Abstract
Objectives
Pill burden during antiretroviral treatment (ART) is associated with worse adherence and impaired virological suppression. We compared the effectiveness, tolerance, and persistence on treatment of single tablet regimens (STRs) with non-STR once-daily regimens in patients receiving first-line ART.
Methods
Retrospective analysis of naïve HIV-1 infected patients prospectively enrolled in the French Dat’AIDS cohort and initiating first-line ART with STRs or once-daily non-STRs from 2004 to 2013. The primary outcome was time to treatment discontinuation defined by any change in the treatment regimen. STR and non-STR groups were compared controlling for baseline risk factors by inverse probability weighted treatment Cox analysis (IPWT) and propensity-score matching (PSM).
Results
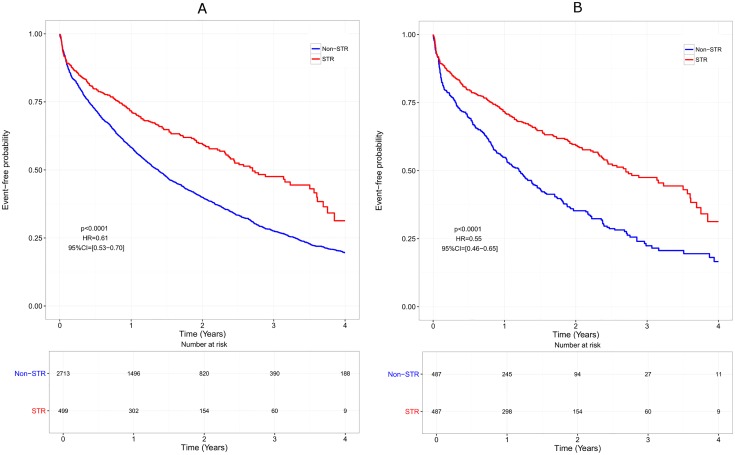
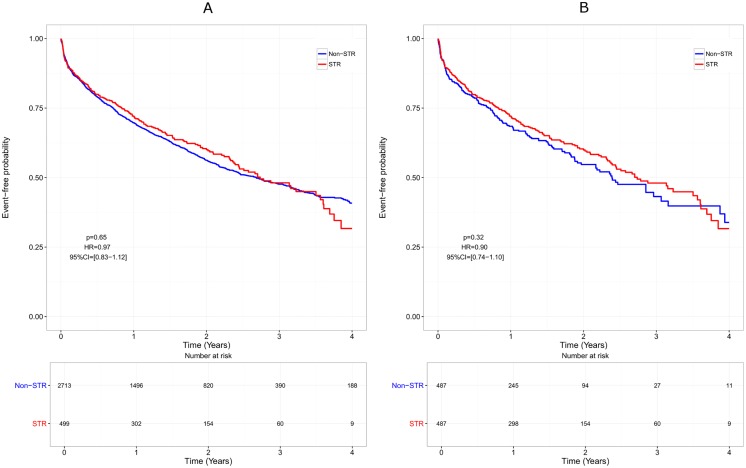
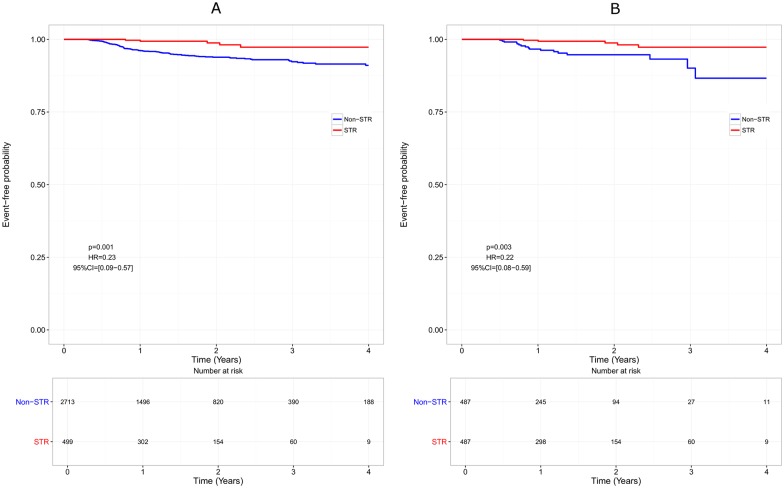
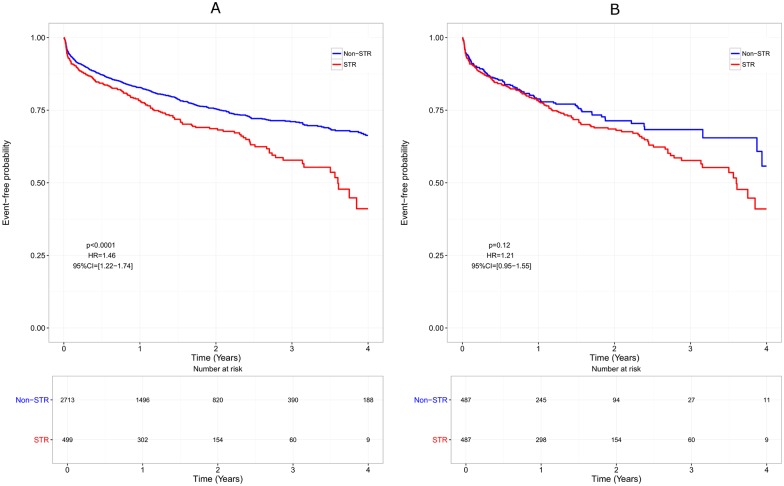
Overall, 3212 patients (STR 499, non-STR 2713) were included. Median time to treatment discontinuation was shorter in non-STR patients than in STR patients, both in the IPWT (HR = 0.61, p<0.0001) and the PSM cohort (HR = 0.55, p<0.0001). This difference disappeared when censoring ART modification for simplification, both in the IPWT (HR = 0.97, p = 0.65) and the PSM cohort (HR = 0.91, p = 0.33). A lower rate of virological failure was observed with STRs than with non-STRs in both cohorts (HR = 0.23; p = 0.002 and HR = 0.22, p = 0.003, respectively). A lower rate of treatment modification for adverse event was observed with non-STRs in the IPWT cohort (HR = 1.46, p<0.0001), but not in the PSM cohort (HR = 1.22, p = 0.11).
Conclusion
First-line therapy with STRs was associated with a longer time to treatment discontinuation than with non-STRs. However, when ART modification for simplification was not considered as a failure, STRs and non-STRs were similar.
Introduction
During the past decades, HIV combined antiretroviral therapy (ART) has drastically evolved with as a consequence a better control of HIV infection and a reduction of HIV-related morbidity and mortality. Adherence to treatment has been reported as a key factor for ART success and international guidelines underscore the importance of simplifying regimens to improve adherence [1]. Treatment simplification first became possible with the development of drugs with longer half-lives hence allowing once-daily dosing. Adherence to these once-daily regimens was shown to be significantly better than with 3-times and 4-times-daily regimens [2]. However, in a meta-analysis, Parienti et al. reported only a modest beneficial effect of once-daily regimens on adherence to treatment compared with twice-daily regimens [3]. In 2006, the first single tablet regimen (STR), a combination of tenofovir (TDF), emtricitabine (FTC), and efavirenz (EFV) became available and recommended in first-line therapy [4–6]. Several other STRs combining TDF/FTC/rilpivirine (RPV), TDF/FTC/cobicistat/elvitegravir and abacavir/lamivudine/dolutegravir have been developed [7,8] and as recommended by international guidelines, STRs appear now as a valid treatment strategy to decrease pill burden [1,9]. Compared with multiple tablet regimens, some STRs have been associated with better adherence [10–15], and improved quality of life (QoL) [15,16]. Moreover, since adherence to treatment is correlated with hospitalization, some studies showed that STRs were also associated with a 17% reduction in total health care costs mostly due to a reduction in hospitalizations [12,17]. Recently, some authors described the different factors to be considered for the choice of a particular STR and stressed the need for careful clinical, virological and immunological monitoring along with regular adherence assessment to achieve treatment success [18].
Since comparisons between STRs and non-STR once-daily regimens are sparse, we compared the effectiveness, tolerance, and persistence on treatment of STRs with non-STR regimens in patients receiving first-line ART in a French large cohort of HIV-infected patients.
Materials and methods
Patients
All adult naive HIV-1 infected patients prospectively enrolled in the French Dat’AIDS cohort and receiving either an STR or non-STR once-daily first-line ART from 2004 to 2013 with HIV-RNA data >6 months were retrospectively analyzed. The Dat’AIDS cohort represents a collaboration between about 30 major French HIV treatment centers throughout the country [19] and includes data on more than 35,000 HIV-infected patients. Patients were followed until occurrence of one of the following events: treatment modification, treatment interruption, death, lost to follow-up, or end of study period (December 31, 2013).
Outcomes
The primary outcome was time to treatment discontinuation defined as the delay between starting and stopping the first line antiretroviral therapy. Reasons for stopping therapy which were prospectively collected included simplification, clinical or biological toxicity, virological failure and other reasons such as pregnancy, pharmacological interactions, or patient’s willingness.
Virological failure definition was similar as that used in the ACTG 5202 study [20] and was characterized by a viral load (VL) ≥ 1000 copies/mL between W16 and W24 or VL ≥ 200 copies/mL after W24. Adverse events not leading to treatment modification were not considered as failure. Simplification was defined as any change of the primary treatment resulting in a lower pill burden. For example, a switch from TDF/FTC/EFV as separate pills to TDF/FTC/EFV as STR was considered as simplification. Treatment was considered interrupted after four weeks of discontinuation.
Four different analyses were conducted: (i) Overall effectiveness: In the main analysis, only patients who remained on the same therapy at the end of follow-up were considered as treatment success. The primary outcome was defined as treatment discontinuation for virological failure, occurrence of adverse event, or any cause of treatment modification. (ii) Overall effectiveness, simplification censored: Same as (i) but treatment simplification was censored. (iii) Virological efficacy: Only virological failure was considered as treatment failure. (iv) Tolerance: Only toxicity requiring treatment modification was considered as treatment failure.
Statistical analysis
Data were expressed as mean ± standard deviation, or median (interquartile range) for quantitative variables or as numbers and percentages for qualitative variables. Baseline differences between patients starting with a non-STR once-daily regimen or an STR were compared using Chi-square or Fisher exact tests for categorical variables and two-tailed, unpaired t test or Wilcoxon rank sum test for continuous variables in the overall cohort. In addition, we compared baseline characteristics by the use of standardized difference.
The association between each endpoint and treatment strategy was evaluated by the hazard ratio (HR) and its 95% confidence interval (CI), with a value <1 being in favor of STR (increased risk of outcome in the non-STR group). Because non-STR and STR were selected by choice rather than by chance, an analysis using propensity scores was conducted to limit potential biases. The propensity score was computed from a logistic regression non-parsimonious model including all baseline characteristics associated with STR with a p<0.5, i.e. age, gender, HIV RNA, CD4 cell count, CDC stage, hepatitis B or C coinfection, HIV risk factor, and type of ART. Two different complementary approaches were used: inverse probability weighting (IPWT) and matching on the propensity score [21]. Each endpoint was modeled by a marginal structural Cox model (IPWT), after checking the proportionality assumption, which was met. Second, a one-to-one greedy 5 to 1 digit technique was performed to match one control (non-STR group) with one case (STR group), based on the propensity score and nested within the overall cohort. In this matched subsample, baseline characteristics included in the propensity score were compared between cases and controls by the standardized difference, as appropriate. The probability of outcome was then modeled in a Cox model with robust sandwich variance estimators to take into account the correlation within each matched pair and included the group (non-STR versus STR) as an explanatory factor. In order to assess the factors associated with the prescription of STR and account for the indication bias in the analyses, we preferred a strategy using propensity score rather than covariable adjustment. A P value <0.05 was considered significant and all P values were two-tailed. No adjustment was made for multiple comparisons. Statistical analyses were performed using SAS statistical software, version 9.4 (SAS Institute Inc., Cary, NC).
Ethical considerations
The Dat’AIDS cohort received approval from the French “Comité consultatif sur le traitement de l'information en matière de recherche dans le domaine de la santé'” (Registration number 15.196) and is registered with identifier NCT02898987 in ClinicalTrial.gov. All patients included in this study gave their written inform consent to allow the use of their personal clinical data. All patient information was entered into a database using anonymous coded identification numbers. This study was conducted in accordance with the principles of the declaration of Helsinki and the French law related to biomedical research.
Results
Patients’ characteristics
Between 2004 and 2013, 3212 patients fulfilling the inclusion criteria were analyzed among whom 499 were treated with STRs, and 2713 with once-daily non-STRs. Patients’ characteristics for the whole cohort and after propensity matching are summarized in Table 1. STR patients were more frequently younger (37.6 vs 39.6 years, p = 0.0002), male (83.4% vs 77.0%, p = 0.002), homo- or bisexual (59.2% vs 48.4%, p<0.0001), had less frequently HBV/HCV coinfection (7.2% vs 10.8%, p = 0.016), were less frequently at CDC stage C (6.0% vs 14.7%) and had higher baseline CD4 level (395/mm3 vs 315/mm3, p<0.0001) and lower baseline HIV-RNA level (4.6 log copies/mL vs 4.7 log copies/mL, p = 0.025) than non-STR patients. A center effect was also observed. Detailed antiretroviral treatment among patients receiving non-STR or STR is presented in S1 Table. Using the propensity score, 487 STR patients were matched with 487 non-STR patients leading to comparable groups (all standardized differences <0.05), except for the type of ART received which was not possible.
Table 1. Patients’ characteristics at treatment initiation.
| Overall cohort | After Propensity matching | ||||||
|---|---|---|---|---|---|---|---|
| Non-STR (n = 2713) |
STR (n = 499) |
p | Standardized difference | Non-STR (n = 487) |
STR (n = 487) |
Standardized difference | |
| Age, mean (SD) | 39.6 (11.0) | 37.6 (10.4) | 0.0002 | 0.19 | 37.6 (10.2) | 37.7 (10.4) | -0.01 |
| Male, n (%) | 2089 (77.0%) | 416 (83.4%) | 0.0016 | -0.16 | 402 (82.6%) | 405 (83.2%) | -0.02 |
| HIV RNA, (log10), mean (SD) | 4.7 (0.84) | 4.6 (0.77) | 0.025 | 0.12 | 4.6 (0.84) | 4.6 (0.77) | 0 |
| CD4, mean (SD) | 314.9 (183.8) | 394.6 (203.4) | <0.0001 | -0.41 | 391.9 (227.4) | 390.9 (201.8) | 0.005 |
| CDC stage C, n (%) | 398 (14.7%) | 30 (6.0%) | <0.0001 | 0.29 | 26 (5.3%) | 30 (6.2%) | -0.04 |
| Hepatitis C or B, n (%) | 293 (10.8%) | 36 (7.2%) | 0.016 | 0.13 | 40 (8.2%) | 36 (7.4%) | 0.03 |
| Risk factors, n(%) | <0.0001 | ||||||
| Heterosexual | 1135 (41.8%) | 157 (31.5%) | 0.21 | 162 (33.3%) | 156 (32.0%) | 0.03 | |
| Homo & Bisexual | 1314 (48.4%) | 295 (59.2%) | -0.22 | 276 (57.3%) | 288 (59.1%) | -0.04 | |
| Other | 264 (9.7%) | 47 (9.4%) | 0.01 | 46 (9.5%) | 43 (8.8%) | 0.02 | |
| Type of ART, n(%) | <0.0001 | ||||||
| 2 NRTI + 1 NNRTI | 872 (32.1) | 499 (100%) | 102 (20.9%) | 487 (100%) | NA | ||
| 2 NRTI + 1 bPI | 1841 (67.9) | 0 (0%) | 385 (79.1%) | 0 (0%) | NA | ||
ART, antiretroviral therapy; NRTI, nucleoside reverse transcriptase inhibitor; NNRTI, non-nucleoside reverse transcriptase inhibitor; bPI, boosted protease inhibitor; SD, standard deviation; STR, single tablet regimen
Overall, the median [Interquartile Range] time before the primary outcome was 1.18 years [0.44–2.26], corresponding to 1.15 years [0.41–2.26] in the non-STR group and 1.34 years [0.59–2.28] in the STR group. During follow-up, 58% of patients receiving STRs had no treatment modification compared with 32% of patients receiving non-STR regimens (p<0.0001, Table 2).
Table 2. Primary reason for treatment modification during follow-up.
| Overall cohort | After Propensity matching | |||||
|---|---|---|---|---|---|---|
| Non-STR (n = 2713) |
STR (n = 499) |
p | Non-STR (n = 487) |
STR (n = 487) |
p | |
| Patients without treatment modification | 878 (32.4%) | 291 (58.3%) | <0.001 | 181 (37.2%) | 282 (57.9%) | <0.001 |
| Reason for treatment modification, n (%) | ||||||
| Adverse event | 553 (20.4%) | 156 (31.3%) | <0.001 | 101 (20.7%) | 154 (31.6%) | <0.001 |
| Virological failure | 154 (5.7%) | 10 (2.0%) | <0.001 | 20 (4.1%) | 10 (2.1%) | 0.0951 |
| Simplification | 723 (26.6%) | 0 (0%) | - | 126 (25.9%) | 0 (0%) | - |
| Other | 405 (14.9%) | 42 (8.4%) | <0.001 | 59 (12.1%) | 41 (8.4%) | 0.072 |
STR, single tablet regimen; Other includes: pregnancy (planned or ongoing), patient willingness, poor adherence, drug-drug interaction, enrollment in clinical trial, toxicity prevention such as switch from didanosine or stavudine to other drugs when the toxicities of these molecules were widely recognized.
Treatment discontinuation over time
The median time to treatment discontinuation was shorter in non-STR patients than in STR patients, both in the whole cohort (1.38 years [1.28–1.47] vs 2.70 [2.36–3.50], HR = 0.61, p<0.0001), and in the matched cohort (1.20 years [1.02–1.38] vs 2.70 [2.36–3.50], HR = 0.55, p<0.0001; Fig 1). However, this difference disappeared when censoring ART modification for simplification, both in the whole cohort (HR = 0.97, p = 0.65) and in the matched cohort (HR = 0.90, p = 0.32; Fig 2). The efficacy analysis based on virological response only, indicated a beneficial effect of STRs compared with non-STR regimens with a longer time to virological failure (HR = 0.23, p = 0.001 in the whole cohort and HR = 0.22, p = 0.003 in the matched cohort; Fig 3).
Fig 1. Overall effectiveness over time.
Only patients remaining on the same therapy at the end of follow-up are considered as treatment success. Failure is defined as treatment discontinuation, occurrence of adverse event, or any cause of treatment modification.
Fig 2. Overall effectiveness over time (simplification censored).
Only patients remaining on the same therapy at the end of follow-up are considered as treatment success. Failure is defined as treatment discontinuation, occurrence of adverse event, or any cause of treatment modification except treatment simplification (censored).
Fig 3. Virological efficacy over time.
Virological failure is defined as viral load (VL) > 1000 copies/mL between W16 and W24 or VL > 200 copies/mL after W24.
Tolerance and toxicity over time
Using the whole cohort, time to occurrence of adverse events leading to treatment discontinuation was shorter in patients treated with STRs than in patients treated with non-STRs (HR = 1.46, p<0.0001). This difference was no longer statistically significant in the matched cohort (HR = 1.21, p = 0.12) (Fig 4).
Fig 4. Tolerance over time: Failure is defined as the occurrence of an adverse event anytime during therapy.
Subgroup analysis
A total of 499 patients receiving an STR with 2 NRTI + 1 NNRTI (100%) were compared with 872 non-STR patients receiving similar drug components (32.1%). Results are presented in S2 Table. Similar virological efficacy and similar tolerance were observed between STR and non-STR groups.
Discussion
Based on a cohort of 3212 naïve patients, our study compared the effectiveness and tolerance of STR and non-STR once-daily regimens in real life conditions. When considering treatment failure as a virological failure or any treatment modification over time, a benefit was observed for STRs, which induced less ART modifications than non-STR regimens. However, our results show that this effect is mainly due to treatment simplifications that occurred in almost 28% of patients in the non-STR group (Table 2). Another study based on a different methodology using data from the French National Healthcare Insurance database, also showed that treatment persistence (continuous treatment without interruption or modification) was higher in patients treated with an STR compared with other administration schedules [22]. However, the reasons for treatment modifications could not be determined in this study.
When focusing on virological efficacy only, a benefit of STRs is observed whereas non-STR once-daily regimens seem to be associated with a better tolerance. It should be noticed that the rate of virological failure in both groups of patients is very low (<5% in the matched cohort). Therefore, the benefit of STRs on virological efficacy, if any, may only have a limited clinical impact. Since the difference in tolerance observed on the whole cohort disappears when focusing on the matched cohort (Fig 4), it is reasonable to believe that the difference resulted from different patients’ characteristics.
The Dat’AIDS cohort is a French large multicenter prospective cohort based on data from about 30 HIV centers scattered throughout the country [19] and including data on more than 35,000 HIV patients. This cohort may be considered as representative of real-life clinical practice. Characteristics at baseline showed significant differences between both treatment strategies indicating that STR and non-STR once-daily regimens are associated with different patient profiles. Patients receiving STR were indeed younger, more often male, had higher CD4 and lower HIV RNA level and had less often a CDC stage C suggesting that these patients had somehow less severe infection than patients receiving a non-STR regimen. To reduce these differences, a matched control cohort was selected based upon propensity scores. After matching, the STR and non-STR groups were comparable in regards to baseline characteristics. However, except for the tolerance analysis (Fig 4), no clear-cut difference appeared when analyzing the whole cohort or the matched cohort.
Nowadays, most international guidelines recommend decreasing pill burden to prevent non-adherence to treatment. Some authors have shown that besides a 20% rate of complete non-adherence, 3–13% of patients reported a selective non-adherence (to one or several compounds in a given regimen) hereby stressing the potential benefit of STRs [23]. Lower pill burden has been associated with both better adherence and virological suppression although a meta-analysis reported that adherence, but not virological suppression, was slightly better with once- vs twice-daily regimens [24]. A recent meta-analysis showed that patients on STR were significantly more adherent than patients both on once- and twice-daily multi-tablet regimens and presented a higher rate of viral load suppression at 48 weeks [25]. However, the meta-analysis by Nachega et al. [24] did not contrast STR versus several pills provided once-daily, which was the purpose of the current analysis. In addition, the potential benefit of STRs should be weighed against the higher costs of these newest branded combinations compared with non-STR regimens that may contain generic compounds [18]. Another drawback is that STRs are based on fixed-dose combinations making it impossible to adapt a single compound unless breaking the regimen into several pills. Our study has some limitations. The most important one is the retrospective comparison with absence of randomization. Comparison of baseline characteristics shows that treatment was allocated by choice. STRs were indeed prescribed to patients with a higher chance of favorable outcomes compared with patients receiving non-STR as first-line ART. Because the database used yielded from a clinical cohort rather than an administrative database [22], this bias was limited by creating a matched cohort of non-STR patients who turned to be closely comparable to STR patients. Another limitation is that the proportion of individual drug components differed between STR and non-STR groups. All STR patients were indeed treated with 2 NRTI + 1 NNRTI compared with only 32% of non-STR patients. When comparing these subgroups (S2 Table), no clear-cut benefit of STRs is observed in terms of virological efficacy and tolerance. It is thus likely that the lower tolerance observed in STR patients in the whole cohort is due to the higher proportion of patients receiving efavirenz. Since newer STRs—especially those containing integrase inhibitors—are probably better tolerated [26,27], our results cannot be extrapolated to all different STRs. At the time of the study, TDF/FTC was the only nucleoside combination available as STR and comparison with abacavir/lamivudine combination could not be performed. However, the small difference in virological efficacy between STR and non-STR regimens suggests a limited impact of nucleosides on virological failure. Another possible limitation is that presence of comorbidities is not controlled for in the model. Patients with multiple comorbidities are indeed more likely to receive other non-HIV medications and have thus a higher chance to discontinue therapy because of pharmacological interaction. Comorbidities may also directly influence the choice of ART or limit the choice of treatment: for example, patients with renal diseases are contraindicated to receive tenofovir and may not receive tenofovir-based STR. It is also possible that non-STR were specifically prescribed to patients because of the presence of resistance associated mutation on genotypic results. However, primary resistance to STR compounds was rare in France at the time of the study (<5%) [28]. Finally, we did not measure adherence to therapy. However, a low level of adherence would have primarily affected the virological results [29,30]. Since the rate of virological failure is extremely low in this real life study, we can hypothesized that insufficient adherence is probably not a significant issue at the population level. Indeed, a previous French study observed a mean adherence rate of 89.6% in patients in the STR group (n = 76) compared with 86.4% in the non-STR once-daily group (n = 242) [22]. These results, as well as our study, suggest that both STR and once-daily non STR regimens are associated with high level of adherence in real life and that both options may be specifically useful in patients struggling for treatment adherence.
In conclusion, the median time to treatment discontinuation was shorter in non-STR patients than in STR patients but this difference was driven by ART modification for simplification while a STR cannot yet be simplified further. Virological efficacy seems slightly better with STRs than with non-STR regimens. STRs were prescribed to patients with a higher chance of favorable outcomes than patients receiving non-STR as first-line ART. After accounting for baseline differences, the superiority of STRs over non-STR regimens was mainly driven by treatment simplification, suggesting a preference for STR rather than indicating failing therapy [31]. STRs were associated with a slightly better virological control while non-STR regimens seemed to be associated with a better tolerance profile. If the preference for a lower pill burden is not considered, limited differences could be expected using current OD regimens instead of STRs as first-line ART. Moreover, switching STRs to non STR once-daily regimens using antiretroviral generics could be similarly efficient and more cost-effective. In this context, STR regimens could be useful in patients struggling for treatment adherence [10].
Supporting Information
(PDF)
“Overall effectiveness” indicates that failure is defined as treatment discontinuation, occurrence of adverse event, or any cause of treatment modification. “Overall effectiveness (simplification censored)” indicates that failure is defined as treatment discontinuation, occurrence of adverse event, or any cause of treatment modification except treatment simplification (censored). “Virological efficacy” indicates that virological failure is defined as viral load (VL) > 1000 copies/mL between W16 and W24 or VL > 200 copies/mL after W24. “Tolerance” indicates that failure is defined as the occurrence of an adverse event anytime during therapy. A Hazard Ratio (HR) <1 is in favor of STR.
(PDF)
Acknowledgments
The authors acknowledge members of the Dat’AIDS group: F. Raffi, C. Allavena, E. Billaud, C. Biron, B. Bonnet, S. Bouchez, D. Boutoille, C. Brunet, T. Jovelin, N. Hall, C. Bernaud, P. Morineau, V. Reliquet, O. Aubry, P. Point, M. Besnier, L. Larmet, H. Hüe, S. Pineau, E. André-Garnier, A. Rodallec (Nantes); S. Brégigeon, O. Faucher, V. Obry-Roguet, M. Orticoni, M.J. Soavi, I. Luquet- Besson, E. Ressiot, I. Pinot, M.J. Ducassou, H. Bertone, S. Gallie, S. Trijau, A.S. Ritleng, A. Ivanova, M. Guignard, C. Blanco-Betancourt, I. Poizot-Martin (Marseille); B. Marchou, P. Massip, E. Bonnet, M. Obadia, M. Alvarez, L. Porte, L. Cuzin, P. Delobel, M. Chauveau, D. Garipuy, I. Lepain, M. Marcel, E. Puntis, K. Sauné (Toulouse); P. Pugliese, C. Ceppi, E. Cua, J. Cottalorda, P. Dellamonica, E. Demonchy, B. Dunais, J. Durant, C. Etienne, S. Ferrando, J.G. Fuzibet, R. Garraffo, K. Risso, V. Mondain, A. Naqvi, N. Oran, I. Perbost, S. Pillet, B. Prouvost-Keller, C. Pradier, S. Wehrlen-Pugliese, E. Rosenthal, S. Sausse, P.M. Roger (Nice); Ph. Choisy, S. Vandame, Th. Huleux, F. Ajana, I. Alcaraz, V. Baclet, TH. Huleux, H. Melliez, N. Viget, M. Valette, E. Aissi, Ch. Allienne, A. Meybeck, B. Riff (Tourcoing); R. Agher, C. Katlama, M.A. Valantin, C. Duvivier (Paris); L. Cotte, D. Peyramond, C. Chidiac, T. Ferry, F. Ader, F. Biron, A. Boibieux, P. Miailhes, T. Perpoint, I. Schlienger, F. Dahoud, J. Lippmann, E. Braun, J. Koffi, C. Longuet, V. Guéripel, C. Augustin-Normand, S. Degroodt (Lyon); A. Cabié, S. Abel, S. Pierre-François, B. Rozé, P. Hochedez (Fort-de-France).
Data Availability
All relevant data are within the paper and its supporting Information files. Individual patients data are available upon request.
Funding Statement
The authors received no specific funding for this work.
References
- 1.European AIDS clinical society. Guidelines for the clinical management and treatment of HIV infected adults in Europe. Version 8.0, October 2015. [Internet]. [cited 31 May 2016]. http://www.eacsociety.org/files/2015_eacsguidelines_8.0-english_revised-20151104.pdf
- 2.Claxton AJ, Cramer J, Pierce C. A systematic review of the associations between dose regimens and medication compliance. Clin Ther. 2001;23: 1296–1310. [DOI] [PubMed] [Google Scholar]
- 3.Parienti J-J, Bangsberg DR, Verdon R, Gardner EM. Better adherence with once-daily antiretroviral regimens: a meta-analysis. Clin Infect Dis Off Publ Infect Dis Soc Am. 2009;48: 484–488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Goicoechea M, Best B. Efavirenz/emtricitabine/tenofovir disoproxil fumarate fixed-dose combination: first-line therapy for all? Expert Opin Pharmacother. 2007;8: 371–382. 10.1517/14656566.8.3.371 [DOI] [PubMed] [Google Scholar]
- 5.Killingley B, Pozniak A. The first once-daily single-tablet regimen for the treatment of HIV-infected patients. Drugs Today Barc Spain 1998. 2007;43: 427–442. [DOI] [PubMed] [Google Scholar]
- 6.Gallant JE, DeJesus E, Arribas JR, Pozniak AL, Gazzard B, Campo RE, et al. Tenofovir DF, emtricitabine, and efavirenz vs. zidovudine, lamivudine, and efavirenz for HIV. N Engl J Med. 2006;354: 251–260. 10.1056/NEJMoa051871 [DOI] [PubMed] [Google Scholar]
- 7.Aldir I, Horta A, Serrado M. Single-tablet regimens in HIV: does it really make a difference? Curr Med Res Opin. 2014;30: 89–97. 10.1185/03007995.2013.844685 [DOI] [PubMed] [Google Scholar]
- 8.Astuti N, Maggiolo F. Single-Tablet Regimens in HIV Therapy. Infect Dis Ther. 2014;3: 1–17. 10.1007/s40121-014-0024-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Thompson MA, Mugavero MJ, Amico KR, Cargill VA, Chang LW, Gross R, et al. Guidelines for improving entry into and retention in care and antiretroviral adherence for persons with HIV: evidence-based recommendations from an International Association of Physicians in AIDS Care panel. Ann Intern Med. 2012;156: 817–833, W,–284, W,–285, W,–286, W,–287, W,–288, W,–289, W,–290, W,–291, W,–292, W,–293, W–294. 10.7326/0003-4819-156-11-201206050-00419 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bangsberg DR, Ragland K, Monk A, Deeks SG. A single tablet regimen is associated with higher adherence and viral suppression than multiple tablet regimens in HIV+ homeless and marginally housed people. AIDS Lond Engl. 2010;24: 2835–2840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Buscher A, Hartman C, Kallen MA, Giordano TP. Impact of antiretroviral dosing frequency and pill burden on adherence among newly diagnosed, antiretroviral-naive HIV patients. Int J STD AIDS. 2012;23: 351–355. 10.1258/ijsa.2011.011292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cohen CJ, Meyers JL, Davis KL. Association between daily antiretroviral pill burden and treatment adherence, hospitalisation risk, and other healthcare utilisation and costs in a US medicaid population with HIV. BMJ Open. 2013;3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Juday T, Gupta S, Grimm K, Wagner S, Kim E. Factors associated with complete adherence to HIV combination antiretroviral therapy. HIV Clin Trials. 2011;12: 71–78. 10.1310/hct1202-71 [DOI] [PubMed] [Google Scholar]
- 14.Sterrantino G, Santoro L, Bartolozzi D, Trotta M, Zaccarelli M. Self-reported adherence supports patient preference for the single tablet regimen (STR) in the current cART era. Patient Prefer Adherence. 2012;6: 427–433. 10.2147/PPA.S31385 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Airoldi M, Zaccarelli M, Bisi L, Bini T, Antinori A, Mussini C, et al. One-pill once-a-day HAART: a simplification strategy that improves adherence and quality of life of HIV-infected subjects. Patient Prefer Adherence. 2010;4: 115–125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ganguli A, Wang J, Gourley DR. Does combining antiretroviral agents in a single dosage form enhance quality of life of HIV/AIDS patients? A cost-utility study. Res Soc Adm Pharm RSAP. 2012;8: 157–165. [DOI] [PubMed] [Google Scholar]
- 17.Sax PE, Meyers JL, Mugavero M, Davis KL. Adherence to antiretroviral treatment and correlation with risk of hospitalization among commercially insured HIV patients in the United States. PloS One. 2012;7: e31591 10.1371/journal.pone.0031591 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gandhi M, Gandhi RT. Single-pill combination regimens for treatment of HIV-1 infection. N Engl J Med. 2014;371: 248–259. 10.1056/NEJMct1215532 [DOI] [PubMed] [Google Scholar]
- 19.Pugliese P, Cuzin L, Cabié A, Poizot-Martin I, Allavena C, Duvivier C, et al. A large French prospective cohort of HIV-infected patients: the Nadis Cohort. HIV Med. 2009;10: 504–511. 10.1111/j.1468-1293.2009.00719.x [DOI] [PubMed] [Google Scholar]
- 20.Sax PE, Tierney C, Collier AC, Daar ES, Mollan K, Budhathoki C, et al. Abacavir/lamivudine versus tenofovir DF/emtricitabine as part of combination regimens for initial treatment of HIV: final results. J Infect Dis. 2011;204: 1191–1201. 10.1093/infdis/jir505 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kwiatkowski F, Slim K, Verrelle P, Chamorey E, Kramar A. [Propensity score: interest and limits]. Bull Cancer (Paris). 2007;94: 680–686. [PubMed] [Google Scholar]
- 22.Raffi F, Yazdanpanah Y, Fagnani F, Laurendeau C, Lafuma A, Gourmelen J. Persistence and adherence to single-tablet regimens in HIV treatment: a cohort study from the French National Healthcare Insurance Database. J Antimicrob Chemother. 2015;70: 2121–2128. 10.1093/jac/dkv083 [DOI] [PubMed] [Google Scholar]
- 23.Antinori A, Angeletti C, Ammassari A, Sangiorgi D, Giannetti A, Buda S, et al. Adherence in HIV-positive patients treated with single-tablet regimens and multi-pill regimens: findings from the COMPACT study. J Int AIDS Soc. 2012;15 (Suppl. 4): 18098. [Google Scholar]
- 24.Nachega JB, Parienti J-J, Uthman OA, Gross R, Dowdy DW, Sax PE, et al. Lower pill burden and once-daily antiretroviral treatment regimens for HIV infection: A meta-analysis of randomized controlled trials. Clin Infect Dis Off Publ Infect Dis Soc Am. 2014;58: 1297–1307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Clay PG, Nag S, Graham CM, Narayanan S. Meta-Analysis of Studies Comparing Single and Multi-Tablet Fixed Dose Combination HIV Treatment Regimens. Medicine (Baltimore). 2015;94: e1677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wilkins EL, Cohen CJ, Trottier B, Esser S, Smith DE, Haas B, et al. Patient-reported outcomes in the single-tablet regimen (STaR) trial of rilpivirine/emtricitabine/tenofovir disoproxil fumarate versus efavirenz/emtricitabine/tenofovir disoproxil fumarate in antiretroviral treatment-naive adults infected with HIV-1 through 48 weeks of treatment. AIDS Care. 2016;28: 401–408. 10.1080/09540121.2015.1096890 [DOI] [PubMed] [Google Scholar]
- 27.Prinapori R, Di Biagio A. Efficacy, safety, and patient acceptability of elvitegravir/cobicistat/emtricitabine/tenofovir in the treatment of HIV/AIDS. Patient Prefer Adherence. 2015;9: 1213–1218. 10.2147/PPA.S88490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lambert-Niclot S, Charpentier C, Storto A, Fofana DB, Soulié C, Fourati S, et al. Prevalence of pre-existing resistance-associated mutations to rilpivirine, emtricitabine and tenofovir in antiretroviral-naive patients infected with B and non-B subtype HIV-1 viruses. J Antimicrob Chemother. 2013;68: 1237–1242. 10.1093/jac/dkt003 [DOI] [PubMed] [Google Scholar]
- 29.Parienti J-J, Das-Douglas M, Massari V, Guzman D, Deeks SG, Verdon R, et al. Not all missed doses are the same: sustained NNRTI treatment interruptions predict HIV rebound at low-to-moderate adherence levels. PloS One. 2008;3: e2783 10.1371/journal.pone.0002783 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Parienti J-J, Massari V, Descamps D, Vabret A, Bouvet E, Larouzé B, et al. Predictors of virologic failure and resistance in HIV-infected patients treated with nevirapine- or efavirenz-based antiretroviral therapy. Clin Infect Dis Off Publ Infect Dis Soc Am. 2004;38: 1311–1316. [DOI] [PubMed] [Google Scholar]
- 31.Eaton EF, Tamhane AR, Burkholder GA, Willig JH, Saag MS, Mugavero MJ. Unanticipated Effects of New Drug Availability on Antiretroviral Durability: Implications for Comparative Effectiveness Research. Open Forum Infect Dis. 2016;3: ofw109 10.1093/ofid/ofw109 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF)
“Overall effectiveness” indicates that failure is defined as treatment discontinuation, occurrence of adverse event, or any cause of treatment modification. “Overall effectiveness (simplification censored)” indicates that failure is defined as treatment discontinuation, occurrence of adverse event, or any cause of treatment modification except treatment simplification (censored). “Virological efficacy” indicates that virological failure is defined as viral load (VL) > 1000 copies/mL between W16 and W24 or VL > 200 copies/mL after W24. “Tolerance” indicates that failure is defined as the occurrence of an adverse event anytime during therapy. A Hazard Ratio (HR) <1 is in favor of STR.
(PDF)
Data Availability Statement
All relevant data are within the paper and its supporting Information files. Individual patients data are available upon request.