Abstract
Aim:
Ocimum basilicum L (Lamiaceae) is used as a traditional remedy for different ailments, including diabetes mellitus. This study investigated the antidiabetic effects of an extract of aerial parts of O. basilicum.
Methods:
Antihyperglycemic effect of the extract was determined by its effects on α-amylase and α-glucosidase in vitro, while antidiabetic properties were studied in alloxan induced diabetic rats treated for 28 days with extract and compared to those treated with oral metformin (150 mg/kg). The study and analysis was conducted between 2014 and 2015.
Results:
The treatment with 100 and 200 mg/kg extract significantly (P < 0.05) reduced fasting blood glucose concentration and slightly increased mean body weight in treated groups. Oral glucose tolerance was also significantly (P < 0.05, 0.001) improved in 100 and 400 mg/kg extract-treated groups. The extract caused a dose-dependent increase in liver glycogen content, while it decreased alanine transferase (18.9-30.56%) and aspartate transferase (6.48-34.3%) levels in a non-dose-dependent manner. A dose of 100 mg/kg also reduced serum cholesterol and triglycerides by 19.3 and 39.54%, compared to a 2.6% reduction of cholesterol seen in the metformin-treated group. The extract was observed to produce significant (P < 0.001) concentration-dependent inhibition of α-glucosidase (35.71-100%) and also α-amylase (23.55-81.52%), with estimated inhibitory concentration values of 1.62 and 3.86 mg/mL, respectively.
Conclusions:
The antidiabetic properties of the extract may be due to its ability to suppress endogenous glucose release, inhibit glycogenolysis and/or stimulate glycogenesis.
KEY WORDS: Antidiabetic, diabetes mellitus, hyperglycemia, Ocimum basilicum
INTRODUCTION
The term diabetes mellitus describes a metabolic disorder of multiple etiology characterized by chronic hyperglycemia with disturbances of carbohydrate, fat, and protein metabolism resulting from defects in insulin secretion, insulin action, or both [1]. The incidence of diabetes has risen rapidly in low and middle-income countries, due to factors such as population growth, urbanization, and increasing the prevalence of obesity due to dietary changes and physical inactivity [2]. Type II diabetes mellitus (Type II DM) is the most common form of diabetes, caused by a combination of factors, including insulin resistance, a condition in which the body’s muscle, fat, and liver cells do not use insulin effectively and develops when the body can no longer produce enough insulin to compensate for the impaired ability to use insulin. This type of diabetes comprises the majority of adult diabetic patients around the world and is still on the increase. Long-term effects of diabetes mellitus include progressive development of the specific complications of retinopathy with potential blindness, nephropathy that may lead to renal failure, and/or neuropathy. Management of Type II DM involves nonpharmacological measures such as dietary modification and exercise and pharmacological approaches with oral antidiabetics, aimed at controlling postprandial hyperglycemia and improving insulin action [3]. These oral hypoglycemic drugs possess a distinct mechanism of actions which enables them to be used independently or in combination. In many developing countries, however, access to these drugs and affordability may be contending issues in proper therapy and management. In these countries, traditional herbal medicines are popular and play an important role in DM management [4]. Recent reports have highlighted different plant extracts screened for antidiabetic activity, which were shown to improve tissue insulin sensitivity and inhibit carbohydrate metabolizing enzymes [5,6]. Extracts of Ocimum basilicum L (Lamiaceae) also commonly known as “Holy basil” have been reported to possess different pharmacological effects, including blood glucose lowering and hepatoprotective properties [7,8]. The plant is widely used in traditional medicine in different cultures and also known for its culinary uses. Reported phytochemical constituents found in O. basilicum extract include linalool, methylchavikol, methyl cinnamate, linolen, rosmarinic acid, citral, eugenol, and geraniol [9-11]. A previous in vitro study showed that aqueous extract of the plant inhibited porcine α-amylase and rat intestinal sucrase and maltase [7]. In an earlier study, the blood glucose-lowering effects of oral administration of a dichloromethane:methanol (1:1) extract and solvent fractions of aerial parts of O. basilicum in diabetic rats were reported [12]. Presently, we investigated the effects of repeated oral administration of the extract on blood glucose control and hepatic glucose mobilization in alloxan-diabetic rats as well as carbohydrate metabolizing enzymes in vitro to propose some likely mechanisms of its antidiabetic activity.
MATERIALS AND METHODS
Materials
Drugs, reagents, and solvents
Metformin, dimethyl sulfoxide (DMSO), 3,5- dinitrosalicylic acid, sodium potassium tartrate, O- toluidine, D- maltose, trichloroacetic acid, oxalic acid, phenol, alloxan monohydrate (Sigma-Aldrich), D-glucose (Fluka Chemicals, USA), acetylene chloride, and methanol (BDH, England). Other reagents and solvents were of analytical grade.
Enzymes and substrates
Porcine pancreatic α-amylase (EC 232-565-6), yeast α-glucosidase, soluble potato starch, and p-nitrophenyl-α-D-glucopyranoside, (Sigma-Aldrich, Germany).
Animals
Adult Wistar rats (100-200 g) of both sexes obtained from the animal facility center of the Department of Pharmacology and Toxicology, National Institute for Pharmaceutical Research and Development (NIPRD), Abuja, were used. The rats were housed in steel cages and allowed access to potable water and standard pelleted feed. All animal experiments were in compliance with NIPRD’s standard operating procedures and the National Institute of Health guide for Care and Use of Laboratory Animals [13].
Methods
The entire study and data analysis was conducted between 2014 and 2015.
Collection and Identification of the Plant Material
Aerial parts of O. basilicum were collected between November and February from Suleja, Niger State and identified at NIPRD where a voucher specimen (NIPRD/H/6594) is maintained. The aerial parts were air dried under shade for 2 weeks and the dry material pulverized to coarse powder using an electric hammer mill.
Extraction of Plant Material
A total of 1.2 kg of dry plant material was extracted by cold maceration in a mixture of dichloromethane:methanol (1:1) for 48 h with occasional agitation. After 48 h, the mixture was filtered, and the residue extracted again with fresh solvent and filtered. The combined filtrates were concentrated under vacuum and then dried in a hot water bath maintained at 50°C. The extract was transferred to an airtight container and stored in a refrigerator (4°C) until required.
Thin Layer Chromatography (TLC) and High-performance Liquid Chromatography (HPLC) Fingerprinting of Extract
Pre-coated thin layer chromatographic glass plates were used for TLC analysis. Extract solution was spotted on heat-activated plates and developed in a mobile phase system of ethyl acetate: Methanol (3:2). Detection was done with sulfuric acid/vanillin reagent spray and heat (110°C for 3 min). Conditions for HPLC were as follows: Mobile phase comprising solvent A: 0.2% v/v formic acid, solvent B: Acetonitrile, mode: Linear gradient, flow rate of 0.6 mL/min, injection volume: 20 µL of 500 µg/mL methanol solution of extract, UV detection at 254 nm, and column oven temperature 40°C. The HPLC operating conditions were programed to give the following; at 0 min, solvent B: 20%; 10 min, solvent B: 25%; 20 min, solvent B: 80%; 25 min, solvent B: 20% return to initial condition. The total run time was 25 min.
Pharmacological Studies
Induction of experimental diabetes
About 40 Swiss albino rats were subjected to an overnight fast with free access to drinking water. Diabetes mellitus was induced in on day 0 by a single intraperitoneal injection of freshly prepared alloxan monohydrate solution in distilled water (160 mg/mL). On day 3, the rats were fasted overnight and blood glucose levels measured on day 4 from tail vein blood using a blood glucometer and its corresponding strips (Accu-Chek, Mannheim, Germany). Rats with blood glucose ≥200 mg/dL were considered diabetic and were used for the study.
Experimental Design
The plant extract was reconstituted with distilled water and tween 80 (1% v/v). Diabetic rats were weighed, randomized, and divided into five groups (n = 6). The rats were treated orally for 30 days; Groups 1 and 2 served as controls and received distilled water (5 mL/kg) and metformin (150 mg/kg), respectively. Groups 3-5 received 100, 200, and 400 mg/kg extract. Individual body weight and fasting blood sugar levels of all the rats were measured at weekly interval during the experimental period.
Oral Glucose Tolerance Test
On the 25th day of treatment, the rats were fasted overnight but allowed free access to water. On the 26th day, the rats were treated accordingly, then after 30 min, an oral glucose load of 1.5 g/kg was administered orally. Blood glucose levels were taken immediately and at 30, 60, 90, and 120 min after the glucose load.
Hepatic Glycogen and Serum Biochemistry Determination
On day 30, the rats were euthanized by chloroform inhalation and blood collected using plain sera tubes for biochemical analysis of protein (total protein and albumin), lipids (cholesterol and triglycerides), and hepatic enzymes. The liver of each rat was excised carefully and weighed. 1 g of each liver was cut for assay of hepatic glycogen according to a method described earlier [14]. Following glycogen hydrolysis, the concentration of glucose obtained was determined using a standard calibration plot of glucose obtained using O-toluidine. The absorbance measured at 355 nm and glycogen content was expressed as g/g liver tissue.
α-amylase Inhibition Assay
The assay was performed according to the chromogenic non-preincubation method described by Ali et al. [15] as modified by Okoli et al. [14]. Test incubations were prepared for 1.25-20 mg/mL of extract to study the concentration dependent enzyme inhibition and to calculate the concentration required to inhibit 50% enzyme activity inhibitory concentration (IC50). For each concentration, blank incubations were prepared by replacing the enzyme solution with distilled water, while control incubations were prepared by replacing extract with 120 µL DMSO. All the tests were run in triplicate. Absorbance was measured at 540 nm (Shimadzu UV-160 spectrophotometer, Kyoto, Japan) and net absorbance (A) due to maltose generated was calculated as:
Net absorbance (A) due to maltose generated was calculated as:
A540nm extract =A540nm test-A540nm blank
From the value obtained, maltose generated (%w/v) was calculated from the equation obtained from the maltose standard calibration curve (0.001-0.1% w/v).
The level of inhibition (%) was calculated thus:
Inhibition (%) = 100 - % reaction (at 3 min)
Where: % reaction= mean maltose in sample ×100/mean maltose in control
Alpha Glucosidase Inhibitory Activity Assay
A chromogenic method described previously was used [14]. A mixture of 0.32 mL of extract, 1.6 mL of buffer solution and 0.8 mL of enzyme solution was incubated for 5 min, followed by addition of 800 µL of substrate. Samples were further incubated for 15 min and the reaction stopped by addition of 320 µL of 200 mm sodium carbonate solution. The release of p-nitrophenol generated was measured at 400 nm. Enzyme and extract solutions were substituted with 800 µL buffer solution and 320 µL DMSO in blank and control incubations respectively. All tests were run in triplicate. The level of enzyme inhibition was calculated thus:
Enzyme inhibition (%) = 100 - [((As-Ab)/Ac) ×100]
Where Ac represents the absorbance of the control without test samples, As= sample absorbance and Ab denotes sample blank absorbance.
Statistical Analysis
Data were analyzed using one-way analysis of variance. The results expressed as mean ± standard error in mean and further subjected to LSD post hoc test for multiple comparisons. Differences between means accepted significant at P < 0.05.
RESULTS
Treatment of diabetic rats with 100 and 200 mg/kg doses of extract caused a decrease in fasting blood glucose levels in a non-dose-dependent manner, producing 59.21 and 38.67% decline in plasma glucose levels, respectively, by the end of the study period [P < 0.001 and P < 0.05; Table 1]. The hypoglycemic effect in extract-treated rats was higher than that in metformin-treated rats. Mean body weight of the diabetic rats treated with extract and the diabetic rats treated with metformin was observed to decrease slightly at the end of the study, but this change was statistically insignificant [P > 0.05, Table 2]. Administration of an oral glucose load increased blood glucose to peak levels in all the rats within 30 min and pretreatment with extract suppressed the rise in blood glucose levels. The extract (100 mg/kg) significantly (P < 0.001) decreased the blood glucose level at 120 min by 27.76%. The extract at 400 mg/kg also significantly (P < 0.05) suppressed the postprandial glucose level. The blood glucose lowering effect of extract was only limited to 90 min in the group treated with 200 mg/kg [Table 3]. Treatment with the extract also produced dose-dependent increase in glycogen content of the liver by 7.1 - 37.4% compared to the untreated control [Table 4]. The extract decreased the levels of aspartate aminotransferase and alanine aminotransferase in the diabetic treated groups, in a non-dose-dependent manner [Table 5]. The treatment with 100 mg/kg extract produced slight decrease in the alkaline phosphatase (ALP), total protein, albumin, and cholesterol levels but elicited marked reduction of serum triglycerides [39.54%, Table 5] compared to that caused by metformin.
Table 1.
Effect of extract on fasting blood glucose level in diabetic rats
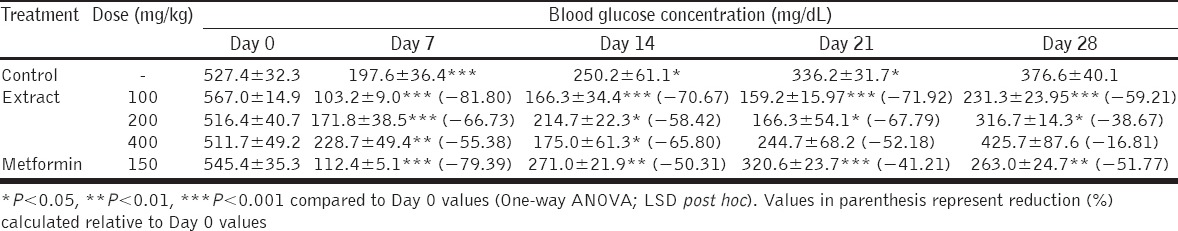
Table 2.
Effect of extract on body weight of diabetic rats
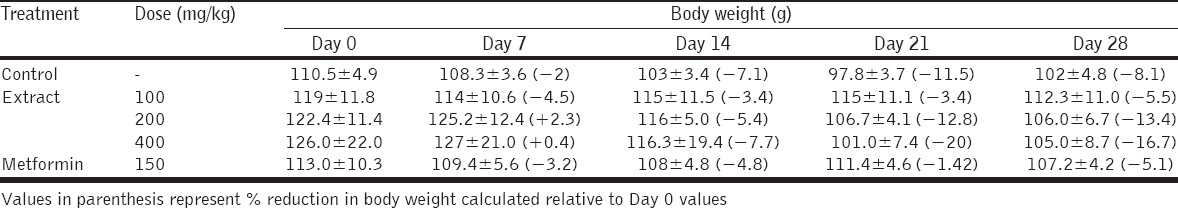
Table 3.
Effect of extract on oral glucose tolerance in diabetic rats
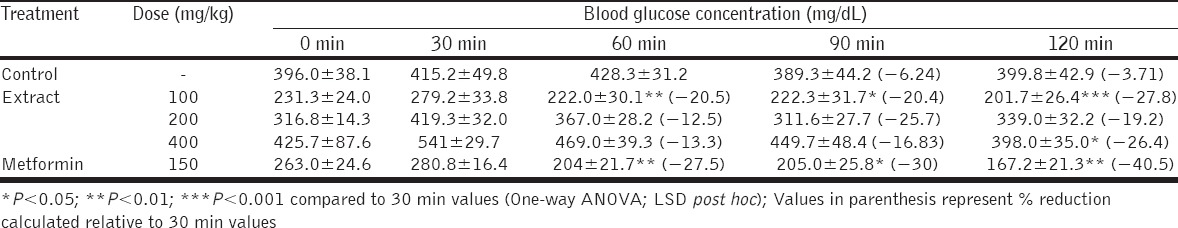
Table 4.
Effect of extract on hepatic glycogen content and liver weight of diabetic rats
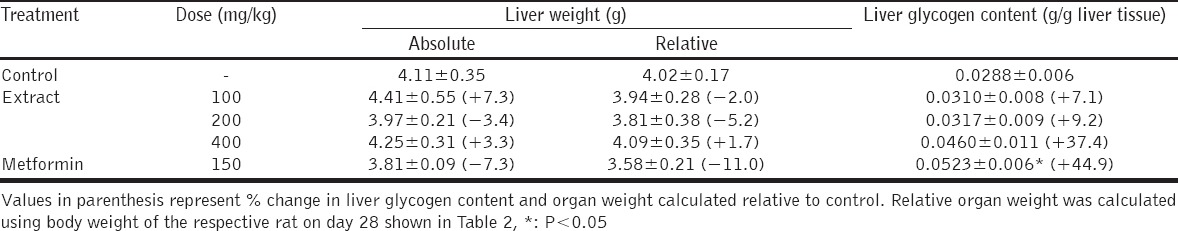
Table 5.
Serum biochemistry of extract-treated diabetic rats
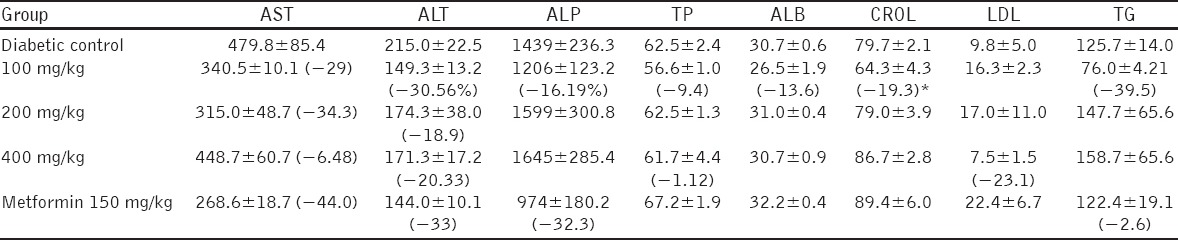
The extract significantly (P < 0.05) inhibited α-glucosidase enzyme, in a concentration-dependent manner [Table 6]. Concentrations of 1.25 and 2.5 mg/mL produced 35.71 and 71.09% inhibition, while at concentrations of 5 and 20 mg/mL, enzyme inhibitory activity was observed to be 100%. The concentration required to inhibit the enzyme by 50% IC50 was estimated to be 1.62 mg/mL. The extract was also observed to inhibit α-amylase mediated generation of maltose in a concentration dependent manner at 2 min after the start of the reaction [Figure 1]. At 3 min, a 20 mg/mL concentration of the extract produced the highest percentage inhibitory effect and was observed to suppress maltose generation by 81.52% while samples containing 1.25, 5, and 10 g/mL produced 23.55-58.33% inhibition [Figure 1]. The IC50 of the extract at 3 min was estimated to be 3.86 mg/mL.
Table 6.
α-glucosidase inhibitory activity of extract
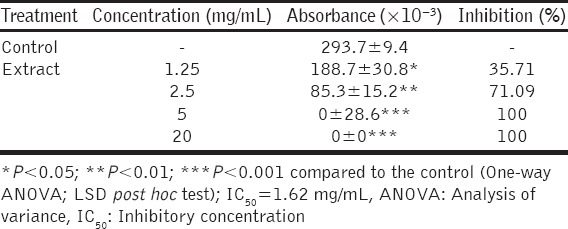
Figure 1.
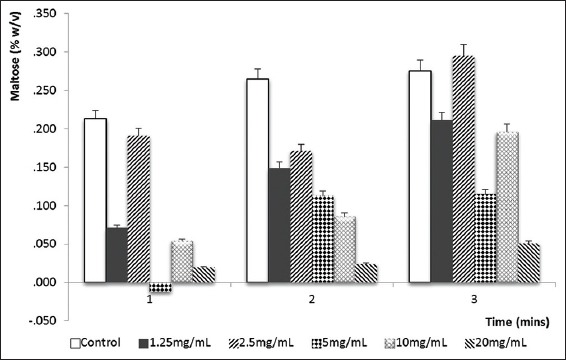
α-amylase inhibitory effect of the extract. Error bars represent standard errors of the mean of tests performed in triplicate
TLC fingerprint of the extract showed 6 spots with retention factors ranging from 0.47 to 0.97. HPLC chromatogram revealed the characteristic peaks of the extracts with retention times ranging between 1.547 and 22.104 min [Figure 2].
Figure 2.
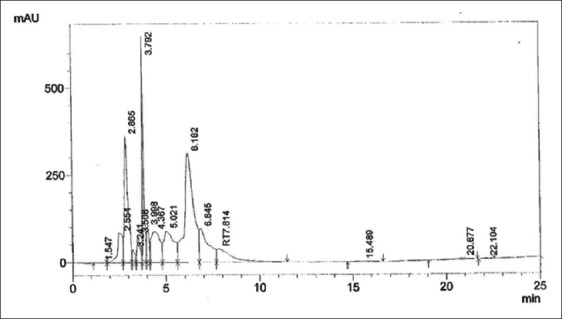
High-performance liquid chromatography fingerprint of extract
DISCUSSION
The various mechanisms have been associated with the antihyperglycemic activities of medicinal plants which include peripheral utilization of glucose, increased synthesis of hepatic glycogen by enhancement of glycogen regulatory enzyme expression in the liver, inhibition of carbohydrate metabolizing enzymes, stimulation of pancreatic insulin release, and inhibition of hepatic glucose production [16-20]. The reduction of fasting blood glucose level by the extract implies that the extract may have exerted this effect through one or more of these mechanisms. The extract also enhanced glucose tolerance by suppressing postprandial rise in glucose level, likely through enhanced insulin sensitivity and/or increased glucose uptake by skeletal muscle and adipose tissue [21].
Effective suppression of the postprandial rise in blood glucose level reflects good tolerance of sudden glucose load, and this may occur as a result of increasing glucose uptake into tissue sites [22]. Postprandial glucose clearance by the liver translates to glycogen synthesis and storage which may be due to enhanced insulin release from β cells [23]. The extract inhibited α-amylase and α-glucosidase, and this indicates it may produce a postprandial antihyperglycemic effect by suppressing carbohydrate metabolism and the consequent glucose release from the lumen of small intestine following a meal [16,23]. This finding is consistent with a previous study which demonstrated the enzyme inhibitory actions of an extract of the plant [7]. Inhibition of both enzymes amounts to reduced glucose absorption and thus, suppressing postprandial hyperglycemia, which plays a central role in development and progression of diabetic complications [24]. Inhibition of the two enzymes in vitro by the extract can be correlated with enzyme inhibition in vivo, which is capable of decreasing glucose entering portal vein from the gut or glucose production from starch [25]. In addition to limiting the extent of glucose absorption, the extract enhanced glucose mobilization by stimulating hepatic glycogen synthesis shown by the increase in liver glycogen content as well as liver weight. This suggests that the extract may enhance glucose uptake by liver and skeletal muscles, an effect secondary to insulin stimulation and enhanced insulin sensitivity in target organs [26]. The reductions observed in hepatic marker enzymes in serum could have been caused by the hepatocellular and cardiac protection offered by the extract and is consistent with an earlier report on an extract of O. basilicum [8]. Hepatic and cardiac tissues release aspartate and alanine transferases and therefore, the elevation of plasma concentrations of these enzymes are indicators of hepatic and cardiac damage as in the case of complications in diabetes mellitus [27]. The reduction in serum ALP activity recorded is suggestive of cellular membrane/hepatocellular membrane protective effects of the plant extract. ALP functions as a biochemical marker enzyme for maintaining membrane integrity. Increase in its plasma activity indicates disruption of cell membrane integrity, which occurs in diseases including diabetes mellitus [28]. These seeming hepatic protective actions of the extract suggest that once daily chronic application may not predispose to hepatic toxicity, albeit in the short term.
The burden of diabetes on individuals is due to its long-term microvascular and macrovascular complications. Hyperlipidemia is a major cause of macrovascular complication associated with diabetes. It is accompanied with premature atherosclerosis which is a major cause of cardiovascular disease [29]. Hyperlipidemia involves elevated total cholesterol and triglycerides. The extract in addition to good glycemic control also lowered the total cholesterol and triglyceride levels in diabetic rats consistent with earlier findings [19]. The extract reduced the total cholesterol, low-density lipoprotein and triglycerides and this may be attributed to a stimulatory effect insulin secretion which improves the action of lipoprotein lipase enzyme and/or by sensitization of target organs such as adipose tissue to insulin action.
The extract used on this study was finger-printed to establish an identity marker as a means of standardization. TLC and HPLC fingerprints of the extract can be used as tools for quality control and standardization of extracts of the plant obtained by similar method to that used for the extract in this study [30].
CONCLUSION
The extract of aerial parts of O. basilicum possesses antidiabetic effects, possibly mediated by limiting glucose absorption through inhibition of carbohydrate metabolizing enzymes and enhancement of hepatic glucose mobilization. Chronic oral administration may not predispose to the risk of hepatotoxicity in the short term. Further studies are warranted to evaluate effects of chronic administration of the extract in diabetes.
ACKNOWLEDGMENT
The authors thankfully acknowledge Mr. Muazzam of NIPRD, Abuja for identifying the plant material and Mr. Andrew Sule and Sunday Dzarma of NIPRD for technical assistance.
Footnotes
Source of Support: Nil,
Conflict of Interest: None declared.
REFERENCES
- 1.American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diab Care. 2013;36(Suppl 1):S67–74. doi: 10.2337/dc13-S067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Popkin BM, Adair LS, Ng SW. Global nutrition transition and the pandemic of obesity in developing countries. Nutr Rev. 2012;70:3–21. doi: 10.1111/j.1753-4887.2011.00456.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Krentz AJ, Patel MB, Bailey CJ. New drugs for Type 2 diabetes mellitus: What is their place in therapy? Drugs. 2008;68:2131–62. doi: 10.2165/00003495-200868150-00005. [DOI] [PubMed] [Google Scholar]
- 4.Rutebemberwa E, Lubega M, Katureebe SK, Oundo A, Kiweewa F, Mukanga D. Use of traditional medicine for the treatment of diabetes in Eastern Uganda: A qualitative exploration of reasons for choice. BMC Int Health Hum Rights. 2013;13:1. doi: 10.1186/1472-698X-13-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Eddouks M, Bidi A, El Bouhali B, Hajji L, Zeggwagh NA. Antidiabetic plants improving insulin sensitivity. J Pharm Pharmacol. 2014;66:1197–214. doi: 10.1111/jphp.12243. [DOI] [PubMed] [Google Scholar]
- 6.Kumar S, Narwal S, Kumar V, Prakash O. α-glucosidase inhibitors from plants: A natural approach to treat diabetes. Pharmacogn Rev. 2011;5:19–29. doi: 10.4103/0973-7847.79096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.El-Beshbishy HA, Bahashwan SA. Hypoglycemic effect of basil (Ocimum basilicum) aqueous extract is mediated through inhibition of α-glucosidase and α-amylase activities. Toxicol Ind Health. 2012;28:42–50. doi: 10.1177/0748233711403193. [DOI] [PubMed] [Google Scholar]
- 8.Yacout G, Elguindy N, Azab E. Hepatoprotective effect of basil (Ocimum basilicum L.). On CCl4-induced liver fibrosis in rats. Afr J Biotech. 2012;11:15702–11. [Google Scholar]
- 9.Opalchenova G, Obreshkova D. Comparative studies on the activity of basil--an essential oil from Ocimum basilicum L.--against multidrug resistant clinical isolates of the genera Staphylococcus, Enterococcus and Pseudomonas by using different test methods. J Microbiol Methods. 2003;54:105–10. doi: 10.1016/s0167-7012(03)00012-5. [DOI] [PubMed] [Google Scholar]
- 10.Renzulli C, Galvano F, Pierdomenico L, Speroni E, Guerra MC. Effects of rosmarinic acid against aflatoxin B1 and ochratoxin-A-induced cell damage in a human hepatoma cell line (Hep G2) J Appl Toxicol. 2004;24:289–96. doi: 10.1002/jat.982. [DOI] [PubMed] [Google Scholar]
- 11.Lalko J, Api AM. Investigation of the dermal sensitization potential of various essential oils in the local lymph node assay. Food Chem Toxicol. 2006;44:739–46. doi: 10.1016/j.fct.2005.10.006. [DOI] [PubMed] [Google Scholar]
- 12.Mbaoji FN, Okoli CO, Ezike AC. Preliminary antihyperglycemic activity-guided studies on the leaf extract and fractions of Ocimum basilicum L. J Chem Pharm Res. 2014;6:575–80. [Google Scholar]
- 13.National Research Council. Guide for the Care and Use of Laboratory Animals. 8th ed. Washington, DC: National Academies Press; 2011. [PubMed] [Google Scholar]
- 14.Okoli CO, Obidike IC, Ezike AC, Akah PA, Salawu OA. Studies on the possible mechanisms of antidiabetic activity of extract of aerial parts of Phyllanthus niruri. Pharm Biol. 2011;49:248–55. doi: 10.3109/13880209.2010.501456. [DOI] [PubMed] [Google Scholar]
- 15.Ali H, Houghton PJ, Soumyanath A. α-Amylase inhibitory activity of some Malaysian plants used to treat diabetes; With particular reference to Phyllanthus amarus. J Ethnopharmacol. 2006;107:449–55. doi: 10.1016/j.jep.2006.04.004. [DOI] [PubMed] [Google Scholar]
- 16.Matsui T, Tanaka T, Tamura S, Toshima A, Tamaya K, Miyata Y, et al. alpha-Glucosidase inhibitory profile of catechins and theaflavins. J Agric Food Chem. 2007;55:99–105. doi: 10.1021/jf0627672. [DOI] [PubMed] [Google Scholar]
- 17.Gao H, Huang YN, Xu PY, Kawabata J. Inhibitory effect on α-glucosidase by the fruits of Terminalia chebula Retz. Food Chem. 2007;105:628–34. [Google Scholar]
- 18.Xu Z, Wang X, Zhou M, Ma L, Deng Y, Zhang H, et al. The antidiabetic activity of total lignan from Fructus Arctii against alloxan-induced diabetes in mice and rats. Phytother Res. 2008;22:97–101. doi: 10.1002/ptr.2273. [DOI] [PubMed] [Google Scholar]
- 19.Eddouks M, Jouad H, Maghrani M, Lemhadri A, Burcelin R. Inhibition of endogenous glucose production accounts for hypoglycemic effect of Spergularia purpurea in streptozotocin mice. Phytomedicine. 2003;10:594–9. doi: 10.1078/094471103322331890. [DOI] [PubMed] [Google Scholar]
- 20.Krishnasamy G, Muthusamy K, Chellappan DR, Subbiah N. Antidiabetic, antihyperlipidaemic, and antioxidant activity of Syzygium densiflorum fruits in streptozotocin and nicotinamide-induced diabetic rats. Pharm Biol. 2016;54:1716–26. doi: 10.3109/13880209.2015.1125932. [DOI] [PubMed] [Google Scholar]
- 21.DeFronzo RA, Goodman AM. Efficacy of metformin in patients with non-insulin-dependent diabetes mellitus. The Multicenter Metformin Study Group. N Engl J Med. 1995;333:541–9. doi: 10.1056/NEJM199508313330902. [DOI] [PubMed] [Google Scholar]
- 22.Atangwho IJ, Yin KB, Umar MI, Ahmad M, Asmawi MZ. Vernonia amygdalina simultaneously suppresses gluconeogenesis and potentiates glucose oxidation via the pentose phosphate pathway in streptozotocin-induced diabetic rats. BMC Complement Altern Med. 2014;14:426. doi: 10.1186/1472-6882-14-426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shalev A. Hope for insulin mimetic oral antidiabetic drugs. Eur J Endocrinol. 1999;141:561–2. doi: 10.1530/eje.0.1410561. [DOI] [PubMed] [Google Scholar]
- 24.Ortiz-Andrade RR, García-Jiménez S, Castillo-España P, Ramírez-Avila G, Villalobos-Molina R, Estrada-Soto S. alpha-Glucosidase inhibitory activity of the methanolic extract from Tournefortia hartwegiana: An anti-hyperglycemic agent. J Ethnopharmacol. 2007;109:48–53. doi: 10.1016/j.jep.2006.07.002. [DOI] [PubMed] [Google Scholar]
- 25.Matsui T, Ueda T, Oki T, Sugita K, Terahara N, Matsumoto K. alpha-Glucosidase inhibitory action of natural acylated anthocyanins. 2. alpha-Glucosidase inhibition by isolated acylated anthocyanins. J Agric Food Chem. 2001;49:1952–6. doi: 10.1021/jf0012502. [DOI] [PubMed] [Google Scholar]
- 26.Bressler R, Johnson DG. Pharmacological regulation of blood glucose levels in non-insulin-dependent diabetes mellitus. Arch Intern Med. 1997;157:836–48. [PubMed] [Google Scholar]
- 27.Ji SK, Jung BJ, Chang WC, Sei CK. Hypoglycemic and antihyperlipidemic effect of four Korean medicinal plants in alloxan induced diabetic rats. Am J Biochem Biotech. 2006;2:154–60. [Google Scholar]
- 28.Bhattacharya S, Gachhui R, Sil PC. Effect of kombucha, a fermented black tea in attenuating oxidative stress mediated tissue damage in alloxan induced diabetic rats. Food Chem Toxicol. 2013;60:328–40. doi: 10.1016/j.fct.2013.07.051. [DOI] [PubMed] [Google Scholar]
- 29.Bonora E, Formentini G, Calcaterra F, Lombardi S, Marini F, Zenari L, et al. HOMA-estimated insulin resistance is an independent predictor of cardiovascular disease in Type 2 diabetic subjects: Prospective data from the Verona Diabetes Complications Study. Diab Care. 2002;25:1135–41. doi: 10.2337/diacare.25.7.1135. [DOI] [PubMed] [Google Scholar]
- 30.Fan XH, Cheng YY, Ye ZL, Lin RC, Qian ZZ. Multiple chromatographic fingerprinting and its application to the quality control of herbal medicines. Anal Chim Acta. 2006;555:217–24. [Google Scholar]


