Abstract
Objective. To describe a student-centered teaching method used to introduce a pharmacist patient care process (PPCP) during the first year of a doctor of pharmacy (PharmD) program.
Design. In the fall of 2014, a cohort of students (n=85) began an integrated pharmacotherapy (IPT) course sequence in the first semester of pharmacy school. The first course in this sequence laid the foundation for the delivery of care, focusing on the individual components of a PPCP. Faculty member used a variety of teaching methods in the course to introduce medication history taking, identification of drug-related problems, identifying components of a patient case, and learning/beginning to write subjective, objective, assessment, plan (SOAP) notes. Students’ SOAP notes submissions and performance on multiple-choice examinations were evaluated to demonstrate evidence of learning. Students also completed online course evaluations.
Assessment. Course-imbedded assessments were designed to measure student learning related to individual School of Pharmacy outcomes and course learning objectives. The mean individual student score on exam questions related to the PPCP topics was 83.7%±18.8%. The majority of students (86%-88%) rated their progress on achieving course learning objectives as “substantial” or “exceptional.” Students also enrolled in the introductory pharmacy practice experience (IPPE) in a community setting after completing the first IPT. The students performed significantly better than a historic cohort in identifying actual and potential drug therapy problems.
Conclusion. The described teaching methods, when introduced in early curricular stages, are effective in building a foundation for learning PPCP.
Keywords: introductory pharmacotherapy course, PPCP (pharmacists’ patient care process), medication history, SOAP notes
INTRODUCTION
Pharmacists are specially educated to focus on medication-related problems to improve and ensure achievement of optimal patient care. Hepler and Strand originally proposed a pharmaceutical care model in which pharmacists would collaborate with other healthcare professionals to design, implement, and monitor a therapeutic plan to achieve desired therapeutic outcomes in their patients.1 This pharmaceutical care model has been incorporated in pharmacy school curricula for over two decades. However, according to the Joint Commission of Pharmacy Practitioners’ (JCPP) report, considerable variability still exists in how this process is taught and practiced.2 The recent revision of the Accreditation Council for Pharmacy Education (ACPE) standards endorses the JCPP Vision of Pharmacy Practice, with the curricular standard stating the need to prepare students who are able to provide patient-centered collaborative care as described in the Pharmacists’ Patient Care Process (PPCP). The process delineates five continuous steps in providing patient care: collecting patient data, assessing and analyzing the information collected, developing a patient-centered treatment plan, implementing the plan, and monitoring/evaluating the care plan and patient as needed. Teaching a systematic approach to patient case evaluation is not unique to pharmacy education: a somewhat similar process, the “model of clinical judgment,” is used in teaching nursing students.3 ACPE’s 2016 Standards recommend incorporating elements of PPCP into pharmacy programs’ didactic and experiential courses.
Given the ever-changing and constantly growing field of pharmacy, there is an increased amount of knowledge that students are expected to accumulate going through the professional curriculum. Additionally, this knowledge rapidly becomes obsolete given new developments and progress made towards developing new medications and better approaches to patient care. In fact, including all of the content necessary to learn to practice competent direct patient care within the didactic curriculum is not possible.4 Therefore, teaching students a standard process for or approach to patient care can help them in navigating through both familiar and unfamiliar scenarios. This approach may better prepare students for the experiential components of their curriculum, and, eventually, for the entry-level practice, where they will be challenged with taking care of patients with more complicated health issues. Learning to implement this systematic process may aid in working up patients with multiple co-morbidities, while taking into consideration socioeconomic/health literacy barriers, and focusing on optimizing patient care through interprofessional collaboration (at the later curricular stages).
In a recent search of medical, nursing, and pharmacy education literature regarding the early introduction of the patient care process or a systematic approach to patient evaluation and management, little data was found. A search of the Medline and CINAHL plus databases was conducted using the search terms “early teaching” and “patient care process.” The search focused on articles published between 2004 and 2016 in medical, nursing, and pharmacy education journals. The search identified 205 articles, of which only 9 were somewhat relevant to this report. Many researchers have investigated using case-based teaching or problem-based teaching in health professional education. Furthermore, in several studies, students reported benefitting from receiving an early overview of the patient care process. However, few researchers reported other measurable outcomes.5-7 More information on the systematic application of the patient care process is available from advanced-level didactic courses or experiential components of the curriculum, in both pharmacy and nursing programs.4,8-10
One research report from a nursing education journal suggested that using more student-centered approaches in developing patient care plans while using concept maps or problem-based learning in first semester undergraduate nursing education resulted in increased critical-thinking scores.11 Critical-thinking skills are important in healthcare professional education.12 Pharmacy students are required to provide care in a complex healthcare environment that requires them to constantly engage in critical thinking. While an important finding, it is not possible to infer from this study whether introducing concept maps early in the curriculum and improving critical thinking scores prepares nursing students for the experiential portion of their education.
Another study in the nursing literature described using mind-mapped care plans in the first semester of a professional program. Mind mapping to plan patient care was implemented early in the nursing curriculum to introduce this approach for future use in an experiential curriculum. The process was introduced gradually, first using nonmedical cases, then using medical cases during classroom instruction, and then using actual patient cases. The mind-mapping process included placing the patient in the center of care, with expected signs and symptoms, assessment data, nursing diagnosis, nursing intervention, and patient-centered outcomes originating from the patient. An optimal level of functioning was defined by both the nursing student and the patient, making this mind-mapping care-planning approach more holistic and individualized.13 In this report, 85% of students surveyed in the final semester of the program reported that using this approach helped them explain their plan of care to their faculty members and peers.
While nursing education journals provided some insight on introducing systematic approaches to patient care early in nursing curricula, neither a search of the databases nor a search of pharmacy education journals identified articles on the early introduction of PCPP or systematic approaches to the delivery of care in pharmacy programs.
Students are expected to have relative proficiency in medication history taking or preparing a patient-centered plan by the time they reach experiential courses.14 However, there may be inconsistencies in the formal teaching and practicing of these essential skills in pharmacy programs, which may be implemented from early to late curricular stages, with the former allowing more time for practice in a low-risk, low-stakes environment.
This article offers a step-wise approach to introducing foundational PPCP concepts in the early curricular stages to build a foundation for the continuous application of PPCP principles in subsequent courses.
DESIGN
This article describes the evaluation of the teaching methods used in educating students on the fundamentals of the delivery of care and PPCP. The educational environment of the Fairleigh Dickinson University’s (FDU’s) School of Pharmacy, specific content from the introductory IPT I course, and specific course assessments provided a relevant context for determining the impact of this approach on student learning. Performance in an experiential course related to this content provides a means of demonstrating an adequate learning of skills related to PPCP and the ability to apply this approach in a clinical setting. This project was evaluated by the FDU Institutional Review Board (IRB) and determined to be exempt from IRB review and approval as it did not to meet the definition of human subjects research.
The school offers a four-year doctor of pharmacy (PharmD) degree. The approximate class size at the time of this study was 85 students per professional year. The school’s student admission requirements included either completion of a baccalaureate degree or 90 credits of undergraduate education. The school’s professional curriculum contained a sequence of 10 integrated pharmacotherapy courses starting in the first semester of the first year. The sequence begins with the Foundations in Integrated Pharmacotherapy I (IPT I) course. This three-credit course provided an introduction to pathophysiology, genetics, immunology, microbiology, and the delivery of care. The course had basic science and clinical components, and had approximately one credit hour allocated to teaching content related to the delivery of patient-centered care. In this segment, students were taught individual components of PPCP, as developed by the JCPP. Faculty member used a variety of case-based application exercises, including: “deconstructing” a patient case, observing a medication history, identifying a drug-related problem using a systematic approach from an observed medication history, developing a plan, and writing a SOAP note.
Students enrolled in the introductory pharmacotherapy course in fall 2014 met twice a week for 75 minutes as an entire cohort of 85 students. The students were seated in an auditorium that contained 11 round tables accommodating nine students each. This seating created self-selected groups for application exercises. All students used iPads to access Internet/library databases and other resources. Instant polling software was used to engage students in case discussions. All of these resources were available to students throughout the PharmD curriculum but were not specifically required for this course.
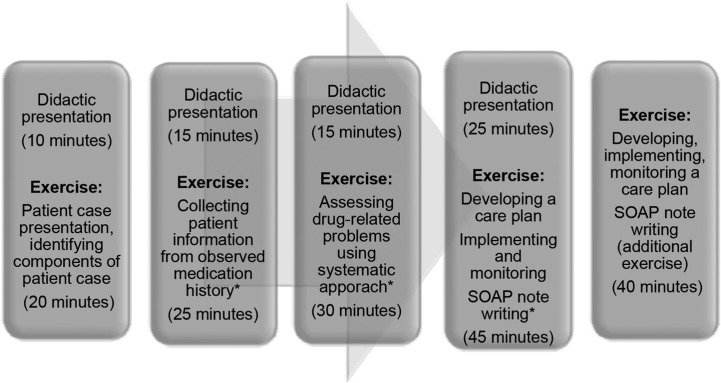
The segment of the introductory IPT I course on the delivery of care and PPCP was primarily applications-based. This segment was introduced after the students had been exposed to immunology, including limited aspects of clinical immunology, and clinical laboratory test interpretation. The student exercises included identifying components of patient case presentations, collecting patient information, assessing drug-related problems, and developing, implementing, and monitoring care plans using SOAP notes. The students went through these exercises twice in the course, applying the contextual material they had learned. Figure 1 illustrates when these exercises were implemented and the time spent on each exercise. Students were assessed formatively throughout the course, using instant polling case questions and rubrics. Rubrics were used primarily as a teaching tool to provide formative feedback to the students as they were learning to apply the complex clinical patient-centered care approach and document patient care activities. Faculty member did not adjust student course grades based on the formative feedback. Thus, faculty member intentionally allowed students to practice in a low-risk environment and to learn from their mistakes. Often the mistakes were collectively discussed in the course with the aim of avoiding them in the future. Below, specific exercises are described in detail.
Figure 1.
Exercises on PPCP/Delivery of Care
For the patient case presentation exercise, students were presented with a “patient story” in paragraph format. They were asked to “deconstruct” the case, which means to reorganize the story and identify the traditional components of a patient case presentation. For instance, students identified the patient’s chief complaint, history of the present illness, social history, review of systems, and all other elements. The students worked individually within a plain text file posted on the Blackboard learning management system to insert appropriate headings and move information around to format it as a patient case presentation. After they attempted this activity, a faculty member demonstrated this deconstruction/reorganization process in real time by projecting the text file on a screen and reorganizing it with students’ input; a discussion on case presentation ensued. No formal assessment of this activity was conducted. This exercise introduced students to a traditional case format that was used to communicate patient information in writing and verbally during interdisciplinary rounds.
The next phase involved collecting patient information where students learned to collect patient information during a simulated medication history scenario. A faculty member and a simulated patient (another faculty member) engaged in role-play, demonstrating how to take a medication history. Students observed this activity and documented the information on a general medication history form/worksheet. Immediately following this simulation, students participated in a faculty-led discussion on ways to improve the medication history-taking technique, what questions may have been missed, and other possible sources of patient information to be collected before an assessment was made. During this discussion, students informally self-assessed on what information they failed to collect, and added the missing information based on the discussion. This exercise introduced the first step of PPCP.
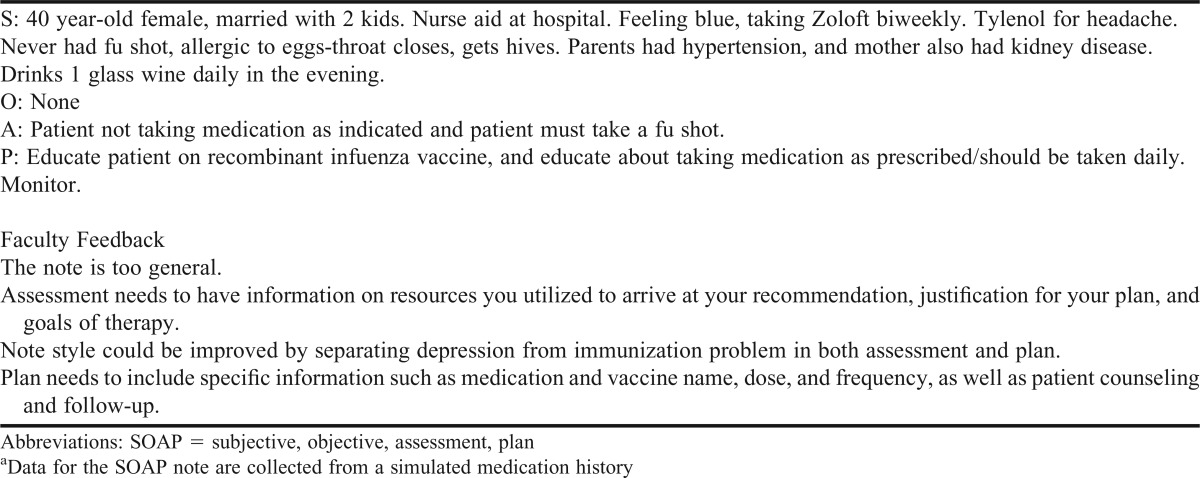
A short didactic segment introduced students to a systematic approach to the identification and assessment of drug-related problems.15 Students answered several multiple-choice polling questions, applying this approach to sample patient cases. At the conclusion of the segment, students were asked to identify drug-related problem(s) from the medication history they observed. This systematic evaluation took students approximately 20 to 30 minutes because this was their first attempt at identification of drug-related problems. The faculty member visited each group to make sure the activity was proceeding on track (ie, that students understood the questions, how to address them, and what to look for). They initially discussed their findings within their group of nine, and then each group reported its finding to the faculty member. The faculty member provided guiding worksheets (Figure 2) that helped students with the systematic evaluation of drug therapy during the exercise. This exercise introduced the “assess” step of PPCP.
Figure 2.
Worksheet for Identification of Drug-Related Problems with an Example Exercise
Based on their assessment of the drug-related problems, students created a care plan for the patient. Students discussed this proposed plan with their peers. After the plan was discussed, students learned about documenting pharmacists’ interventions using SOAP notes. The faculty member presented the concept of a SOAP note, which is a formal approach to document pharmacists’ recommendations/plans, as well as a commonly accepted standard way to communicate with other healthcare practitioners. A 25-minute lecture was given to introduce students to SOAP note writing. Sample patient cases were discussed and sample SOAP notes were presented and critiqued following the lecture. Several multiple-choice polling questions were used again as students applied the course material.
After this exercise, students attempted to write their first SOAP note in groups of 9. The SOAP note was written for the patient for whom the medication history had been collected; the worksheet used to identify drug-related problems in the previous exercise was used to guide the “assessment” and “plan” portions of the SOAP note. Students were given up to 45 minutes to complete this activity. The SOAP note rubric that was used to assess this activity was posted prior to class, and students could refer to it for guidance when they developed their notes. Students submitted their notes to the faculty member in real time during class via google form. The faculty member displayed responses from each table and provided an immediate critique and/or suggestions for improvement. By the next class period, all students received a Microsoft Office Word file containing each group’s submission with the faculty member’s comments and tracked changes (Table 1). To demonstrate evidence of learning, a group SOAP rubric assessment was also performed. In addition, a SOAP note written by the faculty member for this patient was shared with the class and discussed. Implementation and monitoring steps were described briefly to complete the process.
Table 1.
Student Group SOAP Note Submission and Faculty Feedback Examplea
An additional opportunity for students to collect information and assess a patient to develop a SOAP note was presented during the last meeting of the course. This case study incorporated clinical immunology applications and laboratory findings interpretation, both of which were taught in the earlier components of the course. The case also involved students in collecting relevant information from various sources (eg, the patient and an abbreviated medical record, which included a progress note, a physical examination, and a laboratory report). This opportunity challenged the students with a more sophisticated problem, requiring the synthesis of information from multiple sources, and integrated basic science and clinical concepts learned throughout the introductory pharmacotherapy course.
The pedagogy involved in the initial introduction of the complex PPCP involved increasing student/faculty contact, encouraging student cooperation, providing immediate formative feedback, and emphasizing time on task. These pedagogical dimensions are all considered best practices in education.16-18 An open-ended, semi-structured, multi-step exercise allowed students to critically think and evaluate the multitude of factors that pharmacists consider when caring for patients in clinical practice.
EVALUATION AND ASSESSMENT
The learning outcomes and objectives for the IPT I course, as well as student performance on course assessments related to these objectives, are summarized in Table 2. Interactive polling questions evaluated students’ ability to identify subjective and objective evidence related to patient cases, interpret evidence and patient data, and identify and define primary problem. As seen in Table 2, there was substantial variability in student performance on the case-based polling questions (higher on questions classified as application, lower on the questions classified as analysis). Students were challenged because the cases and the questions were specifically designed to be more thought-provoking to facilitate critical thinking and in-class discussion. Polling questions were used primarily as teaching and participation-tracking tools rather than assessments, as the students were still learning the material. Performance on these questions is reported primarily to document students’ growth within individual learning objectives of the course.
Table 2.
Integrated pharmacotherapy I-linked School of Pharmacy Outcomes, Objectives, and Assessments
The students’ first SOAP note demonstrated significant room for improvement (Table 2). The majority of the students were able to appropriately collect, organize, and document subjective and objective data. However, compiling a complete problem list, assessing and prioritizing problems, identifying treatment goals, creating plans and describing comprehensive monitoring parameters proved to be challenging on this first attempt at SOAP note writing.
A multiple-choice examination related to this material was administered. Questions were developed to evaluate the level of learning on individual course objectives. Of the 21 questions related to the delivery of care topics, 5 were classified as “analysis,” 9 as “application,” and 7 as “comprehension” questions based on cognitive Bloom’s taxonomy domains. Questions were distributed between domains to appropriately address the learning objectives of the course. Students’ average score was 83.7%±18.8%. Students performed well across cognitive domains.
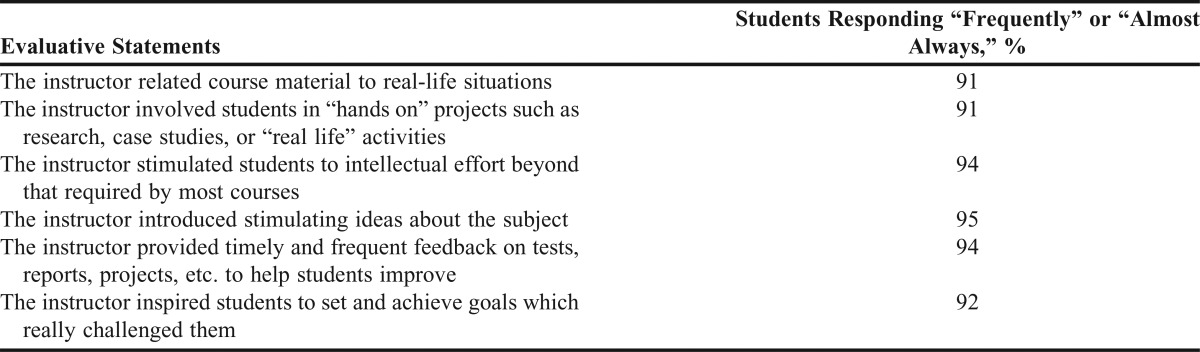
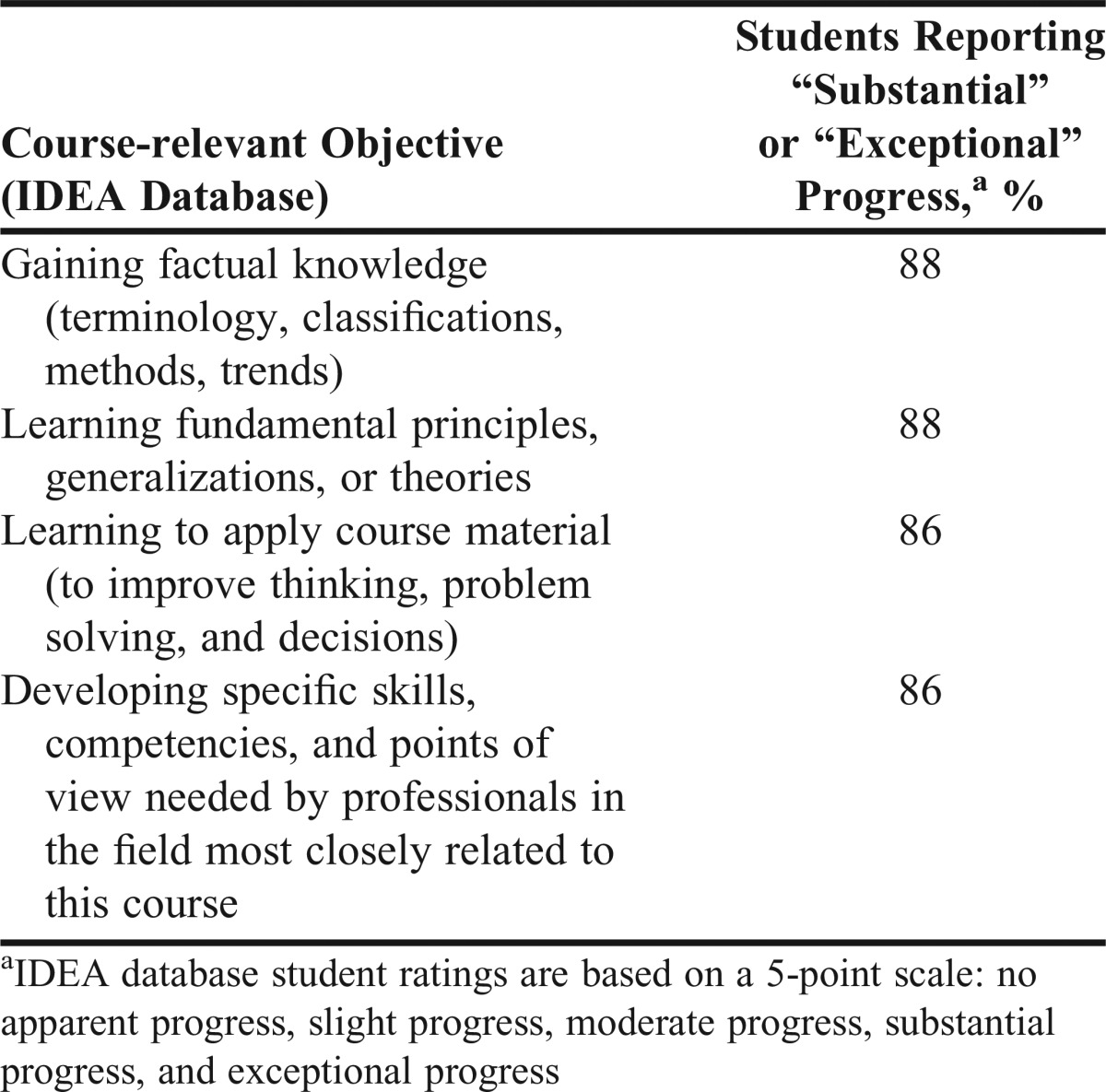
The course evaluations that students completed utilized the university’s IDEA database. IDEA uses a research-based, student ratings of the instruction (SRI) system that is specifically designed to evaluate student learning and outcomes. Sixty-five (76.5%) students voluntarily responded to the online survey, which was designed to have student self-evaluate their progress on course-relevant objectives. The survey instrument used a 5-point scale ranging from “no apparent progress” to “exceptional progress.” In the four learning objectives that the faculty members selected as important for this course, 86%-88% of students rated their own progress as “substantial” or “exceptional” (Table 3).
Table 3.
Student Self-assessment of Progress on Course-relevant Objectives
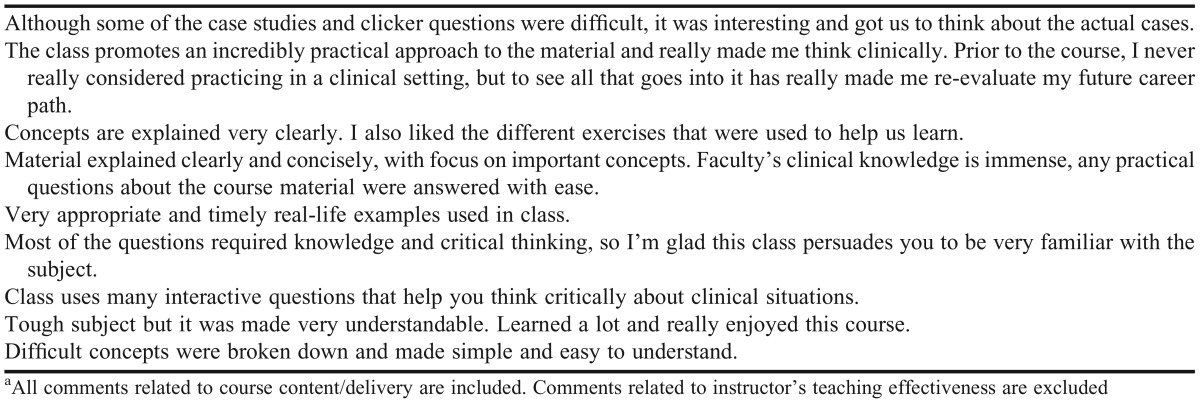
Course and faculty quantitative and qualitative evaluative data are presented in Tables 4 and 5. Overall, students found this course both challenging and stimulating; they report being engaged in case-based, real-life simulation and receiving timely feedback on their performance.
Table 4.
Course and Faculty Evaluation Data (Quantitative)
Table 5.
Course and Faculty Evaluation Data (Qualitative)a
DISCUSSION
This article discussed and evaluated one possible approach to teaching PPCP in the first semester of a PharmD program. In the introductory IPT I course, students achieved reasonably good scores on their summative assessment related to the delivery of care learning objectives. Students were most challenged with the two objectives under the “problem solver” outcome: “identify and define the primary problem” and “implement the most viable solution.” However, their performance improved from their initial attempts in answering polling questions and writing SOAP notes, demonstrating learning during the span of the course. Because students’ performance appeared to improve after completion of the additional practice cases offered during the course, it is reasonable to assume that the learning could be further improved by using additional cases to allow students more time to practice the application of concepts related to the patient care process. While this approach would be ideal, the faculty time currently dedicated to PPCP cannot be increased. Therefore, consideration will be given to required or extra-credit homework assignments specifically focused on these two objectives.
Students responded positively to learning and implementing various steps of the PPCP approach. The majority of the students agreed that the introductory IPT I course helped them in applying content to improve problem solving and decision-making. Also, as evidenced by students’ self-assessment after the IPT I course, these practice-based exercises helped build students’ confidence and understanding of the continuous process of patient-centered care. Students’ self-perceived progress on relevant objectives appears to be in line with their performance in the community IPPE, discussed below.
More than 90% of students reported that the IPT I course inspired them to set and achieve challenging goals. In fact, this was one of the main objectives set by the faculty member for this course. One of the biggest controversies in teaching this course early in the curriculum is students’ lack of foundational clinical knowledge. In fact, several questions originating from the audience during the exercises reminded the faculty member to use more simplistic language to explain PPCP components to these very inexperienced students. However, the faculty member found that students can focus on the systematic process more purely when they are first introduced to this concept and not preoccupied with reaching the “correct” clinical solution. In addition, students find this introduction to be stimulating, and it raises their curiosity and desire to acquire clinical knowledge. The students also strive to deliver the components of PPCP with competence, as evidenced by their course evaluation responses.
Ultimately, students should be able to demonstrate skills related to PPCP in a clinical practice setting. Here, student performance on competencies related to PPCP during their first introductory pharmacy practice experience (IPPE) in a community setting is reported. This course used a validated assessment instrument,19 and assigned students’ performance into one of four possible categories: “excellent,” “competent,” “deficient,” or “no opportunity to observe.” Students were considered competent if they received an “excellent” or “competent” assessment on the individual components of the instrument. Students’ performance was rated as “excellent” if they were able to work unsupervised when appropriate, able to discern when to seek advice, and took the extra steps required to move beyond what was expected in the course guidelines.
On the two competencies evaluated by community IPPE preceptors during the summer following completion of the course, 82% of students demonstrated competency in collecting a medication history and 97% of students demonstrated competency in identifying actual or potential drug therapy problems. Scores from a historic cohort (students who completed the course two years prior, where PPCP was not taught systematically) were compared to the study cohort using a two-tailed chi-square test, with p<.05 considered statistically significant (GraphPad Software Inc., La Jolla, CA). The historic and study cohorts were comparable based on admission parameters, such as gender (63% female vs 65%), age (average 24 years vs 23.7 years), the proportion of students with prior degrees (86% vs 79%), and average entering grade point average (3.4 vs 3.3).
While the overall number of students achieving at least a “competent” rating was similar between the two cohorts, there was a significant difference in the proportion of students rated “excellent” as opposed to “competent” in their ability to identify drug-related problems. In the study cohort, 20.2% more students were rated “excellent” on their ability to identify drug-related problems compared to the historic cohort (69.5% vs 49.3%, p=.04).
While this assessment is not a direct measure of a successful foundation laid in the IPT I, it attests to the potential value of early didactic teaching and formative feedback related to the delivery of care topics. Additional opportunities to the practice application of PPCP principles were provided in the integrated pharmacotherapy laboratory course prior to the commencement of the IPPE. The stepwise approach to the introduction and early practice of the skills related to PPCP laid out in the first year of the program helped more students build toward achieving “excellent” assessment on PPCP-related competencies in the community IPPE course.
Course faculty member encountered several challenges while implementing this teaching strategy in the IPT I course. One of the course’s challenges was the limited time allocated to do the application exercises. Students would benefit from having more time to practice various components of PPCP, especially related to identifying primary problems and implementing the most viable solutions in multiple clinical scenarios. Additional practice could also help build confidence in students when approaching patient care. The amount of time available for introducing new material was limited because the faculty member wanted to provide students with meaningful feedback through formative evaluations based on in-class exercises. While covering all aspects of the topic didactically may be considered important, in the opinion of the author, spending time on student-centered activities that develop their critical-thinking skills and teaching them to “think like a pharmacist” may be the most beneficial way to use class time. Demonstrating the thinking and the evaluative process that a pharmacist goes through before formulating a recommendation and follow-up plan (role-modeling), and then challenging the students to attempt to come up with their own assessment and plan may be the most important aspects of this course.
The application exercises demand more faculty time than traditional lectures. Course faculty member spent additional time designing exercises, engaging other faculty members, and providing feedback to the students (approximately 4-6 extra hours in addition to traditional lecture preparation). Moreover, whenever open-ended discussion ensued, the faculty member needed to be comfortable enough with the subject matter to handle unexpected student inquiries while keeping the discussion on track. In fact, the classroom management obstacles encountered by faculty members in implementing more student-centered activities can be overcome by gaining more experience and establishing a solid set of learning objectives for each exercise.20
In this experience, a slight increase in the faculty member’s time commitment to the course achieved the desired outcome as evidenced by formative and summative course evaluations, as well as by students’ self-assessment of their progress toward course-related objectives. Performance in the experiential course also supported this teaching approach as an effective means of teaching PPCP early in the pharmacy curriculum.
CONCLUSION
This article acknowledges an effective approach to teaching the delivery of care and the pharmacists’ patient care process to students in the first semester of the PharmD program. A consistent, systematic approach to the delivery of patient care curriculum content can benefit students’ development of clinically relevant problem-solving skills and confidence, as well as build a foundation for practicing PPCP in the didactic and experiential components of the curriculum.
REFERENCES
- 1.Hepler CD, Strand LM. Opportunities and responsibilities in pharmaceutical care. Am J Hosp Pharm. 1990;47(3):533–543. [PubMed] [Google Scholar]
- 2.Bennett M, Kliethermes MA, editors. How to Implement the Pharmacists’ Patient Care Process. Washington, DC: American Pharmacists Association; 2015. [Google Scholar]
- 3.Tanner CA. Thinking like a nurse: a research-based model of clinical judgment in nursing. J Nurs Educ. 2006;45(6):204–211. doi: 10.3928/01484834-20060601-04. [DOI] [PubMed] [Google Scholar]
- 4.Nielsen A. Concept-based learning activities using the clinical judgment model as a foundation for clinical learning. J Nurs Educ. 2009;48(6):350–354. doi: 10.3928/01484834-20090515-09. [DOI] [PubMed] [Google Scholar]
- 5.Dutra DK. Implementation of case studies in undergraduate didactic nursing courses: a qualitative study. BMC Nurs. 2013;12(1):15. doi: 10.1186/1472-6955-12-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wong FK, Cheung S, Chung L, et al. Framework for adopting a problem-based learning approach in a simulated clinical setting. J Nurs Educ. 2008;47(11):508–514. doi: 10.3928/01484834-20081101-11. [DOI] [PubMed] [Google Scholar]
- 7.Srinivasan M, Wilkes M, Stevenson F, Nguyen T, Slavin S. Comparing problem-based learning with case-based learning: effects of a major curricular shift at two institutions. Acad Med. 2007;82(1):74–82. doi: 10.1097/01.ACM.0000249963.93776.aa. [DOI] [PubMed] [Google Scholar]
- 8.Armor BL, Bulkley CF, Truong T, Carter SM. Assessing student pharmacists’ ability to identify drug-related problems in patients within a patient-centered medical home. Am J Pharm Educ. 2014;78(1):Article 6. doi: 10.5688/ajpe7816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brady JH, Caldwell DJ, Pate KA, Pate AN. An elective course on application of clinical pharmacy principles. Am J Pharm Educ. 2013;77(10):Article 216. doi: 10.5688/ajpe7710216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lucas KH, Testman JA, Hoyland MN, Kimble AM, Euler ML. Correlation between active-learning coursework and student retention of core content during advanced pharmacy practice experiences. Am J Pharm Educ. 2013;77(8):Article 171. doi: 10.5688/ajpe778171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Orique SB, McCarthy MA. Critical thinking and the use of nontraditional instructional methodologies. J Nurs Educ. 2015;54(8):455–459. doi: 10.3928/01484834-20150717-06. [DOI] [PubMed] [Google Scholar]
- 12.Oyler DR, Romanelli F. The fact of ignorance: revisiting the Socratic method as a tool for teaching critical thinking. Am J Pharm Educ. 2014;78(7):Article 144. doi: 10.5688/ajpe787144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kern CS, Bush KL, McCleish JM. Mind-mapped care plans: integrating an innovative educational tool as an alternative to traditional care plans. J Nurs Educ. 2006;45(4):112–119. doi: 10.3928/01484834-20060401-04. [DOI] [PubMed] [Google Scholar]
- 14.Sando KR, Elliott J, Stanton ML, Doty R. An educational tool for teaching medication history taking to pharmacy students. Am J Pharm Educ. 2013;77(5):Article 105. doi: 10.5688/ajpe775105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Cipolle RJ, Strand LM, Morley PC. Chapter 5: Drug therapy problems. In: Cipolle RJ, Strand LM, Morley PC, eds. Pharmaceutical Care Practice: The Patient-Centered Approach to Medication Management Services. 3rd ed. New York, NY: McGraw-Hill; 2012.
- 16. Chickering AW, Gamson ZF. Seven principles for good practice in undergraduate education. Washington Center News: American Association of Higher Education; 1987.
- 17.Grossman S, Conelius J. Simulation pedagogy with nurse practitioner students: impact of receiving immediate individualized faculty feedback. Creat Nurs. 2015;21(2):100–109. doi: 10.1891/1078-4535.21.2.100. [DOI] [PubMed] [Google Scholar]
- 18.Persky AM, Pollack GM. Using answer-until-correct examinations to provide immediate feedback to students in a pharmacokinetics course. Am J Pharm Educ. 2008;72(4):Article 83. doi: 10.5688/aj720483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ried LD, Doty RE, Nemire RE. A psychometric evaluation of an advanced pharmacy practice experience clinical competency framework. Am J Pharm Educ. 2015;79(2):Article 19. doi: 10.5688/ajpe79219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bonwell C, Eison J. Active learning: creating excitement in the classroom (ASHE-ERIC Higher Education Report No. 1). http://www.ed.gov/databases/ERIC_Digests/ed340272.html. Accessed December 11, 2015.