Abstract
Background
Computer navigation during surgery can help oncologic surgeons perform more accurate resections. However, some navigation studies suggest that this tool may result in unique intraoperative problems and increased surgical time. The degree to which these problems might diminish with experience–the learning curve–has not, to our knowledge, been evaluated for navigation-assisted tumor resections.
Questions/purposes
(1) What intraoperative technical problems were observed during the first 2 years using navigation? (2) What was the mean time for navigation procedures and the time improvement during the learning curve? (3) Have there been any differences in the accuracy of the registration technique that occurred over time? (4) Did navigation achieve the goal of achieving a wide bone margin?
Methods
All patients who underwent preoperative virtual planning for tumor bone resections and operated on with navigation assistance from 2010 to 2012 were prospectively collected. Two surgeons (GLF, LAA-T) performed the intraoperative navigation assistance. Both surgeons had more than 5 years of experience in orthopaedic oncology with more than 60 oncology cases per year per surgeon. This study includes from the very first patients performed with navigation. Although they did not take any formal training in orthopaedic oncology navigation, both surgeons were trained in navigation for knee prostheses. Between 2010 and 2012, we performed 124 bone tumor resections; of these, 78 (63%) cases were resected using intraoperative navigation assistance. During this period, our general indications for use of navigation included pelvic and sacral tumors and those tumors that were reconstructed with massive bone allografts to obtain precise matching of the host and allograft osteotomies. Seventy-eight patients treated with this technology were included in the study. Technical problems (crashes) and time for the navigation procedure were reported after surgery. Accuracy of the registration technique was defined and the surgical margins of the removed specimen were determined by an experienced bone pathologist after the surgical procedure as intralesional, marginal, or wide margins. To obtain these data, we performed a chart review and review of operative notes.
Results
In four patients (of 78 [5%]), the navigation was not completed as a result of technical problems; all occurred during the first 20 cases of the utilization of this technology. The mean time for navigation procedures during the operation was 31 minutes (range, 11–61 minutes), and the early navigations took more time (the regression analysis shielded R2 = 0.35 with p < 0.001). The median registration error was 0.6 mm (range, 0.3–1.1 mm). Registration did not improve over time (the regression analysis slope estimate is −0.014, with R2 = 0.026 and p = 0.15). Histological examinations of all specimens showed a wide bone tumor margin in all patients. However, soft tissue margins were wide in 58 cases and marginal in 20.
Conclusions
We conclude that navigation may be useful in achieving negative bony margins, but we cannot state that it is more effective than other means for achieving this goal. Technical difficulty precluded the use of navigation in 5% of cases in this series. Navigation time decreased with more experience in the procedure but with the numbers available, we did not improve the registration error over time. Given these observations and the increased time and expense of using navigation, larger studies are needed to substantiate the value of this technology for routine use.
Level of Evidence
Level IV, therapeutic study.
Introduction
Computer assistance and navigation-based surgical techniques have been recently introduced in orthopaedic oncology to assist orthopaedic oncology operations. This surgical assistance is becoming more frequently used in limb salvage surgery to preserve as much host tissue as possible without compromising tumor margins and may help surgeons perform more accurate resections [11, 15, 16, 18]. However, previous reports about navigation in trauma and arthroplasty have suggested that computer assistance techniques do not improve patient-reported outcomes and that these techniques add surgical time [6, 8, 13, 20]. Intraoperative problems and increased surgical time might be expected with the adoption of new technology, and a learning curve may apply to surgeons who attempt new methods like navigation [1, 12, 17].
In recent years, orthopaedic oncology surgeons have begun to use computer-assisted surgery for bone tumor resections [2]. The rationale for the use of this assistance is that this technique may improve the accuracy of the resections without adding radiation exposure with acceptable increases in surgical time and with a low rate of handling and operating room setting problems. These advantages may make this technique a safer procedure for the patient. However, the degree to which these problems might diminish with experience–the learning curve–has not, to our knowledge, been evaluated for navigation-assisted tumor resections.
We therefore attempted to answer the following study questions: (1) What intraoperative technical problems were observed during the first 2 years using navigation? (2) What was the mean time for navigation procedures and the time improvement during the learning curve? (3) Have there been any differences in the accuracy of the registration technique that occurred over time? (4) Did navigation achieve the goal of achieving a wide bone margin?
Patients and Methods
This is a retrospective, single-center study that included the initial experience of two surgeons (GLF, LAA-T) with navigation. All of the participating surgeons are high-volume, fellowship-trained, academically based orthopaedic oncology subspecialists. Before the start of the study, these surgeons have been in practice for a median of 8 years (range, 5–15 years) with more than 60 oncology cases per year per surgeon. This series begins with the first navigated bone tumor resection performed at this site. Before using this technology, although neither surgeon took any formal training in orthopaedic oncology navigation, both surgeons were trained in navigation for knee prostheses and had become familiar with the equipment. All preoperative planning and the intraoperative technical support were performed by the same person (LER), who was trained in the navigation factory to provide software and hardware support. All patients who had preoperative virtual planning for bone tumor bone resections and treated by navigation from 2010 to 2012 were prospectively collected for the study and analyzed. Between 2010 and 2012, we performed 124 bone tumor resections; of these, 78 (63%) cases were resected using intraoperative navigation assistance. During this period, our general indications for use of navigation included pelvic and sacral tumors and those tumors that were reconstructed with massive bone allografts to obtain precise matching of the host and allograft osteotomies. Tumor diagnoses were malignant bone tumors in 65 cases and benign locally aggressive bone tumors in 13 cases (Table 1).
Table 1.
Number of cases according to tumor diagnosis
| Diagnosis | Number of cases |
|---|---|
| Chondrosarcoma | 27 |
| Osteosarcoma | 25 |
| Ewing’s sarcoma | 5 |
| Chondromyxoid fibroma | 3 |
| Osteoblastoma | 3 |
| Osteofibrous dysplasia | 3 |
| Bone metastasis | 2 |
| Malignant peripheral nerve sheath tumor | 1 |
| Adamantinoma | 1 |
| Leiomyosarcoma | 1 |
| Chondroblastoma | 1 |
| Chordoma | 1 |
| Fibrosarcoma | 1 |
| Aneurysmal bone cyst | 1 |
| Pleomorphic sarcoma | 1 |
| Giant cell tumor of bone | 1 |
| Phosphaturic mesenchymal tumor | 1 |
Seventy-eight patients treated with navigation for bone tumor resections were included in the study. The mean age of these patients was 33 years (range, 2–78 years). Forty-three of the resections were performed in men and 35 in women.
All patients were followed for a minimum of 24 months or until death. The mean followup was 31 months (range, 5–48 months). No patients were lost to followup. Staging studies included plain radiographs, CT, and MRI. Preoperative diagnoses were made with needle biopsy.
After the preoperative studies were performed, the CT and MRI were fused. Using MIMICS® software (Materialise, Leuven, Belgium), the affected bone was reconstructed with the tumor and the osteotomies for tumor resection were planned in an oncologic meeting. The virtual surgical planning was imported back into a navigation system (Stryker Navigation System II, Orthomap software Version 1.0, Freiburg, Germany) [1]. One centimeter was considered the minimum bone margin for malignant tumors and 0.5 cm in benign or local aggressive tumors. The Stryker navigation system was used in all cases. The navigation computer was positioned opposite to the surgeon approximately 4 feet away from the patient. The camera was located above the patient and directed downward at 45°. After surgical exposure, two 3-mm Apex pins were placed on the affected bone at least 3 cm away from the programmed osteotomy line in an area not affected by the tumor based on the preoperative planning. A navigation tracker was fixed to the pins with the Stryker OrthoLock System. An image-to-patient registration to match precisely the operative anatomy and preoperative virtual CT images is performed by paired points (Fig. 1) and surface points (Fig. 2). In terms of surgical steps, four or at least three landmark points are identified in the affected bone based on the surgical exposure and anatomic visible points. Then, surface mapping of the bone is performed to reduce any mismatch between preoperative images and the patient’s anatomy using at least 50 surface registration points in unaffected bone. After registration, the surgeon must double-check with the navigation pointer if the surface of the patient’s bone in real time correlates with the virtual preoperative images. Afterward, using the navigation pointer, the osteotomies were marked on the bone surface (Fig. 3). The directions of the bone cuts were determined with the pointer and the osteotomies performed with an oscillating saw [15].
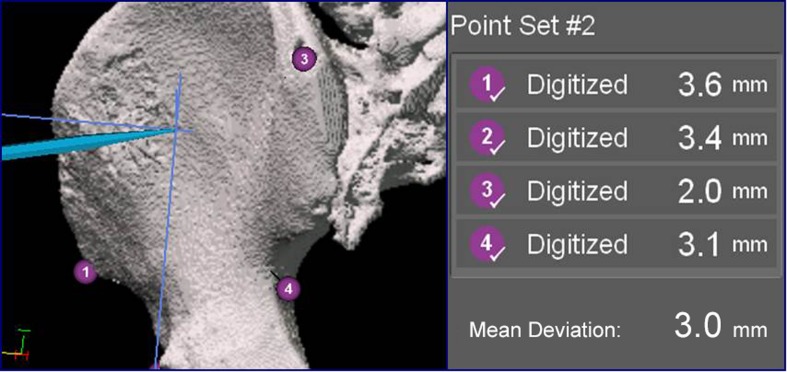
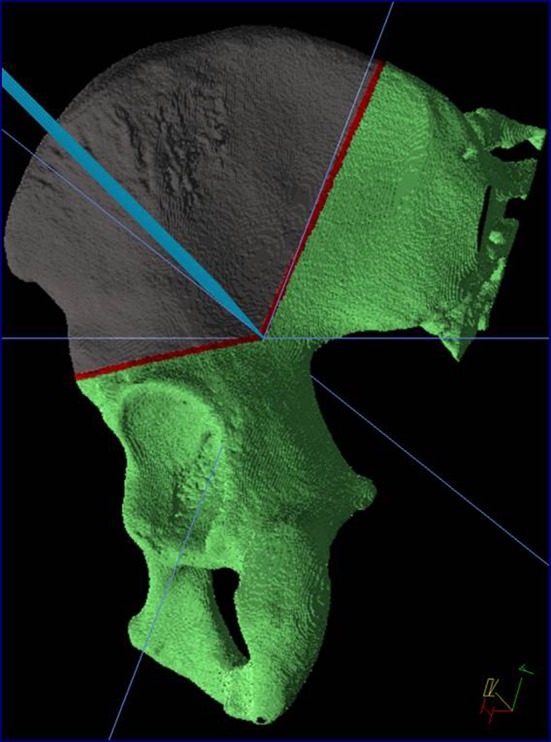
Fig. 1.
This figure shows an image-to-patient registration to match precisely the operative anatomy and preoperative virtual CT images performed by paired points.
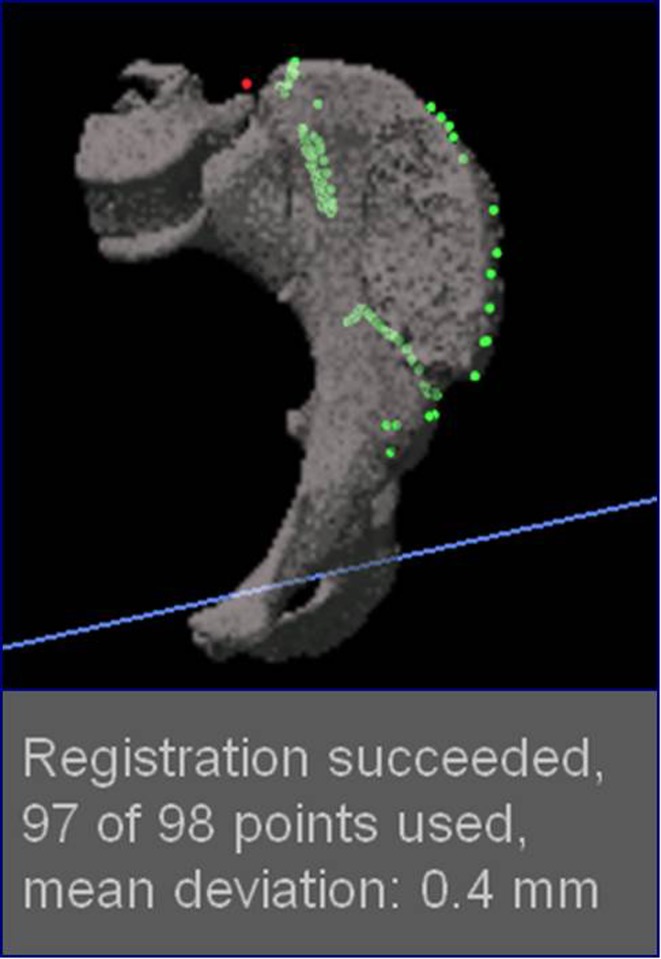
Fig. 2.
This figure shows the surface refinement mapping of the anatomic landmarks to reduce registration error.
Fig. 3.
This figure shows how the planned osteotomies are marked in the patient using a navigated pointer after adequate registration.
To test the first research purpose, we defined technical problems associated with navigation as those intraoperative problems that made it impossible for the surgeon to perform the navigation. So in these cases, the surgeon must continue the surgery without the assistance of navigation. To evaluate this, we registered consecutively in all cases those that we were not able to perform the navigation and afterward we analyzed the problem and divided them into hardware (malfunction of the system, tracker rupture, disruption of the infrared signal between the camera and the surgical tools) or software problems (incompatibility between the images and the navigation system, exceeding the capacity of the programs). When these problems were identified, we performed procedures to avoid them. Intraoperative technical problems were classified as software and hardware crashes and reported after each surgical procedure.
To determine the time required for navigation procedures in bone tumor resection using this technology, we registered in all the procedures in this series the time required for fixation of the device in the bone, registration, marking, and performing the osteotomies.
We defined accuracy of the registration technique as the correspondence between the fused images reconstructed in a three-dimensional virtual platform in the preoperative planning and the real anatomic region in the surgical field. Intraoperative registration of the patient to the patient images is the key step in the navigation process [18] and is calculated by the navigation system software. These data were obtained intraoperatively in the navigation system after point and surface registration and were registered in all the cases in which navigation was performed. Accuracy of the registration technique was classified as good with differences below 1 mm; if it exceeds this, the registration was repeated.
Finally, specimen resection was analyzed by an experienced pathologist to determine bone and soft tissue surgical margins. The existence of a normal soft tissue cuff enveloping the tumor was checked before the specimen was split with the saw to look at margins. The margins are defined as intralesional (when the margins are compromised by the tumor), marginal (when the margins are less than 1 cm for malignant tumor and 5 mm for benign tumors), or wide (when the margins are more than 1 cm for malignant tumor and 5 mm for benign tumors).
Statistical Analysis
To assess whether the registration was improved and the intraoperative navigation time decreased during the first 2 years of using this technology, a linear regression with dependent variable time and error an independent variable the order of each case was performed using the R programming language [14]. Dispersion graphics were performed with Microsoft Office Excel software (Version 2007; Redmond, WA, USA).
Results
Technical Problems with Navigation
Intraoperative technical problems resulted in the navigation not being completed for the procedures in four of 78 patients (5%) in this series. In two of those procedures, we experienced software failure, and we experienced hardware problems in the other two. One of the software technical crashes happened because the computer did not recognize one letter of the patient’s last name (the Spanish ñ). The other software failure occurred when we tried to navigate the position of the osteosynthesis plate for the reconstruction and the information to perform this exceeded the capacity of the computer navigation system so we could not use the navigation data for either the resection or the osteosynthesis plate. Both hardware failures were related to broken trackers undetected during the procedure. All four of these problems occurred during the first 20 cases of the utilization of this technology.
Surgical Time and Improvement Over Time
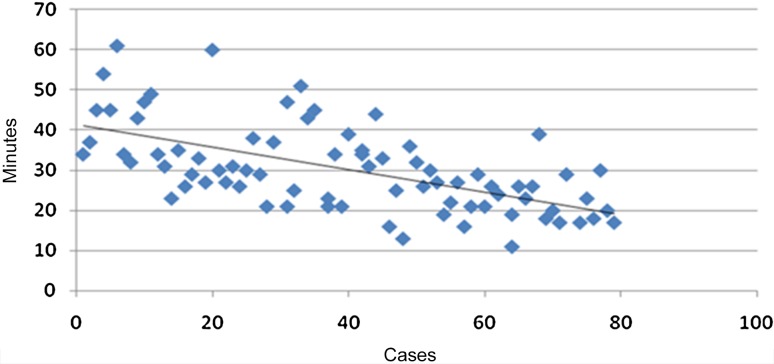
In the 74 procedures in which the computer-assisted procedure could be performed, the mean time for navigation procedures during surgery was 31 minutes (range, 11–61 minutes). We observed that in pelvic tumors, the mean time for the navigation procedure was 41 minutes (range, 23–61 minutes), whereas the mean time for the navigation procedure in extremity tumors was 27 minutes (range, 11–54 minutes). However, with the linear regression analysis, we observed that surgical time decreased as surgeons performed more navigated procedures (inverse correlation slope of −0.28; 95% confidence interval [CI], −0.37 to −0.19; R2 = 0.36; p < 0.001; Fig. 4). That is, in general, the latest computer-assisted surgeries were faster than the first ones (Fig. 4).
Fig. 4.
Diffusion graphic shows how the procedure time decreased over time.
Improvement in Registration Accuracy Over Time?
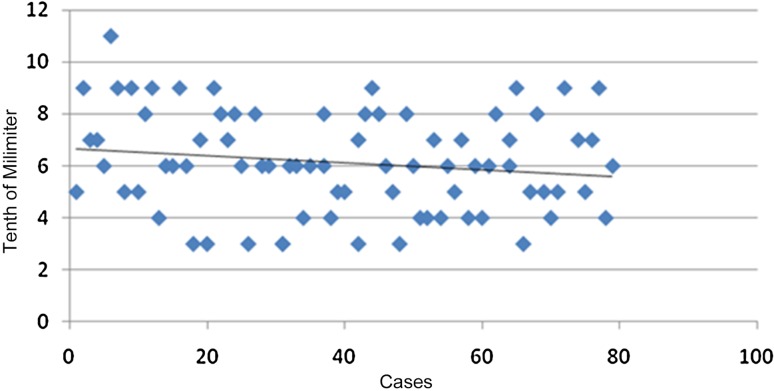
The linear regression analysis, with the data available, suggests that there is no improvement in registration as more cases were performed (inverse correlation slope of −0.01; 95% CI, −0.03 to 0.00; R2 = 0.03; p = 0.15; Fig. 5). Of the 74 cases in which navigation was performed, the median registration error was 0.6 mm (range, 0.3–1.1 mm). Therefore, the range of registration error appears to be constant overtime from the first navigation through the last one (Fig. 5).
Fig. 5.
Diffusion graphic shows how the registration accuracy did not improve over time.
Histological Margins and Local Recurrences
We performed histological examinations of all specimens and they showed a wide bone tumor margin in all patients. However, although the existence of a normal soft tissue cuff enveloping the tumor was checked in all frozen sections, in the soft tissue histologic analysis of margins, 58 had wide soft tissue margins and 20 had marginal ones. No intralesional margins were observed in either bone or in soft tissue resection evaluations. With surgical navigation, it was possible to reproduce the bone margins as planned preoperatively.
Tumors of the soft tissue component were not navigated in any case. In the 18 cases in which the tumor was located in the pelvis, soft tissue margins were wide in five cases and marginal in 13 cases. In the remaining 60 cases, the tumor was located in the extremity; soft tissue margins were wide in 53 cases and marginal in seven cases (Table 2). No intralesional resections were performed. Seven of the 78 patients in whom navigation was performed had a local recurrence (9%). According to the location of local recurrences, we observed that four cases of the 18 pelvic tumors underwent local relapse (22%), and three cases of the 60 tumors located in the extremities had a local recurrence (5%). Most local recurrences were related to patients with soft tissue marginal resections (Table 3).
Table 2.
Demographic data of cases with local recurrence
| Patient number | Sex | Age (years) | Location | Diagnosis |
|---|---|---|---|---|
| 1 | Male | 2 | Tibia | OFD |
| 2 | Male | 17 | Tibia | Osteosarcoma |
| 3 | Male | 24 | Femur | Ewing Sarcoma |
| 4 | Female | 19 | Pelvis | Osteosarcoma |
| 5 | Female | 12 | Pelvis | MPNST |
| 6 | Male | 61 | Pelvis | Chondrosarcoma |
| 7 | Male | 37 | Pelvis | Chondrosarcoma |
OFD = osteofibrous dysplasia; MPNST = malignant peripheral nerve sheath tumor.
Table 3.
Local recurrence frequency according to tumor location
| Cases | Wide soft tissue margins (NLR) | Marginal soft tissue margins (NLR) |
|---|---|---|
| Pelvic benign tumors | – | – |
| Pelvic malignant tumors | 5 (0) | 13 (4) |
| Limb benign tumors | 12 (0) | 1 (1) |
| Limb malignant tumors | 41 (1) | 6 (1) |
Percentages appear in parentheses; NLR = number of local recurrences.
Discussion
The use of computer-assisted navigation technologies might help surgeons perform more accurate resections [2, 11, 15]. However, some papers have reported problems related to the use of navigation, including increased operative time as a result of the additional technological complexity; in addition, there is no evidence of which we are aware suggesting that navigation decreases the risk of local recurrence [7, 16]. It seems to us that for a tool of this sort, the learning curve needs to be considered [12, 17], but to our knowledge, the results of navigation in orthopaedic oncology have not been assessed as a function of surgical experience (number of procedures performed). In this study, we analyzed common problems related with this procedure, surgical time, resection accuracy, and histological margins with a particular focus on how surgical time and accuracy changed during the first 2 years (78 cases) of our experience with this new technology.
Our study has several limitations. The study population is small and so our no-difference finding on registration accuracy could be a function of insufficient statistical power (β error). However, a look at the scatterplot of registration accuracy over time suggests a nearly flat line, and so we believe this is unlikely to be the case. We also had a diverse population of patients of varying diagnoses (benign and malignant) and locations (pelvis and extremity). Also, our study has only short-term followup, so it is conceivable that more local recurrences may be discovered over longer followup. Another important limitation is that we analyzed only the time of the navigation procedure during the surgery; however, this procedure requires considerable time for the preoperative plan before the surgery as well, which was not factored in here but should be considered by surgeons thinking of adopting this tool. Moreover, all preoperative planning and the intraoperative technical support were performed by the same person (LER), which could lead to reduced navigation time during surgery. This technical support is helpful for our group, but this dependency is a main limitation in centers that do not have a designated technician.
In our series, 5% of the navigation procedures were not carried out as a result of technical problems. All these system crashes occurred in the first year using this technology, at the beginning of the learning curve. After 20 cases we no longer saw these problems. If we analyze previous publications, this type of procedure has a risk of failures at the beginning of the learning curve [3, 16]. Another report describes that technical problems occurred in 20% of the analyzed series [18]. The authors indicated that they only used a mean of 20 points during surface registration, which could be the reason for such a high frequency of intraoperative problems. In our series, at least 50 surface registration points were used in unaffected bone.
The mean time for navigation procedures during surgery was 31 minutes in our series, and surgical time decreased over the course of our study. This improvement may be related to increased experience and confidence [3, 19]. In other orthopaedic surgical procedures such as arthroplasty, studies have compared the surgical duration of conventional and navigation-assisted procedures and demonstrated that the times for navigated procedures increased operating time [3, 8, 19, 20]. Nevertheless, tumor operations are different from one patient to another because of the size and location of the tumor in each case. Therefore, the use of navigation assistance helps the surgeon provide anatomic detail about the surgical bed, adding accuracy and precision to the surgical resection [7, 10]. We noted that in pelvic resections, the mean time for navigation was longer. This could be because pelvic anatomy makes tumor resections more complex and time-consuming compared with extremity sites.
The median registration error was 0.6 mm (range, 0.3–1.1 mm). This error is similar to that observed in previous publications [1, 2, 10, 17, 21, 22]. In our study, the amount of registration error did not improve overtime (Fig. 5). To our knowledge, ours is the first study that looked at the learning curve with respect to registration accuracy. We believe that our accuracy did not improve because the median registration error was very small to begin with (under 1 mm).
The overall frequency of local recurrence in our series was 9%. With the numbers we had we could not detect a difference between pelvic tumors and extremity tumors, but there may be a difference if we had a larger study. Several factors could be related to local recurrences [5], but in general, surgical margin is a major factor related to this problem [10]. Computer-assisted surgery has shown that it provides accuracy in oncological resection [15]. However, the surgeon can perform a misreading of preoperative images, making inadequate cuts that could lead to inadequate margins. Histological examinations of all specimens showed a wide bone tumor margin in all patients like in previous reports with this technique [2, 3, 9–11, 21, 22]. Navigation assistance helps the surgeon to reproduce accurately the preoperative plan [4]; this can help to avoid intralesional bone resection, reducing the risk of local recurrence. Nevertheless, soft tissue margins cannot be navigated with the current technologies. Therefore, surgeons cannot reproduce the preoperative planning with the degree of precision achieved in bone margins. Despite this technical limitation, a recent report suggests the utilization of this technology in pelvic tumors, because they found a lower incidence of local recurrences [10].
We conclude that navigation may be useful in achieving negative bony margins but we cannot state that it is more effective than other means for achieving this goal. Although helpful in achieving negative bony margins, it did not preclude recurrences presumably resulting from soft tissue margins, although with the numbers we had and the heterogeneity of our tumor population, a larger study will be necessary to substantiate this observation. Technical difficulty precluded its use in 5% of cases. The surgical navigation time decreased with more experience in the procedure, but with the numbers available, we observed no improvement in the registration error over time. Given these observations and the increased time and expense of using navigation, it will require a larger study with less variation in tumor type to substantiate the value of this technology for routine use.
Footnotes
One of the authors certifies that he (LAA-T) or a member of his immediate family, has or may receive payments or benefits, during the study period, an amount of USD 10,000 to USD 100,000 from Stryker Americas (Miramar, FL, USA).
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research ® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
Each author certifies that his institution has approved the reporting of this case report and that all investigations were conducted in conformity with ethical principles of research.
This work was performed at Carlos E. Ottolenghi Institute of Orthopedics, Italian Hospital of Buenos Aires, Buenos Aires, Argentina.
References
- 1.Aponte-Tinao L, Ritacco LE, Ayerza MA, Muscolo DL, Albergo JI, Farfalli GL. Does intraoperative navigation assistance improve bone tumor resection and allograft reconstruction results? Clin Orthop Relat Res. 2014 Apr 23 [Epub ahead of print]. [DOI] [PMC free article] [PubMed]
- 2.Aponte-Tinao LA, Ritacco LE, Ayerza MA, Muscolo DL, Farfalli GL. Multiplanar osteotomies guided by navigation in chondrosarcoma of the knee. Orthopedics. 2013;36:e325–e330. doi: 10.3928/01477447-20130222-21. [DOI] [PubMed] [Google Scholar]
- 3.Atesok K, Schemitsch EH. Computer-assisted trauma surgery. J Am Acad Orthop Surg. 2010;18:247–258. doi: 10.5435/00124635-201005000-00001. [DOI] [PubMed] [Google Scholar]
- 4.Ayerza MA, Farfalli GL, Aponte-Tinao L, Muscolo DL. Does increased rate of limb-sparing surgery affect survival in osteosarcoma? Clin Orthop Relat Res. 2010;468:2854–2859. doi: 10.1007/s11999-010-1423-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ayerza MA, Muscolo DL, Aponte-Tinao LA, Farfalli G. Effect of erroneous surgical procedures on recurrence and survival rates for patients with osteosarcoma. Clin Orthop Relat Res. 2006;452:231–235. doi: 10.1097/01.blo.0000229314.58878.88. [DOI] [PubMed] [Google Scholar]
- 6.Blakeney WG, Khan RJ, Wall SJ. Computer-assisted techniques versus conventional guides for component alignment in total knee arthroplasty: a randomized controlled trial. J Bone Joint Surg Am. 2011;93:1377–1384. doi: 10.2106/JBJS.I.01321. [DOI] [PubMed] [Google Scholar]
- 7.Cheong D, Letson GD. Computer-assisted navigation and musculoskeletal sarcoma surgery. Cancer Control. 2011;18:171–176. doi: 10.1177/107327481101800304. [DOI] [PubMed] [Google Scholar]
- 8.Hart R, Janecek M, Chaker A, Bucek P. Total knee arthroplasty implanted with and without kinematic navigation. Int Orthop. 2003;27:366–369. doi: 10.1007/s00264-003-0501-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ieguchi M, Hoshi M, Takada J, Hidaka N, Nakamura H. Navigation-assisted surgery for bone and soft tissue tumors with bony extension. Clin Orthop Relat Res. 2012;470:275–283. doi: 10.1007/s11999-011-2094-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jeys L, Matharu GS, Nandra RS, Grimer RJ. Can computer navigation-assisted surgery reduce the risk of an intralesional margin and reduce the rate of local recurrence in patients with a tumour of the pelvis or sacrum? J Bone Joint Surg Br. 2013;95:1417–1424. doi: 10.1302/0301-620X.95B10.31734. [DOI] [PubMed] [Google Scholar]
- 11.Li J, Wang Z, Guo Z, Chen GJ, Yang M, Pei GX. Irregular osteotomy in limb salvage for juxta-articular osteosarcoma under computer-assisted navigation. J Surg Oncol. 2012;106:411–416. doi: 10.1002/jso.23105. [DOI] [PubMed] [Google Scholar]
- 12.MatsenKo L. New technology: safety, efficacy, and learning curves. Clin Orthop Relat Res. 2014;472:1080–1085. doi: 10.1007/s11999-013-3413-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mavrogenis AF, Savvidou OD, Mimidis G, Papanastasiou J, Koulalis D, Demertzis N, Papagelopoulos PJ. Computer-assisted navigation in orthopedic surgery. Orthopedics. 2013;36:631–642. doi: 10.3928/01477447-20130724-10. [DOI] [PubMed] [Google Scholar]
- 14.R Core Team. R: A Language and Environment for Statistical Computing. Vienna, Austria; 2014. Available at: http://www.R-project.org. Accessed June 11, 2015.
- 15.Ritacco LE, Milano FE, Farfalli GL, Ayerza MA, Muscolo DL, Aponte-Tinao LA. Accuracy of 3-D planning and navigation in bone tumor resection. Orthopedics. 2013;36:e942–e950. doi: 10.3928/01477447-20130624-27. [DOI] [PubMed] [Google Scholar]
- 16.Satcher RL., Jr How intraoperative navigation is changing musculoskeletal tumor surgery. Orthop Clin North Am. 2013;44:645–656. doi: 10.1016/j.ocl.2013.07.001. [DOI] [PubMed] [Google Scholar]
- 17.Sclafani JA, Kim CW. Complications associated with the initial learning curve of minimally invasive spine surgery: a systematic review. Clin Orthop Relat Res. 2014;472:1711–1717. doi: 10.1007/s11999-014-3495-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.So TY, Lam YL, Mak KL. Computer-assisted navigation in bone tumor surgery: seamless workflow model and evolution of technique. Clin Orthop Relat Res. 2010;468:2985–2991. doi: 10.1007/s11999-010-1465-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Stulberg SD, Loan P, Sarin V. Computer-assisted navigation in total knee replacement: results of an initial experience in thirty-five patients. J Bone Joint Surg Am. 2002;84(Suppl 2):90–98. doi: 10.2106/00004623-200200002-00011. [DOI] [PubMed] [Google Scholar]
- 20.Suhm N, Messmer P, Zuna I, Jacob LA, Regazzoni P. Fluoroscopic guidance versus surgical navigation for distal locking of intramedullary implants. A prospective, controlled clinical study. Injury. 2004;35:567–574. doi: 10.1016/S0020-1383(03)00312-7. [DOI] [PubMed] [Google Scholar]
- 21.Wong KC, Kumta SM. Computer-assisted tumor surgery in malignant bone tumors. Clin Orthop Relat Res. 2013;471:750–761. doi: 10.1007/s11999-012-2557-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wong KC, Kumta SM. Joint-preserving tumor resection and reconstruction using image-guided computer navigation. Clin Orthop Relat Res. 2013;471:762–773. doi: 10.1007/s11999-012-2536-8. [DOI] [PMC free article] [PubMed] [Google Scholar]