Abstract
Background:
Nasomaxillary hypoplasia is a rare congenital disorder involving the central face. It imparts a distinctive appearance to the individual face as the age advances. Severity of the disorder varies, so do the manifestations.
Methods:
This was a retrospective study conducted on the records and photographic data of 560 rhinoplasty cases performed between 2006 March and 2016 March. About 16 cases of nasomaxillary hypoplasia were selected from the group and they were classified based on the severity of the features. Surgical correction performed in each group was detailed.
Results:
Three percent of the 560 rhinoplasties performed in our centre turned out to be cases of Binder's syndrome. Nasal correction with locoregional autologous cartilage grafts was sufficient in mild cases. Loco-regional cartilage grafts along with costal cartilage grafts were needed for moderate and severe cases. Anterior nasal floor along with alar base augmentation was performed to achieve a proper aesthetic profile in moderate and severe cases. Post-operative results were excellent in mild and moderate cases and acceptable in severe cases.
Discussion:
We attempted to correct the deformity only after growth of the nose and maxilla was completed. We used cartilage grafts as a mainstay as cartilage has long-term stability without resorption unlike bone grafts. Instead of following en bloc technique of cartilage assembly, we have reconstructed the nasal dorsum, columella and tip separately as this principle is more functionally acceptable with less warping or stiffness of the nose. Importance was given to proper anchorage of grafts.
Conclusion:
We have attempted to put together the various features into three categories of mild/moderate/severe based on previous anthropometric studies of nasal anatomical parameters. The second objective of our study was to advise a logical surgical protocol for each group so that future surgeons can follow an easy surgical guideline to attain optimal cosmetic and functional results.
KEY WORDS: Binder's syndrome, classification, nasomaxillary hypoplasia, rhinoplasty
INTRODUCTION
Nasomaxillary hypoplasia or Binder's syndrome is a congenital deformity involving the midfacial skeleton characterised by underdevelopment of the nose and upper jaw, which is also called dish-face deformity.[1] The first case was reported by Noyes in 1939.[2] Binder was the first person to define the condition as a distinct clinical entity in 1962. He reported three cases and recorded six characteristic features: Arhinoid face, abnormal position of the nasal bones, intermaxillary hypoplasia with resultant malocclusion, reduced or absent anterior nasal spine (ANS), atrophy of the nasal mucosa and absence or underdevelopment of frontal sinus.[3] Individuals with this syndrome present with the typical facial appearance of wide frontonasal angle, apparent long nose, short columella, convex upper lip with broad philtrum, acute nasolabial angle and half-moon-shaped nostrils.
The aetiology of this condition is attributed to the inhibition of ossification centre responsible for the growth of lateral and inferior borders of the pyriform aperture during the 5th-6th week of gestation.[4] There is no sexual predominance, and most cases are sporadic.[5] More than 250 cases have been reported in literature so far.[6]
Surgical treatment for this deformity has been challenging to say the least. It has evolved from simple onlay bony cartilaginous grafts to Le Fort's osteotomies for maxillary advancement.
Due to the rarity of the congenital condition, literature reveals either single case reports or small series studies on Binder's syndrome.[6,7,8] Overall, there have been varying reports about the surgical modalities used in Binder's cases of differing severities. No standard protocol has been defined regarding corrective rhinoplasty for nasomaxillary hypoplasia.
The objective of our study is to:
Classify the variants of nasomaxillary hypoplasia based on the clinical features
Advocate a logical treatment protocol for each type described.
This will enable surgeons to categorise the deformity and follow a simple surgical guideline to attain optimal long-term cosmetic and functional results.
METHODS
This was a retrospective study of 16 cases of nasomaxillary hypoplasia (Binder's syndrome) selected from case records and photographs of 560 cases of rhinoplasties performed between March 2006 to March 2016. Diagnosis of Binder's syndrome was based on the typical features.
Age of the patients ranged from 16 to 30 years with an average age of 20 years, 10 months. Ten were females and six were males. There was no familial history of similar disorder. Related random findings were noticed in three individual cases such as congenital pits on the upper lateral cartilages in one case, absence of nasal bones on one case and a submucous cleft in one case. All except two cases had class 1 occlusion. One case has class 3 malocclusion; another had end on occlusion. Cases were classified into mild, moderate and severe, depending on the severity of the clinical features.
All the cases underwent primary rhinoplasty except one case which was a revision case, operated earlier by another surgeon. All the patients were operated by one surgeon and were evaluated by pre- and post-operative photographs. Follow-up ranged from 6 months to 8 years.
Autologous cartilage graft from the nasal septum, ear concha and rib was used for reconstruction [Figure 1a–c]. Our method of harvesting costal cartilage was extracting the upper 2/3rd of the width and preserving the lower 1/3rd to maintain the rib continuity. This reduced post-operative pain and ensured rapid recovery of the local site [Figure 2]. Rib slices were put in normal saline for half an hour before using them to facilitate discarding the warped slices.
Figure 1.

Cartilage grafts; (a) septal and conchal cartilages (b) rib cartilage slices (c) stacked overlay graft
Figure 2.
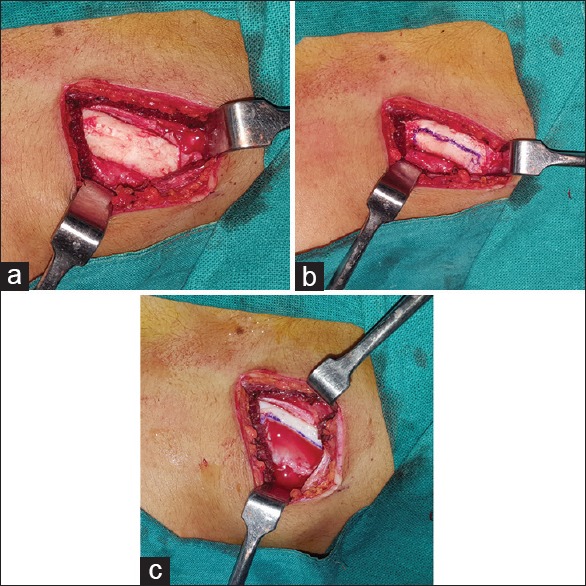
Method of rib cartilage graft harvest; (a) exposed rib cartilage (b) Excision marked (c) Rib continuity after excision
Surgical technique and operative steps
All cases had a common surgical approach; transcolumellar incision and open rhinoplasty. V-Y advancement of columellar incision was planned in severe variety of cases. Dissection was done inferiorly towards ANS in mild cases and extended laterally up to pyriform aperture in moderate and severe cases. Bilateral sublabial incisions were made in severe cases for placement of alar base grafts. Nasal pyramid was degloved in subperichondrial plane. Nasal septum was exposed from the caudal angle/border in bilateral subperichondrial planes by anterior and inferior tunnelling.
Mild cases
Cartilage grafts
Nasal septal cartilage grafts and bilateral conchal cartilage grafts were used.
Columellar projection
Columellar projection was done by septal cartilage graft extended from ANS below to the future tip, fixed to the caudal border of the septum by overlapping margins with 5.0 proline/PDS [Figure 3a].
Figure 3.

Technique for mild cases; (a) caudal strut (b) cartilage dorsum and tip graft
Dorsal projection
The apparent bony hump of the dorsum was resected, and stacked conchal cartilage graft was placed on the cartilage dorsum as an overlay graft. The skin was re-draped and closed comfortably [Figure 3b].
Tip projection
Tip projection was achieved by lateral crural steal, intra- and inter-domal suturing and a small dome graft.
Moderate cases
Cartilage grafts used were septal cartilage, bilateral conchal cartilage and rib cartilage slices.
Columellar projection
A T-shaped cartilage strip assembly was formed from the rib cartilage and fixed in an inverted T manner. The horizontal limb was placed anterior to the short ANS and on the anterior nasal floor, vertical limb formed the caudal strut. The fixation of the assembly was by making a facet in the horizontal limb to fit into the existing ANS, and vertical limb was fixed to the caudal border of the septum in an overlapping manner [Figure 4a and b].
Figure 4.

Technique for moderate cases. (a) Inverted T assembly (b) caudal strut (c) cartilage dorsum and tip graft
Dorsal projection
Cartilaginous dorsum was augmented by first partially separating the upper lateral cartilages and placing two-rib cartilage strips as spreader grafts extended to the tip. Height of the grafts was raised on either side of the septum dorsal border and fixed in an overlapping manner. A full-length overlay cartilage stacked graft was placed to camouflage the dorsum [Figure 4c].
Tip projection
Tip projection was achieved in the same manner as in mild cases.
Severe cases
Cartilage grafts used were good volume of rib cartilage, trivial volume of septal cartilage and bilateral conchal cartilage.
Columellar projection
T-shaped cartilage assembly was created as in moderate cases, but the horizontal limb was fixed to the premaxilla with 6 mm titanium screws [Figure 5a].
Figure 5.

Technique for severe cases; (a) caudal strut (b) extended spreader graft on the right side (c) extended spreader grafts on both sides (d) sutured grafts - functional nasal pyramid (e) alar base graft placement
Dorsal projection
Bilateral upper laterals were detached completely, two-rib cartilage strips were placed as extended spreader grafts and raised above the existing dorsum from the keystone area (bone–cartilage junction) down to the tip. The upper laterals were reattached, and spreaders were fixed at the keystone area with a prolene stitch passed through a drill hole in the nasal bones. This raised cartilage dorsum formed the new functional nasal pyramid [Figure 5b–d]. A full-length overlay conchal cartilage stacked graft further elevated the dorsum.
Tip projection
Tip projection was same as in mild and moderate cases, but weak alar cartilages were reinforced with pieces of conchal cartilage grafts.
Semilunar-shaped alar base grafts were placed through a bilateral sublabial incision [Figure 5e].
A schematic diagram depicting the techniques in mild, moderate and severe cases is shown in Figure 6.
Figure 6.

Schematic diagram showing the type and technical methods
Post-operative results were assessed with nose examination and photographs.
During this study, a long-term review was done on all these patients by telephonic interview. The following six parameters were studied to assess the functional and aesthetic outcome:
Nasal breathing: Normal/reduced
Satisfaction scale: Very satisfied (8-10)/satisfied (5-7)/dissatisfied (<4)
Appearance improvement scale: Great improvement (8-10)/some improvement (5-7)/no improvement (<4)
Tip stiffness: Nil/minimal/bothersome
Donor site: Nil scar/hypertrophic scar/keloid
Columellar scar: Visible/barely visible/well visible.
RESULTS
Almost 3% of the total rhinoplasties performed in our centre were cases of Binder's syndrome. Among the 16 cases, 4 cases were of mild variety, 9 cases belonged to moderate variety and 3 cases were classified under severe type. The longest follow-up case in the whole series was 8 years. The least follow-up case was 6 months. Pre- and post-operative results of the patients are displayed in Figures 7–11. Cartilage grafts were used in all cases except one case where polyethylene implant (Medpor) was placed as L-assembly (due to patient's personal preference).
Figure 7.

Pre-operative (above) and post-operative (below) pictures of a mild type case
Figure 11.

Pre- and post-operative results of a severe case
Figure 8.

Pre- and post-operative pictures of a moderate case
Figure 9.

Pre- and post-operative pictures of a moderate case
Figure 10.

Pre- and post-operative pictures of a moderate case. Post-operative columellar scar in the basal view
There were no major complications such as post-operative infection, skin necrosis and graft resorption. All the patients were satisfied with the cosmetic and functional outcome in the long run. Adverse effects were seen in two cases, both belonging to severe variety. The first one which was a revision case where a large L-assembly with rib cartilage graft had been used resulted in warping of the dorsum. It was corrected after 9 months by incision made locally on the dorsum. Good shape was achieved, followed up for one more year without any adverse outcome [Figure 12a–b]. The second one was a bad columellar scar, after V-Y advancement due to delayed healing as a result of vascular compromise.
Figure 12.

Working of the dorsal rib cartilage graft. (a) Graft assembly with all the parts; dorsal, columellar and nasal floor. (b) Warped rib graft (c) contouring the dorsum of a well-settled graft by making an incision on the dorsum
The results of the telephonic long-term review to assess the six parameters of patient satisfaction were as follows:
We could record the responses of 11/16 patients, the remaining five were unavailable. Breathing was normal in all patients
In the satisfaction scale, 8 of the 11 patients were very satisfied, 3 were satisfied
Nine patients responded as a great improvement in the appearance and two patients responded as some improvement in the appearance
Minimal tip stiffness was complained by five patients, none of the patients complained of bothersome tip stiffness. No patient complained of keloid at any donor site, two patients complained of scar hypertrophy and redness (at <1 year post-operative)
Three patients complained of a visible columellar scar, two of them belonging to severe variety and one to moderate variety. All the three were more than 3 years after surgery.
DISCUSSION
When we collected the 16 cases of Binder's syndrome from our 560 rhinoplasties performed over a decade retrospectively, we found a wide range of severity of the clinical features and tailor-made treatment techniques executed on them. Thus, a correlation between the nature of a deformity and the treatment instituted for each case evolved, leading to the formulation of a classification system of mild, moderate and severe Binder's syndrome along with the proposed surgical correction for each group. Earliest comments on Binder's syndrome as normal length and short nose variants were made by Rintala and Ranta.[9] Although the terms mild and severe were used in many studies on Binder's syndrome, so far no single study has put forward such a classification.[6,7,8,10] We have thus proposed a classification for clinical features and management protocol for nasomaxillary hypoplasia as mentioned in Table 1.[11,12,13]
Table 1.
The proposed classification for clinical features & management protocol in Naso-maxillary hypoplasia

Nasomaxillary hypoplasia is primarily a developmental tissue shortage, so we followed the philosophy of nasal correction once the growth of the nose and maxilla was completed, i.e., after 16 years of age.[10,14]
In our cases, we chose only cartilage grafts (except in one case where the patient insisted on alloplast). Earlier studies have revealed that bone grafts used in distal dorsum, tip and columella undergo partial resorption whereas cartilage maintains its shape and volume even after several years.[7,10,14] We used cartilage from the nasal septum, concha and rib, each donor site having its distinct advantage. About 1–1.2 mm thick core rib cartilage slices are best suited for columellar struts and extended spreader grafts; perichondrium-covered conchal cartilage is good for stacked overlay graft, septal cartilage can be used in any of these areas. We used septal and conchal cartilage for mild cases and additional rib cartilage in moderate and severe cases.
Regarding corrective rhinoplasty, this study differs from the traditional method of placing a L-block assembly of either cartilage or bone on the degloved nasal pyramid.[6,7] We have also not followed the cantilever technique of augmenting the nasal dorsum and tip.[15,16] We believe that the normal nose does not have these en bloc tissue chunks which may result in heaviness, rigidity, warping or unnatural appearance. Hence, we reconstructed the nasal columella, dorsum, and tip separately.
Importance was given to maintaining a functional nasal pyramid and not just augmenting the nose shape. Our method was evolved from the technique of extracorporeal septorhinoplasty.[17] In severe cases, this could be achieved by detaching upper lateral cartilages from the nasal septum followed by inserting and fixing the extended spreader grafts while keeping the nasal mucosa intact.
Fixation of the nasal grafts is another aspect that was given weightage in this study. Naturally existing structures such as the nasal septum, ANS, upper lateral cartilages, nasal bones and premaxilla were used for anchorage. The anchoring points for the cartilage grafts vary according to the degree of the deformity and type of graft used. For instance, inverted T columellar strut was fixed to the hypoplastic ANS by making a facet in the horizontal limb, whereas in case of absent ANS, it was fixed to the premaxilla by screws.
Nowadays, a few surgeons are using diced or minced cartilage pieces wrapped in the fascia as the overlay graft is perceptible on the dorsum, especially in thin skin.[17,18] Since Indians have moderately thick skin, we used stacked cartilage grafts which highlighted the nasal dorsal lines.
Our study has concentrated on only corrective rhinoplasty. We found that more than 80% of the cases of Binder's syndrome presenting for correction belonged to the mild and moderate varieties. We could achieve adequate cosmetic correction of the nose and midface profile with cartilage grafts, the same was supported in a study by Watanabe and Matsuo.[19] We did not perform osteotomy or maxillary advancement because relative prognathism was seen in only two cases and particularly those two were not much eager to undergo the jaw osteotomy. Monasterio et al.[6] quote 15% of class 3 occlusion in their series of Binder's syndrome. However, if required, Le Fort II osteotomy and orthodontic treatment must be included in the management of severe cases as advised in some other studies.[20,21,22] At the same time, management of extreme hypoplasia where there is a requirement of nasal inlay grafting or permanent prosthesis is out of scope of this study.[23]
CONCLUSION
We would like to highlight certain features of our study, which make it different from previous literature on Binder's syndrome. First, we made the observation that most cases of nasomaxillary hypoplasia present as mild or moderate deformity, severe hypoplasia being seen in only a few cases. Second, during surgical reconstruction, locoregional cartilage grafts (septal and conchal) can be used extensively in mild and moderate cases without having to solely depend on costal cartilage for augmentation. The third point of emphasis is the proper anchorage of the grafts to the nasal bones, residual septal cartilage, nasal cartilage and ANS that will ensure excellent long-term results. Finally, we have proposed an easy-to-follow classification of cases into mild, moderate and severe forms of Binder's syndrome with a corresponding treatment strategy.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Ragnell A. A simple method of reconstruction in some cases of dish-face deformity. Plast Reconstr Surg. 1952;10:227–37. doi: 10.1097/00006534-195210000-00002. [DOI] [PubMed] [Google Scholar]
- 2.Noyes FB. Case report. Angle Orthod. 1939;9:160–5. [Google Scholar]
- 3.Binder KH. Dysostosis maxilla-nasalis, an archinencephalic malformation complex. German dentist search. 1962;17:438–44. [Google Scholar]
- 4.Holmstrom H. Clinical and pathologic features of maxillonasal dysplasia (Binders syndrome): Significance of the prenasal fossa on etiology. Plast Reconstr Surg. 1986;78:559–67. doi: 10.1097/00006534-198611000-00001. [DOI] [PubMed] [Google Scholar]
- 5.Olow-Nordenram M, Valentin J. An etiologic study of maxillonasal dysplasia – Binder's syndrome. Scand J Dent Res. 1988;96:69–74. doi: 10.1111/j.1600-0722.1988.tb01410.x. [DOI] [PubMed] [Google Scholar]
- 6.Monasterio FO, Molina F, McClintock JS. Nasal correction in Binder's syndrome: the evolution of a treatment plan. Aesthetic Plast Surg. 1997;21:299–308. doi: 10.1007/s002669900129. [DOI] [PubMed] [Google Scholar]
- 7.Draf W, Bockmühl U, Hoffmann B. Nasal correction in maxillonasal dysplasia (Binder's syndrome): A long term follow-up study. Br J Plast Surg. 2003;56:199–204. doi: 10.1016/s0007-1226(03)00099-7. [DOI] [PubMed] [Google Scholar]
- 8.Deshpande S, Juneja MH. Binders syndrome (Maxillonasal dysplasia) different treatment modalities: Our experience. Indian J Plast Surg. 2012;45:62–6. doi: 10.4103/0970-0358.96588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rintala A, Ranta A. Nasomaxillary hypoplasia – Binders syndrome. Morphology and treatment if two separate varieties. Scand J Plast Reconstr Surg. 1985;19:127. doi: 10.3109/02844318509072370. [DOI] [PubMed] [Google Scholar]
- 10.Goh RC, Chen YR. Surgical management of Binder's syndrome: Lessons learned. Aesthetic Plast Surg. 2010;34:722–30. doi: 10.1007/s00266-010-9533-7. [DOI] [PubMed] [Google Scholar]
- 11.Asharani SK, Lokanathan TH, Rajendra R, Surendra M. Study of nasalindex among students of teriatiary medical care institute in Southern India. Int J Anat Res. 2015;3:1675–9. [Google Scholar]
- 12.Khanderkar B, Srinivasan S, Mokal N. Anthropometric analysis of lip-nose complex in Indian population. Indian J Plast Surg. 2005;38:128–31. [Google Scholar]
- 13.Armijo BS, Brown M, Guyuron B. Defining the ideal nasolabial angle. Plast Reconstr Surg. 2012;129:759–64. doi: 10.1097/PRS.0b013e3182402e12. [DOI] [PubMed] [Google Scholar]
- 14.Tessier P, Tulasne JF, Delaire J, Resche F. Therapeutic aspects of maxillonasal dysostosis (Binder syndrome) Head Neck Surg. 1981;3:207–15. doi: 10.1002/hed.2890030308. [DOI] [PubMed] [Google Scholar]
- 15.Jackson IT, Moos KF, Sharpe DT. Total surgical management of Binder's syndrome. Ann Plast Surg. 1981;7:25–34. doi: 10.1097/00000637-198107000-00004. [DOI] [PubMed] [Google Scholar]
- 16.Banks P, Tanner B. The mask rhinoplasty: A technique for the treatment of Binder's syndrome and related disorders. Plast Reconstr Surg. 1993;92:1038–44. [PubMed] [Google Scholar]
- 17.Gubisch W. Extracorporeal septoplasty for the markedly deviated septum. Arch Facial Plast Surg. 2005;7:218–26. doi: 10.1001/archfaci.7.4.218. [DOI] [PubMed] [Google Scholar]
- 18.Erol OO. The Turkish delight: A pliable graft for rhinoplasty. Plast Reconstr Surg. 2000;105:2229–41. doi: 10.1097/00006534-200005000-00051. [DOI] [PubMed] [Google Scholar]
- 19.Watanabe T, Matsuo K. Augmentation with cartilage grafts around the pyriform aperture to improve the midface and profile in Binder's syndrome. Ann Plast Surg. 1996;36:206–11. doi: 10.1097/00000637-199602000-00020. [DOI] [PubMed] [Google Scholar]
- 20.Henderson D, Jackson IT. Naso-maxillary hypoplasis – The Le Fort II osteotomy. Br J Oral Surg. 1973;11:77–93. doi: 10.1016/0007-117x(73)90022-x. [DOI] [PubMed] [Google Scholar]
- 21.Losken HW, Morris WM, Uys PB. Le Fort II osteotomy in the treatment of maxillonasal dysostosis (Binder's syndrome) S Afr J Surg. 1988;26:88–9. [PubMed] [Google Scholar]
- 22.Converse JM, Horowitz SL, Valauri AJ, Montandon D. The treatment of nasomaxillary hypoplasia. A new pyramidal naso-orbital maxillary osteotomy. Plast Reconstr Surg. 1970;45:527–35. doi: 10.1097/00006534-197006000-00001. [DOI] [PubMed] [Google Scholar]
- 23.Gillies HD. Deformities of the syphilitic nose. Br Med J. 1923;29:977. [Google Scholar]


