Abstract
Objective:
To review the impact of the Joint Principle of the Patient Centered Medical Home (PCMH) on hemoglobin A1C (HbA1C) in primary care patients with diabetes.
Methods:
Systematic review of English articles using approximate terms for (1) the 7 principles of the PCMH, (2) primary care, and (3) HbA1C. We included experimental and observational studies. Three authors independently extracted data and obtained summary estimates for concepts with more than 2 high-quality studies.
Results:
Forty-three studies published between 1998 and 2012 met inclusion criteria, 33 randomized and 10 controlled before–after studies. A physician-directed medical practice (principle 2) lowered HbA1C values when utilizing nursing (mean difference [MD] −0.36, 95% confidence interval [CI] −0.43 to −0.28) or pharmacy care management (MD −0.76; 95% CI −0.93 to −0.59). Whole-person orientation (principle 3) also lowered HbA1C (MD −0.72, 95% CI −0.98 to −0.45). Studies of coordinated and integrated care (principle 4) and quality and safety interventions (principle 5) did not consistently lower HbA1C when reviewed in aggregate. We did not identify high-quality studies to make conclusions for personal physician (principle 1), enhanced access (principle 6), and payment (principle 7).
Conclusion:
Our review found individual interventions that reduced the HbA1C by up to 2.0% when they met the definitions set by of the Joint Principles of the PCMH. Two of the principles—physician-led team and whole-person orientation—consistently lowered the HbA1C. Other principles had limited data or made little to no impact. Based on current evidence, PCMH principles differentially influence the HbA1C, and there are opportunities for additional research.
Keywords: quality improvement, patient centered, medical home, disease management
Introduction
The joint principles of the Patient Centered Medical Home (PCMH), collated in 2007 by the American Academy of Pediatrics, American Osteopathic Association, American College of Physicians, and American Academy of Pediatrics, are the framework for structuring and evaluating primary care practice redesign.1,2 The PCMH builds on the Chronic Care Model that guided practice reform in the 1990s. This model improved patient outcomes using registries to guide care delivery, enhancing patient management support, incorporating nonphysicians, and using technology to deliver health care.3–8 Integrating these concepts, the joint principles of the PCMH were defined in 2007 as having (1) a personal physician, (2) a physician-directed medical practice, (3) whole-person orientation, (4) coordinated and integrated care, (5) incorporation of quality and safety, (6) enhanced access, and (7) payment to support the PCMH.
Diabetes is a frequent target for quality improvement initiatives such as the PCMH. Diabetes and its comorbidities are a leading cause of death and disability in the United States. Up to 8.3% of US adults are currently diagnosed with diabetes and another 35% have prediabetes.9 It is a costly chronic disease estimated at about US$174 billion in 2007 alone.10
The PCMH practice transformations, in aggregate, decrease the cost and improve the quality of diabetes care; however, the relative impact of each of the individual principles is less clear.11–14 Studies suggest that there are differential benefits that may depend on the target condition for improvement. In a study of the PCMH principles’ impact on preventive services delivery, having a personal physician, whole-person orientation, enhanced access, and coordination with community programs were most associated with the receipt of preventive services.15 Within the chronic care model, team changes and care management had larger impacts on diabetes control.16–18
Given the current widespread move toward the PCMH model, there is a need to establish which specific strategies drive improvements in disease control.16,18–20 In this article, we review the evidence of each PCMH principle on glycemic control.
Research Design and Methods
Study Identification
Each PCMH principle was cross-referenced using a Medical Subject Heading (MeSH) search to obtain the research synonyms (Table 1). We derived our search terms from the title of the PCMH principle and or the key terms defining the principle. Using a Population, Intervention, Comparison, and Outcome (PICO) format, we combined the synonyms with population—primary care, comparison—usual care, and outcome—hemoglobin A1C (HbA1C). We searched MEDLINE, Cochrane Effective Practice and Organization of Care (EPOC) database, and scanned the reference list of all included studies.
Table 1.
Patient Centered Medical Home Concept Definition/Key Terms.
| PCMH Concept Definition/Key Terms | MeSH Synonym | |
|---|---|---|
| Population | ||
| Primary care | Primary care practice, outpatient, or ambulatory care | Primary care OR ambulatory care OR outpatient |
| Study type | Randomized, controlled before-after studies | Epidemiologic studies OR case control OR cohort study OR cohort analys* OR follow-up study OR observational study OR longitudinal OR retrospective OR cross sectional study |
| Outcome | Measures of diabetes outcomes including fasting or nonfasting glucose and hemoglobin A1C | Glycemic control OR hemoglobin A1C OR A1C OR preprandial capillary plasma glucose OR peak postprandial capillary plasma glucose |
| Comparison | Usual care | |
| Intervention | Concept Definition | Search Term |
| Principle #1 Personal physician | Each patient has an ongoing relationship with a personal physician trained to provide first contact, continuous, and comprehensive care | Care AND continu* AND Patient |
| Principle #2 Physician-directed medical practice | The personal physician leads a team of individuals at the practice level who collectively take responsibility for the ongoing care of patients | Patient care team OR interdisciplinary team OR medical care team |
| Principle #3 Whole-person orientation | The personal physician is responsible for providing for all the patient’s health care needs or taking responsibility for appropriately arranging care with other qualified professionals. This includes care for all stages of life, acute care, chronic care, preventive services, and end-of-life care | Comprehensive health care OR whole-person orientation OR (acute AND chronic) OR prevent* care |
| Principle #4 Coordinated and integrated care | Care is coordinated and/or integrated across all elements of the complex health care system (eg, subspecialty care, hospitals, home health agencies, and nursing homes) and the patient’s community (eg, family, public, and private community based services). Care is facilitated by registries, information technology, health information exchange, and other means to assure that patients get the indicated care when and where they need and want it in a culturally and linguistically appropriate manner | Patient-centered care OR integrat* care OR coordinat* care OR Community Based services OR Registr* OR information technology OR (health information (exchange OR system)) |
| Principle #5 Quality and safety are hallmarks | Quality and safety are hallmarks of the medical home Practices advocate for their patients to support the attainment of optimal, patient-centered outcomes that are defined by a care planning process driven by a compassionate, robust partnership between physicians, patients, and the patient’s family. Evidence-based medicine and clinical decision-support tools guide decision making Physicians in the practice accept accountability for continuous quality improvement through voluntary engagement in performance measurement and improvement Patients actively participate in decision making, and feedback is sought to ensure patients’ expectations are being met Information technology is utilized appropriately to support optimal patient care, performance measurement, patient education, and enhanced communication Practices go through a voluntary recognition process by an appropriate nongovernmental entity to demonstrate that they have the capabilities to provide patient centered services consistent with the medical home model Patients and families participate in quality improvement activities at the practice level | (((Individual OR customized) AND (patient care plan OR patient care planning)) OR (Evidence-based (practice OR medicine)) OR quality improvement) OR performance measure* OR Clinical decision support |
| Principle #6 Enhanced access to care | Enhanced access to care is available through systems such as open scheduling, expanded hours and new options for communication between patients, their personal physician, and practice staff | Health care access OR appointments OR scheduling OR ((patient physician relations OR doctor patient relations) AND technology) OR office hours OR email OR (electronic AND (communication OR access)) OR Web Access OR Web Portal OR enhanced communication |
| Principle #7 Payment | Appropriately recognizes the added value provided to patients who have a patient-centered medical home. The payment structure should be based on the following framework: It should reflect the value of physician and nonphysician staff patient-centered care management work that falls outside of the face-to-face visit It should pay for services associated with coordination of care both within a given practice and between consultants, ancillary providers, and community resources It should support adoption and use of health information technology for quality improvement It should support provision of enhanced communication access such as secure e-mail and telephone consultation It should recognize the value of physician work associated with remote monitoring of clinical data using technology It should allow for separate fee-for-service payments for face-to-face visits (payments for care management services that fall outside of the face-to-face visit, as described previously, should not result in a reduction in the payments for face-to-face visits) It should recognize case mix differences in the patient population being treated within the practice It should allow physicians to share in savings from reduced hospitalizations associated with physician-guided care management in the office setting It should allow for additional payments for achieving measurable and continuous quality improvements | Incentive* pay* OR shared savings OR reimburse* OR compensation |
Abbreviations: MeSH, Medical Subject Heading; PCMH, Patient Centered Medical Home.
We included studies conducted on both type 1 and 2 diabetes occurring in the pediatric or adult primary care populations. We excluded those not published in English, conducted in a specialty care setting, or without HbA1C or plasma glucose as an outcome.
Data Extraction and Analysis
Three authors independently screened the articles for full-text review. We included articles with 2-author agreement and recorded the principle, intervention, reliability of measurements, protection of the control group against contamination, and follow-up period. We used EPOC guidelines, published by the Cochrane Collaboration for systematic reviews of health care interventions to assess the quality of studies and guide data collection.21 These guidelines specify 7 different criteria to judge the quality of randomized controlled and controlled before–after studies.
We extracted baseline and final HbA1C means, mean change, standard deviation, and confidence intervals (CIs). Review Manager (RevMan) [Windows], Version 5.2, Copenhagen, was used to obtain a summary estimate of the intervention effect as a weighted average of the treatment effects with fixed effects.22 We pooled the mean difference (MD) into a summary estimate when we found more than 2 high-quality studies, given our analysis model.
We used GRADE Profiler (GRADEPro) for the summary of estimates table (Table 2).64,65 The GRADE Profiler rating system uses the study design to establish the initial confidence in the estimate, which is then adjusted based on the strength of association, dose response, risk of bias, inconsistency, indirectness, imprecision, and publication bias to derive a high, moderate, or low confidence in the estimate.
Table 2.
Summary of Findings for the Joint Principles of the Patient Centered Medical Home impact on Hemoglobin A1C.
| Illustrative Comparative Risks1 (95% CI) | |||||
|---|---|---|---|---|---|
| Assumed Risk | Corresponding Risk | ||||
| Outcomes | Control | PCMH Principles | No of Participants (Studies) | Quality of the Evidence (GRADE)(2) | References |
| Impact of personal physician on change in A1C (PCMH 1) | Not estimable | Not estimable | 0 (0) | Not estimable | No high-quality studies identified. |
| Impact of nurse care management on change in A1C (PCMH 2.A) Follow-up: mean 15 months Baseline mean A1C of all 5 studies: 8.24 | The mean impact of the control intervention (PCMH 2.A) was −0.37 points | The mean impact of nurse care management on change in A1C (PCMH 2.A) in the intervention groups was 0.36 lower than control (0.43-0.28 lower) | 7174 (5 studiesa) | High b,c | Meta-analysis Dorr et al,17 Aubert et al,23 Mousques et al,24 and Krein et al25 Review Gary et al26 |
| Impact of pharmacist care management on change in A1C (PCMH 2.B) Follow-up: mean 24 months Baseline mean A1C of all 5 studies: 10.06 | The mean impact of the control intervention (PCMH 2.B) was −0.42 points | The mean impact of pharmacist care management on change in A1C (PCMH 2.B) in the intervention groups was 0.76 lower than control (0.93-0.59 lower) | 972 (5 studiesa) | High a,b,c | Meta-analysis Johnson et al,27 Choe et al,28 Neto et al,29 and Salvo et al30 Review Jameson and Baty31 |
| Impact of whole-person orientation on change in A1C (PCMH 3) Follow-up: mean 9 months Baseline mean A1C of 7 (excludes Rocco 2011—not reported) studies: 8.87 | The mean impact of the control intervention (PCMH 3) −0.4 points | The mean impact of whole-person orientation on change in A1C (PCMH 3) in the intervention groups was 0.72 lower than control (0.98-0.45 lower) | 983 (8 studiesa) | High a | Meta-analysis Song et al,32 Hornsten et al,33 Kirsh et al,34 Schillinger et al,35 and Polonsky et al36 Review Naik et al,37 Glasgow et al,38 and Rocco et al39 |
| Impact of care coordination with information technology on change in A1C (PCMH 4.A) Follow-up: mean 9 months | See commentd | See commentd | 1841 (4 studies) | High c,e | Review McCarrier et al,40 Piette et al,41 Shea et al,42 and Stone et al43 |
| Impact of depression integration on change in A1C (PCMH 4.B) Follow-up: mean 9.75 months | See commentd | See commentd | 1631 (6 studies) | Moderate f,g | Review Katon et al,44 Piette et al,45 Pouwer et al,46 Snoek et al,47 Bogner and de Vries,48 and Ismail et al49 |
| Impact of care manager integrated into primary care office (PCMH 4.C) Follow-up: mean 12 months | Single study identified | Single study identified | 545 (1 study) | See commentb | Review Davidson et al50 |
| Impact of self-monitoring of blood glucose integrated with technology on change in A1C (PCMH 5.A) Follow-up: mean 9 months | See commentd | See commentd | 914 (6 studies) | High d | Review Rodriguez-Idigoras et al,51 Istepanian et al,52 Farmer et al,53 Augstein et al,54 and Lim et al55 |
| Impact of clinical decision support for use of clinical practice guidelines on A1C (PCMH 5.B) Follow-up: mean 21 months | See commentd | See commentd | 10287 (7 studiesa) | Moderate f | Review O'Connor et al, 2011,56 Guldberg et al,57 Maclean et al,58 Weitzman et al,59 Benjamin et al,60 Ziemer et al,61 and Holbrook et al62 |
| Impact of use of electronic medical records on change in A1C (PCMH 5.C) Follow-up: mean 48 months | Single study identified | Single study identified | 2556 (1 study) | See commentb | Review O'Connor et al63 |
| Impact of enhanced access on change in A1C (PCMH 6)—not measured | Not estimable | Not estimable | – | Not estimable | No high-quality studies identified |
| Impact of payment on change in A1C (PCMH 7)—not measured | Not estimable | Not estimable | – | Not estimable | No high-quality studies identified |
Abbreviations: CI, Confidence interval; PCMH, Patient Centered Medical Home.
1The basis for the assumed risk (eg, the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI).
2GRADE Working Group grades of evidence: high quality: further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: we are very uncertain about the estimate.
a≥50% RCT.
bObservational study design introduced risk.
cAt least 2 studies had a RR > 2.
dData not pooled due to heterogeneity.
eTwo studies had SD close to or encompassing 0.
fDiffering estimates of effect.
gWide confidence intervals noted.
Results
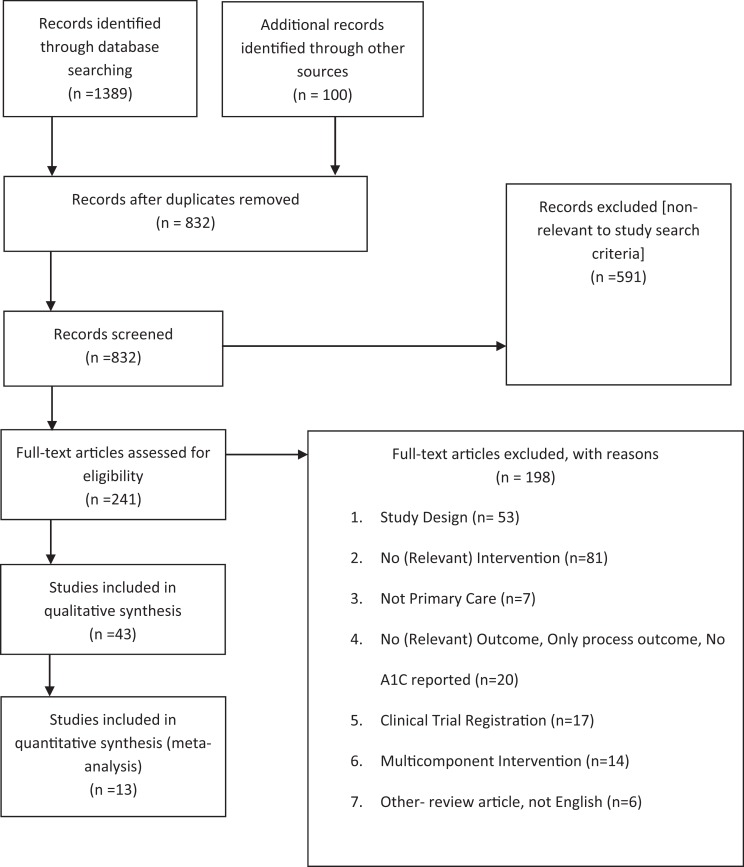
Forty-three studies published between 1998 and 2012 (median 2008; interquartile range 2005-2010) met the inclusion criteria (Figure 1). In all, 33 were randomized and 10 were controlled before–after. The median (interquartile range) follow-up was 12 (6.5-14.25) months, and the average baseline HbA1C was 8.52%.
Figure 1.
Review study identification, selection, and exclusion.
Principle 1: Personal Physician
We found only observational studies without comparison groups for this principle. In Hueston et al., a minimum of 2 visits to the same physician over a 3-year period lowered HbA1C.66 In Dearinger et al, 45% continuity with the same resident physician lowered HbA1C.67 Team continuity was similar to individual continuity.68,69
Principle 2: Physician-Directed Medical Practice
This principle identified studies that used nurses or pharmacists to incorporate care management by (1) triaging patients based on glycemic control, (2) developing collaborative plans, (3) providing education and self-management training, (4) reviewing medications, and (5) modifying patient management.
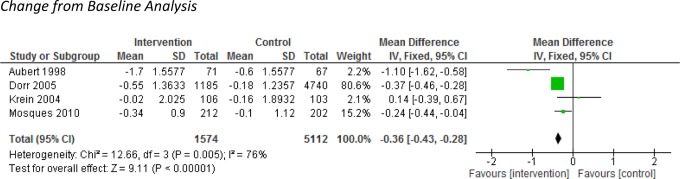
2.A Nursing
Four studies of a nurse care manager collectively lowered the HbA1C significantly more than controls (MD −0.36, 95% CI −0.43 to −0.28) from an average baseline of 8.31 (Figure 2).17,23–25 One study included a community health worker with the nurse care manager but had no impact on the HbA1C.26
Figure 2.
Impact of nurse care management on change in A1C (Patient Centered Medical Home [PCMH] 2.A).
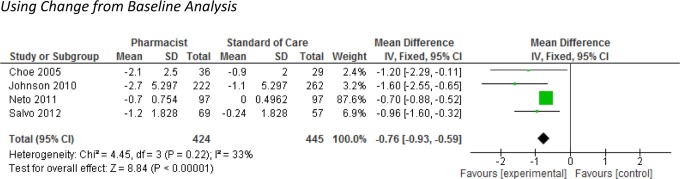
2.B Pharmacists
Four studies of pharmacist care management collectively reduced the HbA1C when compared to the control intervention (MD −0.76, 95% CI −0.93 to −0.59) from a baseline of 9.81 (Figure 3).27–30 Jameson et al had no impact on the HbA1C from a baseline of at least 9 and was excluded from the analysis because it reported skewed data.31
Figure 3.
Impact of pharmacist care manager on change in A1C (Patient Centered Medical Home [PCMH] 2.B).
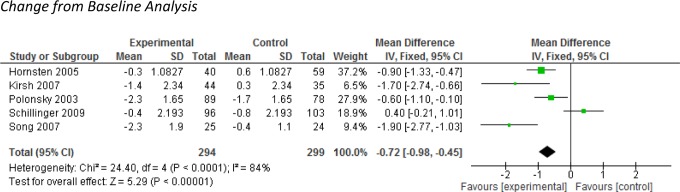
Principle 3: Whole-Person Orientation
The studies we retrieved for whole-person orientation were of physician-led interventions addressing lifestyle modification using behavior theory to enhance patients’ self-efficacy, goal setting, nutrition, physical activity, and psychological wellness. Five such studies collectively lowered the HbA1C significantly compared to controls (MD −0.72, 95% CI −0.98 to −0.45) from an average baseline of 9.02 (Figure 4).32–36 Naik et al found reductions in the HbA1C but did not report enough data to be included in the analysis.37 In Rocco et al, physicians and patients using a care plan to set goals lowered the HbA1C by 0.35 points, but the baseline HbA1C was not reported.39 In Glasgow et al, an internet-based self-managed lifestyle program with or without social contact did not reduce the HbA1C.38
Figure 4.
Impact of whole-person orientation on change in A1C (Patient Centered Medical Home [PCMH] 3).
Principle 4: Coordinated and Integrated Care
We identified two major concepts and an additional study during the review for this term.
4.A Care coordination with information technology
Here, four studies used technology enhancements to supplement the care coordination provided by a nurse care manager through telemedicine portals. In Shea et al, nurse care managers used video conferencing and reduced the HbA1C (MD −0.18, 95% CI −0.17 to −0.19) from a baseline of 7.35.42,70 In Stone et al, patients transmitted their blood glucose to trigger care management contact and this reduced the HbA1C (MD −0.9, 95% CI −0.64 to −1.16) from a baseline of 9.6.43 Two smaller studies, one using e-mail and another automated telephone contact, had no impact on the HbA1C.40,41
4.B Depression integration
Diabetes and depression are well-established comorbid conditions.71–74 Two studies provided cognitive behavioral therapy (CBT) and none reduced the HbA1C.45,47 Ismail et al combined CBT with motivational enhancement therapy and reduced the HbA1C (MD −0.45, 95% CI −0.12 to −0.79) from a baseline of 9.6.49 Problem-solving therapy or assessing psychological well-being had no impact on the HbA1C.44,46 In Bogner et al, integrating a care manager for depression and diabetes reduced the HbA1C (MD −1.2, 95%CI −1.56 to −0.84) from a baseline of 7.2.48
4.C Embedded care manager
One study, Davidson et al, examined the integration of an embedded nurse care manger in the primary care practice compared to referring patients to a care manager independent of the practice. Both models reduced the HbA1C by 2.0 points from an average baseline HbA1C of 10.50
Principle 5: Quality and Safety
In this category, we identified multiple subconcepts.
5.A Electronic delivery of blood glucose self-monitoring to physicians
Five studies assessed self-monitoring of blood glucose (SMBG) feedback delivered electronically to the Physician’s office. Of these, two studies delivered results to the clinic with automated responses generated for abnormal values, while one simply delivered the results. None reduced the HbA1C.51–53 Augstein et al and Lim et al combined SMBG with personalized decision support using the patient’s diet and physical activity and lowered the HbA1C by 0.5 (baseline of 7) and 0.4 (baseline of 7.8), respectively.54,55
5.B Clinical decision support
In two studies where physicians received point-of-care recommendations and population feedback, neither lowered the HbA1C.57,58 When both patients and physicians received these data, 1 study reduced the HbA1C by 0.2 points while another did not.59,62 In O'Connor et al and Benjamin et al, collaborative adoption of clinical decision support (CDS) with workflow changes reduced the HbA1C by 0.26 points from a baseline of 8.5 and 0.9 points from a baseline of 9.30, respectively.56,60 In Ziemer et al, the availability of CDS reduced HbA1C only when a provider received individualized feedback about its use.61
5.C Electronic medical documentation
In O'Connor et al, there was no effect of using an electronic version of the medical record on the HbA1C.63
Principle 6: Enhanced Access
We found no high-quality studies for this principle. In 2 descriptive studies, patient–provider electronic messaging users were notably younger and had better control of their HbA1C.75,76 In Morrison et al, a visit frequency of every 2 weeks achieved the fastest control of HbA1C.77 Schectman et al found that for each 10% increase in missed appointments, the odds of poor HbA1C control increased.78
Principle 7: Payment
We found no high-quality studies for this principle. In Kloos et al, in addition to standard fee-for-service, a €25 payment to physicians to identify patients at risk, provide structured patient education, and strengthen patient self-management skills reduced the HbA1C by 0.55 points over 9 years.79,80
Methodological Considerations
Three groups of studies were from the same trial, and only the most relevant study from each group was included in the analysis.42,47,48,54,70,81–84 Of the 33 randomized trials, 5 were cluster randomized of which only Hornsten et al was included in the meta-analysis for PCMH 3.33,57,58,59,56 We included Hornsten et al, given that the authors analyzed their data using hierarchical analysis of variance to account for clustering. We conducted sensitivity analysis by excluding the study and obtained similar results.
Naik et al did not include a standard deviation for the difference in the mean change for the intervention and control, which precluded it from a meta-analysis using the mean difference.37 We conducted a final mean analysis as sensitivity analysis, which did not change the estimate significantly. We used the final mean analysis approach (where the baseline means were similar) to obtain our pooled estimates for all the meta-analysis and obtained similar results. Five studies did not have similar baseline HbA1C between the intervention and the control groups and could not be included in the final mean analysis.17,34,36,37,42
We excluded one study that had a single control and intervention site.85 One study was prone to contamination because the same provider implemented the intervention and the control activities.54 One did not report baseline HbA1C.39 All but 2 of the trials had >80% patient follow-up rates.23,58 The statistical heterogeneity describing the percentage of variation across the studies that were pooled had an I2 range from 33 to 84 (Figures 2 –4).
Discussion
We conducted this review to understand the relative value of individual PCMH practice improvement strategies on the HbA1C of diabetic patients.
Two PCMH principles improved the HbA1C: physician-directed medical care with nursing or pharmacist care management (principle 2) and whole-person orientation with lifestyle modification support (principle 3). Both principles emphasize a team approach to patient care with the inclusion of the patient as a member of the health care team. They also highlight the value of the expanded roles and skills of both physicians and nonphysician team members.
The review for coordinated and integrated care (principle 4) and quality and safety (principle 5) each had more than five robust studies researching their impact; however, variability in the way these concepts were implemented limited the collective interpretation of results. Nevertheless, we noted the importance of personalization. When personalization was combined with information technology (principle 4.A), electronic reporting of patients’ self-monitored blood glucose (principle 5), or the adoption of CDS tools (principle 5) by health professionals, the studies reported lowered HbA1Cs.
Several concepts were identified, which require further research to determine their direct effect on health outcomes. Although not supported by rigorous studies, a personal physician (principle 1) seems associated with lower HbA1C, an effect that may extend to a team of physicians.68,69 Enhanced access (principle 6) and payment (principle 7) may also improve diabetes outcomes.16,18,20
The impact of these interventions on the HbA1C ranged from a 0.18% to a 2% reduction and none of the studies reviewed worsened the HbA1C. This is important because a 1% reduction in HbA1C levels has been associated with a 37% decrease in the risk of microvascular complications and a 21% reduction in death, making the PCMH a key component in attaining optimal patient outcomes.86
A major limitation of this study is the omission of some potentially relevant studies. To operationalize the PCMH principles, we stayed true to the concept definitions. This undoubtedly limited our search results but was important because current PCMH efforts build on the principles.87–90 Another limitation is the heterogeneity of the studies, which was seen with the different approaches to implementing the PCMH concepts, baseline HbA1C, length of follow-up, and study size. We performed subgroup analysis to address this, collating the studies that appeared to measure the same concepts. A third limitation is the possible regression to the mean effect with most studies having a baseline HbA1C higher than 8%.16
Despite these limitations, our findings are consistent with studies that have examined the effects of health care delivery changes in diabetes outcomes. In the review by Renders et al, interventions that expanded nursing roles or involved patients, improved outcomes.18 Estimates of the effects of team change interventions by Shojania et al ranged from 0.3% to 0.8%, which is similar to our findings for principle 2.16 Similarly, Ferrante et al described the relational PCMH principles of a personal physician and whole-person orientation as having a stronger correlation with the delivery of preventive services.15 These relational principles are core to primary care and reflect the 1994 IOM definition of primary care as providing integrated care and addressing a large majority of personal health care needs while developing partnership with patients.
Various evaluations show that the PCMH practice transformation process improves glycemic control in diabetic patients, and our review suggests that the PCMH principles of physician-directed team care (principle 2) and whole-person orientation (principle 3) are most influential.
Acknowledgments
The authors acknowledge Amy Allison, MLS, AHIP, Head of Clinical Informationist Services, Woodruff Health Sciences Center Library, Emory University.
Author Biographies
Toyosi O. Morgan, MD, MPH, MBA, is board certified in family medicine and preventive medicine and is an Assistant Professor in the Emory University Department of Family and Preventive Medicine where she also serves as Director for the Preventive Medicine Residency program. Dr. Morgan leads primary care providers, staff, residents and students to leverage ongoing health system changes to achieve improved patient outcomes while developing training and practice models for replication
Darcie L. Everett, MD, MPH, is board certified in internal medicine, pediatrics and preventive medicine and is a Medical Officer practicing public health in Maryland. Her current interests are maternal and child health and vaccine preventable diseases.
Anne L. Dunlop, MD, MPH, is board certified in family medicine and preventive medicine and is an Associate Professor in the Emory University Department of Family and Preventive Medicine and the Office of Academic Advancement of the Emory University Nell Hodgson Woodruff School of Nursing. Dr. Dunlop has experience designing and conducting primary care health services and clinical research in public and private clinic settings and epidemiologic analyses and health policy research to better understand the impact of health policies on primary care utilization and health outcomes.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. The Patient Centered Medical Home. History, Seven Core Features, Evidence and Transformational Change. Washington, DC: Center for Policy Studies in Family Medicine and Primary Care; Robert Graham Center; 2007. Web site http://www.aafp.org/online/etc/medialib/aafp_org/documents/about/pcmh.Par.0001.File.dat/PCMH.pdf. Accessed August 28, 2013. [Google Scholar]
- 2. Bojadzievski T, Gabbay RA. Patient-centered medical home and diabetes. Diabetes Care. 2011;34 (4):1047–1053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Nutting PA, Dickinson WP, Dickinson LM, et al. Use of chronic care model elements is associated with higher-quality care for diabetes. Ann Fam Med. 2007;5 (1):14–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Wagner EH. Improving chronic illness care: translating evidence into action. Health Aff. 2001;20 (6):64–78. [DOI] [PubMed] [Google Scholar]
- 5. Coleman K, Austin BT, Brach C, Wagner EH. Evidence on the chronic care model in the new millennium. Health Aff (Millwood). 2009;28 (1):75–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Gabbay RA, Bailit MH, Mauger DT, Wagner EH, Siminerio L. Multipayer patient-centered medical home implementation guided by the chronic care model. Jt Comm J Qual Patient Saf. 2011;37 (6):265–273. [DOI] [PubMed] [Google Scholar]
- 7. Barcelo A, Cafiero E, de Boer M, et al. Using collaborative learning to improve diabetes care and outcomes: the VIDA project. Prim Care Diabetes. 2010;4 (3):145–153. [DOI] [PubMed] [Google Scholar]
- 8. Hariharan J, Tarima S, Azam L, Meurer J. Chronic care model as a framework to improve diabetes care at an academic internal medicine faculty-resident practice. J Ambul Care Manage. 2014;37 (1):42–50. [DOI] [PubMed] [Google Scholar]
- 9. Centers for Disease Control and Prevention. National Diabetes Fact Sheet: National Estimates and General Information on Diabetes and Prediabetes in the United States, 2011. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention; 2011. [Google Scholar]
- 10. National Healthcare Quality Report. AHRQ Publication No. 12-0005; 2012; Web site http://www.ahrq.gov/research/findings/nhqrdr/nhqr11/nhqr11.pdf. Published March 2012. Accessed July 21, 2014.
- 11. Nielsen M LB, Zema C, Hacker T, Grundy P. Benefits of Implementing the Primary Care Patient-Centered Medical Home: A Review of Cost & Quality Results, 2012, Patient-Centered Primary Care Collaborative; 2012. Web site http://www.pcpcc.org/guide/benefits-implementing-primary-care-medical-home#sthash.tiGKFisR.dpuf. Published September 2013. Accessed August 29, 2013.
- 12. Steiner BD, Denham AC, Ashkin E, Newton WP, Wroth T, Dobson LA., Jr Community care of North Carolina: improving care through community health networks. Ann Fam Med. 2008;6 (4):361–367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Phillips RL, Jr, Bronnikov S, Petterson S, et al. Case study of a primary care-based accountable care system approach to medical home transformation. J Ambul Care Manage. 2011;34 (1):67–77. [DOI] [PubMed] [Google Scholar]
- 14. Takach M. Reinventing Medicaid: state innovations to qualify and pay for patient-centered medical homes show promising results. Health Aff (Millwood). 2011;30 (7):1325–1334. [DOI] [PubMed] [Google Scholar]
- 15. Ferrante JM, Balasubramanian BA, Hudson SV, Crabtree BF. Principles of the patient-centered medical home and preventive services delivery. Ann Fam Med. 2010;8 (2):108–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Shojania KG, Ranji SR, McDonald KM, et al. Effects of quality improvement strategies for type 2 diabetes on glycemic control: a meta-regression analysis. JAMA. 2006;296 (4):427–440. [DOI] [PubMed] [Google Scholar]
- 17. Dorr DA, Wilcox A, Donnelly SM, Burns L, Clayton PD. Impact of generalist care managers on patients with diabetes. Health Serv Res. 2005;40 (5 pt 1):1400–1421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Renders CM, Valk GD, Griffin SJ, Wagner EH, Eijk Van JT, Assendelft WJ. Interventions to improve the management of diabetes in primary care, outpatient, and community settings: a systematic review. Diabetes Care. 2001;24 (10):1821–1833. [DOI] [PubMed] [Google Scholar]
- 19. Schouten LM, Hulscher ME, van Everdingen JJ, Huijsman R, Niessen LW, Grol RP. Short- and long-term effects of a quality improvement collaborative on diabetes management. Implementat Sci. 2010;5:94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Weingarten SR, Henning JM, Badamgarav E, et al. Interventions used in disease management programmes for patients with chronic illness—which ones work? Meta-analysis of published reports. BMJ. 2002;325 (7370):925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Effective Practice and Organisation of Care (EPOC). EPOC resources for review authors. 2013; Web site http://epocoslo.cochrane.org/epoc-specific-resources-review-authors. Accessed August 28, 2013.
- 22. Borenstein M, Hedges LV, Higgins JPT, Rothstein HR. Introduction to Meta-Analysis. Hoboken, NJ: John Wiley & Sons, Ltd, 2009: ISBN: 978-0-470-05724-7. [Google Scholar]
- 23. Aubert RE, Herman WH, Waters J, et al. Nurse case management to improve glycemic control in diabetic patients in a health maintenance organization. A randomized, controlled trial. Ann Intern Med. 1998;129 (8):605–612. [DOI] [PubMed] [Google Scholar]
- 24. Mousques J, Bourgueil Y, Le Fur P, Yilmaz E. Effect of a French experiment of team work between general practitioners and nurses on efficacy and cost of type 2 diabetes patients care. Health Policy (Amsterdam, Netherlands). 2010;98 (2-3):131–143. [DOI] [PubMed] [Google Scholar]
- 25. Krein SL, Klamerus ML, Vijan S, et al. Case management for patients with poorly controlled diabetes: a randomized trial. Am J Med. 2004;116 (11):732–739. [DOI] [PubMed] [Google Scholar]
- 26. Gary TL, Batts-Turner M, Yeh HC, et al. The effects of a nurse case manager and a community health worker team on diabetic control, emergency department visits, and hospitalizations among urban African Americans with type 2 diabetes mellitus: a randomized controlled trial. Arch Intern Med. 2009;169 (19):1788–1794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Johnson KA, Chen S, Cheng IN, et al. The impact of clinical pharmacy services integrated into medical homes on diabetes-related clinical outcomes. Ann Pharmacother. 2010;44 (12):1877–1886. [DOI] [PubMed] [Google Scholar]
- 28. Choe HM, Mitrovich S, Dubay D, Hayward RA, Krein SL, Vijan S. Proactive case management of high-risk patients with type 2 diabetes mellitus by a clinical pharmacist: a randomized controlled trial. Am J Manag Care. 2005;11 (4):253–260. [PubMed] [Google Scholar]
- 29. Neto PR, Marusic S, de Lyra Junior DP, et al. Effect of a 36-month pharmaceutical care program on the coronary heart disease risk in elderly diabetic and hypertensive patients. J Pharm Pharm Sci. 2011;14 (2):249–263. [DOI] [PubMed] [Google Scholar]
- 30. Salvo MC, Brooks AM. Glycemic control and preventive care measures of indigent diabetes patients within a pharmacist-managed insulin titration program vs standard care. Ann Pharmacother. 2012;46 (1):29–34. [DOI] [PubMed] [Google Scholar]
- 31. Jameson JP, Baty PJ. Pharmacist collaborative management of poorly controlled diabetes mellitus: a randomized controlled trial. Am J Manag Care. 2010;16 (4):250–255. [PubMed] [Google Scholar]
- 32. Song MS, Kim HS. Effect of the diabetes outpatient intensive management programme on glycaemic control for type 2 diabetic patients. J Clin Nurs. 2007;16 (7):1367–1373. [DOI] [PubMed] [Google Scholar]
- 33. Hornsten A, Lundman B, Stenlund H, Sandstrom H. Metabolic improvement after intervention focusing on personal understanding in type 2 diabetes. Diabetes Res Clin Pract. 2005;68 (1):65–74. [DOI] [PubMed] [Google Scholar]
- 34. Kirsh S, Watts S, Pascuzzi K, et al. Shared medical appointments based on the chronic care model: a quality improvement project to address the challenges of patients with diabetes with high cardiovascular risk. Qual Saf Health Care. 2007;16 (5):349–353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Schillinger D, Handley M, Wang F, Hammer H. Effects of self-management support on structure, process, and outcomes among vulnerable patients with diabetes: a three-arm practical clinical trial. Diabetes Care. 2009;32 (4):559–566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Polonsky WH, Earles J, Smith S, et al. Integrating medical management with diabetes self-management training: a randomized control trial of the Diabetes Outpatient Intensive Treatment program. Diabetes Care. 2003;26 (11):3048–3053. [DOI] [PubMed] [Google Scholar]
- 37. Naik AD, Palmer N, Petersen NJ, et al. Comparative effectiveness of goal setting in diabetes mellitus group clinics: randomized clinical trial. Arch Intern Med. 2011;171 (5):453–459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Glasgow RE, Kurz D, King D, et al. Twelve-month outcomes of an Internet-based diabetes self-management support program. Patient Educ Counsel. 2012;87 (1):81–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Rocco N, Scher K, Basberg B, Yalamanchi S, Baker-Genaw K. Patient-centered plan-of-care tool for improving clinical outcomes. Qual Manag Health Care. 2011;20 (2):89–97. [DOI] [PubMed] [Google Scholar]
- 40. McCarrier KP, Ralston JD, Hirsch IB, et al. Web-based collaborative care for type 1 diabetes: a pilot randomized trial. Diabetes Technol Ther. 2009;11 (4):211–217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Piette JD, Weinberger M, Kraemer FB, McPhee SJ. Impact of automated calls with nurse follow-up on diabetes treatment outcomes in a Department of Veterans Affairs Health Care System: a randomized controlled trial. Diabetes Care. 2001;24 (2):202–208. [DOI] [PubMed] [Google Scholar]
- 42. Shea S, Weinstock RS, Starren J, et al. A randomized trial comparing telemedicine case management with usual care in older, ethnically diverse, medically underserved patients with diabetes mellitus. J Am Med Inform Assoc. 2006;13 (1):40–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Stone RA, Rao RH, Sevick MA, et al. Active care management supported by home telemonitoring in veterans with type 2 diabetes: the DiaTel randomized controlled trial. Diabetes Care. 2010;33 (3):478–484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Katon WJ, Von Korff M, Lin EH, et al. The Pathways Study: a randomized trial of collaborative care in patients with diabetes and depression. Arch Gen Psychiatry. 2004;61 (10):1042–1049. [DOI] [PubMed] [Google Scholar]
- 45. Piette JD, Richardson C, Himle J, et al. A randomized trial of telephonic counseling plus walking for depressed diabetes patients. Med Care. 2011;49 (7):641–648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Pouwer F, Snoek FJ, van der Ploeg HM, Ader HJ, Heine RJ. Monitoring of psychological well-being in outpatients with diabetes: effects on mood, HbA(1c), and the patient's evaluation of the quality of diabetes care: a randomized controlled trial. Diabetes Care. 2001;24 (11):1929–1935. [DOI] [PubMed] [Google Scholar]
- 47. Snoek FJ, van der Ven NC, Twisk JW, et al. Cognitive behavioural therapy (CBT) compared with blood glucose awareness training (BGAT) in poorly controlled Type 1 diabetic patients: long-term effects on HbA moderated by depression. A randomized controlled trial. Diabet Med. 2008;25 (11):1337–1342. [DOI] [PubMed] [Google Scholar]
- 48. Bogner HR, de Vries HF. Integrating type 2 diabetes mellitus and depression treatment among African Americans: a randomized controlled pilot trial. Diabetes Educ. 2010;36 (2):284–292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Ismail K, Maissi E, Thomas S, et al. A randomised controlled trial of cognitive behaviour therapy and motivational interviewing for people with type 1 diabetes mellitus with persistent sub-optimal glycaemic control: a Diabetes and Psychological Therapies (ADaPT) study. Health Technol Assess (Winchester, England). 2010;14(22):1–101, iii–iv. [DOI] [PubMed] [Google Scholar]
- 50. Davidson MB, Blanco-Castellanos M, Duran P. Integrating nurse-directed diabetes management into a primary care setting. Am J Manag Care. 2010;16 (9):652–656. [PubMed] [Google Scholar]
- 51. Rodriguez-Idigoras MI, Sepulveda-Munoz J, Sanchez-Garrido-Escudero R, et al. Telemedicine influence on the follow-up of type 2 diabetes patients. Diabetes Technol Ther. 2009;11 (7):431–437. [DOI] [PubMed] [Google Scholar]
- 52. Istepanian RS, Zitouni K, Harry D, et al. Evaluation of a mobile phone telemonitoring system for glycaemic control in patients with diabetes. J Telemed Telecare. 2009;15 (3):125–128. [DOI] [PubMed] [Google Scholar]
- 53. Farmer AJ, Wade AN, French DP, et al. Blood glucose self-monitoring in type 2 diabetes: a randomised controlled trial. Health Technol Assess (Winchester, England). 2009;13(15):iii–iv, ix,–xi, 1–50. [DOI] [PubMed] [Google Scholar]
- 54. Augstein P, Vogt L, Kohnert KD, Freyse EJ, Heinke P, Salzsieder E. Outpatient assessment of Karlsburg Diabetes Management System-based decision support. Diabetes Care. 2007;30 (7):1704–1708. [DOI] [PubMed] [Google Scholar]
- 55. Lim S, Kang SM, Shin H, et al. Improved glycemic control without hypoglycemia in elderly diabetic patients using the ubiquitous healthcare service, a new medical information system. Diabetes Care. 2011;34 (2):308–313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. O'Connor PJ, Sperl-Hillen JM, Rush WA, et al. Impact of electronic health record clinical decision support on diabetes care: a randomized trial. Ann Fam Med. 2011;9 (1):12–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Guldberg TL, Vedsted P, Kristensen JK, Lauritzen T. Improved quality of type 2 diabetes care following electronic feedback of treatment status to general practitioners: a cluster randomized controlled trial. Diabetic Med. 2011;28 (3):325–332. [DOI] [PubMed] [Google Scholar]
- 58. Maclean CD, Gagnon M, Callas P, Littenberg B. The Vermont diabetes information system: a cluster randomized trial of a population based decision support system. J Gen Intern Med. 2009;24 (12):1303–1310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Weitzman S, Greenfield S, Billimek J, et al. Improving combined diabetes outcomes by adding a simple patient intervention to physician feedback: a cluster randomized trial. Isr Med Assoc J. 2009;11 (12):719–724. [PubMed] [Google Scholar]
- 60. Benjamin EM, Schneider MS, Hinchey KT. Implementing practice guidelines for diabetes care using problem-based learning. A prospective controlled trial using firm systems. Diabetes Care. 1999;22 (10):1672–1678. [DOI] [PubMed] [Google Scholar]
- 61. Ziemer DC, Doyle JP, Barnes CS, et al. An intervention to overcome clinical inertia and improve diabetes mellitus control in a primary care setting: Improving Primary Care of African Americans with Diabetes (IPCAAD) 8. Arch Intern Med. 2006;166 (5):507–513. [DOI] [PubMed] [Google Scholar]
- 62. Holbrook A, Thabane L, Keshavjee K, et al. Individualized electronic decision support and reminders to improve diabetes care in the community: COMPETE II randomized trial. CMAJ. 2009;181 (1-2):37–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. O'Connor PJ, Crain AL, Rush WA, et al. Impact of an electronic medical record on diabetes quality of care. Ann Fam Med. 2005;3 (4):300–306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Review Manager (RevMan) (for Windows) [computer program]. Version 5.2 Copenhagen: The Cochrane Collaboration; 2012. [Google Scholar]
- 65. GRADEpro (for Windows). Version 3.2 [computer program]. Jan Brozek, Andrew Oxman, Holger Schünemann; 2008. [Google Scholar]
- 66. Hueston WJ. Does having a personal physician improve quality of care in diabetes? J Am Board Fam Med. 2010;23 (1):82–87. [DOI] [PubMed] [Google Scholar]
- 67. Dearinger AT, Wilson JF, Griffith CH, Scutchfield FD. The effect of physician continuity on diabetic outcomes in a resident continuity clinic. J Gen Intern Med. 2008;23 (7):937–941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Litaker D, Ritter C, Ober S, Aron D. Continuity of care and cardiovascular risk factor management: does care by a single clinician add to informational continuity provided by electronic medical records? Am J Manag Care. 2005;11 (11):689–696. [PubMed] [Google Scholar]
- 69. Manious AG, Koopman RJ, Gill JM, Baker R, Pearson WS. Relationship between continuity of care and diabetes control: evidence from the third National Health and Nutrition Examination Survey. Am J Public Health. 2004;94 (1):66–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Shea S, Weinstock RS, Teresi JA, et al. A randomized trial comparing telemedicine case management with usual care in older, ethnically diverse, medically underserved patients with diabetes mellitus: 5 year results of the IDEATel study. J Am Med Inform Assoc. 2009;16 (4):446–456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Golden SH, Lazo M, Carnethon M, et al. Examining a bidirectional association between depressive symptoms and diabetes. JAMA. 2008;299 (23):2751–2759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. de Groot M, Jacobson AM, Samson JA, Welch G. Glycemic control and major depression in patients with type 1 and type 2 diabetes mellitus. J Psychosom Res. 1999;46 (5):425–435. [DOI] [PubMed] [Google Scholar]
- 73. Gavard JA, Lustman PJ, Clouse RE. Prevalence of depression in adults with diabetes. An epidemiological evaluation. Diabetes Care. 1993;16 (8):1167–1178. [DOI] [PubMed] [Google Scholar]
- 74. Anderson RJ, Freedland KE, Clouse RE, Lustman PJ. The prevalence of comorbid depression in adults with diabetes: a meta-analysis. Diabetes Care. 2001;24 (6):1069–1078. [DOI] [PubMed] [Google Scholar]
- 75. Harris LT, Haneuse SJ, Martin DP, Ralston JD. Diabetes quality of care and outpatient utilization associated with electronic patient–provider messaging: a cross-sectional analysis. Diabetes Care. 2009;32 (7):1182–1187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Tenforde M, Nowacki A, Jain A, Hickner J. The association between personal health record use and diabetes quality measures. J Gen Intern Med. 2012;27 (4):420–424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Morrison F, Shubina M, Turchin A. Encounter frequency and serum glucose level, blood pressure, and cholesterol level control in patients with diabetes mellitus. Arch Intern Med. 2011;171 (17):1542–1550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Schectman JM, Schorling JB, Voss JD. Appointment adherence and disparities in outcomes among patients with diabetes. J Gen Intern Med. 2008;23 (10):1685–1687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Calvert M, Shankar A, McManus RJ, Lester H, Freemantle N. Effect of the quality and outcomes framework on diabetes care in the United Kingdom: retrospective cohort study. BMJ. 2009;338:b1870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Kloos C, Muller N, Wolf G, Hartmann P, Lehmann T, Müller UA. Better HbA1c and blood pressure control in patients with diabetes mellitus treated at a primary health care level 10 years after initiation of a diabetes quality improvement program. Exp Clin Endocrinol. 2011;119 (8):459–462. [DOI] [PubMed] [Google Scholar]
- 81. van der Ven NC, Hogenelst MH, Tromp-Wever AM, et al. Short-term effects of cognitive behavioural group training (CBGT) in adult Type 1 diabetes patients in prolonged poor glycaemic control. A randomized controlled trial. Diabet Med. 2005;22 (11):1619–1623. [DOI] [PubMed] [Google Scholar]
- 82. Augstein P, Vogt L, Kohnert KD, Heinke P, Salzsieder E. Translation of personalized decision support into routine diabetes care. J Diabetes Sci Technol. 2010;4 (6):1532–1539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Salzsieder E, Augstein P. The Karlsburg Diabetes Management System: translation from research to eHealth application. J Diabetes Sci Technol. 2011;5 (1):13–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Bogner HR, Morales KH, de Vries HF, Cappola AR. Integrated management of type 2 diabetes mellitus and depression treatment to improve medication adherence: a randomized controlled trial. Ann Fam Med. 2012;10 (1):15–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Maislos M, Weisman D. Multidisciplinary approach to patients with poorly controlled type 2 diabetes mellitus: a prospective, randomized study. Acta Diabetol. 2004;41 (2):44–48. [DOI] [PubMed] [Google Scholar]
- 86. Stratton IM, Adler AI, Neil HA, et al. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. BMJ. 2000;321 (7258):405–412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. The Joint Commission. Primary Care Medical Home. Web site http://www.jointcommission.org/accreditation/pchi.aspx. Accessed July 21, 2014.
- 88. Accreditation Association for Ambulatory Health Care. Medical Home. Web site http://www.aaahc.org/en/accreditation/primary-care-medical-home/. Accessed July 17, 2014.
- 89. National Committee for Quality Assurance. NCQA Patient-Centered Medical Home Recognition; 2014. Web site http://www.ncqa.org/Programs/Recognition/Practices/PatientCenteredMedicalHomePCMH.aspx. Accessed July 2014, 2014. [DOI] [PubMed]
- 90. Utilization Review Accreditation Commission. URAC’s Patient Centered Medical Home program. Web site https://www.urac.org/accreditation-and-measurement/accreditation-programs/all-programs/patient-centered-medical-home/. Accessed July 21, 2014.