Abstract
Background:
Many spine surgeons recommend stringent weight loss, including bariatric bypass procedures, prior to “elective” spine surgery (should not be for axial back pain alone) in morbidly obese patients (defined by a body mass index (BMI) of >40 mg/kg2 or >35 mg/kg2 with two or more major comorbidities) to reduce their greater risk for major perioperative complications. Although bypasses typically lead to marked weight reduction and even reduced axial back pain, they also promote unrecognized and often insufficiently treated vitamin D deficiency and loss of bone mineral density.
Methods:
Morbidly obese patients who are under consideration for “elective” spine operations (other than for back pain alone) are often told to lose weight. Some choose to undergo bariatric bypass procedures, but are unaware of the potential risks/complications of these procedures.
Results:
Within the first 2 years following most bariatric bypass procedures, patients experience not only marked loss of weight and muscle mass, but also significant vitamin D deficiency and loss of bone mineral density, increasing their susceptibility to fractures. Nevertheless, some patients also experience a sufficient reduction of axial back pain to avoid spinal surgery.
Conclusions:
Morbidly obese patients under consideration for “elective” spine surgery may undergo bariatric bypass procedures that lead to a significant reduction of vitamin D levels and loss of bone mineral density. However, potential benefits may include a sufficient reduction of axial back pain to avoid surgery in a select subset of patients altogether.
Keywords: Bariatric surgery, bone, bypass, morbid obesity, spine surgery
INTRODUCTION
Many spine surgeons recommend that patients with morbid obesity (body mass index (BMI) of >40 mg/kg2 or >35 mg/kg2 with two or more major comorbidities) warranting “elective” surgery undergo significant weight reduction prior to spine surgery. “Elective” spine surgery in these patients with significant neurological/radiographic pathology (not for pain alone, non-emergent) may result in major life-threatening complications. Therefore, with the help of their internists, these patients may weigh the pros and cons of bariatric bypass procedures. Nevertheless, they should be aware of the bariatric bypass risks; significant decreases in Vitamin D level and loss of bone mineral density (BMD) that increases the risk of fractures. An added unanticipated benefit, however, may be sufficient alleviation of axial back pain to avoid, in some patients with lesser deficits, spine surgery altogether.
MORBIDLY OBESE PATIENTS HAVE HIGHER MORBIDITY RATES WITH SPINE SURGERY
Morbidly obese patients and their spine surgeons should be familiar with the markedly increased frequency of adverse events/medical/surgical complications associated with spine surgery. As this knowledge prompts more spine surgeons to first recommend stringent weight loss, patients and their medical consultants must choose among the myriad of weight loss measures that now include bariatric bypasses.
INCREASED RISKS OF SPINE SURGERY IN MORBIDLY OBESE PATIENTS
Morbidly obese patients are at greater risk for major complications/adverse events when undergoing elective spine surgery.[3,5,8,9,11] Here, we define morbid obesity by a BMI of >40 kg/m2 or >35 kg/m2 with two or more major comorbidities (e.g., hypertension, diabetes, etc.). In 2003, Olsen et al. observed longer lengths of stay and 30-day postoperative readmission rates in morbidly obese patients undergoing spine surgery.[8] Patel et al. documented in 2007 that higher complication rates correlated with greater degrees of obesity; they observed a 14% complication rate for BMI of <25, 20% for BMI ≥25–30, and 36% rate for BMI >40.[9] In 2009, Vaidya et al. noted noted that morbidly obese patients required longer surgical times and exhibited a 45% higher rate of complications.[11] In 2016, Higgens et al. described a 2.5 times greater risk of medical complications, and 10-fold greater risk of wound complications in morbidly obese patients undergoing spinal procedures.[5]
BARIATRIC BYPASS SURGERY CONTRIBUTES TO SIGNIFICANT LOSS OF BONE MINERAL DENSITY AND DECREASED VITAMIN D LEVELS WITHIN FIRST 2 POSTOPERATIVE YEARS
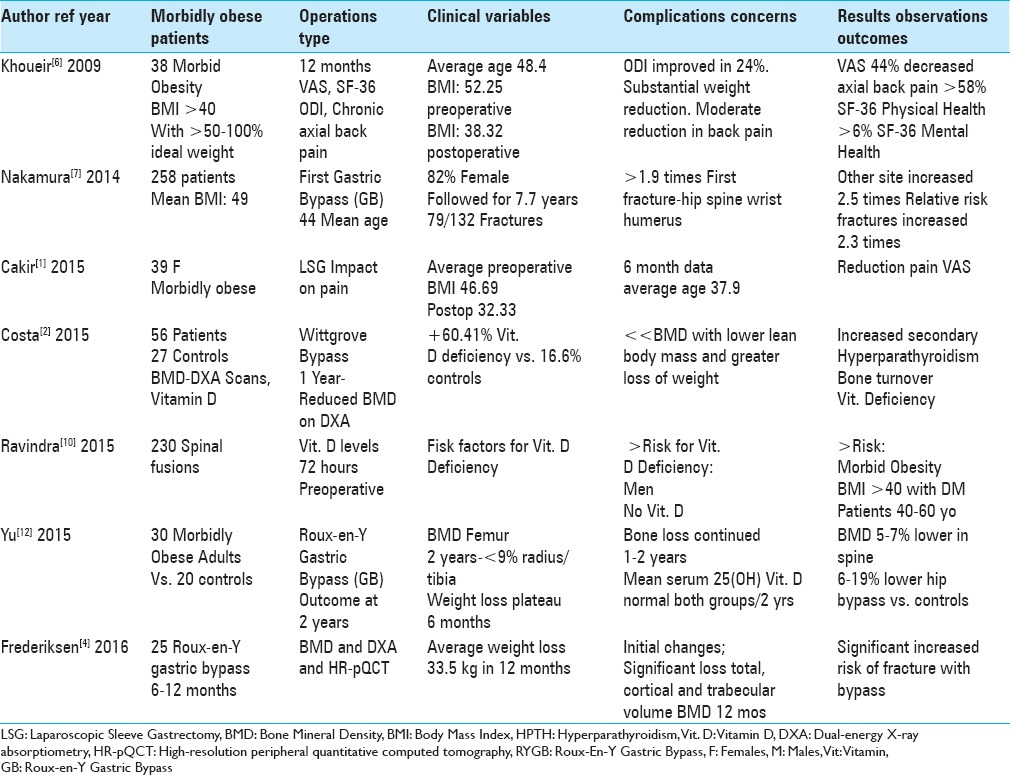
Bariatric bypass procedures result not only in marked weight loss/reduction in muscle mass in the first postoperative year, but also in significant vitamin D deficiency and progressive loss of BMD continuing into the second postoperative year.[2,4,7,12] The latter may result in osteopenia/osteoporosis that contributes to a heighted risk of fractures, including to the lumbar spine. In 2014, Nakamura et al. documented that bariatric surgery increased the risk of osteoporosis and skeletal fractures when they evaluated 258 patients undergoing gastric bypasses (94%; 1985–2004) [Table 1].[7] The average preoperative BMI was 49.0 ± 8.4 kg/m2; 82% (212) were females averaging 44 years of age, and were followed-up for an average of 7.7 years (range, 6 days to 25 years). Notably, 79 patients experienced 132 fractures; the overall risk of fractures was 2.3 times the norm, and involved the hip, spine, wrist, or humerus. Costa et al. (2015) similarly found that bariatric surgery (Wittgrove technique: 1-year evaluation) resulted in 56 patients (vs. 27 controls) experiencing a greater reduction of BMD, greater Vitamin D deficiency, increased bone turnover documented on Dual-energy X-ray absorptiometry (DXA) scans, and a greater potential risk for fractures [Table 1].[2] They recommended early/immediate treatment with Vitamin D supplementation to avoid reduced lumbar BMD and a 60.41% incidence of vitamin D deficiency vs. a lesser 16.6% incidence found for control group patients.
Table 1.
Impact of bariatric surgery on bone mineral density and spinal complaints
1–2 YEAR CHANGES IN BONE DENSITY AFTER ROUX-EN-Y GASTRIC BYPASS SURGERY
Roux-en-Y gastric bypasses similarly contributed to reductions of BMD and vitamin D deficiency.[4,12] In 2015, Yu et al. evaluated bone density utilizing quantitative computed tomography (QCT) and DEXA at 0–24 months following Roux-en-Y gastric bypass [Table 1].[12] At 24 months, for bypass patients, BMD was 5–7% lower in the spine, and 6-10% lower in the hips compared to control patients. Notably, significant bone loss continued within the second postoperative year, despite stabilization of weight loss after the first year. Nevertheless, mean serum calcium, 25(OH)-vitamin D, and hyperparathyroid (PTH) levels were maintained within the normal range for both groups. Utilizing DXA and high-resolution peripheral quantitative computed tomography (HR-pQCT), Frederiksen et al. in 2016 assessed the 6–12-month impact on bone loss and fracture risk following Roux-en-Y gastric bypass surgery in 25 morbidly obese (15 females, 10 males) patients [Table 1].[4] Patients lost an average of 33.5 ± 12.1 kg (25.8 ± 8.5%) in 12 months, during which time BMD loss in the tibias was also marked, increasing fracture risks.
POTENTIAL BENEFIT OF BARIATRIC SURGERY: IMPROVED AXIAL BACK PAIN
An unanticipated benefit of bariatric surgery, in addition to weight loss, was the potential for alleviating axial back pain in select patients [Table 1].[1,6] Khoueir et al., in 2009, compared preoperative vs. postoperative changes (over 6 months) in chronic axial low back pain for 58 morbidly obese patients undergoing bypass surgery (morbid obesity defined as 50–100% above ideal the body weight or BMI >40 kg/m2). Outcomes analyses revealed a statistically significant mean 44% decrease in axial back pain on the visual analog scale (VAS), an average 58% increase in Short Form-36 (SF-36) physical health, and a significant 24% decrease in the postoperative Oswestry Disability Index (ODI). Cakir et al. in 2015 similarly documented that weight loss resulting from laparoscopic sleeve gastrectomy (LSG) relieved pain (head, neck, shoulder, low back, knee) for 39 (average age of 37.9) severely morbidly obese females [Table 1].[1] Their average preoperative BMIs were 46.49 kg/m2, and postoperative BMIs were 32.33 kg/m2, respectively. Interestingly, for females within the first 6 postoperative months, the extent of pain (VAS scale) was directly proportional to the weight loss.
CONCLUSIONS
As many spine surgeons are increasingly recommending stringent weight loss for morbidly obese patients under consideration for “elective” spine surgery (those with significant neurological/radiographic deficits), patients are increasingly choosing bariatric bypass procedures. Nevertheless, both the morbidly obese patients and their potential surgeons must be aware that these operations not only contribute to significant vitamin D deficiency and decreases in BMD, but may also reduce axial back pain, which may be sufficient in some cases to avoid spine surgery altogether.
Footnotes
REFERENCES
- 1.Çakır T, Oruç MT, Aslaner A, Duygun F, Yardımcı EC, Mayir B, et al. The effects of laparoscopic sleeve gastrectomy on head, neck, shoulder, low back and knee pain of female patients. Int J Clin Exp Med. 2015;8:2668–73. [PMC free article] [PubMed] [Google Scholar]
- 2.Costa TL, Paganotto M, Radominski RB, Kulak CM, Borba VC. Calcium metabolism, vitamin D and bone mineral density after bariatric surgery. Osteoporos Int. 2015;26:757–64. doi: 10.1007/s00198-014-2962-4. [DOI] [PubMed] [Google Scholar]
- 3.Epstein NE. How much medicine do spine surgeons need to know to better select and care for patients? Surg Neurol Int. 2012;3(Suppl 5):S329–49. doi: 10.4103/2152-7806.103866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Frederiksen KD, Hanson S, Hansen S, Brixen K, Gram J, Jørgensen NR, et al. Bone Structural Changes and Estimated Strength After Gastric Bypass Surgery Evaluated by HR-pQCT. Calcif Tissue Int. 2016;98:253–62. doi: 10.1007/s00223-015-0091-5. [DOI] [PubMed] [Google Scholar]
- 5.Higgins DM, Mallory GW, Planchard RF, Puffer RC, Ali M, Gates MJ, et al. Understanding the Impact of Obesity on Short-term Outcomes and In-hospital Costs After Instrumented Spinal Fusion. Neurosurgery. 2016;78:127–32. doi: 10.1227/NEU.0000000000001018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Khoueir P, Black MH, Crookes PF, Kaufman HS, Katkhouda N, Wang MY. Prospective assessment of axial back pain symptoms before and after bariatric weight reduction surgery. Spine J. 2009;9:454–63. doi: 10.1016/j.spinee.2009.02.003. [DOI] [PubMed] [Google Scholar]
- 7.Nakamura KM, Haglind EG, Clowes JA, Achenbach SJ, Atkinson EJ, Melton LJ, 3rd, et al. Fracture risk following bariatric surgery: A population-based study. Osteoporos Int. 2014;25:151–8. doi: 10.1007/s00198-013-2463-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Olsen MA, Mayfield J, Lauryssen C, Polish LB, Jones M, Vest J, et al. Risk factors for surgical site infection in spinal surgery. J Neurosurg. 2003;98(2 Suppl):149–55. [PubMed] [Google Scholar]
- 9.Patel N, Bagan B, Vadera S, Maltenfort MG, Deutsch H, Vaccaro AR, et al. Obesity and spine surgery: Relation to perioperative complications. J Neurosurg Spine. 2007;6:291–7. doi: 10.3171/spi.2007.6.4.1. [DOI] [PubMed] [Google Scholar]
- 10.Ravindra VM, Godzik J, Guan J, Dailey AT, Schmidt MH, Bisson EF et al. Prevalence of Vitamin D Deficiency in Patients Undergoing Elective Spine Surgery: A Cross-Sectional Analysis. World Neurosurg. 2015;83:1114–9. doi: 10.1016/j.wneu.2014.12.031. [DOI] [PubMed] [Google Scholar]
- 11.Vaidya R, Carp J, Bartol S, Ouellette N, Lee S, Sethi A. Lumbar spine fusion in obese and morbidly obese patients. Spine. 2009;34:495–500. doi: 10.1097/BRS.0b013e318198c5f2. [DOI] [PubMed] [Google Scholar]
- 12.Yu EW, Bouxsein ML, Putman MS, Monis EL, Roy AE, Pratt JS, et al. Two-year changes in bone density after Roux-en-Y gastric bypass surgery. J Clin Endocrinol Metab. 2015;100:1452–9. doi: 10.1210/jc.2014-4341. [DOI] [PMC free article] [PubMed] [Google Scholar]


