Abstract
Diabetes has become the third largest cause of death in humans worldwide. Therefore, effective treatment for this disease remains a critical issue. Glucagon-like peptide-1 (GLP-1) plays an important role in glucose homeostasis, and therefore represents a promising candidate to use for the treatment of diabetes. Native GLP-1, however, is quickly degraded in in the circulatory system; which limits its clinical application. In the present study, a chemically-synthesized, modified analogue of human GLP-1 (mGLP-1) was designed. Our analyses indicated that, relative to native GLP-1, mGLP-1 is more resistant to trypsin and pancreatin degradation. mGLP-1 promotes mouse pancreatic β-cell proliferation by up-regulating the expression level of cyclin E, CDK2, Bcl-2 and down-regulating Bax, p21, and stimulates insulin secretion. An oral glucose tolerance test indicated that mGLP-1 significantly improved glucose tolerance in mice. Intraperitoneal injections of mGLP-1 into streptozotocin (STZ)-induced type 2 diabetic mice significantly reduced blood sugar levels and stimulated insulin secretion. Oral gavages of mGLP-1 in diabetic mice did not result in significant hypoglycemic activity.
Introduction
Diabetes is a major chronic, systemic metabolic disease that threatens human health and reduces the quality of life [1]. In 2015, the International Diabetes Federation (IDF) reported that 415 million adults have diabetes worldwide and that by 2040, approximately 10% of the world’s population will be living with this disease [2]. Roughly 90% of all cases of diabetes in humans belong to type 2 diabetes, which is characterized by β-cell dysfunction and insulin resistance [3]. Both of these parameters impair insulin secretion, induce a glucose metabolism disorder, and thus lead to continuous hyperglycemia. Long-term hyperglycemia causes dysfunction and damage to various organs; especially the eyes, kidneys, heart, blood vessels, and nerves.
β-cell dysfunction resulting from glucose toxicity is potentially reversible if metabolic control can be restored [4]. Therefore, controlling and reducing the glucose toxicity may delay the deterioration of β-cell function. At the present time, drugs that effectively control blood sugar levels are not available. Glucagon-like Peptide-1 (GLP-1), a short incretin hormone, is primarily synthesized and secreted by proximal small intestine enteroendocrine L-cells [5]. The mature form of GLP-1 is comprised of 30 amino acids and GLP-1 has pleiotropic therapeutic effects on β-cell restoration and proliferation [6–8]. GLP-1 stimulates insulin secretion in response to glucose, lipids, or mixed oral nutrient ingestion in a glucose dependent manner and becomes inactive when the concentration of blood sugar is less than 3.6 mM. Hence, GLP-1 is an excellent candidate for use as a prophylactic treatment for maintaining glucose homeostasis in diabetic patients and has been extensively investigated. The very short plasma half-life (less than 2 minutes in the circulatory system), however, limits its pharmacotherapy study and clinical application [9–11]. Dipeptidyl peptidase IV (DPP-IV)-mediated cleavage at Ala8 of mature N-terminal GLP-1 results in the production of inactivated N-terminal truncated peptides, GLP-1(9–36) or GLP-1 (9–37). In addition, the kidney also quickly eliminates GLP-1 [12].
Various approaches to extend the half-life of GLP-1 have been investigated, such as developing GLP-1 analogues and DPP-IV inhibitors. DPP-IV- mediated GLP-1 degradation can be avoided by identifying naturally existing DPP-IV-resistant GLP-1 analogs, such as exendin-4 [13], by making N-terminal modifications of GLP-1 [14] or shielding of its cleavage site [15]. In this study, a trypsin-resistant GLP-1 analogue (mGLP-1) was designed and synthesized. The Ala8, Lys26, 34 amino acid residues in human GLP-1 (7–36) were replaced with Gly8, Gln26, and Asp34, respectively. Arg36 was retained at the C-terminal in order to maintain bioactivity. The mGLP-1 analogue exhibited a significant level of resistance to trypsin-induced cleavage. The bioactivity of mGLP-1, both in vitro and in vivo, was also investigated. Results indicated that mGLP-1 promoted pancreatic β-cell proliferation, stimulated insulin secretion, and lowered glucose levels in mice.
Materials and methods
Peptides and experimental mice
Modified human GLP-1 (mGLP-1) and native human GLP-1were both synthesized by ChinaPeptides Co., Ltd. (Shanghai, China). A total of thirty-eight week-old, SPF grade, male KM mice were purchased from Vital River Laboratories Company (Beijing, China) and maintained with standard food pellets under a 12 h light-dark cycle. All animal protocols were reviewed and approved by the Chinese Academy of Agriculture Sciences (CAAS) Institutional Animal Ethical and Welfare Committee (No: BRISPF-2016-03). All mice (30) were euthanized three months after experiments by CO2 asphyxiation.
Trypsin and pepsin proteolysis assay
The resistance of GLP-1 and mGLP-1 to trypsin proteolysis was evaluated by incubating samples of mGLP-1 (10 mg/mL) or GLP-1 (10 mg/mL) with trypsin (4 mg/mL) in PBS (pH 7.4) buffer (1×) at 37°С for 1, 2, 4, 8, 12, 24, 48-h or 1, 2, 4, and 8-h, respectively. GLP-1 (2.5 mg/mL) or mGLP-1 (2.5 mg/mL) were also incubated with 1.0 mg/mL pancreatin (TCI, JPN) in PBS (pH 7.4) at 37°С over various time intervals to evaluate the stability against simulated intestinal fluid. Resistance to pepsin degradation was evaluated by incubating mGLP-1 (1 mg/mL) or GLP-1 (1 mg/mL) with pepsin (2 mg/mL, Sigma) in a hydrochloric acid (HCl) solution (pH 1.5~2.0) at 37°С for 10min. Samples (20 μL) treated with either trypsin or pepsin for different lengths of time were then mixed with SDS-PAGE loading buffer (2×), heated at 100°С for 10 min, and then analyzed with SDS-PAGE. Protein bands on the gels were visualized by silver staining.
Cell proliferation
Mouse insulinoma cells (MIN6) (iCell Bioscience, Inc. Shanghai, China) were cultured in a 25 cm2 cell culture flasks and then seeded into 96-well microplates at a density of 6.0×104 cells per well for the cell proliferation assay. The culture was incubated in an incubator with 5% CO2 at 37°С and 95% RH for 12 h. mGLP-1 or GLP-1 at different concentrations (0.3, 3, 15, and 30-μM) was then mixed into the cell cultures. After 48 h of incubation, 10 μL CCK-8 solution (cell counting kit, Dojindo China Co., Ltd. Shanghai, China) was gently mixed into the culture and the culture was further incubated for 1 to 4 hours. A microplate reader (Bio-Rad, USA) was used to measure cell viability at a 450 nm wavelength (OD450). The cell viability ratio (CRV) was calculated as (A-A0)/A0 × 100% (where A was the absorbance of the treated cell culture and A0 was the OD450 value of a blank (RPMI 1640 medium only)).
RT-qPCR of mGLP-1-regulated gene expression
For screening the expression level of cell proliferation and apoptosis-related genes, total RNA from (GLP-1-treated, mGLP-1-treated, and control) MIN6 cells was extracted using a MiniBEST Universal RNA Extraction Kit (Takara) according to the manufacturer’s instructions. The total RNA in each sample was quantified by UV spectroscopy. Generation of cDNA was performed using a PrimeScript™ RT reagent Kit (Takara) according to the manufacturer’s instructions. RT-qPCR was performed to detect the levels of Bcl-2, Bax, cyclin E, CDK2, and p21 genes expression. The gene-specific primers used in the analysis are listed in Table 1. RT-qPCR analysis was performed using a standard SYBR Fast qPCR Mix kit (Takara) protocol on a 7900HT Fast Real-Time PCR System (Applied Biosystems). Relative expression levels were calculated using the 2-ΔΔCt method.
Table 1. Gene-specific primers designed for the designated mouse genes (Genbank ID) and used to determine the expression levels by RT-qPCR.
| Name | Genbank ID | Sequence (5'->3') | product length (bp) |
|---|---|---|---|
| GAPDH | gi|53237094| | TTGCAGTGGCAAAGTGGAGA | 175 |
| GTCTCGCTCCTGGAAGATGG | |||
| Bcl-2 | gi|929981607| | GAACTGGGGGAGGATTGTGG | 176 |
| CCAGACATGCACCTACCCAG | |||
| Bax | gi|133778943| | CACTAAAGTGCCCGAGCTGA | 167 |
| TGAGGACTCCAGCCACAAAG | |||
| Cyclin E | gi|443939| | TATGGTGTCCTCGCTGCTTC | 202 |
| GGGTCTGGATGTTGTGGGAG | |||
| CDK2 | gi|162287299| | GTGGTACCGAGCACCTGAAA | 188 |
| CTGGCCAAACCACCTCATCT | |||
| p21 | gi|50300976| | TTGCACTCTGGTGTCTGAGC | 190 |
| GGGAAGGGCTGGAATGTTCT |
Insulin secretion assay
Three days after incubation in an incubator with 5% CO2 at 37°С and 95% RH, MIN6 cells were washed two times using Dulbecco's phosphate buffered saline (DPBS) plus 0.1% BSA (Sigma), and then kept in starvation in DPBS with 0.1% BSA for an hour. GLP-1 (15 μM) or mGLP-1 (15 μM) was then added along with 10mM glucose (10 mM) for various lengths of time as described by Brandsma [16]. Cell culture supernatant was then collected and insulin was measured with a mouse insulin ELISA kit (JiNingShiYe Ltd. Shanghai, China) according to the manufacturer’s instructions.
Oral Glucose Tolerance Test (OGTT) in mice
OGTT was conducted on eight-week-old mice that had fasted overnight. A bolus of glucose (2 g/kg body weight) was loaded into the stomach via oral gavage. Then, 30 min or 90 min prior to the OGTT, mGLP-1, GLP-1, or PBS alone was delivered into the mice by intraperitoneal (IP) injection at a concentration of 0.1 mg/kg body weight. The glucose level in blood samples obtained from tail veins was measured at 0, 15, 30, 60, and 120-min after gavage with a glucometer (Sannuo, Changsha, China) as described by Yuelin Kong et al [17].
Glucose levels and insulin secretion in STZ-induced mice
A diabetic condition was induced in eight-week-old mice by intraperitoneal injection (IP) of STZ (30 mg/kg body weight, Beijing BioDee Biotechnology Co., Ltd.) for 4 consecutive days after being fed a high diet food (with crude protein content ≥15%, crude fat ≥12%, and about 4000 kcal/kg calories, data provided by Beijing Vital River Laboratory Animal Technology Co., Ltd, Beijing, China) for 1 month [18]. GLP-1 or mGLP-1 (2 mg/kg body weight) was administered by IP injection. PBS alone was injected as a negative control. Glucose levels were measured at multiple time points after injection in blood samples obtained from tail veins. Insulin concentration at the 180 min time point after injection, when blood sugar levels were at their peak, was measured with a mouse insulin ELISA Kit (JiNingShiYe Ltd. Shanghai, China).
Statistical analysis
All data are expressed as a mean ± standard deviation (SD), and significant differences between treatments were determined by ANOVA using IBM SPSS Statistic 19.0 software. A value of p< 0.05 (*) was considered as statistically significant.
Results and discussion
Design and synthesis of mGLP-1
GLP-1 is a potent incretin hormone which is composed of 30 amino acids. It plays a critical role in glucose homeostasis via glucose-dependent insulin production and secretion, restoration of impaired β-cell secretory function and inhibition of glucagon secretion, etc. The multiple roles of GLP-1 on the process of glucose-stimulated insulin secretion makes it an ideal candidate for the treatment of type 2 diabetes. Its short half-life (less than 2 min), however, significantly limits its clinical application.
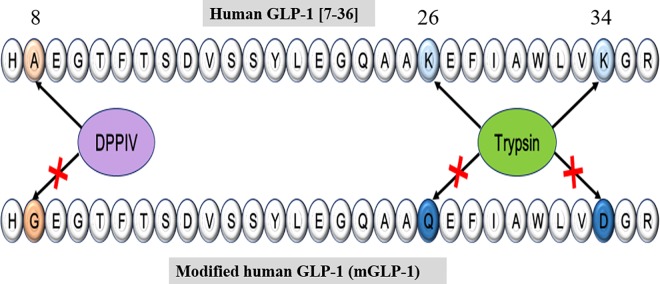
In the present study, a functional, long-acting, protease-resistant mGLP-1 analogue was developed by making several amino acid substitutions in native GLP-1 (Fig 1). When GLP-1 is secreted in response to the assimilation of nutrients, the ubiquitous enzyme, DPP-IV, immediately cleaves the mature GLP-1 peptide at His7-Ala8 and produces two inactive forms, GLP-1(9–36) amide and GLP-1(9–37). GLP-1(9–36) amide may even act as an antagonist on the pancreatic receptor [19]. DPP-IV cleavage is the major factor responsible for the rapid degradation of GLP-1. When Ala8 is replaced by Gly8, as in the potent GLP-1 receptor agonist exdendin-4 [20], it becomes resistant to DPP-IV-mediated degradation. Lys residues are susceptible to serine protease cleavage. In previous studies, when Lys26, 34 was replaced with Gln26 and Asp34, the modified GLP-1 also exhibited greater resistance to proteolytic digestion than the native peptide [14, 21]. In order to eliminate the DPP-IV target in GLP-1 and increase protease resistance, Ala8 was replaced with Gly8, and Lys26, 34 was replaced with Gln26 and Asp34 to synthesize a modified human GLP-1 (mGLP-1). The computed parameters of ExPASy—ProtParam (http://web.expasy.org/protparam) estimated the half-life of mGLP-1 and GLP-1 are 3.5 hours in mammalian reticulocytes and over 10 hours in Escherichia coli, respectively. The instability index (II) of mGLP-1 is computed to be 16.92 which classifies the protein as stable.
Fig 1. Design of modified mature human GLP-1 (mGLP-1).
The amino acid sequence of human native GLP-1 (above) and the synthesized, modified mGLP-1 (below). Substituted amino acids are indicated in color: Ala8→Gly8, Lys26, 34→Gln26, Asp34. The blue substitutions were designed to make the mGLP-1 resistant to trypsin degradation and the brown substitution was designed to inhibit DPPIV degradation.
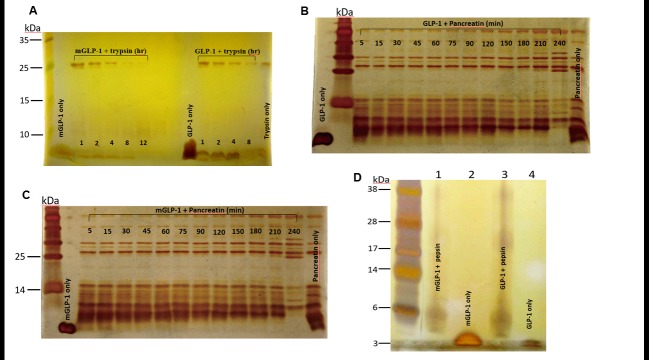
mGLP-1 is resistant to trypsin and pancreatin degradation but not pepsin hydrolysis
Although GLP-1 is susceptible to proteolytic enzymes, our results, utilizing silver-stained electrophoretic gels, indicated that mGLP-1 was more resistant than native GLP-1 to trypsin and pancreatin cleavage but not pepsin degradation (Fig 2). mGLP-1 was resistant to trypsin cleavage for up to 8 hours, whereas native GLP-1 was completely degraded at 8-h (Fig 2A). Both mGLP-1 and GLP-1 were quickly degraded after 5 min with pancreatin reaction (Fig 2B and 2C). After 15 min in pancreatin, GLP-1 was completely destroyed (Fig 2B), whereas faint mGLP-1 was still detectable (Fig 2C). These results demonstrate that replacement of Lys26, 34 with Gln26, and Asp34 in mGLP-1 result in increased resistance to trypsin and pancreatin digestion.
Fig 2. Resistance to trypsin cleavage, pancreatin degradation and pepsin hydrolysis.
Both GLP-1 and mGLP-1 were treated with trypsin (A), pancreatin (Band C) or pepsin (D) at 37°C. The reaction solutions were sampled at different time points and analyzed by SDS-PAGE. Protein bands were visualized using silver staining. mGLP-1 only; mGLP-1 incubated with trypsin for 1, 2, 4, 8, and 12 hours, respectively; GLP-1 only; GLP-1 incubated with trypsin for 1, 2, 4, and 8 hours, respectively. Negative control is trypsin only. GLP-1 (B) and mGLP-1 (C) were incubated with pancreatin for 5, 15, 30, 45, 60, 75, 90, 120, 150, 180, 210, and 240-min, respectively. (D) Lane 1: mGLP-1 incubated with pepsin; Lane 2: mGLP-1 only; Lane 3: GLP-1 incubated with pepsin; Lane 4: GLP-1 only.
In contrast to trypsin, silver staining of electrophoretic gels indicated that GLP-1 and mGLP-1 were both degraded by pepsin within 10 min (Fig 2D). Neither native GLP-1 nor mGLP-1 was resistant to pepsin degradation. This is because pepsin mainly hydrolyzes peptide bonds of aromatic amino acids and acidic amino acids [22]. The presence of those bonds in GLP-1 and mGLP-1 increase their susceptibility to pepsin hydrolysis.
mGLP-1 promotes mouse pancreatic β-cell proliferation, regulates gene expression, and stimulates insulin secretion
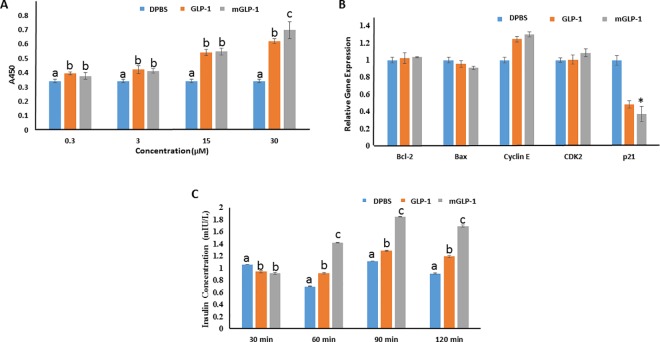
Insulin, which is the most potent anabolic human hormone known to decrease glucose levels, is produced and released by β-cells in response to elevated levels of blood glucose [23, 24]. The impairment of β-cells results in insulin deficiency, which in turn promotes elevated blood glucose levels. A chronically elevated blood glucose level is toxic to β-cells, causing even greater impairment and damage to β-cells [23]. GLP-1 has multiple beneficial effects on β-cells, including increasing the number of β-cells by inhibiting apoptosis, enhancing β-cell neogenesis, and promoting their proliferation [25, 26]. In the present study, the mouse pancreatic β-cell line, MIN6, was used to determine the effect of mGLP-1 on cell proliferation (Fig 3A and 3B). Both mGLP-1 and GLP-1 stimulated MIN6 cells proliferation in a dose-dependent manner. At a concentration of 30 μM, mGLP-1 exhibited greater cell viability rate (104.10% ± 1.94%) than GLP-1 (81.37% ± 5.87%) (P≤0.05) (Table 2). These results indicate that mGLP-1 performed in a similar manner to native human GLP-1 in promoting MIN6 β-cell proliferation. Relative to GLP-1, mGLP-1 was more stable when incubated with MIN6 cells for 48 hours in vitro and induced a higher rate of cell proliferation. The relative expression level of genes related to cell proliferation and apoptosis was also consistent with the effect of GLP-1 and mGLP-1 on the level of cell proliferation (Fig 3B). The cyclin E-CDK2 complex plays an important role in regulating the G1 phase of the G1/S cell cycle [27], while p21 is a universal cyclin-dependent kinase inhibitor (CKI) [28]. The relative expression of cyclin E and CDK2 genes were upregulated in mGLP-1- and GLP-1-treated cells, while the p21gene was down-regulated. Bcl-2 and Bax genes are two important members of the Bcl-2 gene family but they have the opposite function of either inhibiting or promoting cell apoptosis, respectively [29]. The relative expression of Bcl-2 was slightly upregulated in GLP-1- and mGLP-1-treated cells while Bax was down-regulated.
Fig 3.
Mouse pancreatic β cell proliferation (A), RT-qPCR analysis of gene expression (B), and insulin secretion (C). MIN6 cells were seeded into flat-bottomed 96-well microtiter plates at a density of 6.0×104 cells per well. (A) Cell proliferation assay: cells were treated with various concentrations (0.3, 3, 15 and 30 μM) of mGLP-1 or GLP-1 for 48h, 10 μL CCK8 was then added to each well and incubated for 1 to 4 hours to determine the optimal reading of OD450. The control was cell cultures treated with DPBS only. (B) Relative expression of genes related with proliferation and apoptosis in cells treated with mGLP-1, GLP-1, or DPBS as determined by RT-qPCR (n = 3). (C) Insulin secretion assay: Mouse pancreatic β cells were incubated with 15 μM GLP-1 or mGLP-1 in the presence of glucose (10 mM) for 30, 60, 90, or 120 min. The controls were cells incubated with just DPBS in the presence of 10mM glucose. Cell culture supernatants were collected and insulin concentration determined using a mouse insulin ELISA kit (JiNingShiYe Ltd. Shanghai, China). Data shown represent the mean ±SD (n = 6). Different letters or (*) indicate significant difference at p<0.05.
Table 2. Cell viability ratio (CRV) of MIN6 cells treated with different concentrations of GLP-1 or mGLP-1.
| Concentration (μM) | CRV (%) | |
|---|---|---|
| mGLP-1 | GLP-1 | |
| 0.3 | 10.58 | 15.65 |
| 3 | 20.58 | 23.65 |
| 15 | 60.26 | 58.56 |
| 30 | 104.10 | 81.37 |
GLP-1 stimulates pancreatic β-cells insulin secretion in a glucose-dependent manner. Therefore, the ability of mGLP-1to stimulate insulin secretion in a mouse pancreatic β-cell line, MIN6, was assessed. In this assay, 15μM GLP-1 or mGLP-1, in conjunction with 10 mM glucose, was incubated with MIN6 cells for various times. As illustrated in Fig 3C, both GLP-1 and mGLP-1 promoted insulin release from MIN6 cells, relative to 10 mM glucose alone. It appeared that mGLP-1 had a greater ability than GLP-1 to stimulate insulin secretion. At 60, 90 and 120-min of incubation, mGLP-1 clearly induced a higher level of insulin secretion from MIN6 cells than did GLP-1. Furthermore, the relative gene expression level of pancreatic-specific and duodenal homeobox gene 1 (Pdx1) and Ins1 were significantly up-regulated in mGLP-1- and GLP-1-treated cells (data not shown). Many transcription factors are involved in regulating the expression of the insulin gene and studies have linked the expression of the Pdx1 transcription factor to the occurrence of type 2 diabetes [30]. Pdx1, as a transcription factor expressed in pancreatic endocrine cells, promotes the expression of the pro-insulin gene, Glut2 gene, as well as other genes [31]. Thus far, the collective results indicate that mGLP-1 retains the bioactivity of native GLP-1 and is more stable and potent than GLP-1 in vitro.
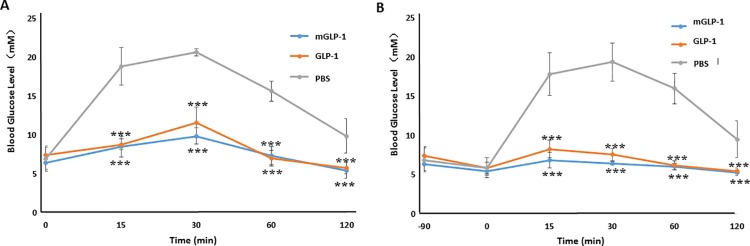
mGLP-1 improves Oral Glucose Tolerance (OGTT) in mice
An OGTT test was performed in order to assess the bioactivity of mGLP-1 on blood glucose (Fig 4). The glucose level in the plasma of mice was significantly (p<0.001) reduced at various time points (15, 30, 60 and 90-min) in mice that received a bolus administration of glucose after receiving a prior intraperitoneal injection of GLP-1 or mGLP-1. The level of glucose reduction in mice treated with mGLP-1 or GLP-1 30 min prior to a glucose challenge was not significantly different (Fig 4A). mGLP-1 and GLP-1 also decreased blood glucose significantly when they were administered 90 min prior to the bolus administration of glucose (Fig 4B). These data indicate that mGLP-1 improved glucose tolerance and promoted insulin secretion in mice in a manner similar to native GLP-1.
Fig 4. Oral glucose tolerance test (OGTT) in mice.
GLP-1 or mGLP-1 was administered to mice by intraperitoneal injection (IP) 30min (A) or 90 min (B) prior to a glucose challenge (OGTT). Blood glucose level was analyzed with a glucometer (Sannuo, Changsha, China). Data shown represent the mean ±SD (n = 6). *** indicates a significant difference at p<0.001.
mGLP-1 lowers plasma glucose in STZ-induced type 2 diabetic mice
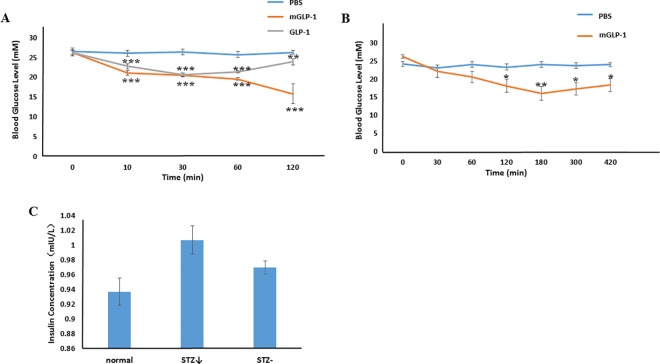
STZ is toxic to pancreatic β-cells and is often used to experimentally induce diabetes mellitus in mouse and rat. As compared to intraperitoneal injection of phosphate-buffered saline (PBS) alone, injection of mGLP-1 or GLP-1 into STZ-induced diabetic mice both significantly decreased blood glucose levels over a 10–120 min period of time (Fig 5A). Glucose levels in GLP-1-treated mice initially decreased relative to the control within the first 30 min but then gradually increased from 30 to 120 min. In contrast, blood glucose levels continually decreased in mGLP-1-treated mice over the entire 120 min (Fig 5A). In fact, glucose levels continually decreased for up to 180 min in mGLP-1-treated mice, after which time they gradually increased from 180–420 min. However, glucose levels at the latest time point were still lower than in PBS-treated mice (Fig 5B). In comparison, glucose levels were significantly lower in mGLP-1-treated mice for 300 min longer than in GLP-1-treated mice. These results demonstrate that GLP-1 has less potency than mGLP-1 in lowering blood glucose levels. This may be due to the shorter half-life of native GLP-1 caused by DPP-IV, trypsin, or pancreatin digestion as illustrated in Fig 2. mGLP-1 may be more resistant to DPP-IV degradation than GLP-1 due to the mutation of the DPP-IV target amino acid and the ability of mGLP-1 to stimulate the release of insulin as shown in Fig 5C. Therefore, mGLP-1 may have a longer half-life than GLP-1 and exhibit prolonged longer period of biological activity than native GLP-1.
Fig 5. Glucose levels and insulin secretion in STZ-induced mice.
Blood glucose levels in measured in STS-induced mice that received an intraperitoneal injection (IP) of PBS (control), GLP-1 or mGLP-1. (A) The blood glucose level was measured at 0, 10, 30, 60 and 120 min. (B) Intraperitoneal injection (IP) of PBS (control) or mGLP-1 in STZ-induced diabetic mice. The blood glucose level was measured at 0, 30, 60, 120, 180, 300, and 420 min. (C) Insulin secretion at the 180 min time point (n = 3). STZ↓: mGLP-1-treated STZ-induced diabetic mice with reduced blood sugar; STZ-: STZ-induced diabetic mice with high glucose level. Data shown represent the mean ±SD (n = 6, except where noted). * represents p<0.05; ** represents p<0.01; *** represents p<0.001.
It is interesting to note that when an oral gavage was used to administer either GLP-1 or mGLP-1 to STZ-induced diabetic mice, no differences in glucose levels were observed at various time points relative to PBS-treated mice (data not shown). Small peptides, such as GLP-1 or mGLP-1, can be easily degraded in the alimentary canal due to the presence of various proteases, such as pepsin, a powerful proteolytic enzyme [32]. It is also possible that native GLP-1 and mGLP-1 are metabolized by the liver and therefore, do not have a chance to be systemically distributed in the blood stream [33]. Peptides and larger proteins have become increasingly explored as therapeutic agents because of their efficacy, potency and selectivity [34]. Oral administration of drugs is the most widely-used, and preferred method of delivering therapeutic agents. Therefore, further studies will be required to enhance the absorption of the mGLP-1 analogue and improve its resistance to degradation by proteases.
In summary, the present study demonstrated that synthetic mGLP-1 is more resistant to trypsin and pancreatin than native GLP-1. mGLP-1 promotes β-cell proliferation by increasing the relative expression of cyclin E, CDK2, Bcl-2 genes and down-regulation of the p21 and Bax genes; all of which are involved in the regulation of cell proliferation and apoptosis. mGLP-1 also improved glucose tolerance in mice. Collectively, the data in the present study demonstrates that mGLP-1 significantly reduces blood sugar levels and stimulates insulin secretion in mice. Further research and development of mGLP-1 will increase its potential as a therapeutic agent to be used as a GLP-1 analogue in type 2 diabetic patients.
Data Availability
All relevant data are within the paper.
Funding Statement
This work was supported by the National Biotechnology Development Plan (2016ZX08005-004), and the Researcher Foundation of the Chinese Academy of Agricultural Sciences.
References
- 1.American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2012;35:S64–S71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.International Diabetes Federation. 2015;http://www.diabetesatlas.org/.
- 3.American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2010; 33:S62–S69. 10.2337/dc10-S062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.LeRoith D. β-cell dysfunction and insulin resistance in type 2 diabetes: role of metabolic and genetic abnormalities. Am J Med. 2002;113:3S–11S. [DOI] [PubMed] [Google Scholar]
- 5.Bell GI, Sanchez-Pescador R, Laybourn PJ, Najarian RC. Exon duplication and divergence in the human preproglucagon gene. Nature. 1983;304:368–371. [DOI] [PubMed] [Google Scholar]
- 6.Perfetti R, Merkel P. Glucagon-like peptide-1: a major regulator of pancreatic beta-cell function. Eur J Endocrinol. 2000;143:717–725. [DOI] [PubMed] [Google Scholar]
- 7.Holst JJ. The physiology of glucagon-like peptide 1. Physiol Rev. 2007;87:1409–1439. 10.1152/physrev.00034.2006 [DOI] [PubMed] [Google Scholar]
- 8.Kreymann B, Ghatei MA, Williams G, Bloom SR. Glucagon-like peptide-1 7–36: a physiological incretin in man. The Lancet. 1987;330:1300–1304. [DOI] [PubMed] [Google Scholar]
- 9.Kieffer TJ, McIntosh CH, Pederson RA. Degradation of glucose-dependent insulinotropic polypeptide and truncated glucagon-like peptide 1 in vitro and in vivo by dipeptidyl peptidase IV. Endocrinology. 1995;136:3585–3596. 10.1210/endo.136.8.7628397 [DOI] [PubMed] [Google Scholar]
- 10.Marchetti P, Lupi R, Bugliani M, Kirkpatrick CL, Sebastiani G, Grieco FA, et al. A local glucagon-like peptide 1 (GLP-1) system in human pancreatic islets. Diabetologia. 2012;55:3262–3272. 10.1007/s00125-012-2716-9 [DOI] [PubMed] [Google Scholar]
- 11.Green BD, Liu HK, McCluskey JT, Duffy NA, O'Harte FPM, McClenaghan NH, Flatt PR. Function of a long-term, GLP-1-treated, insulin-secreting cell line is improved by preventing DPP IV-mediated degradation of GLP-1. Diabetes Obes Metab. 2005;7:563–569. 10.1111/j.1463-1326.2004.00430.x [DOI] [PubMed] [Google Scholar]
- 12.Knudsen LB, Nielsen PF, Huusfeldt PO, Johansen NL, Madsen K, Pedersen FZ, et al. Potent derivatives of glucagon-like peptide-1 with pharmacokinetic properties suitable for once daily administration. J Med Chem. 2000;43:1664–1669. [DOI] [PubMed] [Google Scholar]
- 13.DeFronzo RA, Ratner RE, Han J, Kim DD, Fineman MS, Baron AD.Effects of exenatide (exendin-4) on glycemic control and weight over 30 weeks in metformin-treated patients with type 2 diabetes. Diabetes Care. 2005;28:1092–1100. [DOI] [PubMed] [Google Scholar]
- 14.Jomori T, Hayashi YJ, Makino M. GLP-1 Derivative and use thereof. International Patent Application. 2008;2008056726.
- 15.Cho YM, Fujita Y, Kieffer TJ. Glucagon-like peptide-1: glucose homeostasis and beyond. Annu Rev Physiol. 2014;76:535–559. 10.1146/annurev-physiol-021113-170315 [DOI] [PubMed] [Google Scholar]
- 16.Brandsma M, Wang X, Diao H, Kohalmi SE, Jevnikar AM, Ma S. A proficient approach to the production of therapeutic glucagon-like peptide-1 (GLP-1) in transgenic plants. Open Biotechnol J. 2009;3:57–66. [Google Scholar]
- 17.Kong Y, Tong Y, Gao M, Chen C, Gao X, Yao W. Linker engineering for fusion protein construction: improvement and characterization of a GLP-1 fusion protein. Enzyme Microb Tech. 2016;82:105–109. [DOI] [PubMed] [Google Scholar]
- 18.Furman BL. Streptozotocin-induced diabetic models in mice and rats. Curr Protoc Pharmacol. 2015;5:1–20. [DOI] [PubMed] [Google Scholar]
- 19.Knudsen LB, Pridal L. GLP-1 (9–36) amide is major metabolite of GLP-1 (7–36) amide after in vivo administration to dogs, and it acts as an antagonist on the pancreatic receptor. Eur J Pharmacol. 1996;318:429–435. [DOI] [PubMed] [Google Scholar]
- 20.Kieffer TJ, Francis HJ. The glucagon-like peptides. Endocr Rev. 1999;20:876–913. 10.1210/edrv.20.6.0385 [DOI] [PubMed] [Google Scholar]
- 21.Tu P, Ma Z, Wang H, Ma B, Li X, Duan H, et al. Expression of CTB-10× rolGLP-1 in E. coli and its therapeutic effect on type 2 diabetes. Curr Pharm Biotech. 2015;16:564–572. [DOI] [PubMed] [Google Scholar]
- 22.Daly MM, Mirsky AE, Ris H. The amino acid composition and some properties of histones. J Gen Physiol. 1951;34:439–450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Scheen AJ. Pathophysiology of type 2 diabetes. Acta Clin Belg. 2014;58:335–341. [DOI] [PubMed] [Google Scholar]
- 24.Saltiel AR, Kahn CR.Insulin signalling and the regulation of glucose and lipid metabolism. Nature. 2001;414:799–806. 10.1038/414799a [DOI] [PubMed] [Google Scholar]
- 25.Bulotta A, Farilla L, Hui H, Perfetti R. The role of GLP-1 in the regulation of islet cell mass. Cell Biochem Biophy. 2004;40:65–77. [DOI] [PubMed] [Google Scholar]
- 26.Ma B, Tu P, Zhao X, Zhang Y, Wang Y, Ma C, et al. Expression and Purification of Optimized rolGLP-1, A novel GLP-1 analog, in Escherichia Coli BL21 (DE3) and its good glucoregulatory effect on type 2 diabetic mice. Curr Pharm Biotech. 2013;14:985–994. [DOI] [PubMed] [Google Scholar]
- 27.Koff A, Giordano A, Desai D, Yamashita K, Harper JW, Elledge S, et al. Formation and activation of a cyclin E-cdk2 complex during the G1 phase of the human cell cycle. Science. 1992;257:1689–1694. [DOI] [PubMed] [Google Scholar]
- 28.Xiong Y, Hannon GJ, Zhang H, Casso D, Kobayashi R, Beach D. p21 is a universal inhibitor of cyclin kinases. Nature. 1993;366:701–704. 10.1038/366701a0 [DOI] [PubMed] [Google Scholar]
- 29.Oltval ZN, Milliman CL, Korsmeyer SJ. Bcl-2 heterodimerizes in vivo with a conserved homolog, Bax, that accelerates programed cell death. Cell. 1993;74:609–619. [DOI] [PubMed] [Google Scholar]
- 30.Hagman DK, Hays LB, Parazzoli SD, Poitout V. Palmitate inhibits insulin gene expression by altering PDX-1 nuclear localization and reducing MafA expression in isolated rat islets of Langerhans. J Biol Chem. 2005;280:32413–32418. 10.1074/jbc.M506000200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wang H, Iezzi M, Theander S, Antinozzi PA, Gauthier BR, Halban PA, Wollheim CB Suppression of Pdx-1 perturbs proinsulin processing, insulin secretion and GLP-1 signalling in INS-1 cells. Diabetologia. 2005;48:720–731. 10.1007/s00125-005-1692-8 [DOI] [PubMed] [Google Scholar]
- 32.Tozaki H, Odoriba T, Iseki T, Taniguchi T, Fujita T, Murakami M, et al. Use of protease inhibitors to improve calcitonin absorption from the small and large intestine in rats. J Pharm Pharmacol. 1998;50:913–920. [DOI] [PubMed] [Google Scholar]
- 33.Gibaldi M, Boyes RN, Feldman S. Influence of first‐pass effect on availability of drugs on oral administration. J Pharm Sci. 1971;60:1338–1340. [DOI] [PubMed] [Google Scholar]
- 34.Frokjaer S, Otzen DE. Protein drug stability: a formulation challenge. Nat Rev Drug Discov. 2005;4:298–306. 10.1038/nrd1695 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All relevant data are within the paper.