Abstract
Non-communicable diseases (NCDs) are the leading causes of death worldwide, with higher rates of premature mortality in low- and middle-income countries (LMICs). This places a high economic burden on these countries, which usually have limited capacity to address this public health problem. We developed a guided self-assessment tool for describing national capacity for NCD prevention and control. The purpose of this tool was to assist countries in identifying key opportunities and gaps in NCD capacity. It was piloted in three countries between 2012 and 2013: Mozambique, Colombia, and the Dominican Republic. The tool includes details about NCD burden; health system infrastructure and primary care services; workforce capacity; surveillance; planning, policy, and program management; and partnerships. In the three pilot countries, the tool helped to identify differences in capacity needs pertaining to staff, training, and surveillance, but similarities were also found related to NCD challenges and opportunities. The NCD tool increased our understanding of needs and critical capacity elements for addressing NCDs in the three pilot countries. This tool can be used by other LMICs to map their efforts toward addressing NCD goals and defining priorities.
Keywords: non-communicable diseases, capacity assessment, global health
Introduction
In 2012, there were 38 million deaths worldwide (68% of all deaths) due to non-communicable diseases (NCDs), which include cardiovascular disease, cancer, diabetes, and chronic respiratory diseases (1). Approximately 40% of NCD deaths occurred prematurely (i.e. before the age of 70); thus, during the most productive years of life. Almost 80% of the global NCD mortality occurred in low- and middle-income countries (LMICs) where resources and capacity are scarce (1). The Global Burden of Disease study showed an increase of approximately 8 million more deaths due to NCDs between 1990 and 2010, equivalent to a 30% change, or two out of every three deaths worldwide in 2010 (2). The main causes of NCDs are preventable and include behavioral (poor diet and physical activity, tobacco use, excessive alcohol consumption) and biologic (overweight and obesity, hypertension, raised blood lipids and glucose) risk factors (3). The consequences of NCDs place a large burden on governments, health systems, and individuals, especially in resource-constrained countries. According to a report by the world economic forum (4), by the year 2030, NCDs will cost approximately US$30 trillion globally, which represents almost 75% of the global gross domestic product (GDP) in 2010.
In September 2011, the United Nations (UN) held a High-Level Meeting on NCDs (5), which brought together leaders from around the world to highlight NCDs in the global development agenda and adopted a resolution that calls for international collaboration, including the need to build capacity for NCDs, especially in LMICs (6). With the UN declaration and the strong political momentum, the World Health Organization (WHO) developed the 2012 Global Action Plan for the prevention and control of NCDs (7), which includes indicators and voluntary targets that focus on achieving a global goal of a 25% reduction in premature mortality from NCDs by 2025 (also known as the 25x25 target) (8). Two of the six WHO objectives of this framework are related directly to strengthening national capacity for the management and control of NCDs. Due to the recent NCD global response, the US Centers for Disease Control and Prevention’s (CDC) global technical assistance expanded to target NCDs specifically in LMICs, with a focus on increasing epidemiologic and surveillance capacity and strengthening healthcare systems.
Assessing and building global NCD capacity, especially in LMICs, has been challenging (9,10). Capacity may be defined as an ability to perform (11), financial, economic, or political capacity (12), knowledge or technical ability (12), and even institutional or organizational capacity (13). Efforts to measure capacity have been documented within a series of tools and measures, particularly at the system level (14). Some capacity surveys and evaluations have been performed with different sets of indicators and objectives, such as the WHO global survey to assess country capacity for NCDs (15), as well as some regional surveys in Asia (16) and the Pacific Islands (17). In addition, a capacity survey for NCD surveillance for the Americas was conducted by the Pan-American Health Organization (PAHO) (18), and at the local/state level the Sustainability Tools for Assessing and Rating (STAR) Communities survey in the US was conducted by the National Association of Chronic Disease Directors (NACCD) (19). These assessments have been helpful for planning and implementation purposes, strengthening ongoing efforts, and increasing collaboration (16). However, it is important to acknowledge that health capacity challenges are not straightforward, especially in LMICs where there is a large degree of heterogeneity. Strengthening capacity for NCDs in LMICs requires understanding of the complex financial, infrastructure, human, and institutional conditions in a country (20). Additionally, the burden and causes of NCDs vary among LMICs (21).
With the WHO 25x25 target framework and CDC’s global NCD focus, we developed an assessment tool (NCD tool) to present a comprehensive and objective evaluation of a country’s capacity in the following areas: health system infrastructure; primary care services; workforce capacity; surveillance; planning, policy, and program management; and partnerships. In this paper we describe the rationale, methodology, and pilot testing of this NCD capacity assessment tool in three countries: Mozambique, Colombia, and the Dominican Republic.
Methods
Tool development
The NCD tool was developed to help respond to technical assistance requests, and was intended to be a guided self-assessment, facilitating the process of consultation between the CDC and in-country public health stakeholders. The NCD tool is designed to exchange the most current information available regarding the country’s NCD capacity with the CDC and other partners. These data can be used by each country to identify gaps and strengths in areas such as training for NCDs, surveillance, planning, program management, policies, and partnerships.
The specific objectives of the tool are to: (i) build a comprehensive profile to better understand current national capacity for NCD prevention and control; (ii) assist the country to identify key opportunities, priorities, and gaps in capacity; and (iii) strengthen the technical assistance process and collaborations between the CDC, the country’s Ministry of Health (MOH), and additional partners.
In order to develop the NCD tool, a literature review was conducted in August 2011 to identify scientific papers, reports, and expert opinion for assessing health system capacity in NCDs. Subsequently, the NCD tool was developed based on this review and the WHO NCD monitoring framework (22). The development of the tool was an iterative process and included feedback from in-country interviewees to enhance ease of administration, increase relevance, and reduce respondent burden.
Topics covered by the tool
The framework for the NCD tool included the following sections: (i) Demographics and NCD burden; (ii) Health system infrastructure and primary care services; (iii) Workforce capacity building; (iv) Surveillance and health information; (v) Planning, policy, and program management; and (vi) Partnerships.
The NCD tool covered the public health system and primary care services by including questions about the type of healthcare system, the organization of NCD control departments in the country, and specific budget and resource allocation for NCDs. In terms of data available, the tool addressed questions related to vital statistics and civil registration, surveillance systems in place related to NCDs and its risk factors, and how the data are processed and managed. In terms of workforce, the tool helped us to assess the availability of trained individuals working with NCDs and the availability of training mechanisms and links with other academic institutions for training MOH staff (e.g. Field Epidemiology Training Program) (23). For planning policy and programs, the tool includes questions regarding a national NCD strategic plan, which topic areas the plan covers (e.g. diabetes, cancer, cardiovascular disease, and chronic pulmonary disease), and the risk factors associated with each topic area. The tool also includes questions on the availability of national guidelines for the prevention and treatment of NCDs, as well as the availability of prevention programs and policies for tobacco, alcohol control, hypertension, nutrition, physical activity, and road traffic injury. Finally, the tool allowed us to evaluate the cross-collaboration and formal partnerships the MOH might have with other stakeholders, such as Non-Governmental Organizations (NGOs), academia, the private sector, and multilateral and regional partnerships.
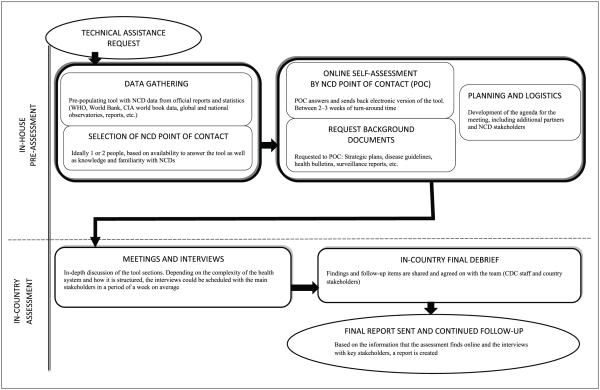
The NCD tool can be completed by more than one person or organization because it covers several areas. The tool consists of two parts (Figure 1). The first part is the in-house pre-assessment, which consists of local data review and preparation, and the identification of NCD-specific points of contact in relevant public and private organizations. The tool is completed several weeks in advance of a technical assistance field visit, enabling local staff to get acquainted with the topics covered in the tool and to schedule time for meetings with appropriate subject matter experts to discuss topics covered in the tool.
Figure 1.
Non-communicable disease capacity assessment tool process.
The second part is the in-country assessment, which consists of a series of face-to-face meetings between the technical assistance team and in-country partners, as well as a final debrief and report sent out to the country with specific follow-up activities for CDC staff and/or country stakeholders. By including objective assessments (surveillance data and reports) and more qualitative data (face-to-face interviews and briefings), the tool provides a comprehensive perspective on how NCD prevention and control is structured in the country.
Implementation and dissemination
The information for the first part of the NCD tool was obtained through literature searches from web documents and online databases (e.g. WHO Global Infobase, CIA World Factbook, or surveillance reports posted online, including International Cancer Registries, Global Tobacco Surveys, and Demographic Health Surveys). For the second part of the tool, the country point of contact verified the accuracy and relevance of the data and additional information was obtained during face-to-face interviews. In 2012, the Global Health Promotion Office in the National Center for Chronic Disease Prevention and Health Promotion piloted the tool to prepare for providing technical assistance in Mozambique, Colombia, and the Dominican Republic. These three countries were selected for the pilot based on ongoing collaboration between CDC and the country; a specific request for technical assistance; willingness from the country to collaborate; and geographic diversity (Africa, South America, and the Caribbean). The tool was translated into Spanish and Portuguese where necessary, and interviews in Colombia and the Dominican Republic were conducted in Spanish by native speakers. The interview in Mozambique was conducted in both English and Portuguese.
After receiving the self-guided portion of the NCD tool from the point of contact in each country, interviews with key informants were held between March and September 2012. These key informants were identified and selected prior to the field visit by the local point of contact from the MOH’s NCD unit or equivalent office. Additionally, we met with other important NCD stakeholders in each country, ranging from the Ministry of Education, Ministry of Sports (or equivalent), Institute of Public Health, NGOs (e.g. Diabetes Association in Mozambique and Population Services International (PSI) in Dominican Republic), international agencies (e.g. Pan-American Health Organization in the Dominican Republic), hospitals, foundations, academic institutions, and independent researchers. This tool was developed to be used by other researchers and practitioners in order to further evaluate capacity in LMIC countries and aid the process of providing NCD technical assistance. The tool can be downloaded from the Emory Global Diabetes Research Center (EGDRC) website, a unit within the Rollins School of Public Health, Hubert Department of Global Health, at Emory University.i
Results
NCD assessment tool pilots
Table 1 provides a summary of some of the information that was obtained through the NCD tool. The results for the assessments showed that even though these three countries are very different in terms of geography, population, culture, and readiness to address NCDs, they also shared many similarities related to the challenges and opportunities associated with NCDs in LMICs. The time it took for part 1 (in-house self-guided assessment) was approximately one month, including the collection of data, identifying the point of contact(s), having the online tool answered, and collecting background documents. For the second part, the face-to-face interviews, meetings with different stakeholders, and the final in-country debrief, 3–4 days were required (Colombia and the Dominican Republic: 4 meeting days; Mozambique: 3 meeting days) and the final report to the country was sent one month later.
Table 1.
Summary of results from piloting of the NCD assessment tool in Colombia, the Dominican Republic, and Mozambique.
| Area | Indicator | Colombia | Dominican Republic | Mozambique |
|---|---|---|---|---|
|
NCD
governance and health system infrastructure |
NCD unit or department Coverage of health services |
NCD sub-directorate nested in the MOH working with National Institute of Public Health (INS) 98% coverage: 53% in the subsidized regime, 40% in the contributive, the rest (2.3%) affiliated to the military, Ecopetrol, or police. 4.4% are not affiliated (2010) |
NCD program nested in the MOH created in 2010 52% coverage (2012) through the Plan Basico de Salud. Contributive 53.7% and subsidized 45.7% |
NCD Unit (DDNT) within the MOH (created in 2002) working mostly with academic partners 60% coverage of public services. Mostly public sector |
| Provision of health services |
Health sector is structured through 'Promoting Health Entities' (Entidades Promotoras de Salud) which offer services through health insurance plans according to the 'Mandatory Health Plan' |
Divided into three levels of care: primary (health clinics), secondary (provincial hospitals), and tertiary (reference hospitals) |
Structured in four levels: primary healthcare clinics and health posts, district-level hospitals, provincial-level hospitals, and central-level hospitals |
|
| Surveillance | Surveillance system in place for NCDs |
Complex system that integrates information from various databases: the Unique Registry for Social Security (RUAF) and the Individual Registry for health care services (RIPS) (information provided by insurance companies). Additionally, the National Statistics Department (DANE) compiles the information and analyzes it along with the National Institute of Public Health |
There is no formal surveillance system in place, most information obtained by independent surveys |
The Department of Health Information is in charge of collecting morbidity data |
| Specific NCD information available |
Mortality information for Cardiovascular disease (CVD), Cancer, Diabetes, Chronic Obstructive Pulmonary Disease (COPD), and injury is gathered and available at a local, department (state), and national level. There are population cancer registries done by some universities and financed by the MOH through the National Cancer Institute |
The mortality data for NCDs available is for cardiovascular disease, cancer, diabetes, COPD, and injury (all at a hospital level). Some information from specific point-in- time surveys. Cancer and renal chronic disease morbidity data are available from the primary level of care |
Hospital-based cancer registry since 1992 (three major hospitals). One population-based registry in one city. Surveillance for injury - hospital based |
|
| Risk factor surveys |
2007 National Health Survey: blood pressure, tobacco, diabetes, hyperglycemia, and cholesterol. Periodicity: every five years. 2005 and 2010 National Nutrition Survey (Encuesta Nacional de la situación nutricional (ENSIN)): 2010 version includes anthropometry, biochemical indicators, food security, food frequency, physical activity, TV viewing time, and perception of body image. Additionally, there is the Tobacco and Alcohol Survey (ENTAB) based on the Global Youth Tobacco Survey (GYTS) every four years available in some cities |
2007 National Demographic and Health Survey (ENDESA): tobacco, alcohol, breastfeeding, self-reported diabetes, hypertension, cancer, and cardiovascular disease. 2003 World health survey Dominican Republic: tobacco, alcohol, intake of fruit and vegetables, and physical activity. 1998 and 2008 Risk Factors for cardiovascular and metabolic syndrome in the Dominican Republic (EFRICARD) I/II: CVD, hypertension, overweight and obesity, glucose and lipid profile |
2005 WHO STEPwise approach to Surveillance (STEPS) survey: obesity, tobacco and alcohol consumption, diabetes, hypertension, and CVD |
|
|
Workforce
capacity |
NCD workforce capacity |
MOH: 35 staff members (four permanent positions). INS: 16 staff members (three permanent positions). Coldeportes: three staff members. the Field Epidemiology Training Program (FETP) NCD courses (basic, short and basic plus) have been adapted and piloted in several locations, one FETP in the MOH working on NCDs and 11 at the INS |
National Program for Chronic Diseases (PRONCEC) in the Dominican Republic has three staff members. The head of NCD program is an FETP graduate. FETP is strong in the country with a strong infectious disease focus |
DDNT works with three people. Additionally, two FETPs working on cancer and injury projects. FETP is strong for infectious diseases. NCD basic course was taught on 2012 to the NCD local coordinators for the 11 regions in the country |
|
Partnerships
and collaboration |
There is extensive collaboration between MOH, INS, and Coldeportes. Additional collaboration for specific projects with the Ministry of education, the National Institute for Food Surveillance and Safety (INVIMA), and several universities and research institutions. The NGO side is relatively weak for NCDs, even though some organizations do some work |
Some formal agreements with the Nutrition Institute for Central America and Panama (INCAP), the Autonomous University of Santo Domingo and University of Puerto Rico. Partnerships with NGOs are mostly for infectious diseases, but PSI is interested in engaging in diabetes, nutrition and physical activity work |
Some links with the department of transportation for injury prevention. Also there are linkages with maternal and child health in tobacco and alcohol areas. NGOs focus is mainly EBV and infectious diseases |
|
|
NCD policy
and guidelines |
National NCD policy |
Framework document for the management of NCDs is under development |
NCD strategic plan 2009-2016 | 2008-2014 strategic plan for NCD prevention and control |
| National guidelines |
Cancer treatment and comprehensive care guidelines. CVD guidelines (includes acute myocardial infarction and hypertension). Diabetes treatment guidelines (under review at the moment). Physical activity guidelines (technical document from Coldeportes) |
PAHO NCD and risk factor guidelines are used for the country. Available cancer and hypertension guidelines focus on treatment and management |
Hypertension, diabetes, and cancer guidelines exist in the country |
NCD burden
The data obtained by the tool revealed that even when the burden of communicable diseases (notably HIV, malaria, and tuberculosis) remains high, NCDs already account for a significant percentage of mortality (cardiovascular disease, stroke, cancer, diabetes,and injury) in these LMICs.In Mozambique, chronic conditions are rising rapidly; for example, in 2004, NCDs accounted for 26% of all deaths reported, but more recent estimates indicate that mortality for NCDs is now as high as 40%. At the time of the assessment, in the Dominican Republic and Colombia, the deaths attributable to NCDs were 68% and 66%, respectively.
Health system infrastructure
Piloting in these three countries revealed that even though there are differences in terms of the complexity of the organization, they all had a dedicated department for NCDs housed in the MOH. The NCD department in each country had different capacities. For example, Mozambique’s MOH has a small NCD unit with limited staff (one NCD director) created in 2002, whereas the Dominican Republic has a medium-sized NCD program sitting under the vice MOH National Program for Prevention of Chronic Diseases (PRONECEC), with three staff hired since 2010. In contrast, Colombia has a more comprehensive and complex structure with many partners and stakeholders working on NCDs, ranging from the National Institute of Public Health (INS), the Sub-directorate of NCDs in the MOH, the Ministry of Sports (Coldeportes), several academic, scientific, and medical societies and research institutions, and think tanks. As for the provision and coverage of healthcare services, Mozambique has a predominantly public sector, and the healthcare system is structured in four levels: 1) primary healthcare clinics and health posts; 2) district level hospitals; 3) provincial level hospitals; and 4) central level hospitals (three main central hospitals in the country). The Dominican Republic’s NCD unit (PRONECEC) works in coordination with the regional health services, which are divided into three levels of care: primary (health clinics), secondary (provincial hospitals – about 1700 in the country), and tertiary (reference hospitals). Health services coverage is both public and private, having a mix of subsidized and private insurance regimes for healthcare services. In Colombia, healthcare services are provided by 69 entities that act as health insurers, and can be public or private and provide services offered by the mandatory national health plan.
Workforce capacity
The tool helped identify some strengths and weaknesses within the MOH related to training and capacity building for NCDs. The workforce performance reported is good and in most cases there are sufficient trainings and opportunities for professional growth. However, most of the staff are contractors, which makes it hard to strengthen some work groups and ensure the continuity of NCD activities and programs. The disciplines working within the NCD units varied greatly and we found very different professional profiles including: public health, medicine, biostatistics, epidemiology, psychology, nutrition, nursing, pedagogy, economy, political sciences, demography, administration, and communication, with some staff having graduate degrees such as an Master in Public Health (MPH) and very few with doctoral degrees or above. In summary, NCD workforce was identified as a challenge, in part, because of the limited number of staff within the MOH to address NCDs and lack of stability for employees; many staff are temporary contractors with few full-time employees, resulting in high staff turnover.
Surveillance
NCD surveillance, prevention, and control activities are being implemented with some success but we found through the interviews that this area is quite limited by funding. In terms of NCD surveillance, the results show that data are available for most of the NCDs and risk factors; however, some of the data are either not collected periodically or recently, or results are not publicly available. For example, in Colombia data for NCDs and risk factors are collected periodically through two national surveys (National Nutrition Survey (ENSIN) and National Health Survey (ENS). The Dominican Republic and Mozambique have performed surveys that include risk factors like obesity, tobacco consumption, or alcohol use. Additionally, Mozambique has a population cancer registry in the city of Beira along with an injury hospital registry in Maputo – the capital’s central hospital. For each country, there was a consistent lack of funding and clear needs for training in surveillance, program management, and evaluation.
Discussion
Overall, the use of the NCD tool provides a profile of the readiness of each piloted country to address NCDs. Specifically, the NCD tool helped us to understand in greater depth the NCD burden and data availability, health system capacity, human and financial resources, deployment of interventions, policy development and implementation, and main NCD players in each of the countries. The profile created by the tool was used to assist the countries to identify needs, opportunities, and priorities, while strengthening capacity-building efforts between the CDC, MOHs, and regional partners. NCDs have a very broad spectrum, and gaps and strengths in one country or region might not translate to others. The structured approach for assessing NCD capacity across several domains seems to aid in identifying and prioritizing different areas for capacity building and follow-up.
Piloting the tool increased awareness of cross-collaboration within the MOH, the CDC and of other key partners working on NCDs in the country. Incorporating multi-sectoral approaches has helped to build capacity and build on existing infrastructure (24). The MOH recognized that there was a lot of overlap in efforts to address NCDs; however, cross-collaboration and communication could improve the NCD work done in each country. The NCD tool can help to increase and foster relationships inside and outside the government and throughout topic areas. The overall process can also help stakeholders to think about topic areas and partners not previously considered in the NCD arena, such as a collaboration between NCDs and communicable diseases, especially in lower income countries which are still struggling with diseases such as HIV, Tuberculosis, or Malaria but are also affected with NCDs (25,26). The process also helped to plan ahead for gaps in capacity, as some of the countries didn’t have a complete overview of NCD national capacity.
The findings also reveal that capacity for NCDs is still in its early stages, especially in Mozambique and the Dominican Republic where infectious diseases like HIV comprise a significant portion of the health agenda. However, we found through the interviews that after the UN NCD summit (5) and with the WHO 25×25 framework (7), government leaders have been paying more attention to NCDs and trying to increase resource allocation for NCDs. It is important to note that the assessments took place in 2012 and some things have changed since then; after the pilot assessment in Mozambique took place in 2012, the NCD unit moved to the Mozambique National Public Health Institute in 2014 and has increased in size to include the NCD director and three public health staff. The NCD tool facilitated the identification of financial resources as a barrier for all the countries assessed, coinciding with previous research done on NCD capacity (27). For example, a common barrier identified for surveillance and data collection by the three pilot countries is the need for external funders (e.g. CDC and WHO) to provide financial resources and training. Financial resources and political will were common constraints. This aligns with the traditional model of international aid (10) and underscores the importance of building sustainability into the technical assistance process.
Human resource capacity and lack of training were also identified as common challenges. Specifically, the availability of a trained and knowledgeable workforce to address NCDs has been a challenge; in many cases the internal processes make it hard to hire full-time health staff and, in turn, the MOH must depend on contractors or temporary staff. This issue, along with low wages and insufficient training, is one that many LMICs face (28); however, other stakeholders and institutes within the government, private sector, and non-profit sector may be able to partner and join forces with the NCD department to address NCDs and risk factors. We also learned through the interviews that while countries have identified priorities through a specific framework and strategic plan to address NCDs, there is still a gap between policy and implementation. NCD plans and frameworks exist, but often they are not executed due to financial constraints, lack of staff, or a lack of implementation capability. Additionally, and in-line with some reviews (29,30), it is important for the availability of data and high-quality scientific literature to come from the LMIC where the mortality burden is greatest. A mentoring system and partnering with neighbor countries could be viable solutions to address this gap. Additionally, as some authors have suggested (25,31,32), encouraging and investing in high-quality research and capacity building in LMICs can be translated into great examples of good practice, not only in LMICs but also in developed countries.
Surveillance for NCDs and its risk factors was at different development stages in all three countries, but remains a challenge in all three countries due to a lack of financial and human resources. The goal of ongoing periodic data collection is potentially burdensome and not yet a reality. This is of special concern as strong monitoring frameworks need to be in place to assess progress towards the WHO 25×25 targets and achieve the goal of a 25% reduction in premature mortality by 2025. Surveillance data could help direct and prioritize efforts, which, in turn, might enhance accountability for monitoring progress.
Some limitations of the tool were that it is not 100% comprehensive for all NCDs or all capacity areas, due to potential respondent burden. Additionally, while the in-house collection of data helped to gauge NCD burden, data available to outside stakeholders were typically not up to date and required updating during the interview.
Conclusion
The information gathered using the NCD tool facilitated understanding of how to address technical assistance needs for NCDs and the critical capacity elements for moving forward with NCD prevention in each of the three countries. The results from the tool can be used as a bi-directional way of communication between the CDC and other groups providing technical assistance and countries in identifying needs and opportunities and strengthening capacity-building efforts. The process of developing and piloting the NCD tool clearly demonstrated the value of an instrument for systematically measuring national NCD capacity. This tool has the potential to be used by other LMICs to guide and prioritize their efforts to address NCDs. Additionally, the process of measuring NCD capacity stimulated a productive discussion within the three pilot countries and increased awareness of neglected areas and non-traditional partners that might have not been contemplated in a traditional framework.
Acknowledgements
The authors wish to acknowledge the NCD Units within the Ministries of Health from Mozambique, Dominican Republic and Colombia for their assistance, support and collaboration in this assessment. Special thanks to Carla Silva Matos, Erick Seastedt, Fernando Ramirez, Franklyn Prieto and Maritza Gonzalez.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Footnotes
Declaration of conflicting interests
None declared.
Note
For review and dissemination purposes, the NCD tool is posted at the EGDRC within the Emory School of Public Health website: http://diabetes.emory.edu/capacity%20building/NCD%20Country%20Capacity%20Assessment%20Tools.html
References
- 1.World Health Organization (WHO) Report. World Health Organization; Geneva, Switzerland: 2014. Global Status Report on Noncommunicable Diseases. [Google Scholar]
- 2.Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. The Lancet. 2012;380:2095–2128. doi: 10.1016/S0140-6736(12)61728-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bauer UE, Briss PA, Goodman RA, Bowman BA. Prevention of chronic disease in the 21st century: elimination of the leading preventable causes of premature death and disability in the USA. The Lancet. 2014;384:45–52. doi: 10.1016/S0140-6736(14)60648-6. [DOI] [PubMed] [Google Scholar]
- 4.Bloom DE, Cafiero ET, Jané-Llopis E, Abrahams-Gessel S, Bloom LR, Fathima S, et al. The Global Economic Burden of Noncommunicable Diseases. World Economic Forum; Geneva: 2011. [Google Scholar]
- 5.United Nations . High Level Meeting on Prevention and Control of Non-Communicable Diseases. New York: 2011. 2011. Available from: http://www.un.org/en/ga/ncdmeeting2011/ (accessed March 16, 2015) [Google Scholar]
- 6.United Nations General Assembly . Political declaration of the High-level Meeting of the General Assembly on the Prevention and Control of Non-Communicable Diseases. New York: 2011. A/66/L.1. [Google Scholar]
- 7.World Health Organization . Global Action Plan for the Prevention and Control of Noncommunicable Diseases 2013–2020. World Health Organization; Geneva, Switzerland: 2013. [Google Scholar]
- 8.Beaglehole R, Bonita R, Ezzati M, Alleyne G, Dain K, Kishore SP, et al. NCD Countdown 2025: accountability for the 25 × 25 NCD mortality reduction target. The Lancet. 2014;384:105–107. doi: 10.1016/S0140-6736(14)61091-6. [DOI] [PubMed] [Google Scholar]
- 9.Mizrahi Y. Capacity Enhancement Indicators, Review of the Literature. World Bank Institute; Washington, DC: 2004. [Google Scholar]
- 10.Pratt M, Lamarre M-C. The new world of global health. Glob Health Promot. 2013;20:3–5. doi: 10.1177/1757975913513116. [DOI] [PubMed] [Google Scholar]
- 11.Milen A. An Overview of Existing Knowledge and Good Practice. World Health Organization; Geneva, Switzerland: 2001. What Do We Know About Capacity Building? [Google Scholar]
- 12.Imbeau L, Chenard K, Dudas A. The Conditions for a Sustainable Public Health System in Canada. Comission on the future of health care Canada. 2002 [Google Scholar]
- 13.White J. Three meanings of capacity; or, why the federal government is most likely to lead on insurance access issues. J Health Polit Policy Law. 2003;28:217–244. doi: 10.1215/03616878-28-2-3-217. [DOI] [PubMed] [Google Scholar]
- 14.LaFond AK, Brown L, Macintyre K. Mapping capacity in the health sector: a conceptual framework. Int J Health Plann Manage. 2002;17:3–22. doi: 10.1002/hpm.649. [DOI] [PubMed] [Google Scholar]
- 15.World Health Organization . Assessing National Capacity for the Prevention and Control of Noncommunicable Diseases. World Health Organization; Geneva, Switzerland: 2012. [Google Scholar]
- 16.Engelgau M, El-Saharty S, Kudesia P, Rajam V, Rosenhouse S, Okamoto K. Capitalizing on the DemographicTransition:Tackling Noncommunicable Diseases in South Asia. The World Bank; Washington, DC: 2011. [Google Scholar]
- 17.Aitaoto N, Ichiho HM. Assessing the health care system of services for non-communicable diseases in the US-affiliated Pacific Islands: a Pacific regional perspective. Hawaii J Med Public Health. 2013;72:106–114. [PMC free article] [PubMed] [Google Scholar]
- 18.Choi BC, Corber SJ, McQueen DV, Bonita R, Zevallos JC, Douglas KA, et al. Enhancing regional capacity in chronic disease surveillance in the Americas. Rev Panam Salud Publica. 2005;17:130–141. doi: 10.1590/s1020-49892005000200012. [DOI] [PubMed] [Google Scholar]
- 19.STAR State Technical Assistance and Review Program Guide for states. National Association of Chronic Disease Directors. 2008 Available from: http://c.ymcdn.com/sites/www.chronicdisease.org/resource/resmgr/services/star_guideforstates_january2.pdf (accessed March 15, 2015)
- 20.Ali MK, Rabadan-Diehl C, Flanigan J, Blanchard C, Narayan KM, Engelgau M. Systems and capacity to address noncommunicable diseases in low- and middle-income countries. Sci Transl Med. 2013;5:1–4. doi: 10.1126/scitranslmed.3005121. [DOI] [PubMed] [Google Scholar]
- 21.McQueen D, Pratt M, Blanchard C. Commentary on a meeting entitled ‘Building global capacity for non-communicable diseases (NCD) prevention: defining direction and roles’. Glob Health Promot. 2013;20:93–96. doi: 10.1177/1757975913509656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.World Health Organization . NCD Global Monitoring Framework. Geneva: 2013. Available from: http://www.who.int/nmh/global_monitoring_framework/en/ [Google Scholar]
- 23.Centers for Disease Control and Prevention . Field Epidemiology Training Program. Centers for Disease Control and Prevention; 2015. Available from: http://www.cdc.gov/globalhealth/healthprotection/fetp/index.htm (September 24, 2015) [Google Scholar]
- 24.Hospedales CJ, Jané-Llopis E. A multistakeholder platform to promote health and prevent noncommunicable diseases in the region of the Americas: the Pan American Health Organization partners forum for action. J Health Commun. 2011;16:191–200. doi: 10.1080/10810730.2011.601245. [DOI] [PubMed] [Google Scholar]
- 25.Jaacks LM, Ali MK, Bartlett J, Bloomfield GS, Checkley W, Gaziano TA, et al. Global noncommunicable disease research: opportunities and challenges. Ann Intern Med. 2015;163(9):712–714. doi: 10.7326/M15-1068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Oni T, Unwin N. Why the communicable/non-communicable disease dichotomy is problematic for public health control strategies: implications of multimorbidity for health systems in an era of health transition. Int Health. 2015;7(6):390–399. doi: 10.1093/inthealth/ihv040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.World Health Organization . Scaling up Actions Against Non-Communicable Diseases: How Much Will It Cost? World Health Organization; Geneva, Switzerland: 2011. [Google Scholar]
- 28.Vujicic M, Ohiri K, Sparkes S. Working in Health: Financing and Managing the Public Sector Health Workforce. The World Bank; Washington, DC: 2009. [Google Scholar]
- 29.Salvo D, Reis RS, Sarmiento OL, Pratt M. Overcoming the challenges of conducting physical activity and built environment research in Latin America: IPEN Latin America. Prev Med. 2014;69:S86–S92. doi: 10.1016/j.ypmed.2014.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pratt M, Sarmiento OL, Montes F, Ogilvie D, Marcus BH, Perez LG, et al. The implications of megatrends in information and communication technology and transportation for changes in global physical activity. The Lancet. 380:282–293. doi: 10.1016/S0140-6736(12)60736-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Syed S, Dadwal V, Martin G. Reverse innovation in global health systems: towards global innovation flow. Global Health. 2013;9:36. doi: 10.1186/1744-8603-9-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Syed S, Dadwal V, Rutter P, Storr J, Hightower J, Gooden R, et al. Developed-developing country partnerships: benefits to developed countries? Glob Heal. 2012;8:17. doi: 10.1186/1744-8603-8-17. [DOI] [PMC free article] [PubMed] [Google Scholar]