “personal coaching” appears advantageous, it is hardly feasible in clinical practice and defeats the purpose of a patient-friendly practical App.
Diet remains an important aspect of the bowel preparation particularly with the more tolerable low-volume preparations such as oral sodium sulfate and sodium picosulfate/magnesium citrate.5, 6, 7 Although tolerability of the bowel preparation remains an issue in general, it is an unlikely occurrence in clinical practice for patients to actually forget to take the purgative solution. In addition, SPS is a very well tolerated preparation in terms of volume and taste.4, 28 Arguably, the added value of a smartphone application lies therefore not only in replacing paper instructions but also in providing notifications to remind patients to adhere to dietary instructions that, depending on the preparation method, may start as early as 3 days before colonoscopy. We have recently shown that compared with split-dose PEG regimens, low-volume split-dose sodium picosulfate/magnesium citrate (SPS) is associated with increased hunger as a result of stricter and longer dietary restriction. Hunger may even be more pronounced in obese patients, possibly leading to non-adherence with diet and worse outcome in terms of bowel preparation in real life.29 Our finding of significant non-adherence in obese patients to the more demanding clear fluid diet for 1 day supports this possibility. Despite a numerical improvement in full adherence with all components of the recommended diet (delta of 4.0–7.5%, P=NS) and a slightly higher rate of excellent preparations (delta of 5.2%, NS) in the App group, there was no effect on the overall quality of the bowel preparation. This may be attributable to sample size but is more likely the result of a proven intervention that is, physician-delivered patient education8 as well as the efficacy of the preparation regimen (SPS and diet) in healthy non-constipated individuals with a fair degree of health literacy. As patient compliance and preparation efficacy are directly related, interventions to enhance compliance (especially with diet) are needed and may be facilitated by widely available smartphone technology. Current technological challenges are expected to decline with time, given the increasing availability of smartphones, and the feasibility of in-app video integration and application improvements.
Our study has a few limitations. It is a single center study with a particular study population of educated smartphone owners limiting the generalizability of the results. Lebanon has a smartphone penetration of >50%,30 and although the same rate may be lower in developing countries in Asia or Africa, smartphone ownership and internet usage have continued to climb in emerging economies. Technology adoption is an expected result of an increasingly interconnected world and the number of smartphone users is forecast to grow from 1.5 billion in 2014 to around 2.5 billion in 2019. Just over 36% of the world population is projected to use a smartphone by 2018, up from about 10% in 2011(http://www.statista.com/statistics/203734/global-smartphone-penetration-per-capita-since-2005/). In 2013, a median of 45% across 21 emerging and developing countries reported using the internet at least occasionally or owning a smartphone. In 2015, that figure rose to 54%, with much of the increase coming from large emerging economies such as China, Malaysia, and Brazil. By comparison, a median of 87% of people use the internet in the United States and Canada, Western Europe, and in developed Pacific nations.30
In summary, our study confirms that a customized smartphone mobile App for bowel preparation is effective, user-friendly, and can potentially replace traditional paper instructions in this information age era. Future modifications such as the implementation of a visual aid to compare different bowel preparations, including information on volume and taste characteristics, and required dietary modifications can help patients customize their bowel preparation choice to their liking, leading to improved expectations, adherence, and possibly further improving the quality of bowel preparation.
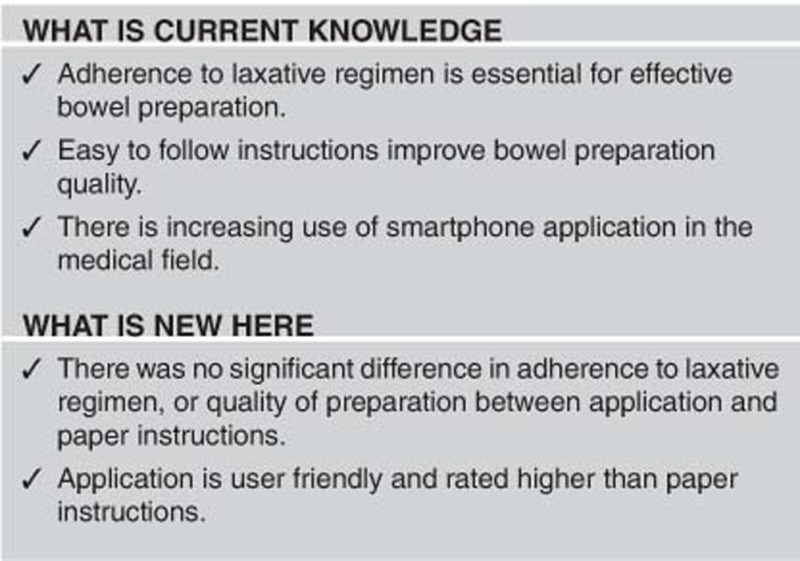
Study Highlights
Footnotes
Guarantor of the article: Ala I. Sharara, MD, FACG, AGAF.
Specific author contributions: Ala I. Sharara: Study idea, concept, design and supervision, App design and development, patient recruitment, data collection and interpretation of the data, review of the literature; drafting of the manuscript. Jean M. Chalhoub: data collection, statistical analysis, interpretation of the data, review of literature, regulatory administration, critical review of the manuscript. Maya Beydoun: literature review, App development and design, data collection, regulatory administration, drafting of the manuscript. Rani H. Shayto: data analysis, regulatory administration, drafting of the manuscript. Ali H. Harb: review of literature, App design and development, regulatory administration, patient recruitment, critical review of the manuscript. Hamed Chehab: patient recruitment, data collection, regulatory administration, critical review of the manuscript. Fadi Mourad: patient recruitment, data interpretation, critical review of the manuscript. Fayez S. Sarkis: study design, critical review of the manuscript. All authors approved the submitted version of the manuscript.
Financial support: This work was supported by a restricted research grant for an investigator-initiated study from Ferring Pharmaceuticals (AIS).
Potential competing interests: None.
References
- Sharara AI, Abou Mrad RR. The modern bowel preparation in colonoscopy. Gastroenterol Clin North Am 2013; 42: 577–598. [DOI] [PubMed] [Google Scholar]
- Burke CA, Church JM. Enhancing the quality of colonoscopy: the importance of bowel purgatives. Gastrointest Endosc 2007; 66: 565–573. [DOI] [PubMed] [Google Scholar]
- Rex DK. Bowel preparation for colonoscopy: entering an era of increased expectations for efficacy. Clin Gastroenterol Hepatol 2014; 12: 458–462. [DOI] [PubMed] [Google Scholar]
- Sharara AI, El Reda ZD, Harb AH et al. The burden of bowel preparations in patients undergoing elective colonoscopy. United European Gastroenterol J 2016; 4: 314–318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rex DK, Katz PO, Bertiger G et al. Split-dose administration of a dual-action, low-volume bowel cleanser for colonoscopy: the SEE CLEAR I study. Gastrointest Endosc 2013; 78: 132–141. [DOI] [PubMed] [Google Scholar]
- Rex DK, DiPalma JA, McGowan J et al. A comparison of oral sulfate solution with sodium picosulfate: magnesium citrate in split doses as bowel preparation for colonoscopy. Gastrointest Endosc 2014; 80: 1113–1123. [DOI] [PubMed] [Google Scholar]
- Song GM, Tian X, Ma L et al. Regime for bowel preparation in patients scheduled to colonoscopy: low-residue diet or clear liquid diet? evidence from systematic review with power analysis. Medicine 2016; 95: e2432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shieh TY, Chen MJ, Chang CW et al. Effect of physician-delivered patient education on the quality of bowel preparation for screening colonoscopy. Gastroenterol Res Pract 2013; 2013: 570180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tae JW, Lee JC, Hong SJ et al. Impact of patient education with cartoon visual aids on the quality of bowel preparation for colonoscopy. Gastrointest Endosc 2012; 76: 804–811. [DOI] [PubMed] [Google Scholar]
- Spiegel BM, Talley J, Shekelle P et al. Development and validation of a novel patient educational booklet to enhance colonoscopy preparation. Am J Gastroenterol 2011; 106: 875–883. [DOI] [PubMed] [Google Scholar]
- Suffoletto B, Calabria J, Ross A et al. A mobile phone text message program to measure oral antibiotic use and provide feedback on adherence to patients discharged from the emergency department. Acad Emerg Med 2012; 19: 949–958. [DOI] [PubMed] [Google Scholar]
- Castano PM, Bynum JY, Andres R et al. Effect of daily text messages on oral contraceptive continuation: a randomized controlled trial. Obstet Gynecol 2012; 119: 14–20. [DOI] [PubMed] [Google Scholar]
- Mitchell JD, Collen JF, Petteys S et al. A simple reminder system improves venous thromboembolism prophylaxis rates and reduces thrombotic events for hospitalized patients1. J Thromb Haemost 2012; 10: 236–243. [DOI] [PubMed] [Google Scholar]
- Johnston MJ, King D, Arora S et al. Smartphones let surgeons know whatsapp: an analysis of communication in emergency surgical teams. Am J Surg 2015; 209: 45–51. [DOI] [PubMed] [Google Scholar]
- Park J, Kim TO, Lee NY et al. The effectiveness of short message service to assure the preparation-to-colonoscopy interval before bowel preparation for colonoscopy. Gastroenterol Res Pract 2015; 2015: 628049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lorenzo-Zuniga V, Moreno de Vega V, Marin I et al. Improving the quality of colonoscopy bowel preparation using a smart phone application: a randomized trial. Dig Endosc 2015; 27: 590–595. [DOI] [PubMed] [Google Scholar]
- Kavathia NH, Berggreen P, Gerkin R. 190 Outcomes of smart phone application assisted bowel preparation for colonoscopy. Gastrointest Endosc 2013; 77: AB132. [Google Scholar]
- Foreman KF, Stockl KM, Le LB et al. Impact of a text messaging pilot program on patient medication adherence. Clin Ther 2012; 34: 1084–1091. [DOI] [PubMed] [Google Scholar]
- Johnson DA, Barkun AN, Cohen LB et al. Optimizing adequacy of bowel cleansing for colonoscopy: recommendations from the US Multi-Society Task Force on Colorectal Cancer. Am J Gastroenterol 2014; 109: 1528–1545. [DOI] [PubMed] [Google Scholar]
- Rex DK, Imperiale TF, Latinovich DR et al. Impact of bowel preparation on efficiency and cost of colonoscopy. Am J Gastroenterol 2002; 97: 1696–1700. [DOI] [PubMed] [Google Scholar]
- Rex DK. Optimal bowel preparation—a practical guide for clinicians. Nat Rev Gastroenterol Hepatol 2014; 11: 419–425. [DOI] [PubMed] [Google Scholar]
- Basch CH, Hillyer GC, Basch CE et al. Characteristics associated with suboptimal bowel preparation prior to colonoscopy: results of a national survey. Int J Prev Med 2014; 5: 233–237. [PMC free article] [PubMed] [Google Scholar]
- Nguyen DL, Wieland M. Risk factors predictive of poor quality preparation during average risk colonoscopy screening: the importance of health literacy. J Gastrointestin Liver Dis 2010; 19: 369–372. [PubMed] [Google Scholar]
- Smith SG, von Wagner C, McGregor LM et al. The influence of health literacy on comprehension of a colonoscopy preparation information leaflet. Dis Colon Rectum 2012; 55: 1074–1080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang CW, Shih SC, Wang HY et al. Meta-analysis: the effect of patient education on bowel preparation for colonoscopy. Endosc Int Open 2015; 3: E646–E652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi HS, Shim CS, Kim GW et al. Orange juice intake reduces patient discomfort and is effective for bowel cleansing with polyethylene glycol during bowel preparation. Dis Colon Rectum 2014; 57: 1220–1227. [DOI] [PubMed] [Google Scholar]
- Kang X, Zhao L, Leung F et al. Delivery of instructions via mobile social media app increases quality of bowel preparation. Clin Gastroenterol Hepatol 2016; 14: 429–435 e3. [DOI] [PubMed] [Google Scholar]
- Olabi A, George C, Daroub H et al. Sensory evaluation of commercial bowel cleaning solutions. Gastroenterology 2016; 8: 508–516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharara AI, Harb AH, Sarkis FS et al. Body mass index and quality of bowel preparation: real life vs. clinical trials. Arab J Gastroenterol 2016; 17: 11–16. [DOI] [PubMed] [Google Scholar]
- Poushter J. Smartphone Ownership and Internet Usage Continues to Climb in Emerging Economics: Pew Research Center, 2016. Available at www.pewglobal.com (Accessed on 23 Febraury 2016).