Case Presentation
The patient is a 31 year old male student and Operation Iraqi Freedom (OIF) Army Veteran who served two tours in Iraq as a medic in 2010 and 2012. He presented to a campus psychiatric student health clinic in March 2014 with the following chief complaint: “I feel on edge all the time… I keep thinking about what I saw in Iraq.”
History of Present Illness
During his deployments, the patient witnessed multiple injuries and casualties of comrades, civilians, and enemy combatants. He separated from the military in June 2013 and subsequently in enrolled in community college with a goal of obtaining a nursing degree(Figure 1). In January 2014, within weeks of beginning his studies, he began to experience recurrent disturbing thoughts of combat experiences and frequent panic attacks (heart pounding, difficulty breathing, sweating), particularly during dissections in anatomy lab. These severe reactions caused him to often leave lab prematurely and miss assignments. Simultaneously, he became increasingly irritable, with frequent angry outbursts toward students and professors. He reported severe insomnia(difficulty falling/ staying asleep, frequent snoring) and significant weight gain(30 pounds) since separating from the military. He reported that at the start of the semester he had initiated a vigorous fitness regimen and had purchased a bodybuilding supplement online to lose weight. He followed the package instructions and used it orally twice daily before workouts. He could not remember the brand name of the supplement, but said it was the same product he and many members of his military unit used during deployments in Iraq. He reported that bodybuilding supplement use was extremely common in the military, recalling “all of my friends used [supplements] to work out.” He denied any other medication or substance use, with the exception of binge alcohol use approximately once a month with military friends. He reported feeling distanced and “cut off” from the emotional experiences of people other than his military friends. Family history was notable for alcohol use disorder and posttraumatic stress disorder (PTSD) in an uncle who served in the military. Diagnostic and Statistical Manual- IV (DSM-IV) PTSD Checklist(PCL)(1) score at the time of entering treatment was 65(cutoff score=45–50), with prominent hyperarousal, re-experiencing, and avoidance symptoms.
Figure 1.
Timeline of Events.
PCL = PTSD Checklist Score
Course of Treatment
At the initial visit in March 2014, the patient was diagnosed with PTSD. He was prescribed a selective serotonin reuptake inhibitor(SSRI), sertraline 25 milligrams daily for 7 days, then 50 milligrams daily; instructed to provide a list of all supplements; and referred for cognitive behavioral therapy for PTSD and an evaluation for sleep apnea. He was encouraged to abstain from alcohol and educated about healthy drinking limits. He agreed to reduce his alcohol use and declined substance abuse treatment.
The patient returned for follow-up one month later. He reported adherence with the SSRI and therapy and no binge alcohol use. He noted some improvement of his PTSD scores(PCL score=55), with reduction in avoidance symptoms. However, he continued to endorse prominent hyperarousal, panic and re-experiencing symptoms that were interfering with his academic studies. He had been diagnosed with sleep apnea and started on continuous positive airway pressure (CPAP), but continued to report difficulty with sleep initiation and maintenance. He had lost six pounds on his fitness regimen and reported continued use of the bodybuilding supplement, which he identified as “Jack 3-D,”manufacturer USP Laboratories, with the following ingredients: 1, 3 dimethylamylamine(DMAA), arginine alpha-ketoglutarate, creatine monohydrate, beta alanine, schizandrol A, and caffeine. He reported using two 5.55 gram scoops of the product with 8 ounces of water before workouts twice daily and denied compulsive use or overuse. His providers educated him about the risks of continued unprescribed supplement use and strongly advised him to stop using it, which he agreed to do. No other changes were made to his treatment plan.
Several weeks later, the patient returned for his second follow-up appointment. He had remained adherent with the treatment plan and had discontinued the supplement as recommended by his providers. At this visit, there was a notable drop in his self-reported PTSD symptoms (PCL score=36) and he no longer met full criteria for PTSD. In particular, hyperarousal, re-experiencing, and insomnia symptoms had noticeably improved since the prior visit. He was better able to tolerate anatomy lab without experiencing panic or extreme irritability. The patient had regained five pounds since discontinuation of the supplement and was referred to a nutritionist. He has continued to engage in weekly individual therapy and medication management every 1–2 months and his PTSD symptoms have remained in remission since discontinuation of the supplement.
Stimulant-Based Supplements: Difficult to Regulate, Easy Access
The current case describes the onset and exacerbation of hyperarousal, panic, insomnia, and re-experiencing symptoms of PTSD with concomitant DMAA ingestion in a combat veteran. DMAA is a sympathomimetic amine stimulant(2) and additive in popular workout supplements marketed to promote weight loss and improve strength and performance. The patient was adherent with the SSRI and outpatient therapy during the observed period, so it is possible that his symptom reduction can be entirely attributed to engagement in treatment. However, the temporal relationship between symptom onset and initiation of the supplement and remission of symptoms with discontinuation suggests an association, though causality cannot be established.
In response to numerous reports of adverse events associated with DMAA, including cardiac arrest, liver failure, hemorrhagic stroke, and death(2), the Food and Drug Administration (FDA) banned products containing DMAA from the market in April 2013(3). The Department of Defense (DoD) prohibited DMAA use in military personnel and removed DMAA- containing products from military commissary shelves. While these actions have likely curtailed use of DMAA-containing products, DMAA and many other stimulant-containing nutritional supplements remain widely available to consumers and have been difficult to regulate (2). Examples of stimulant bodybuilding products available online include 1,3-dimethylbutylamine (DMBA) supplements such as “Frenzy” (Driven Sports) and “Contraband” (Iron Forged Nutrition)(4) and beta-methylphenylethylamine (BMPEA) products such as “Black Widow” (Hi-Tech Pharmaceuticals) and “Jet Fuel Superburn” (GAT)(5).
Performance-Enhancing Supplement and Stimulant Use in Active Duty Military and Veterans
Use of performance-enhancing supplements is widespread among younger generations of military personnel. Cross-sectional data from the Millennium Cohort Study, a survey of 106,698 active duty service members conducted in 2007 during the wars in Afghanistan (Operation Enduring Freedom, [OEF]) and Iraq ([OIF]), revealed that 46.7% of respondents reported bodybuilding, energy, and weight-loss supplement use (6), and 22.0% reported use of multiple supplements. Deployment (odds ratio [OR], 1.25; 95% confidence interval [CI], 1.19, 1.31) strength training (OR, 3.48; 95% CI, 3.30, 3.67) and birthdate after 1980 (OR, 4.86; 95% CI, 4.29, 5.50) were associated with increased odds of using bodybuilding supplements in male respondents. A smaller survey study of 329 active duty Marines deployed to Afghanistan found that 42% of female and 72% of male respondents reported supplement use while in the combat zone (7). In that study, 75% of supplement users reported use of stimulant-containing products. Though less is known about supplement use in veterans, it is likely that former service members restart or continue supplement use after separation from the military. A retrospective, longitudinal cohort analysis of Veterans Health Administration (VHA) records (n=496,722) revealed that 75% of treatment-seeking OEF/OIF veterans in VHA care are overweight and obese, and those with PTSD and depression were in the highest risk categories for obesity compared to those without these conditions (8). Nutritional supplement manufacturers heavily market their products for weight loss, and former military personnel who used supplements during deployment may seek out these products after military service to lose weight.
In addition to unprescribed supplements, prescribed psychostimulants are also used in military settings to enhance performance and alertness, most commonly to combat fatigue in air force pilots (9). A DoD survey of 28,546 military personnel reported an estimated past-year prevalence of prescription stimulant misuse of 2.3% (10). An anonymous survey of 498 active duty military found that self-reported psychostimulant misuse in the past 5 years was 5%, and was associated with mental health conditions, deployment-related injuries, and new physical injuries (11).
Stimulant Use: A Risk Factor for PTSD?
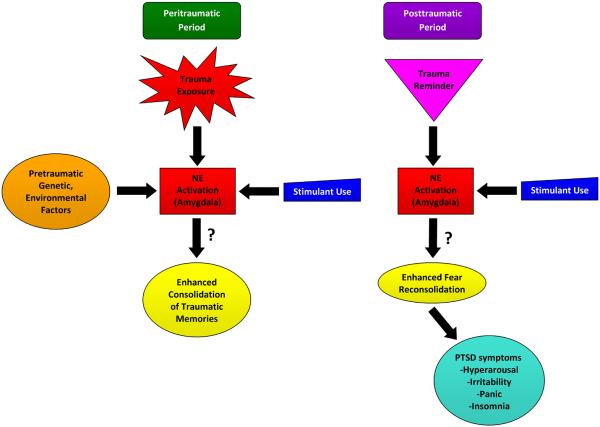
In spite of the widespread use of stimulant-based supplements, little is known about the behavioral effects of chronic use of these products or whether they induce or exacerbate psychiatric symptoms. Stimulants in performance-enhancing supplements include amphetamines, caffeine, ephedrine, pseudoephedrine, and phenylephrine(12). Common behavioral effects of stimulants include increased alertness and wakefulness, anxiety, irritability, restlessness, mood swings, and psychosis(13). At the time of a traumatic event, a cascade of noradrenergic signaling occurs in the brain, promoting the consolidation of fear-based memories in the amygdala (Figure 2). Central nervous system stimulants, such as DMAA, trigger the release of dopamine, serotonin and norepinephrine(14). If an individual is using stimulants at the time of a traumatic event, this may contribute to excessive noradrenergic activity during trauma, enhancing the encoding of the traumatic memory and subsequently leading to exaggerated fear responses (e.g., heightened arousal). Noradrenergic overactivation of the amygdala from stimulant use and enhancement of trauma-related memory consolidation may thus predispose trauma-exposed individuals to subsequent PTSD symptoms and may exacerbate PTSD symptoms in those already diagnosed with PTSD(15,16).
Figure 2.
Putative Conceptual Model of Stimulant-Induced PTSD Symptoms.
NE = Noradrenergic Activity
Question marks identify potential, unconfirmed mechanisms.
It is unclear whether noradrenergic activation from stimulant use precipitates or worsens symptoms of PTSD. A recent analysis of medical and pharmacy records in active duty military found a strong relationship between receipt of a prescription stimulant and later PTSD diagnosis at follow up 2–4 years later (hazard ratio = 5.09, 95% CI, 3.05, 8.50) (17). The study's authors conclude that stimulant use may contribute to the pathogenesis of PTSD. Other preclinical data and a small (n=32) randomized controlled trial have found that psychostimulants may improve PTSD symptoms, possibly by enhancing learning, promoting a feeling of well-being, and targeting attention and concentration difficulties(14,18,19). Dopaminergic and serotonergic mechanisms may be implicated in the ameliorative effect of psychostimulants observed in these studies(14,19). It is likely that the relationship between stimulants and PTSD symptomatology may vary depending on timing, quantity, and duration of stimulant use during or after traumatic exposures as well as individual genetic and environmental factors(17). Importantly, the dose of stimulant is difficult to establish in unregulated supplement products, unlike that of prescribed psychostimulants in therapeutic doses. Many stimulant supplements have never been tested in humans and their safety has not yet been established(4,5). Some workout products, including “Jack-3D” used by this patient, contain caffeine and multiple other ingredients in addition to the amine stimulant. Prospective studies and larger randomized controlled trials are urgently needed to clarify the relationship between stimulant use and PTSD.
In the current case, the patient reported use of DMAA both during traumatic combat experiences in Iraq and over a year after his last deployment, when he presented for treatment. It is possible that stimulant use in the peritraumatic period made him vulnerable to develop PTSD symptoms, or that his PTSD symptoms worsened with the resumption of stimulant use after deployment. Off-label stimulant use from workout supplements may thus be a previously unknown risk factor for PTSD.
Conclusions
This case highlights the potential association between a stimulant-containing dietary supplement and PTSD symptom exacerbation in a college-age recently returned combat veteran. Noradrenergic overactivation in the amygdala and enhanced consolidation of traumatic memories may mediate the observed relationship between stimulant use and PTSD symptomatology. While severe adverse effects of DMAA and other stimulant nutritional products have been described, the impact of DMAA on psychiatric symptoms including PTSD has not been previously reported. This case highlights the importance of comprehensive assessment of dietary and herbal supplements in mental health settings. Given the popularity and continued availability of stimulant-containing nutritional supplements, providers should be aware of the potential behavioral effects of these products in addition to medical adverse effects. With increasing numbers of veterans seeking care in non-VA settings(20), mental health providers should be aware of the high prevalence of supplement use in this population. Screening for supplement use is especially important in high-risk groups, including young adults, athletes, high school and college students, military personnel, and veterans(6,7,12). Future studies are critical to elucidate whether stimulant use during or after traumatic events contributes to the pathogenesis of PTSD.
Supplementary Material
Acknowledgments
Dr. Ellen Herbst is currently funded by a UCSF Hellman Foundation Award. Dr. Kalapatapu is currently funded by K23DA034883.
This work has not been previously presented. This work was completed at the Student Veteran Health Program (SVHP), a Veterans Integration To Academic Leadership (VITAL) program, Mental Health Services, SFVAHCS and the Department of Psychiatry, UCSF.
Footnotes
Disclosures:Dr. McCaslin reports no competing interests.
References
- 1.Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Gusman FD, Charney DS, et al. The development of a Clinician-Administered PTSD Scale. J Trauma Stress. 1995;8(1):75–90. doi: 10.1007/BF02105408. [DOI] [PubMed] [Google Scholar]
- 2.Karnatovskaia LV, Leoni JC, Freeman ML. Cardiac arrest in a 21-year-old man after ingestion of 1,3-DMAA-containing workout supplement. Clin J Sport Med. 2015;25(1):e23–5. doi: 10.1097/JSM.0000000000000103. [DOI] [PubMed] [Google Scholar]
- 3.Q & A on DMAA in dietary supplements [Accessed December 22, 2015];US Food and DrugAdministration (FDA) website. http://www.fda.gov/Food/DietarySupplements/QADietarySupplements/ucm346576.htm.
- 4.Cohen PA, Travis JC, Venhuis BJ. A synthetic stimulant never tested in humans, 1,3-dimethylbutylamine (DMBA), is identified in multiple dietary supplements. Drug Test Anal. 2015;7(1):83–7. doi: 10.1002/dta.1735. [DOI] [PubMed] [Google Scholar]
- 5.Cohen PA, Bloszies C, Yee C, Gerona R. An amphetamine isomer whose efficacy and safety in humans has never been studied, β-methylphenylethylamine (BMPEA), is found in multiple dietary supplements. Drug Test Anal. 2015 doi: 10.1002/dta.1793. [DOI] [PubMed] [Google Scholar]
- 6.Jacobson IG, Horton JL, Smith B, Wells TS, Boyko EJ, Lieberman HR, et al. Bodybuilding, energy, and weight-loss supplements are associated with deployment and physical activity in U.S. military personnel. Ann Epidemiol. 2012;22(5):318–30. doi: 10.1016/j.annepidem.2012.02.017. [DOI] [PubMed] [Google Scholar]
- 7.Cassler NM, Sams R, Cripe PA, McGlynn AF, Perry AB, Banks BA. Patterns and perceptions of supplement use by U.S. Marines deployed to Afghanistan. Mil Med. 2013;178(6):659–64. doi: 10.7205/MILMED-D-12-00440. [DOI] [PubMed] [Google Scholar]
- 8.Maguen S, Madden E, Cohen B, Bertenthal D, Neylan T, Talbot L, et al. The relationship between body mass index and mental health among Iraq and Afghanistan veterans. J Gen Intern Med. 2013;28(Suppl 2):S563–70. doi: 10.1007/s11606-013-2374-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gore RK, Webb TS, Hermes ED. Fatigue and stimulant use in military fighter aircrew during combat operations. Aviat Space Environ Med. 2010;81(8):719–27. doi: 10.3357/asem.2755.2010. [DOI] [PubMed] [Google Scholar]
- 10.Jeffery DD, Babeu LA, Nelson LE, Kloc M, Klette K. Prescription drug misuse among U.S. active duty military personnel: a secondary analysis of the 2008 DoD survey of health related behaviors. Mil Med. 2013;178(2):180–95. doi: 10.7205/milmed-d-12-00192. [DOI] [PubMed] [Google Scholar]
- 11.Kennedy JN, Bebarta VS, Varney SM, Zarzabal LA, Ganem VJ. Prescription stimulant misuse in a military population. Mil Med. 2015;180(3 Suppl):191–4. doi: 10.7205/MILMED-D-14-00375. [DOI] [PubMed] [Google Scholar]
- 12.Momaya A, Fawal M, Estes R. Performance-enhancing substances in sports: a review of the literature. Sports Med. 2015;45(4):517–31. doi: 10.1007/s40279-015-0308-9. [DOI] [PubMed] [Google Scholar]
- 13.Kirkpatrick MG, Johanson CE, de Wit H. Personality and the acute subjective effects of d-amphetamine in humans. J Psychopharmacol. 2013;27(3):256–64. doi: 10.1177/0269881112472564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Toledano D, Gisquet-Verrier P. Only susceptible rats exposed to a model of PTSD exhibit reactivity to trauma-related cues and other symptoms: an effect abolished by a single amphetamine injection. Behav Brain Res. 2014;272:165–74. doi: 10.1016/j.bbr.2014.06.039. [DOI] [PubMed] [Google Scholar]
- 15.Dębiec J, Bush DE, LeDoux JE. Noradrenergic enhancement of reconsolidation in the amygdala impairs extinction of conditioned fear in rats--a possible mechanism for the persistence of traumatic memories in PTSD. Depress Anxiety. 2011;28(3):186–93. doi: 10.1002/da.20803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.O'Donnell T, Hegadoren KM, Coupland NC. Noradrenergic mechanisms in the pathophysiology of post-traumatic stress disorder. Neuropsychobiology. 2004;50(4):273–83. doi: 10.1159/000080952. [DOI] [PubMed] [Google Scholar]
- 17.Crum-Cianflone NF, Frasco MA, Armenta RF, Phillips CJ, Horton J, Ryan MA, et al. Prescription Stimulants and PTSD Among U. S. Military Service Members. J Trauma Stress. 2015;28(6):585–9. doi: 10.1002/jts.22052. [DOI] [PubMed] [Google Scholar]
- 18.McAllister TW, Zafonte R, Jain S, Flashman LA, George MS, Grant GA, et al. Randomized Placebo-Controlled Trial of Methylphenidate or Galantamine for Persistent Emotional and Cognitive Symptoms Associated with PTSD and/or Traumatic Brain Injury. Neuropsychopharmacology. 2015 doi: 10.1038/npp.2015.282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Aga-Mizrachi S, Cymerblit-Sabba A, Gurman O, Balan A, Shwam G, Deshe R, et al. Methylphenidate and desipramine combined treatment improves PTSD symptomatology in a rat model. Transl Psychiatry. 2014;4:e447. doi: 10.1038/tp.2014.82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Affairs DoV Expanded Access to Non-VA Care Through the Veterans Choice Program. Interim final rule. Fed Regist. 2015;80(230):74991–6. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.