Abstract
Here we argue functional neuroanatomy for posture-gait control. Multi-sensory information such as somatosensory, visual and vestibular sensation act on various areas of the brain so that adaptable posture-gait control can be achieved. Automatic process of gait, which is steady-state stepping movements associating with postural reflexes including headeye coordination accompanied by appropriate alignment of body segments and optimal level of postural muscle tone, is mediated by the descending pathways from the brainstem to the spinal cord. Particularly, reticulospinal pathways arising from the lateral part of the mesopontine tegmentum and spinal locomotor network contribute to this process. On the other hand, walking in unfamiliar circumstance requires cognitive process of postural control, which depends on knowledges of self-body, such as body schema and body motion in space. The cognitive information is produced at the temporoparietal association cortex, and is fundamental to sustention of vertical posture and construction of motor programs. The programs in the motor cortical areas run to execute anticipatory postural adjustment that is optimal for achievement of goal-directed movements. The basal ganglia and cerebellum may affect both the automatic and cognitive processes of posturegait control through reciprocal connections with the brainstem and cerebral cortex, respectively. Consequently, impairments in cognitive function by damages in the cerebral cortex, basal ganglia and cerebellum may disturb posture-gait control, resulting in falling.
Keywords: Multisensory information, midbrain locomotor region, reticulospinal system, body schema, motor programs, Parkinson’s disease.
GENERAL SCHEMA OF POSTURE-GAIT CONTROL
Figure 1 illustrates our recent understanding of basic signal flows involved in motor control. Sensory signals arising from external stimuli and/or internal visceral information have various functions. For example, they are to be utilized for cognitive processing such as production of working memory which guides future behavior. Alternatively, they may affect emotional and arousal states. Sensory signals are further available to detect and correct postural instability by acting on the cerebral cortex, cerebellum, and brainstem. Accordingly, animal initiates movements depending on either a “cognitive reference” or an “emotional reference” [1,2].
Figure 1.
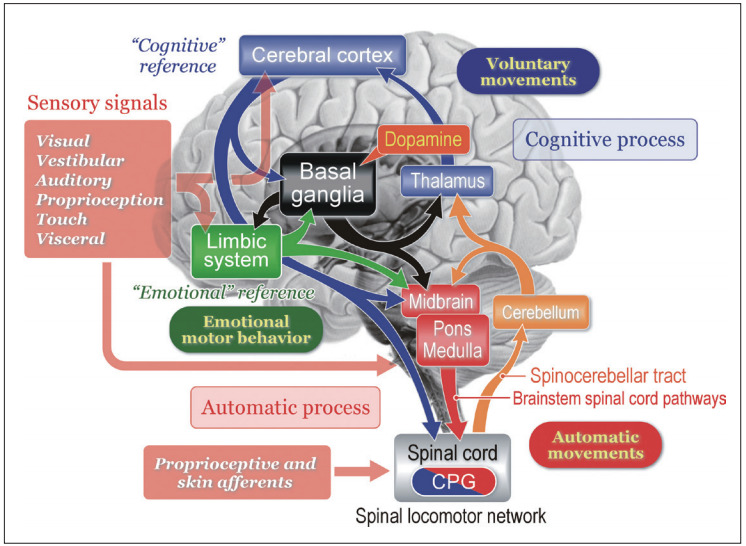
Basic signal flow involved in postural control. Multisensory signals from the visual, vestibular, auditory, somatosensory (proprioceptive), and visceral receptors act on various sites in the central nervous system. These signals may provide cognitive and emotional references to the cerebral cortex and limbic system, respectively, so that the subject may elicit either voluntary movements or emotional motor behavior depending on the context. In each case, automatic process of postural control, such regulation of postural muscle tone and basic postural reflexes, by the brainstem and spinal cord is required. On the other hand, cognitive postural control is particularly important when the subject learns motor skills and behaves in unfamiliar circumstance. See text for detail explanation. Modified from Takakusaki. Mov Disord 2013;28:1483-1491, with permission of Wiley [6].
Voluntary movements are derived from intentionally-elicited motor commands arising from the cerebral cortex to the brainstem and spinal cord. On the other hand, emotional reference may contribute to emotional motor behavior which is generated by the projections from the limbic-hypothalamus to the brainstem, such as fight or flight reactions [1,3,4]. Regardless of whether the initiation is volitional or emotional, goal-directed behaviors are always accompanied by automatic process of postural control including balance adjustment and muscle tone regulation. The subject is largely unaware of this process which is evoked by sequential activations of neurons in the brainstem and spinal cord. Basic locomotor motor pattern is generated by spinal locomotor networks that is termed as the central pattern generators (CPG). However, in order to learn motor skills or behave in unfamiliar circumstance, the subject requires cognitive posture-gait control that depends on cognition of self-body information together with spatial localization of objects in extra-personal space.
The cerebellum regulates the cognitive and automatic processes of posture-gait control by acting on the cerebral cortex via the thalamocortical projection and on the brainstem, respectively. Both the feedforward information from the cerebral cortex via the cortico-ponto-cerebellar pathway and real-time sensory feedback via the spinocerebellar tract to the cerebellum may play major roles in these operations. The basal ganglia may also contribute to the modulation of each process though its gamma-aminobutyric acid (GABA)-ergic projections to the cerebral cortex and brainstem [2,5,6]. The degree of GABAergic influence from the basal ganglia is regulated by the midbrain dopaminergic neurons [7].
BRAINSTEM AND SPINAL CORD; CORE-STRUCTURES OF POSTURE-GAIT CONTROL
In the absence of their forebrain, like a decerebrate cat, it can walk, trot and gallop. When the decerebration is made at precollicular-postmammillary level, the cat initiates locomotion by electrical or chemical stimulation applied to the mesencephalic or midbrain locomotor region (MLR) [1,8,9]. However, if the neuraxis is transected slightly higher at the precollicular-premammillary level, cats can spontaneously elicit locomotion with well-coordinated postural control [10]. Therefore, a critical region exists between these decerebrate levels. This area is recognized as the subthalamic locomotor region (SLR), which mostly corresponds to the lateral hypothalamic area. Stimulation of the SLR evoked locomotion after a large lesion was made in the MLR area [11], indicating that the SLR has direct connections with the brainstem locomotor pathway beyond the MLR. However, the walking in the decerebrate preparations is machine-like and is neither goal-directed nor adaptive to the environment. Hence, the SLR connections to the MLR are likely important for normal control of posture and gait.
So far three locomotor regions have been identified in animals: the MLR in the mesopontine tegmentum, the SLR and the cerebellar locomotor region (CLR) in the mid-part of the cerebellum [12]. Human imaging study demonstrated that the organization of these supraspinal locomotor centers was preserved during the transition to bipedal locomotion human [13]. The clinical relevance of these centers has so far been largely neglected.
Role of the mesencephalic area in the control of posture and locomotion
The MLR appears to be present in all classes of vertebrates [14]. It likely includes the cuneiform nucleus (CNF) and the pedunculopontine tegmental nucleus (PPN), although the precise location of the locomotor regulation still remains a matter of debate. The PPN is located in the ventrolateral part of the caudal mesencephalic reticular formation, composed of a heterogeneous population of neurons, containing GABA and glutamate in addition to acetylcholine [15]. Different neuronal types within the PPN area may have different functions with their own inter-connections to multiple parts of the brain. There are connections to cerebral cortex, multiple basal ganglia and limbic areas, the thalamus, the brainstem, the spinal cord and the cerebellum [16]. This key location including multiple segregate functions, renders figuring out the precise function of these regions quite complicated [17].
In the experiments using decerebrate cats, activation of neurons in the PPN suppress muscle tone via its cholinergic projections to the pontine reticular formation (PRF), while activation of neurons in the CNF mostly elicits locomotion [5,15,18-20]. Microstimulation of the transition zone between the two areas induced a mixture of locomotor rhythm with associated muscle tone suppression (Figure 2). Moreover, blocking the PRF by injecting atropine sulfate, blocked the PPN-induced atonia but facilitated MLR-induced locomotion, indicating that cholinergic PPN neurons not only control the level of muscle tone but also modulate the locomotor pattern, and do this by effects at the pontine level [15,18]. Studies in rats by Sherman et al. [21] show non-cholinergic neurons just medial to the PPN have projections to the spinal cord, while the cholinergic neurons of the PPN do not. This area at the mesopontine junction may be the true MLR. The dorsal neurons of this MLR area (laterodorsal tegmental nucleus) with spinal projections are active in locomotion, while the ventral neurons are active in standing and do not have spinal projections.
Figure 2.
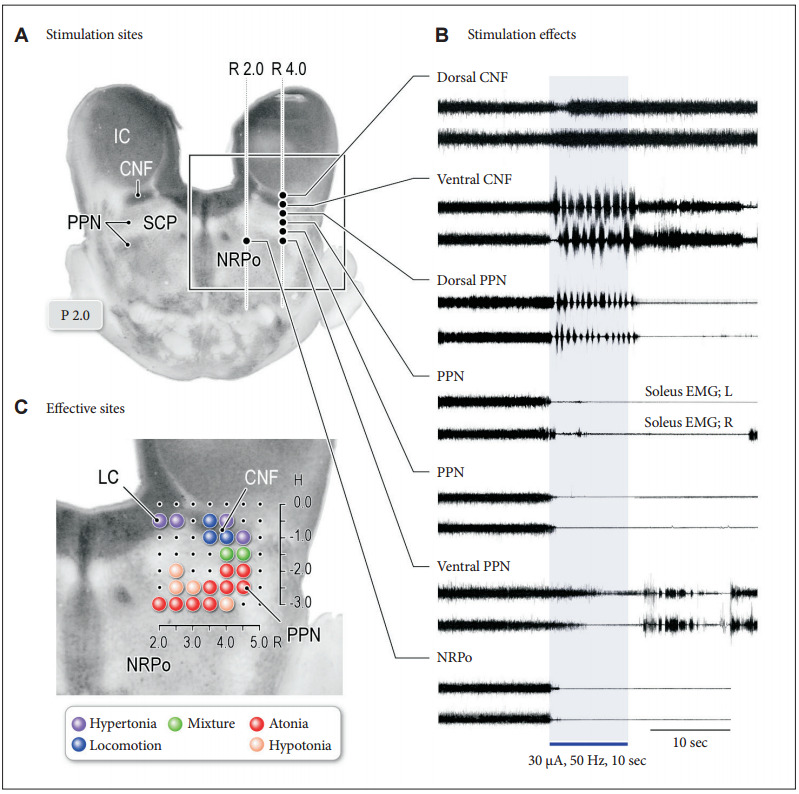
Effects of midbrain stimulation on posture and locomotion in decerebrate cat preparation. A: Stimulation sites in the right mesopontine tegmentum. Stimulation consists of 30 μA in intensity and 50 Hz in frequency with a duration of 10 seconds. B: Effects of stimulation applied to each site in (A) on left and right soleus muscle electromyograms. Stimulation of the dorsal part of the CNF induced muscle tone augmentation. While stimulation of the ventral CNF and the dorsal PPN induced locomotor rhythm, the latter was accompanied by a decrease in muscle tone. Stimulation of the PPN and PRF corresponding to the nucleus reticularis pontis oralis (NRPo) immediately suppressed soleus muscle activities. C: Topography of stimulus effects in the mesopontine tegmentum. Locomotion was evoked by stimulating the CNF (blue). Stimulation of the locus coeruleus (LC) and dorsolateral CNF induced hypertonia (violet; muscle tone augmentation). Ventrolateral part of the PPN and NRPo, induced muscular atonia (red) and hypotonia (orange). Stimuli applied to the locomotion-evoking sites and atonia-evoking sites elicited a mixture of rhythmic limb movements and muscle tone suppression (green). Modified from Takakusaki et al. J Neural Transm (Vienna) 2016;123:695-729, with permission of Springer [15]. CNF: cuneiform nucleus, PPN: pedunculopontine tegmental nucleus, IC: inferior colliculus, SCP: superior cerebellar peduncle.
Functional organization of the reticular formation in the control of posture
It is generally agreed that the reticulospinal tract (RST) contributes to regulation of the level of muscle tone. There may exist functional organization in the pontomedullary reticular formation (PMRF) in relation to the control of postural muscle tone (Figure 3) [15]. Direct recording of reticulospinal neurons (RSNs) revealed that those located in the dorso-medial part of the PMRF are active during the period of muscle tone suppression or muscular atonia (Figure 3Aa), and those in the ventromedial part are active during reflex standing due to decerebrate rigidity or hypertonus (Figure 3Ab). Accordingly, functional topographical organization may exist in the PMRF in the control of postural muscle tone. On the other hand, during MLR-elicited locomotion or spontaneously evoked locomotion in high-decerebrated preparation, RSNs located in both the dorsomedial and ventromedial PMRF were modulated in response to step cycles (Figure 3Ac), indicating that muscle tone-related RSNs participate in the execution of locomotion so that locomotor rhythm and muscle tone can be simultaneously regulated by the reticulospinal system during locomotion.
Figure 3.
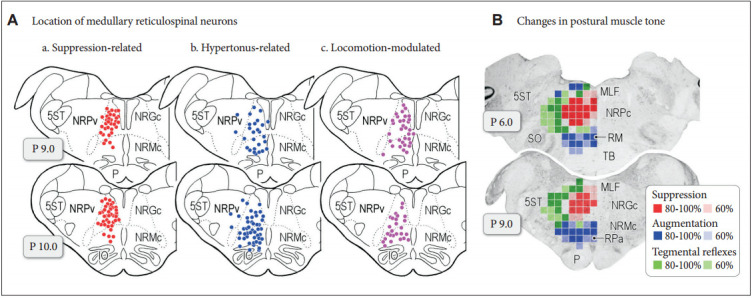
Functional organization of medullary reticulospinal systems in decerebrate cats. A: Locations of the medullary reticulospinal neurons relating to muscle tone suppression (a), muscle tone augmentation (hypertonus) (b), and locomotion (c). During reflex standing of the decerebrate cats, reticulospinal neurons with a firing frequency more than 10 Hz during reflex standing of decerebrate cats are judged as hypertonus-related reticulospinal neurons (b; n = 76). When carbachol (long-acting cholinomimetic agents) was injected into the pontine reticular formation muscle tone of decerebrate cats was abolished. Reticulospinal neurons of which firing frequency was increased to more than 10 Hz during carbachol-induced atonia are judged as atonia-related reticulospinal neurons (a; n = 75). During reflex standing (decerebrate rigidity) these cells usually had no spontaneous firing. Locomotion-related neurons (n = 59) were judged as those displaying rhythmic firing relating to step cycles of locomotion. Recording was made in both high decerebrated cats which displayed spontaneous locomotion and normal decerebrated cats with stimulation of the MLR. B: Results obtained from five animals are superimposed on representative coronal planes of the caudal pons and medulla. Sites from which either suppression (red), augmentation (blue), or tegmental reflexes (green) was elicited in more than three out of five animals are marked. Sites from which the stimulation induced postural changes in more than four animals are indicated by darker colored squares; conversely, light colored squares indicate that the postural changes were induced in three animals. Modified from Takakusaki et al. J Neural Transm (Vienna) 2016;123:695-729, with permission of Springer [15]. P: pyramidal tract, MLF: medial longitudinal fasciculus, 5ST: spinal trigeminal tract, NRPc: nucleus reticularis pontis caudalis, TB: trapezoid body, RM: nucleus raphe magnus, SO: superior olive, NRGc: nucleus reticularis gigantocellularis, NRMc: nucleus reticularis magnocellularis, RPa: nucleus raphe pallidus, NRPv: nucleus reticulars parvocellularis.
Presence of such an organization was supported by experiments using microstimulation applied to the PMRF (Figure 3B). Stimulation applied to the dorsomedial part of the PMRF resulted in general suppression of muscle tone (Figure 3B, red areas), and those applied to the ventromedial PMRF induced general augmentation of muscle tone (Figure 3B, blue areas). Neuroanatomical studies revealed that RSNs in the dorsomedial and ventromedial PMRF descend through ventral and lateral funiculi, indicating that the ventral and lateral RST are responsible for muscle tone suppression and augmentation, respectively. On the other hand, tegmental reflex, or asymmetrical postural figures, which was characterized by extension of the unilateral limb and flexion of the contralateral limb, was evoked from the area between the inhibitory and excitatory areas and the lateral part of the PMRF where few RSNs arise in the cat (Figure 3B, green areas).
In addition to the RST, vestibulospinal tract (VST) plays an important role in the control of postural equilibrium by its similar architectonic organization of descending fibers within the spinal cord with the RST [22,23]. Matsuyama and Drew [24,25] examined firing property of neurons in the RST and VST in the cat during locomotion on an inclined surface. Specifically, the VST controls primarily the overall level of postural muscle tone, while the RST has an additional role in determining the relative level of different muscles, particularly when the pattern is asymmetric.
Locomotor pathway and its control by the forebrain structures
In the “locomotor pathway”, signals from the MLR also activate medullary RSNs, in turn commanding the spinal locomotor network to generate the oscillatory pattern of locomotion [8,26]. However, the SLR and CLR may also activate this reticulospinal locomotor pathway through distinct and direct projections [27]. Signals from the MLR may also activate monoaminergic descending pathways including the coerulospinal and raphespinal tracts, acting as a muscle tone excitatory system [28-30]. Then we focus on the inputs of the forebrain structures to the midbrain MLR/PPN area. In decerebrate cats, the basal ganglia control locomotion and posture using different GABAergic output pathways of the substantia nigra reticulata (SNr); the lateral part of the SNr blocks the PPN-induced muscle tone suppression, whereas the medial part of the SNr suppresses the MLR-induced locomotion [18,20,31]. Recent rat studies confirm that inhibitory input from the SNc (GABAergic and dopaminergic) to ventral MLR regulate posture, while inhibitory projection from the GABAergic SNr to the dorsal MLR regulates locomotion [21]. In Parkinson’s disease (PD), GABAergic outputs of the basal ganglia are abnormally increased [7], so excessive SNr-inhibition of the MLR may cause gait disturbance and muscle rigidity [5,18].
However, it is unknown whether these mechanisms are the same for bipedal humans and quadrupedal animals. It is also unclear what drives or dictates the SNr-induced control of movements. There are sub-compartments in the basal ganglia; neostriatum-dorsal pallidal pathway (“dorsal pathway”, Figure 4A) and ventral striatum-ventral pallidal pathway (“ventral pathway”, Figure 4B). The nucleus accumbens, as a component of the limbic system, may be important in releasing locomotion, via GABAergic projections disinhibiting the MLR via the ventral pallidum [32,33] and via fibers to the SNr (Figure 4B) [34]. Because the nucleus accumbens also receives inputs from the hippocampus and amygdala, the ventral pathway may be implicated in reward-oriented locomotor behaviors, as it receives inputs from ventral tegmental area, hippocampus and amygdala. On the other hand, the more recently evolved parts of the basal ganglia make up the dorsal system (Figure 4A) [35]. These parts may achieve locomotor control depending on cognitive behavioral context, such as sensoryguided locomotor control.
Figure 4.
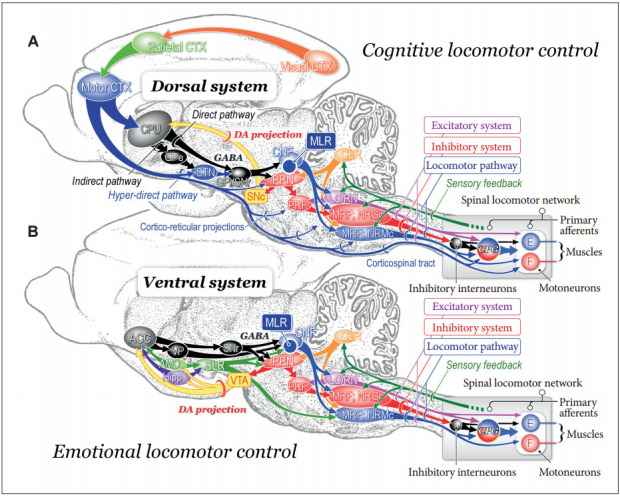
Neuronal mechanisms of cognitive (A) and emotional (B) control of locomotion in the cat. A: Dorsal system for cognitive locomotor control. A visuo-motor pathway from the visual cortex to motor cortex via the parietal cortex contributes to this control. Corticofugal projections act on to the basal ganglia nuclei, brainstem and spinal cord. Dopaminergic projection from the substantia nigra pars compacta (SNc) to the caudate-putamen (CPu) may be involved in learning the locomotor behaviors. GABAergic output from the basal ganglia nuclei (internal segment of the globus pallidus and substantia nigra pars reticulata; GPi/SNr) acts on MLR/PPN area may control locomotion and posture. Efferents from the midbrain locomotor region (MLR) recruit excitatory system, inhibitory system and locomotor pathway. The excitatory system arises from the LC and the raphe nuclei. The inhibitory system which arises from cholinergic neurons in the PPN sequentially activates PRF neurons, medullary reticulospinal neurons in the nucleus reticularis gigantocellularis (NRGc) and spinal inhibitory interneurons. The inhibitory interneurons may inhibit both motoneurons and interneurons. The locomotor pathway consists of reticulospinal neurons arising from the ventromedial medulla corresponding to the nucleus reticularis magnocellularis (NRMc). Cholinergic and glutamatergic projections from the PPN excite SNc-DA neurons. These descending tracts act on CPGs in spinal cord so that muscle tone and locomotion are regulated. Efferents from the (CLR may excite locomotor pathway. B: Ventral system for emotional locomotor control. Efferents from the amygdala (AMD) and hippocampus (Hipp) project to the nucleus accumbens (NAc). GABAergic NAc neurons project to ventral pallidum (VP) and the SNr, which control activity of the MLR/PPN neurons. Efferents from the AMD and the Hipp also act on lateral hypothalamic area, which corresponds to the SLR. DA projections from the ventral tegmental area (VTA) may contribute to the rewardoriented locomotor behaviors. Modified from Snijders et al. Ann Neurol 2016;80:644-659, with permission of Wiley [164]. E: extensor motoneurons, F: flexor motoneurons, PRF: pontine reticular formation, PPN: pedunculopontine tegmental nucleus, LC: locus coeruleus, RN: raphe nuclei, DA: dopamine, CLR: cerebellar locomotor region, SLR: subthalamic locomotor region, CNF: cuneiform nucleus, CTX: cortex, GPe: external segment of the globus pallidus.
Spinal control of posture and gait
Spinal circuitry involved in the stretch reflex, reciprocal inhibition, non-reciprocal inhibition (or autogenic inhibition) and flexion reflexes are involved in the control of posture. Particularly, stretch reflex and non-reciprocal inhibition (Ib inhibition) play major role in static control of posture. On the other hand, interneuronal networks involved in reciprocal Ia inhibition and flexion reflexes including crossed-extension reflex and are critical to produce postural figures with extension-flexion movements of left-right leg alternation during walking. Integration of all spinal reflex networks therefore can be essential to full execution of muscle tone regulation during movement. While spinal reflex networks generate rhythm and pattern of locomotor movements through the activation of the CPG, they play crucial role in supporting body during stance phase of locomotion as well. Because spinal preparations in quadruped animals do not express postural reflex described above, neural networks within the spinal cord alone does not enable to control postural equilibrium [36,37], and integration of descending supraspinal signals and peripheral sensory afferents at the level of spinal cord is necessary for full execution of postural control.
Organization of the spinal locomotor network
Once animals start locomotion, muscle tone must be regulated depending on locomotor cycles. A particular group of spinal interneuronal networks that generates rhythmic activity in the absence of rhythmic inputs is termed CPG [1,36,37]. The rhythmic interneuronal activity is sent to the second-order interneurons in the intermediate region (lamina IV-VII of Rexed), which shape “locomotor patterns” of each limb’s movements [26,38]. The signals are then transmitted to the target motoneurons innervating ipsilateral limb muscles through their excitatory and inhibitory actions [26,36]. Reciprocal Ia interneurons, classical Ib interneurons and Renshaw cells are likely included in this group [36]. On the other hand, lamina VIII interneurons projecting to the contralateral side contribute to the left-right alternations of limb movements [39,40]. The rhythm and pattern are transmitted back to the supraspinal structures via the spinothalamic, spinoreticular and spinocerebellar tracts so that the supraspinal structures monitor all events in the spinal cord [36].
Spinal control of muscle tone during locomotion
Activity of the spinal locomotor networks is modulated by sensory afferents in a phase dependent manner [36,38,41,42]. For example, proprioceptors in muscles at the hip joint are primarily responsible for regulating the stance phase. Afferents from proprioceptors in extensor muscles regulate transition from stance to swing phase. It should be critically noted that signals in Ib afferents from tendon organ in ankle extensor muscles inhibit homonymous motoneurons at rest, while they excite extensor motoneurons during stance phase [36,41]. The functional consequence of this “reflex reversal” is that the swing phase is not initiated until the extensor muscles are unloaded and the forces exerted by these muscles are low.
Skin afferents also exert a powerful influence on the CPG [26,36,41]. Skin receptors are important to detect obstacles and adjust stepping to avoid them such as the “stumble-corrective reaction [43]. Importantly, the corrective flexion movements are produced only if the paw is stimulated during the swing phase. An identical stimulus applied during stance phase elicits the opposite response, an excitation of extensor muscles that reinforces the ongoing extensor activity. This is another example of the reflex reversal. The reflex reversal phenomenon is critically involved in postural control during locomotion. However, its mechanisms have not been elucidated.
HIGHER-ORDER REGULATION OF POSTURE-GAIT CONTROL
Classical lesion studies in the cat
Even cerebral cortex was removed, the kitten can alive more than several years [44]. They could eat and exhibit periods of rest, become active, search for fool, and were able to remember the location of food. They utilized the visual and haptic senses with respect to external space. However, in the adult cats, skilled locomotor performance was disturbed when lesions were made in the motor-related cortical regions [45]. If the caudate nucleus of the cat is selectively removed both sides [46], a remarkable behavior develops referred to as the “compulsory approaching syndrome”. The cat faithfully followed any moving object that catches its attention, seemingly unable to terminate the locomotor behavior. This was referred to as “visually-determined cortical automatism [47]”. The main manifestations consisted of loss of drive (apathy), obsessive-compulsive behavior, cognitive deficits, stimulus-bound perseverative behavior, and hyperactivity [46]. On the other hand, removal of both the cerebral cortex and the striatum (diencephalic cat; the thalamus and hypothalamus were preserved) resulted in the cats walking incessantly, even though they did not attend to any environmental stimuli [48].
Forebrain structure including the cerebral cortex, the limbic-hypothalamic structures, and the basal ganglia as well as the cerebellum control posture and gait largely by acting on the reticulospinal system through their direct and indirect connections via the MLR/PPN area (Figure 4). These cortical and subcortical projections may enable animals to express volitional and emotional motor behaviors depending on the context [2,14].
Control by the cerebral cortex
While basic locomotor synergy was not largely disturbed if pyramidal tracts were bilaterally disconnected [49], skilled locomotor task was severely impaired. Liddell and Phillips [50] found after unilateral or bilateral pyramidal lesions that the cats became ‘helplessly immobile’, unable to take a step without slipping or falling, when they were required to walk along a narrow beam or horizontal ladder. Such a skilled performance became more severely damaged by postcruciate than by precruciate lesions. After postcruciate lesions including both the somatosensory and parietal cortices, the cat refused to walk on narrow trucks [45]. The precruciate area, which corresponds to supplementary motor area (SMA) and premotor area (PM) of the primates, may be involved in movement initiation. On the other hand, the postcruciate cortices may utilize specific somatosensory inputs to fulfil a role in the regulation of ongoing movements [51] in the manner of anticipatory or feed-forward adjustments [52]. Skilled posture-gait control, therefore, can be achieved on the basis of knowledges of the orientation and motion of the body in space as well as motion perception and spatial localization of objects in extra-personal space [53-55]. Such a knowledge is provided by integration of vestibular, somatosensory and visual sensory signals which occurs at both the cerebral cortex and cerebellum (Figure 5A) [56].
Figure 5.
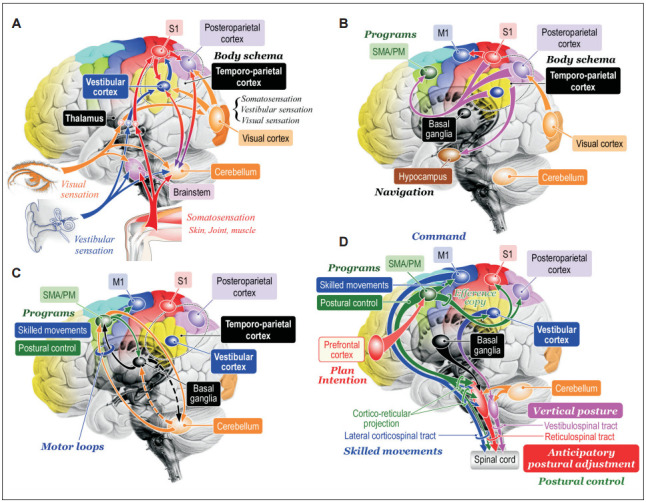
Hypotheses of cognitive process of posture-gait control. A: Cognition of bodily information. Sensory signals flowing into the central nervous system converge to the brainstem, cerebellum, thalamus, and cerebral cortex. At the level of cerebral cortex, signals from the visual cortex, vestibular cortex and primary sensory cortex (S1) is integrated and internal model of self-body, such as body schema and verticality can be constructed at the temporoparietal cortex including the vestibular cortex and posteroparietal cortex. Reciprocal connection between the temporoparietal cortex and cerebellum may contribute to this process. B: Transmission of the bodily information. The bodil y information is then transmitted to the supplementary motor area (SMA) and premotor area (PM) where the information can be utilized as materials to produce motor programs. Similarly, the information is transferred to hippocampus and is used to navigate further behaviors. C: Motor programming. The motor cortical areas closely cooperate with the basal ganglia and cerebellum so that appropriate motor programs are constructed. D: Postural control by corticofugal projections to the brainstem and spinal cord. The bodily information generated at the vestibular cortex may be utilized for sustention of vertical posture via cortico-vestibular and vestibulospinal tract. Signals from the prefrontal cortex including plans and intentions may trigger to run motor programs in the SMA/PM, which may include those for purposeful movements and associating postural control. The postural control program may be utilized to generate anticipatory postural adjustment via cortico-reticular and reticulospinal tract. Then motor programs are sent to the M1 so that goal-directed purposeful skilled movements can be achieved. Modified from http://dx.doi.org/10.1080/01691864.2016.1252690, with permisson of Taylor & Francis [165].
Precise visuomotor coordination occurred at the cerebral cortex plays critical roles in the execution of precise arm-hand movements such as reaching and grasping [57]. Similarly, when a walking subject encounters obstacles, each leg must be placed with a high degree of accuracy through the visuo-parieto-frontal cortical projection, as in the subject has to modify the leg trajectory in each step in order to achieve appropriate foot placement [58]. Such a visuomotor coordination is particularly necessary in quadrupeds because an obstacle is no longer within the visual field by the time the hindlimbs are stepping over it. When the posterior parietal cortex was bilaterally removed, the cat’s hindlimbs did not step over the obstacles if their forelimbs cleared them [59]. Therefore, the posterior parietal cortex must be engaged to register and store the temporospatial relationship between the obstacle and one’s bodily information, such as body schema, in short-term memory that is utilized to produce motor programs in the motor cortices (Figure 5B) so that the cat can precisely modify the limb trajectory [59,60]. To successfully achieve such an accurate control of limb movements during walking, posture must be optimized in advance to the purposeful action so that bodily equilibrium can be maintained. Therefore, the visuo-parieto-frontal cortical projection (Figure 5B) is critically involved in the fulfilment of ongoing purposeful control via anticipatory adjustments of posture [61]. It follows that both the intentional limb movements and anticipatory postural adjustment are programmed at motor cortical areas (Figure 5B and D).
Anticipatory postural adjustment
Then, what part of the motor cortex contributes to the programming of the anticipatory postural adjustments? One of the most candidate areas is the SMA and PM (Figure 5B and C). In bipedal walking monkey, an inactivation of the leg area of the primary motor cortex (M1) by injecting muscimol (GABAA agonist) partly paralyzed the contralateral leg [62]. On the other hand, muscimol injections into the trunk/leg regions of the bilateral SMA largely disturbed postural control without inducing paralysis [63]. When it was injected into the dorsal PM, spontaneous walking was maintained; however, the monkey could not start walking using sensory cue. These findings indicate the SMA and PM may contribute to postural control during bipedal walking and initiation of gait, respectively.
Studies using neural tracers have demonstrated abundant cortico-fugal projections to the PMRF from the premotor cortices (SMA/PM) in quadruped [64] and biped [65] animals. Recent studies have focused onto the importance of cortico-pedunculopontine projection in terms of motor control. Probabilistic diffusion tractography in rhesus monkey as well as humans, shows that the SMA is strongly connected to the lateral PPN, while the dorsal PM is connected to the medial PPN [66]. The RST innervates whole spinal segments [22] so that it controls postural muscle tone and symmetric postural figures (Figure 3) [15]. Therefore, the cortico-reticular and RST may achieve anticipatory postural adjustment (Figure 5D) Possibly, the SMA contributes to the anticipatory postural adjustment for step initiation, which is impaired in PD patients [67]. On the other hand, the PM/SMA may forward programs of precise leg-foot movement to the M1 [68], which, in turn, sends motor command via the corticospinal tract.
Consequently, cognitive information in the temporoparietal cortex is essential for accurate gait control particularly when the subject encounters an unfamiliar environment. Therefore, the deficiency in the information processing from the temporoparietal cortex to the frontal cortex (frontoparietal network) may cause errors in anticipatory postural adjustment and gait difficulties such as the “freezing of gait”. It follows that deficits in cognitive function in elder persons and in patients with Alzheimer’s disease are at higher risk of falling particularly when more cognitive tasks are required [69,70].
Maintenance of vertical posture
Next critical question as to the cortical control of posture is “how does the brain acquire access to an internal estimate of body motion and postural verticality?” Postural vertical is supported by a sense of verticality which is synthesized by visual, somatosensory and vestibular information [71-75]. Among them, the vestibular sensation is superior to others in terms of absoluteness of sensation because it always refers the gravity [76], and the vestibular system provides the brain with sensory signals about three-dimensional head rotations and translations. Vestibulothalamic projections are bilateral and mainly involve the posterior thalamus [77-79]. While there was no cortical area that receives inputs exclusively from vestibular afferents, there are multiple presentations of vestibular information in the cerebral cortex [80], such as the frontal eye field, PM, somatosensory cortex, ventral intraparietal cortex, medial superior temporal area, and parieto-insular vestibular cortex (PIVC). The PIVC has particularly dense connections with other vestibular-relating cortical areas, and receives information from other sensory modalities [81-83]. Now, both the posterior thalamus and PIVC are areas of interest for the internal model of postural verticality [84-88]. Because the PIVC has descending projections to the contralateral vestibular nuclei [79,89-91], the vestibular cortical systems possibly contribute to upright standing by acting to the vestibulospinal system based on the internal model of postural verticality (Figure 5B).
Postural verticality is often disturbed in pathological conditions such as “pusher syndrome” after stroke and “Pisa syndrome” in advanced PD. Stroke patients with pusher syndrome actively push away from the ipsilesional side and have a tendency to fall towards their paretic, contralesional side (the left side for right-hemisphere patients). They had lesions including the parietal insular cortex or posterior thalamus [84,87,88,92]. This phenomenon is more prominent when patients are upright compared to when lying down. Now the pusher phenomenon can be arising from a conflict or mismatch between visual and postural vertical [84,87,88]. However, it is still uncertain whether the same pathophysiological mechanism is operating in Pisa syndrome.
Posture-gait control by the cerebellum
Postural control by the cerebellum highly depends on sensory afferents. Signals from the labyrinth ascend the vestibular nerve to the floccules and vermis of the cerebellum in addition to the vestibular nuclei. The fastigial nuclei (FN) receive a copy of the output of the spinal cord in addition to peripheral sensory information via spinocerebellar tracts [93]. The FN also receive visual [94] and vestibular [95] information. These multisensory features may provide “an error-correction mechanism”, which permits FN neurons to affect motor functions such as coordinating postural responses during walking which entail changes in limb position. The FN may therefore send highly integrated bodily information to the posture-gait related areas in the brainstem and motor cortical areas [96].
Action on the brainstem structures
Output from the FN to the brainstem contributes to the control of postural muscle tone. Electrical stimulation applied to the mid-part of the cerebellar white matter in decerebrate cats either increased [97] or reduced the level of muscle tone [98]. The cerebellar stimulation possibly activated the excitatory RST and VST of both sides so that extensor muscle tone was bilaterally increased. On the other hand, the decrease in the level of muscle tone is considered to be due to withdrawal of excitatory influence upon motoneurons [98]. Because, postural muscle tone is generally reduced by the damage of the medial part of the cerebellum, the cerebellum contributes to the activation of antigravity muscles. Possibly, the FN regulates posture-gait subprograms in the brainstem and spinal cord by inparallel activation of fastigio-spinal, fastigio-reticular, and fastigio-vestibular pathways [27,99,100]. Therefore, the deficiency in these pathways may reduce the degree of α–γ linkage in patients with cerebellar diseases, resulting in hypotonia. The hypotonia state reduces the accuracy of the sensory feedback so that posture-gait control can be seriously disturbed.
Cerebellar actions on the cerebral cortex
Reciprocal connections between the cerebellum and cerebral cortex (Figure 5C) may be critically involved in the cognitive and programing processes of postural control. More recently, it has been recognized that cerebellar output reaches vast areas of the cerebral cortex including prefrontal and posterior parietal cortices in addition to motor-related areas [101]. The FN in the cerebellum, as well as the vestibular cortex (PIVC), is critically involved in encoding internal postural model in space and self-motion [56]. Some studies have suggested the presence of FN projections to the parietal cortex [102,103], motor cortex and multimodal visual areas [104]. Reciprocal connection between parietal cortex and the cerebellum may be involved in perception of body motion in space (Figure 5B). Such a bodily information can be utilized to maintain upright posture during standing and to achieve anticipatory postural adjustment. The latter may involve reciprocal connections between the motor cortical area (SMA/PM) and cerebellum (motor loop) in order to construct motor programs (Figure 5C) [105,106]. Accordingly, cerebellar disease patients may have problems in cognitive process of postural control. However, the perception of verticality in patients with cerebellar ataxia may only deteriorate in a more advanced stage of the disease [107]. In addition, only few abnormalities of anticipatory postural adjustment were found in the cerebellar disease patients compared to controls, while the patients appeared to be less able to use predictive information [108]. Because the cerebellum is reciprocally connected with the basal ganglia [109], it is possible that basal ganglia in addition to the cerebral cortex may complement the cerebellar role of cognitive process of postural control.
Posture-gait control by the basal ganglia in relation to PD
Because posture-gait control is seriously impaired in PD, the basal ganglia has long been functionally regarded to be predominantly involved in motor control but is increasingly recognized to play additional roles in sensory processing, cognition, and behavior [110-112]. Here, emphasis has been placed on the mechanisms of posture-gait impairment in PD so that understanding the role of basal ganglia to the postural control is facilitated. Based on our recent understanding, postural disturbances in PD attribute to following mechanisms: 1) disturbances in the dopaminergic and cholinergic systems, 2) impairment of cognitive functions due to failure of integrative sensory processing that allows to produce internal postural model (body schema), 3) failure in motor programming due to reduced activity in the motor cortical areas, and 4) disturbances in posture-gait areas in the brainstem [15,18,113].
Disturbances in the dopaminergic and cholinergic systems
Recent clinical studies suggest that the postural impairments in PD is based on dysfunction of both the dopaminergic and cholinergic systems. Disturbances in these chemospecific systems may critically contribute to posture-gait failure in this disease. For example, a damage of dopamine (DA) neurons in the substantia nigra pars compacta (SNc), which project to the basal ganglia nuclei, is considered to increase in the GABAergic inhibitory output from the basal ganglia [7,114,115]. This may strongly inhibit thalamocortical systems and brainstem structures (Figure 1).
In addition, cholinergic neurons in the PPN (brainstem) and basal forebrain (BF) are seriously damaged in PD [116-119]. Indeed, a reduction of the thalamic cholinergic innervation in patients with PD has no cognitive and motor impairments but exhibits an increase in postural sway speed [120]. Cholinergic PPN neurons project to the non-specific thalamocortical system [121-123], basal ganglia nuclei including DA neurons in the SNc and PMRF [124-126]. On the other hand, cholinergic BF projections to the cerebral cortex are necessary for attentional performance and cognitive processing [127].
Therefore, disturbances in attention, sensori-motor integration and cognitive processing in PD can be largely attributed to the damage of the cholinergic systems. Accordingly, both of the excessive inhibition from the basal ganglia and the damage of cholinergic systems may impair both the cortical and subcortical, particularly the brainstem, functions.
Impairments in sensory processing and cognition
Cortical activity was substantially reduced in patients in PD compared control subject during walking [128,129]. This may cause failure of integrative sensory processing, which in turn, disturb construction internal postural model and motor programming. It has been shown that a loss of cholinergic neurons in the BF and PPN associates with fallers in PD [116,130]. Müller and Bohnen [131] suggested that reduced activities in the cholinergic PPN neurons may disturb multi-sensory integration at the level of the thalamus. This may also explain why patients in PD with more severe posture-gait instability have a high risk of developing dementia [131]. Impairment of the integration of sensory information, particularly proprioception [132] and vestibular graviception [133], may result in deficits of internal model of postural verticality which is possibly constructed at the temporoparietal association area including the vestibular cortex. Therefore, asymmetry in the activity of the left and right vestibular cortices may induce leaning upright posture, which is often called as Pisa syndrome. Pisa syndrome is a dystonic lateroflexion of the trunk with a postural disturbance resembling the leaning tower of Pisa, and is more often observed in patients with advanced PD [134]. The marked lateroflexion become worsen during walking but is almost completely alleviated by passive mobilization or supine positioning [135]. Because PD without Pisa syndrome also had deficiencies in postural verticality compared to healthy controls [132,136-138], mismatch between proprioception and vestibular gravitation in PD may alter subjective postural verticality, resulting in Pisa syndrome. Alternatively, asymmetry of the basal ganglia output, which is due to cholinergic-dopaminergic imbalance in the striatum [134,139,140] or disturbance of the pallidal output [141,142], may also elicit left-right disproportion of the thalamocortical processing of vestibular information.
Failure in motor programming
The motor cortical areas including the M1, SMA, and PM have connections with the basal ganglia and cerebellum, constituting motor loop that contributes to execution and motor programming of voluntary movements (Figure 5C) [105,106]. Because of increasing inhibitory output from the basal ganglia to the thalamocortical projections in addition to reduced cognitive information processing, the capability of producing motor programs in response to changes in circumstance can be deteriorated. In fact, the SMA contributes to the anticipatory postural adjustment for step initiation via corticofugal projections to the PPN and PMRF, and this process is seriously impaired in PD patients [67]. Also, the dorsal part of the PM is involved in sensory-guided gait control as suggested in bipedally walking monkey [62]. Because the activity of dorsal part of the PM was increased during visually-guided paradoxical gait in PD, posture-gait programs in SMA/PM became reusable by the activation of visuo-motor pathway [129]. Accordingly, failure in motor programming in PD can be due to the decrease in excitability of the motor cortical areas in addition to impairment of sensory processing in the temporoparietal cortices. Recently, role of the cerebellum in the pathophysiology of PD is highly recognized [143,144]. Because the cerebellum has reciprocal connections with the basal ganglia (Figure 5C) in addition to the cerebral cortex and brainstem, there is a need to elucidate whether the cerebellum participates in compensatory mechanisms associated with the disease or contributes to the pathophysiology of PD.
Reduced activity in posture-gait area in the midbrain
We propose that reduced excitability in the mesopontine tegmentum including the PPN/MLR can be also involved in posture-gait failure in PD [6,15,18,20,113]. In decerebrate cats, the basal ganglia control locomotion and posture using different GABAergic output pathways of the SNr; the lateral part of the SNr blocks the PPN-induced muscle tone suppression, whereas the medial part of the SNr suppresses the MLR-induced locomotion [18]. Recent studies in rodents confirm that inhibitory input from the SNr to the glutamatergic neurons in the MLR regulates locomotion [21,145]. In PD, GABAergic outputs of the basal ganglia are abnormally increased [7,114], so excessive SNr-inhibition of the MLR may cause gait disturbance and muscle rigidity acting on MLR and muscle tone inhibitory region in the PPN [18]. Muscle tone rigidity in PD is called as “lead-pipe like rigidity” which is characterized by co-contraction of extensor and flexor muscles. Such a co-contraction is observed in neck, back and leg muscles, resulting in flexion posture including camptocormia [146].
PD patients with cholinergic cell loss in the PPN showed more severe motor disabilities with gait and posture, which were associated with L-3,4-dihydroxyphenylalanine (L-DOPA)-resistant akinesia [147,148]. Subsequent post-mortem study in PD patients established a correlation between the occurrence of falls and freezing and the loss of cholinergic PPN neurons. However, the degree of neuronal loss in the CNF was not significantly different between fallers and non-fallers in PD patients [147]. In PD patients, individual neurons in the dorsal PPN increased their firing rates with increased stepping frequency [149]. Moreover, gait speed in PD patients was correlated with a power of alpha-oscillations (7–10 Hz) of field potentials recorded from the PPN area [150].
As one of clinical procedures for alleviating gaitposture deficiency in PD, deep brain stimulation (DBS) targeting the PPN with the aim of stimulating remaining cholinergic neurons [151-155]. The first studies using DBS in advanced PD patients concluded that low-frequency stimulation of the PPN could be effective to control freezing of gait and falls. However, further clinical studies concluded that freezing of gait were mildly improved by PPN-DBS but some results were rather disappointing [156,157]. These results emphasize the need to determine the optimal surgical target [158,159]. Ferraye et al. [156] suggest that the most suitable targets are located slightly posterior to the PPN pars compacta, probably in the ventral part of the CNF where stimulation-induced locomotion has been reported in animals [18]. This area possibly corresponds to the subcuneiform nucleus as described by Alam et al. [160] and Karachi et al. [161] also suggest that it may be the case that treating PD patients suffering from failure of gait initiation versus falling may require specifically targeting the CNF and the dorsal part of the PPN, respectively.
Reorganization of cortico-cerebello-brainstem pathways in PD
In human, Fling et al. [162] used functional neuroimaging approach and revealed strong functional connectivity between the SMA and PPN/MLR area, which was positively correlated with freezing severity in patients of PD. In contrast, connectivity between the STN and SMA was lost. They suggested that the former connectivity may potentially due to a maladaptive compensation, and the latter may reflect the reduced automatic control of gait by the basal ganglia. A study using diffusion tensor imaging revealed the connection between the cerebellum and the PPN in PD patients without freezing of gait. However, freezers of patients in PD showed the absence of cerebellotegmental connectivity and increased visibility of the decussation of corticopontine fibers in the anterior pons [163]. These findings highlight the importance of corticopontine-cerebellar pathways in the pathophysiology of gait when the cerebellotegmental connection that may contribute to automatic execution of gait control is damaged in freezers of PD.
Acknowledgments
This work is partially supported by grants from JSPS KAKENHI (Grant Numbers 26120004 and 25290001) and from Japan Agency for Medical Research and Development (AMED) for K.T. KT is also supported by granting foundations from the QOLER Medical Group and Sasson Hospital.
Footnotes
Conflicts of Interest
The author has no financial conflicts of interest.
REFERENCES
- 1.Grillner S. In: Handbook of physiology. The nervous system II. Brookhart JM, Mountcastle VB, editors. Bethesda, MD: American Physiological Society; 1981. Control of locomotion in bipeds, tetrapods, and fish; pp. 1179–1236. [Google Scholar]
- 2.Takakusaki K. Forebrain control of locomotor behaviors. Brain Res Rev. 2008;57:192–198. doi: 10.1016/j.brainresrev.2007.06.024. [DOI] [PubMed] [Google Scholar]
- 3.Sinnamon HM. Preoptic and hypothalamic neurons and the initiation of locomotion in the anesthetized rat. Prog Neurobiol. 1993;41:323–344. doi: 10.1016/0301-0082(93)90003-b. [DOI] [PubMed] [Google Scholar]
- 4.Takakusaki K, Takahashi K, Saitoh K, Harada H, Okumura T, Kayama Y, et al. Orexinergic projections to the cat midbrain mediate alternation of emotional behavioural states from locomotion to cataplexy. J Physiol. 2005;568(Pt 3):1003–1020. doi: 10.1113/jphysiol.2005.085829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Takakusaki K, Tomita N, Yano M. Substrates for normal gait and pathophysiology of gait disturbances with respect to the basal ganglia dysfunction. J Neurol. 2008;255 Suppl 4:19–29. doi: 10.1007/s00415-008-4004-7. [DOI] [PubMed] [Google Scholar]
- 6.Takakusaki K. Neurophysiology of gait: from the spinal cord to the frontal lobe. Mov Disord. 2013;28:1483–1491. doi: 10.1002/mds.25669. [DOI] [PubMed] [Google Scholar]
- 7.DeLong MR, Wichmann T. Circuits and circuit disorders of the basal ganglia. Arch Neurol. 2007;64:20–24. doi: 10.1001/archneur.64.1.20. [DOI] [PubMed] [Google Scholar]
- 8.Armstrong DM. Supraspinal contributions to the initiation and control of locomotion in the cat. Prog Neurobiol. 1986;26:273–361. doi: 10.1016/0301-0082(86)90021-3. [DOI] [PubMed] [Google Scholar]
- 9.Mori S. Integration of posture and locomotion in acute decerebrate cats and in awake, freely moving cats. Prog Neurobiol. 1987;28:161–195. doi: 10.1016/0301-0082(87)90010-4. [DOI] [PubMed] [Google Scholar]
- 10.Hinsey JC, Ranson SW, McNattin RF. The role of the hypothalamus and mesencephalon in locomotion. Arch NeurPsych. 1930;23:1–43. [Google Scholar]
- 11.Shik ML, Orlovsky GN. Neurophysiology of locomotor automatism. Physiol Rev. 1976;56:465–501. doi: 10.1152/physrev.1976.56.3.465. [DOI] [PubMed] [Google Scholar]
- 12.Mori S, Matsui T, Kuze B, Asanome M, Nakajima K, Matsuyama K. Stimulation of a restricted region in the midline cerebellar white matter evokes coordinated quadrupedal locomotion in the decerebrate cat. J Neurophysiol. 1999;82:290–300. doi: 10.1152/jn.1999.82.1.290. [DOI] [PubMed] [Google Scholar]
- 13.Jahn K, Deutschländer A, Stephan T, Kalla R, Wiesmann M, Strupp M, et al. Imaging human supraspinal locomotor centers in brainstem and cerebellum. Neuroimage. 2008;39:786–792. doi: 10.1016/j.neuroimage.2007.09.047. [DOI] [PubMed] [Google Scholar]
- 14.Grillner S, Georgopoulos AP, Jordan LM. In: Neurons, networks, and motor behavior. Stein PSG, Grillner S, Selverston AI, Stuart DG, editors. Cambridge, MA: The MIT Press; 1997. Selection and initiation of motor behavior; pp. 3–19. [Google Scholar]
- 15.Takakusaki K, Chiba R, Nozu T, Okumura T. Brainstem control of locomotion and muscle tone with special reference to the role of the mesopontine tegmentum and medullary reticulospinal systems. J Neural Transm (Vienna) 2016;123:695–729. doi: 10.1007/s00702-015-1475-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mena-Segovia J. Structural and functional considerations of the cholinergic brainstem. J Neural Transm (Vienna) 2016;123:731–736. doi: 10.1007/s00702-016-1530-9. [DOI] [PubMed] [Google Scholar]
- 17.Petzold A, Valencia M, Pál B, Mena-Segovia J. Decoding brain state transitions in the pedunculopontine nucleus: cooperative phasic and tonic mechanisms. Front Neural Circuits. 2015;9:68. doi: 10.3389/fncir.2015.00068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Takakusaki K, Habaguchi T, Ohtinata-Sugimoto J, Saitoh K, Sakamoto T. Basal ganglia efferents to the brainstem centers controlling postural muscle tone and locomotion: a new concept for understanding motor disorders in basal ganglia dysfunction. Neuroscience. 2003;119:293–308. doi: 10.1016/s0306-4522(03)00095-2. [DOI] [PubMed] [Google Scholar]
- 19.Takakusaki K, Habaguchi T, Saitoh K, Kohyama J. Changes in the excitability of hindlimb motoneurons during muscular atonia induced by stimulating the pedunculopontine tegmental nucleus in cats. Neuroscience. 2004;124:467–480. doi: 10.1016/j.neuroscience.2003.12.016. [DOI] [PubMed] [Google Scholar]
- 20.Takakusaki K, Obara K, Nozu T, Okumura T. Modulatory effects of the GABAergic basal ganglia neurons on the PPN and the muscle tone inhibitory system in cats. Arch Ital Biol. 2011;149:385–405. doi: 10.4449/aib.v149i4.1383. [DOI] [PubMed] [Google Scholar]
- 21.Sherman D, Fuller PM, Marcus J, Yu J, Zhang P, Chamberlin NL, et al. Anatomical location of the mesencephalic locomotor region and its possible role in locomotion, posture, cataplexy, and parkinsonism. Front Neurol. 2015;6:140. doi: 10.3389/fneur.2015.00140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kuze B, Matsuyama K, Matsui T, Miyata H, Mori S. Segment-specific branching patterns of single vestibulospinal tract axons arising from the lateral vestibular nucleus in the cat: a PHA-L tracing study. J Comp Neurol. 1999;414:80–96. [PubMed] [Google Scholar]
- 23.Matsuyama K, Takakusaki K, Nakajima K, Mori S. Multisegmental innervation of single pontine reticulospinal axons in the cervico-thoracic region of the cat: anterograde PHA-L tracing study. J Comp Neurol. 1997;377:234–250. [PubMed] [Google Scholar]
- 24.Matsuyama K, Drew T. Vestibulospinal and reticulospinal neuronal activity during locomotion in the intact cat. I. Walking on a level surface. J Neurophysiol. 2000;84:2237–2256. doi: 10.1152/jn.2000.84.5.2237. [DOI] [PubMed] [Google Scholar]
- 25.Matsuyama K, Drew T. Vestibulospinal and reticulospinal neuronal activity during locomotion in the intact cat. II. Walking on an inclined plane. J Neurophysiol. 2000;84:2257–2276. doi: 10.1152/jn.2000.84.5.2257. [DOI] [PubMed] [Google Scholar]
- 26.Rossignol S. In: Handbook of physiology, section 12. Exercise: regulation and integration of multiple systems. Rowell LB, Sheperd JT, editors. New York, NY: Oxford University Press; 1996. Neural control of stereotypic limb movements; pp. 173–216. [Google Scholar]
- 27.Mori S, Matsui T, Kuze B, Asanome M, Nakajima K, Matsuyama K. Cerebellar-induced locomotion: reticulospinal control of spinal rhythm generating mechanism in cats. Ann N Y Acad Sci. 1998;860:94–105. doi: 10.1111/j.1749-6632.1998.tb09041.x. [DOI] [PubMed] [Google Scholar]
- 28.Fung SJ, Barnes CD. Evidence of facilitatory coerulospinal action in lumbar motoneurons of cats. Brain Res. 1981;216:299–311. doi: 10.1016/0006-8993(81)90132-3. [DOI] [PubMed] [Google Scholar]
- 29.Mori S, Kawahara K, Sakamoto T, Aoki M, Tomiyama T. Setting and resetting of level of postural muscle tone in decerebrate cat by stimulation of brain stem. J Neurophysiol. 1982;48:737–748. doi: 10.1152/jn.1982.48.3.737. [DOI] [PubMed] [Google Scholar]
- 30.Sakai M, Matsunaga M, Kubota A, Yamanishi Y, Nishizawa Y. Reduction in excessive muscle tone by selective depletion of serotonin in intercollicularly decerebrated rats. Brain Res. 2000;860:104–111. doi: 10.1016/s0006-8993(00)02022-9. [DOI] [PubMed] [Google Scholar]
- 31.Takakusaki K, Saitoh K, Harada H, Okumura T, Sakamoto T. Evidence for a role of basal ganglia in the regulation of rapid eye movement sleep by electrical and chemical stimulation for the pedunculopontine tegmental nucleus and the substantia nigra pars reticulata in decerebrate cats. Neuroscience. 2004;124:207–220. doi: 10.1016/j.neuroscience.2003.10.028. [DOI] [PubMed] [Google Scholar]
- 32.Sławińska U, Kasicki S. Theta-like rhythm in depth EEG activity of hypothalamic areas during spontaneous or electrically induced locomotion in the rat. Brain Res. 1995;678:117–126. doi: 10.1016/0006-8993(95)00174-o. [DOI] [PubMed] [Google Scholar]
- 33.Swanson LW, Mogenson GJ. Neural mechanisms for the functional coupling of autonomic, endocrine and somatomotor responses in adaptive behavior. Brain Res. 1981;228:1–34. doi: 10.1016/0165-0173(81)90010-2. [DOI] [PubMed] [Google Scholar]
- 34.Lynd-Balta E, Haber SN. Primate striatonigral projections: a comparison of the sensorimotor-related striatum and the ventral striatum. J Comp Neurol. 1994;345:562–578. doi: 10.1002/cne.903450407. [DOI] [PubMed] [Google Scholar]
- 35.Robertson B, Kardamakis A, Capantini L, Pérez-Fernández J, Suryanarayana SM, Wallén P, et al. The lamprey blueprint of the mammalian nervous system. Prog Brain Res. 2014;212:337–349. doi: 10.1016/B978-0-444-63488-7.00016-1. [DOI] [PubMed] [Google Scholar]
- 36.Rossignol S, Dubuc R, Gossard JP. Dynamic sensorimotor interactions in locomotion. Physiol Rev. 2006;86:89–154. doi: 10.1152/physrev.00028.2005. [DOI] [PubMed] [Google Scholar]
- 37.Rossignol S, Barrière G, Frigon A, Barthélemy D, Bouyer L, Provencher J, et al. Plasticity of locomotor sensorimotor interactions after peripheral and/or spinal lesions. Brain Res Rev. 2008;57:228–240. doi: 10.1016/j.brainresrev.2007.06.019. [DOI] [PubMed] [Google Scholar]
- 38.McCrea DA, Rybak IA. Organization of mammalian locomotor rhythm and pattern generation. Brain Res Rev. 2008;57:134–46. doi: 10.1016/j.brainresrev.2007.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jankowska E. Interneuronal relay in spinal pathways from proprioceptors. Prog Neurobiol. 1992;38:335–378. doi: 10.1016/0301-0082(92)90024-9. [DOI] [PubMed] [Google Scholar]
- 40.Matsuyama K, Takakusaki K. In: Handbook on White Matter: Structure, Function and Changes. Westland TB, Calton RN, editors. New York, NY: Nova Science Publishing; 2009. Organizing principles of axonal projections of the long descending reticulospinal pathway and its target spinal lamina VIII commissural neurons: with special reference to the locomotor function; pp. 335–356. [Google Scholar]
- 41.Pearson KG. Generating the walking gait: role of sensory feedback. Prog Brain Res. 2004;143:123–129. doi: 10.1016/S0079-6123(03)43012-4. [DOI] [PubMed] [Google Scholar]
- 42.Frigon A, Sirois J, Gossard JP. Effects of ankle and hip muscle afferent inputs on rhythm generation during fictive locomotion. J Neurophysiol. 2010;103:1591–1605. doi: 10.1152/jn.01028.2009. [DOI] [PubMed] [Google Scholar]
- 43.Forssberg H. Stumbling corrective reaction: a phase-dependent compensatory reaction during locomotion. J Neurophysiol. 1979;42:936–953. doi: 10.1152/jn.1979.42.4.936. [DOI] [PubMed] [Google Scholar]
- 44.Bjursten LM, Norrsell K, Norrsell U. Behavioural repertory of cats without cerebral cortex from infancy. Exp Brain Res. 1976;25:115–130. doi: 10.1007/BF00234897. [DOI] [PubMed] [Google Scholar]
- 45.Adkins RJ, Cegnar MR, Rafuse DD. Differential effects of lesions of the anterior and posterior sigmoid gyri in cats. Brain Res. 1971;30:411–414. doi: 10.1016/0006-8993(71)90092-8. [DOI] [PubMed] [Google Scholar]
- 46.Villablanca JR. Why do we have a caudate nucleus? Acta Neurobiol Exp (Wars) 2010;70:95–105. doi: 10.55782/ane-2010-1778. [DOI] [PubMed] [Google Scholar]
- 47.Denny-Brown D. The midbrain and motor integration. Proc R Soc Med. 1962;55:527–538. doi: 10.1177/003591576205500701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Villablanca J, Marcus R. Sleep-wakefulness, EEG and behavioral studies of chronic cats without neocortex and striatum: the ‘diencephalic’ cat. Arch Ital Biol. 1972;110:348–382. [PubMed] [Google Scholar]
- 49.Eidelberg E, Yu J. Effects of corticospinal lesions upon treadmill locomotion by cats. Exp Brain Res. 1981;43:101–103. doi: 10.1007/BF00238815. [DOI] [PubMed] [Google Scholar]
- 50.Liddell EGT, Phillips CG. Pyramidal section in the cat. Brain. 1944;67:1–9. [Google Scholar]
- 51.Brooks VB, Stoney SD., Jr Motor mechanisms: the role of the pyramidal system in motor control. Annu Rev Physiol. 1971;33:337–392. doi: 10.1146/annurev.ph.33.030171.002005. [DOI] [PubMed] [Google Scholar]
- 52.Vicario DS, Martin JH, Ghez C. Specialized subregions in the cat motor cortex: a single unit analysis in the behaving animal. Exp Brain Res. 1983;51:351–367. [Google Scholar]
- 53.Maurer C, Mergner T, Peterka RJ. Multisensory control of human upright stance. Exp Brain Res. 2006;171:231–250. doi: 10.1007/s00221-005-0256-y. [DOI] [PubMed] [Google Scholar]
- 54.Mergner T, Becker W. A modeling approach to the human spatial orientation system. Ann N Y Acad Sci. 2003;1004:303–315. doi: 10.1196/annals.1303.028. [DOI] [PubMed] [Google Scholar]
- 55.Horak FB, Shupert CL, Dietz V, Horstmann G. Vestibular and somatosensory contributions to responses to head and body displacements in stance. Exp Brain Res. 1994;100:93–106. doi: 10.1007/BF00227282. [DOI] [PubMed] [Google Scholar]
- 56.Shaikh AG, Meng H, Angelaki DE. Multiple reference frames for motion in the primate cerebellum. J Neurosci. 2004;24:4491–4497. doi: 10.1523/JNEUROSCI.0109-04.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kravitz DJ, Saleem KS, Baker CI, Mishkin M. A new neural framework for visuospatial processing. Nat Rev Neurosci. 2011;12:217–230. doi: 10.1038/nrn3008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Georgopoulos AP, Grillner S. Visuomotor coordination in reaching and locomotion. Science. 1989;245:1209–1210. doi: 10.1126/science.2675307. [DOI] [PubMed] [Google Scholar]
- 59.Lajoie K, Andujar JE, Pearson K, Drew T. Neurons in area 5 of the posterior parietal cortex in the cat contribute to interlimb coordination during visually guided locomotion: a role in working memory. J Neurophysiol. 2010;103:2234–2254. doi: 10.1152/jn.01100.2009. [DOI] [PubMed] [Google Scholar]
- 60.Marigold DS, Drew T. Contribution of cells in the posterior parietal cortex to the planning of visually guided locomotion in the cat: effects of temporary visual interruption. J Neurophysiol. 2011;105:2457–2470. doi: 10.1152/jn.00992.2010. [DOI] [PubMed] [Google Scholar]
- 61.Massion J. Movement, posture and equilibrium: interaction and coordination. Prog Neurobiol. 1992;38:35–56. doi: 10.1016/0301-0082(92)90034-c. [DOI] [PubMed] [Google Scholar]
- 62.Nakajima K, Mori F, Tachibana A, Nambu A, Mori S. Cortical mechanisms for the control of bipedal locomotion in Japanese monkeys: I. Local inactivation of the primary motor cortex (M1) Neurosci Res. 2003;46(Suppl 1):S156. [Google Scholar]
- 63.Mori F, Nakajima K, Tachibana A, Nambu A, Mori S. Cortical mechanisms for the control of bipedal locomotion in Japanese monkeys: II. Local inactivation of the supplementary motor area (SMA) Neurosci Res. 2003;46(Suppl 1):S157. [Google Scholar]
- 64.Matsuyama K, Drew T. Organization of the projections from the pericruciate cortex to the pontomedullary brainstem of the cat: a study using the anterograde tracer Phaseolus vulgaris-leucoagglutinin. J Comp Neurol. 1997;389:617–641. doi: 10.1002/(sici)1096-9861(19971229)389:4<617::aid-cne6>3.0.co;2-3. [DOI] [PubMed] [Google Scholar]
- 65.Keizer K, Kuypers HG. Distribution of corticospinal neurons with collaterals to the lower brain stem reticular formation in monkey (Macaca fascicularis) Exp Brain Res. 1989;74:311–318. doi: 10.1007/BF00248864. [DOI] [PubMed] [Google Scholar]
- 66.Aravamuthan BR, McNab JA, Miller KL, Rushworth M, Jenkinson N, Stein JF, et al. Cortical and subcortical connections within the pedunculopontine nucleus of the primate Macaca mulatta determined using probabilistic diffusion tractography. J Clin Neurosci. 2009;16:413–420. doi: 10.1016/j.jocn.2008.03.018. [DOI] [PubMed] [Google Scholar]
- 67.Jacobs JV, Lou JS, Kraakevik JA, Horak FB. The supplementary motor area contributes to the timing of the anticipatory postural adjustment during step initiation in participants with and without Parkinson’s disease. Neuroscience. 2009;164:877–885. doi: 10.1016/j.neuroscience.2009.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Hoshi E, Tanji J. Distinctions between dorsal and ventral premotor areas: anatomical connectivity and functional properties. Curr Opin Neurobiol. 2007;17:234–242. doi: 10.1016/j.conb.2007.02.003. [DOI] [PubMed] [Google Scholar]
- 69.Snijders AH, van de Warrenburg BP, Giladi N, Bloem BR. Neurological gait disorders in elderly people: clinical approach and classification. Lancet Neurol. 2007;6:63–74. doi: 10.1016/S1474-4422(06)70678-0. [DOI] [PubMed] [Google Scholar]
- 70.Cohen RG, Nutt JG, Horak FB. Errors in postural preparation lead to increased choice reaction times for step initiation in older adults. J Gerontol A Biol Sci Med Sci. 2011;66:705–713. doi: 10.1093/gerona/glr054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Barbieri G, Gissot AS, Fouque F, Casillas JM, Pozzo T, Pérennou D. Does proprioception contribute to the sense of verticality? Exp Brain Res. 2008;185:545–552. doi: 10.1007/s00221-007-1177-8. [DOI] [PubMed] [Google Scholar]
- 72.Bisdorff AR, Wolsley CJ, Anastasopoulos D, Bronstein AM, Gresty MA. The perception of body verticality (subjective postural vertical) in peripheral and central vestibular disorders. Brain. 1996;119(Pt 5):1523–1534. doi: 10.1093/brain/119.5.1523. [DOI] [PubMed] [Google Scholar]
- 73.Merfeld DM, Zupan L, Peterka RJ. Humans use internal models to estimate gravity and linear acceleration. Nature. 1999;398:615–618. doi: 10.1038/19303. [DOI] [PubMed] [Google Scholar]
- 74.Van Beuzekom AD, Van Gisbergen JA. Properties of the internal representation of gravity inferred from spatial-direction and body-tilt estimates. J Neurophysiol. 2000;84:11–27. doi: 10.1152/jn.2000.84.1.11/F. [DOI] [PubMed] [Google Scholar]
- 75.Pérennou DA, Mazibrada G, Chauvineau V, Greenwood R, Rothwell J, Gresty MA, et al. Lateropulsion, pushing and verticality perception in hemisphere stroke: a causal relationship? Brain. 2008;131(Pt 9):2401–2413. doi: 10.1093/brain/awn170. [DOI] [PubMed] [Google Scholar]
- 76.Lopez C, Falconer CJ, Deroualle D, Mast FW. In the presence of others: self-location, balance control and vestibular processing. Neurophysiol Clin. 2015;45:241–254. doi: 10.1016/j.neucli.2015.09.001. [DOI] [PubMed] [Google Scholar]
- 77.Akbarian S, Grüsser OJ, Guldin WO. Thalamic connections of the vestibular cortical fields in the squirrel monkey (Saimiri sciureus) J Comp Neurol. 1992;326:423–441. doi: 10.1002/cne.903260308. [DOI] [PubMed] [Google Scholar]
- 78.Lopez C, Blanke O. The thalamocortical vestibular system in animals and humans. Brain Res Rev. 2011;67:119–146. doi: 10.1016/j.brainresrev.2010.12.002. [DOI] [PubMed] [Google Scholar]
- 79.Fukushima K. Corticovestibular interactions: anatomy, electrophysiology, and functional considerations. Exp Brain Res. 1997;117:1–16. doi: 10.1007/pl00005786. [DOI] [PubMed] [Google Scholar]
- 80.Faugier-Grimaud S, Ventre J. Anatomic connections of inferior parietal cortex (area 7) with subcortical structures related to vestibulo-ocular function in a monkey (Macaca fascicularis) J Comp Neurol. 1989;280:1–14. doi: 10.1002/cne.902800102. [DOI] [PubMed] [Google Scholar]
- 81.Guldin WO, Grüsser OJ. Is there a vestibular cortex? Trends Neurosci. 1998;21:254–259. doi: 10.1016/s0166-2236(97)01211-3. [DOI] [PubMed] [Google Scholar]
- 82.Brandt T, Dieterich M. The vestibular cortex. Its locations, functions, and disorders. Ann N Y Acad Sci. 1999;871:293–312. doi: 10.1111/j.1749-6632.1999.tb09193.x. [DOI] [PubMed] [Google Scholar]
- 83.Sugiuchi Y, Izawa Y, Ebata S, Shinoda Y. Vestibular cortical area in the periarcuate cortex: its afferent and efferent projections. Ann N Y Acad Sci. 2005;1039:111–123. doi: 10.1196/annals.1325.011. [DOI] [PubMed] [Google Scholar]
- 84.Barra J, Marquer A, Joassin R, Reymond C, Metge L, Chauvineau V, et al. Humans use internal models to construct and update a sense of verticality. Brain. 2010;133(Pt 12):3552–3563. doi: 10.1093/brain/awq311. [DOI] [PubMed] [Google Scholar]
- 85.Maffei V, Mazzarella E, Piras F, Spalletta G, Caltagirone C, Lacquaniti F, et al. Processing of visual gravitational motion in the peri-sylvian cortex: evidence from brain-damaged patients. Cortex. 2016;78:55–69. doi: 10.1016/j.cortex.2016.02.004. [DOI] [PubMed] [Google Scholar]
- 86.Zhang LL, Wang JQ, Qi RR, Pan LL, Li M, Cai YL. Motion sickness: current knowledge and recent advance. CNS Neurosci Ther. 2016;22:15–24. doi: 10.1111/cns.12468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Pérennou D, Piscicelli C, Barbieri G, Jaeger M, Marquer A, Barra J. Measuring verticality perception after stroke: why and how? Neurophysiol Clin. 2014;44:25–32. doi: 10.1016/j.neucli.2013.10.131. [DOI] [PubMed] [Google Scholar]
- 88.Karnath HO, Dieterich M. Spatial neglect--a vestibular disorder? Brain. 2006;129(Pt 2):293–305. doi: 10.1093/brain/awh698. [DOI] [PubMed] [Google Scholar]
- 89.Wilson VJ, Zarzecki P, Schor RH, Isu N, Rose PK, Sato H, et al. Cortical influences on the vestibular nuclei of the cat. Exp Brain Res. 1999;125:1–13. doi: 10.1007/s002210050651. [DOI] [PubMed] [Google Scholar]
- 90.Akbarian S, Grüsser OJ, Guldin WO. Corticofugal connections between the cerebral cortex and brainstem vestibular nuclei in the macaque monkey. J Comp Neurol. 1994;339:421–437. doi: 10.1002/cne.903390309. [DOI] [PubMed] [Google Scholar]
- 91.Akbarian S, Grüsser OJ, Guldin WO. Corticofugal projections to the vestibular nuclei in squirrel monkeys: further evidence of multiple cortical vestibular fields. J Comp Neurol. 1993;332:89–104. doi: 10.1002/cne.903320107. [DOI] [PubMed] [Google Scholar]
- 92.Ticini LF, Klose U, Nägele T, Karnath HO. Perfusion imaging in pusher syndrome to investigate the neural substrates involved in controlling upright body position. PLoS One. 2009;4:e5737. doi: 10.1371/journal.pone.0005737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Stecina K, Fedirchuk B, Hultborn H. Information to cerebellum on spinal motor networks mediated by the dorsal spinocerebellar tract. J Physiol. 2013;591:5433–5443. doi: 10.1113/jphysiol.2012.249110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Büttner U, Glasauer S, Glonti L, Guan Y, Kipiani E, Kleine J, et al. Multimodal signal integration in vestibular neurons of the primate fastigial nucleus. Ann N Y Acad Sci. 2003;1004:241–251. doi: 10.1196/annals.1303.021. [DOI] [PubMed] [Google Scholar]
- 95.McCall AA, Miller DJ, Catanzaro MF, Cotter LA, Yates BJ. Hindlimb movement modulates the activity of rostral fastigial nucleus neurons that process vestibular input. Exp Brain Res. 2015;233:2411–2419. doi: 10.1007/s00221-015-4311-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Cavdar S, Onat FY, Yananli HR, Sehirli US, Tulay C, Saka E, et al. Cerebellar connections to the rostral reticular nucleus of the thalamus in the rat. J Anat. 2002;201:485–491. doi: 10.1046/j.1469-7580.2002.00119.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Asanome M, Matsuyama K, Mori S. Augmentation of postural muscle tone induced by the stimulation of the descending fibers in the midline area of the cerebellar white matter in the acute decerebrate cat. Neurosci Res. 1998;30:257–269. doi: 10.1016/s0168-0102(98)00006-6. [DOI] [PubMed] [Google Scholar]
- 98.Llinas R. Mechanisms of supraspinal actions upon spinal cord activities. Differences between reticular and cerebellar inhibitory actions upon alpha extensor motoneurons. J Neurophysiol. 1964;27:1117–1126. doi: 10.1152/jn.1964.27.6.1117. [DOI] [PubMed] [Google Scholar]
- 99.Eccles JC, Nicoll RA, Schwarz WF, Táboriková H, Willey TJ. Reticulospinal neurons with and without monosynaptic inputs from cerebellar nuclei. J Neurophysiol. 1975;38:513–530. doi: 10.1152/jn.1975.38.3.513. [DOI] [PubMed] [Google Scholar]
- 100.Fukushima K, Peterson BW, Uchino Y, Coulter JD, Wilson VJ. Direct fastigiospinal fibers in the cat. Brain Res. 1977;126:538–542. doi: 10.1016/0006-8993(77)90604-7. [DOI] [PubMed] [Google Scholar]
- 101.Bostan AC, Dum RP, Strick PL. Cerebellar networks with the cerebral cortex and basal ganglia. Trends Cogn Sci. 2013;17:241–254. doi: 10.1016/j.tics.2013.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Sasaki K, Kawaguchi S, Oka H, Sakai M, Mizuno N. Electrophysiological studies on the cerebellocerebral projections in monkeys. Exp Brain Res. 1976;24:495–507. doi: 10.1007/BF00234966. [DOI] [PubMed] [Google Scholar]
- 103.Amino Y, Kyuhou S, Matsuzaki R, Gemba H. Cerebellothalamo-cortical projections to the posterior parietal cortex in the macaque monkey. Neurosci Lett. 2001;309:29–32. doi: 10.1016/s0304-3940(01)02018-3. [DOI] [PubMed] [Google Scholar]
- 104.Kyuhou S, Kawaguchi S. Cerebellocerebral projection from the fastigial nucleus onto the frontal eye field and anterior ectosylvian visual area in the cat. J Comp Neurol. 1987;259:571–590. doi: 10.1002/cne.902590407. [DOI] [PubMed] [Google Scholar]
- 105.Middleton FA, Strick PL. Basal ganglia and cerebellar loops: motor and cognitive circuits. Brain Res Rev. 2000;31:236–250. doi: 10.1016/s0165-0173(99)00040-5. [DOI] [PubMed] [Google Scholar]
- 106.Hikosaka O. GABAergic output of the basal ganglia. Prog Brain Res. 2007;160:209–226. doi: 10.1016/S0079-6123(06)60012-5. [DOI] [PubMed] [Google Scholar]
- 107.Tarnutzer AA, Marti S, Straumann D. Gravity perception in cerebellar patients. Prog Brain Res. 2008;171:369–372. doi: 10.1016/S0079-6123(08)00654-7. [DOI] [PubMed] [Google Scholar]
- 108.Timmann D, Horak FB. Perturbed step initiation in cerebellar subjects: 2. Modification of anticipatory postural adjustments. Exp Brain Res. 2001;141:110–120. doi: 10.1007/s002210100858. [DOI] [PubMed] [Google Scholar]
- 109.Bostan AC, Dum RP, Strick PL. The basal ganglia communicate with the cerebellum. Proc Natl Acad Sci U S A. 2010;107:8452–8456. doi: 10.1073/pnas.1000496107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Brown LL, Schneider JS, Lidsky TI. Sensory and cognitive functions of the basal ganglia. Curr Opin Neurobiol. 1997;7:157–163. doi: 10.1016/s0959-4388(97)80003-7. [DOI] [PubMed] [Google Scholar]
- 111.Bloem BR, Valkenburg VV, Slabbekoorn M, van Dijk JG. The multiple tasks test. Strategies in Parkinson’s disease. Exp Brain Res. 2001;137:478–486. doi: 10.1007/s002210000672. [DOI] [PubMed] [Google Scholar]
- 112.Bhatia KP, Marsden CD. The behavioural and motor consequences of focal lesions of the basal ganglia in man. Brain. 1994;117(Pt 4):859–876. doi: 10.1093/brain/117.4.859. [DOI] [PubMed] [Google Scholar]
- 113.Takakusaki K, Saitoh K, Harada H, Kashiwayanagi M. Role of basal ganglia-brainstem pathways in the control of motor behaviors. Neurosci Res. 2004;50:137–151. doi: 10.1016/j.neures.2004.06.015. [DOI] [PubMed] [Google Scholar]
- 114.Filion M, Tremblay L. Abnormal spontaneous activity of globus pallidus neurons in monkeys with MPTP-induced parkinsonism. Brain Res. 1991;547:142–151. [PubMed] [Google Scholar]
- 115.Nambu A. Seven problems on the basal ganglia. Curr Opin Neurobiol. 2008;18:595–604. doi: 10.1016/j.conb.2008.11.001. [DOI] [PubMed] [Google Scholar]
- 116.Bohnen NI, Albin RL. The cholinergic system and Parkinson disease. Behav Brain Res. 2011;221:564–573. doi: 10.1016/j.bbr.2009.12.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Hirsch EC, Graybiel AM, Duyckaerts C, Javoy-Agid F. Neuronal loss in the pedunculopontine tegmental nucleus in Parkinson disease and in progressive supranuclear palsy. Proc Natl Acad Sci U S A. 1987;84:5976–5980. doi: 10.1073/pnas.84.16.5976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Jellinger K. The pedunculopontine nucleus in Parkinson’s disease, progressive supranuclear palsy and Alzheimer’s disease. J Neurol Neurosurg Psychiatry. 1988;51:540–543. doi: 10.1136/jnnp.51.4.540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Zweig RM, Jankel WR, Hedreen JC, Mayeux R, Price DL. The pedunculopontine nucleus in Parkinson’s disease. Ann Neurol. 1989;26:41–46. doi: 10.1002/ana.410260106. [DOI] [PubMed] [Google Scholar]
- 120.Müller ML, Albin RL, Kotagal V, Koeppe RA, Scott PJ, Frey KA, et al. Thalamic cholinergic innervation and postural sensory integration function in Parkinson’s disease. Brain. 2013;136(Pt 11):3282–3289. doi: 10.1093/brain/awt247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Jones BE. From waking to sleeping: neuronal and chemical substrates. Trends Pharmacol Sci. 2005;26:578–586. doi: 10.1016/j.tips.2005.09.009. [DOI] [PubMed] [Google Scholar]
- 122.Steriade M, McCormick DA, Sejnowski TJ. Thalamocortical oscillations in the sleeping and aroused brain. Science. 1993;262:679–685. doi: 10.1126/science.8235588. [DOI] [PubMed] [Google Scholar]
- 123.Winn P. Experimental studies of pedunculopontine functions: are they motor, sensory or integrative? Parkinsonism Relat Disord. 2008;14 Suppl 2:S194–S198. doi: 10.1016/j.parkreldis.2008.04.030. [DOI] [PubMed] [Google Scholar]
- 124.Dautan D, Huerta-Ocampo I, Witten IB, Deisseroth K, Bolam JP, Gerdjikov T, et al. A major external source of cholinergic innervation of the striatum and nucleus accumbens originates in the brainstem. J Neurosci. 2014;34:4509–4518. doi: 10.1523/JNEUROSCI.5071-13.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Mena-Segovia J, Winn P, Bolam JP. Cholinergic modulation of midbrain dopaminergic systems. Brain Res Rev. 2008;58:265–271. doi: 10.1016/j.brainresrev.2008.02.003. [DOI] [PubMed] [Google Scholar]
- 126.Takakusaki K, Shiroyama T, Yamamoto T, Kitai ST. Cholinergic and noncholinergic tegmental pedunculopontine projection neurons in rats revealed by intracellular labeling. J Comp Neurol. 1996;371:345–361. doi: 10.1002/(SICI)1096-9861(19960729)371:3<345::AID-CNE1>3.0.CO;2-2. [DOI] [PubMed] [Google Scholar]
- 127.Hasselmo ME, Sarter M. Modes and models of forebrain cholinergic neuromodulation of cognition. Neuropsychopharmacology. 2011;36:52–73. doi: 10.1038/npp.2010.104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Hanakawa T, Fukuyama H, Katsumi Y, Honda M, Shibasaki H. Enhanced lateral premotor activity during paradoxical gait in Parkinson’s disease. Ann Neurol. 1999;45:329–336. doi: 10.1002/1531-8249(199903)45:3<329::aid-ana8>3.0.co;2-s. [DOI] [PubMed] [Google Scholar]
- 129.Hanakawa T, Katsumi Y, Fukuyama H, Honda M, Hayashi T, Kimura J, et al. Mechanisms underlying gait disturbance in Parkinson’s disease: a single photon emission computed tomography study. Brain. 1999;122(Pt 7):1271–1282. doi: 10.1093/brain/122.7.1271. [DOI] [PubMed] [Google Scholar]
- 130.Bohnen NI, Müller ML, Koeppe RA, Studenski SA, Kilbourn MA, Frey KA, et al. History of falls in Parkinson disease is associated with reduced cholinergic activity. Neurology. 2009;73:1670–1676. doi: 10.1212/WNL.0b013e3181c1ded6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Müller ML, Bohnen NI. Cholinergic dysfunction in Parkinson’s disease. Curr Neurol Neurosci Rep. 2013;13:377. doi: 10.1007/s11910-013-0377-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Scocco DH, Wagner JN, Racosta J, Chade A, Gershanik OS. Subjective visual vertical in Pisa syndrome. Parkinsonism Relat Disord. 2014;20:878–883. doi: 10.1016/j.parkreldis.2014.04.030. [DOI] [PubMed] [Google Scholar]
- 133.Vitale C, Marcelli V, Furia T, Santangelo G, Cozzolino A, Longo K, et al. Vestibular impairment and adaptive postural imbalance in parkinsonian patients with lateral trunk flexion. Mov Disord. 2011;26:1458–1463. doi: 10.1002/mds.23657. [DOI] [PubMed] [Google Scholar]
- 134.Villarejo A, Camacho A, García-Ramos R, Moreno T, Penas M, Juntas R, et al. Cholinergic-dopaminergic imbalance in Pisa syndrome. Clin Neuropharmacol. 2003;26:119–121. doi: 10.1097/00002826-200305000-00004. [DOI] [PubMed] [Google Scholar]
- 135.Doherty KM, van de Warrenburg BP, Peralta MC, SilveiraMoriyama L, Azulay JP, Gershanik OS, et al. Postural deformities in Parkinson’s disease. Lancet Neurol. 2011;10:538–549. doi: 10.1016/S1474-4422(11)70067-9. [DOI] [PubMed] [Google Scholar]
- 136.Vaugoyeau M, Azulay JP. Role of sensory information in the control of postural orientation in Parkinson’s disease. J Neurol Sci. 2010;289:66–68. doi: 10.1016/j.jns.2009.08.019. [DOI] [PubMed] [Google Scholar]
- 137.Vaugoyeau M, Viel S, Assaiante C, Amblard B, Azulay JP. Impaired vertical postural control and proprioceptive integration deficits in Parkinson’s disease. Neuroscience. 2007;146:852–863. doi: 10.1016/j.neuroscience.2007.01.052. [DOI] [PubMed] [Google Scholar]
- 138.Pollak L, Prohorov T, Kushnir M, Rabey M. Vestibulocervical reflexes in idiopathic Parkinson disease. Neurophysiol Clin. 2009;39:235–240. doi: 10.1016/j.neucli.2009.07.001. [DOI] [PubMed] [Google Scholar]
- 139.Michel SF, Arias Carrión O, Correa TE, Alejandro PL, Micheli F. Pisa syndrome. Clin Neuropharmacol. 2015;38:135–140. doi: 10.1097/WNF.0000000000000092. [DOI] [PubMed] [Google Scholar]
- 140.Solla P, Cannas A, Congia S, Floris G, Aste R, Tacconi P, et al. Levodopa/carbidopa/entacapone-induced acute Pisa syndrome in a Parkinson’s disease patient. J Neurol Sci. 2008;275:154–156. doi: 10.1016/j.jns.2008.07.017. [DOI] [PubMed] [Google Scholar]
- 141.van de Warrenburg BP, Bhatia KP, Quinn NP. Pisa syndrome after unilateral pallidotomy in Parkinson’s disease: an unrecognised, delayed adverse event? J Neurol Neurosurg Psychiatry. 2007;78:329–330. doi: 10.1136/jnnp.2006.103358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Spanaki C, Zafeiris S, Plaitakis A. Levodopa-aggravated lateral flexion of the neck and trunk as a delayed phenomenon of unilateral pallidotomy. Mov Disord. 2010;25:655–656. doi: 10.1002/mds.22988. [DOI] [PubMed] [Google Scholar]
- 143.Mirdamadi JL. Cerebellar role in Parkinson’s disease. J Neurophysiol. 2016;116:917–919. doi: 10.1152/jn.01132.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Lewis MM, Galley S, Johnson S, Stevenson J, Huang X, McKeown MJ. The role of the cerebellum in the pathophysiology of Parkinson’s disease. Can J Neurol Sci. 2013;40:299–306. doi: 10.1017/s0317167100014232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Roseberry TK, Lee AM, Lalive AL, Wilbrecht L, Bonci A, Kreitzer AC. Cell-type-specific control of brainstem locomotor circuits by basal ganglia. Cell. 2016;164:526–537. doi: 10.1016/j.cell.2015.12.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Castrioto A, Piscicelli C, Perennou D, Krack P, Debu B. The pathogenesis of Pisa syndrome in Parkinson’s disease. Mov Disord. 2014;29:1100–1117. doi: 10.1002/mds.25925. [DOI] [PubMed] [Google Scholar]
- 147.Karachi C, Grabli D, Bernard FA, Tandé D, Wattiez N, Belaid H, et al. Cholinergic mesencephalic neurons are involved in gait and postural disorders in Parkinson disease. J Clin Invest. 2010;120:2745–2754. doi: 10.1172/JCI42642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Rinne JO, Ma SY, Lee MS, Collan Y, Röyttä M. Loss of cholinergic neurons in the pedunculopontine nucleus in Parkinson’s disease is related to disability of the patients. Parkinsonism Relat Disord. 2008;14:553–557. doi: 10.1016/j.parkreldis.2008.01.006. [DOI] [PubMed] [Google Scholar]
- 149.Piallat B, Chabardès S, Torres N, Fraix V, Goetz L, Seigneuret E, et al. Gait is associated with an increase in tonic firing of the sub-cuneiform nucleus neurons. Neuroscience. 2009;158:1201–1205. doi: 10.1016/j.neuroscience.2008.10.046. [DOI] [PubMed] [Google Scholar]
- 150.Thevathasan W, Pogosyan A, Hyam JA, Jenkinson N, Foltynie T, Limousin P, et al. Alpha oscillations in the pedunculopontine nucleus correlate with gait performance in parkinsonism. Brain. 2012;135(Pt 1):148–160. doi: 10.1093/brain/awr315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Benarroch EE. Pedunculopontine nucleus: functional organization and clinical implications. Neurology. 2013;80:1148–1155. doi: 10.1212/WNL.0b013e3182886a76. [DOI] [PubMed] [Google Scholar]
- 152.Hamani C, Moro E, Lozano AM. The pedunculopontine nucleus as a target for deep brain stimulation. J Neural Transm (Vienna) 2011;118:1461–1468. doi: 10.1007/s00702-010-0547-8. [DOI] [PubMed] [Google Scholar]
- 153.Pereira EA, Nandi D, Jenkinson N, Stein JF, Green AL, Aziz TZ. Pedunculopontine stimulation from primate to patient. J Neural Transm (Vienna) 2011;118:1453–1460. doi: 10.1007/s00702-011-0631-8. [DOI] [PubMed] [Google Scholar]
- 154.Stefani A, Lozano AM, Peppe A, Stanzione P, Galati S, Tropepi D, et al. Bilateral deep brain stimulation of the pedunculopontine and subthalamic nuclei in severe Parkinson’s disease. Brain. 2007;130:1596–1607. doi: 10.1093/brain/awl346. [DOI] [PubMed] [Google Scholar]
- 155.Mazzone P, Sposato S, Insola A, Scarnati E. The clinical effects of deep brain stimulation of the pedunculopontine tegmental nucleus in movement disorders may not be related to the anatomical target, leads location, and setup of electrical stimulation. Neurosurgery. 2013;73:894–906. doi: 10.1227/NEU.0000000000000108. discussion 905-906. [DOI] [PubMed] [Google Scholar]
- 156.Ferraye MU, Debû B, Fraix V, Goetz L, Ardouin C, Yelnik J, et al. Effects of pedunculopontine nucleus area stimulation on gait disorders in Parkinson’s disease. Brain. 2010;133(Pt 1):205–214. doi: 10.1093/brain/awp229. [DOI] [PubMed] [Google Scholar]
- 157.Moro E, Hamani C, Poon YY, Al-Khairallah T, Dostrovsky JO, Hutchison WD, et al. Unilateral pedunculopontine stimulation improves falls in Parkinson’s disease. Brain. 2010;133(Pt 1):215–224. doi: 10.1093/brain/awp261. [DOI] [PubMed] [Google Scholar]
- 158.Mazzone P, Scarnati E, Garcia-Rill E. Commentary: the pedunculopontine nucleus: clinical experience, basic questions and future directions. J Neural Transm (Vienna) 2011;118:1391–1396. doi: 10.1007/s00702-010-0530-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Mazzone P, Vilela Filho O, Viselli F, Insola A, Sposato S, Vitale F, et al. Our first decade of experience in deep brain stimulation of the brainstem: elucidating the mechanism of action of stimulation of the ventrolateral pontine tegmentum. J Neural Transm (Vienna) 2016;123:751–767. doi: 10.1007/s00702-016-1518-5. [DOI] [PubMed] [Google Scholar]
- 160.Alam M, Schwabe K, Krauss JK. The pedunculopontine nucleus area: critical evaluation of interspecies differences relevant for its use as a target for deep brain stimulation. Brain. 2011;134(Pt 1):11–23. doi: 10.1093/brain/awq322. [DOI] [PubMed] [Google Scholar]
- 161.Karachi C, André A, Bertasi E, Bardinet E, Lehéricy S, Bernard FA. Functional parcellation of the lateral mesencephalus. J Neurosci. 2012;32:9396–9401. doi: 10.1523/JNEUROSCI.0509-12.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Fling BW, Cohen RG, Mancini M, Carpenter SD, Fair DA, Nutt JG, et al. Functional reorganization of the locomotor network in Parkinson patients with freezing of gait. PLoS One. 2014;9:e100291. doi: 10.1371/journal.pone.0100291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Schweder PM, Hansen PC, Green AL, Quaghebeur G, Stein J, Aziz TZ. Connectivity of the pedunculopontine nucleus in parkinsonian freezing of gait. Neuroreport. 2010;21:914–916. doi: 10.1097/WNR.0b013e32833ce5f1. [DOI] [PubMed] [Google Scholar]
- 164.Snijders AH, Takakusaki K, Debu B, Lozano AM, Krishna V, Fasano A, et al. Physiology of freezing of gait. Ann Neurol. 2016;80:644–659. doi: 10.1002/ana.24778. [DOI] [PubMed] [Google Scholar]
- 165.Takakusaki K, Takahashi M, Obara K, Chiba R. Neural substrates involved in the control of posture. Adv Robot. 2016 Dec 6; doi: 10.1080/01691864.2016.1252690. [Epub]. [DOI] [Google Scholar]


