Abstract
Background
It is difficult to evaluate the effectiveness of interventions aimed at reducing early childhood obesity using randomized trials.
Objective
To illustrate how observational data can be analyzed using causal inference methods to estimate the potential impact of behavioral “interventions” on early childhood adiposity.
Methods
We used longitudinal data from 1054 children 1–5 years old enrolled in the Special Supplemental Nutrition Program for Women, Infants and Children (WIC) and followed from 2008 to 2010 for a mean duration of 23 months. The data came from a random sample of WIC families living in Los Angeles County in 2008. We used the parametric g-formula to estimate the impact of various hypothetical behavioral interventions.
Results
Adjusted mean weight-for-height Z score at the end of follow-up was 0.73 (95% CI 0.65, 0.81) under no intervention, and 0.63 (95% CI 0.38, 0.87) for all interventions given jointly. Exclusive breastfeeding for six months or longer was the most effective intervention [population mean difference = −0.11 (95% CI −0.22, 0.01)]. Other interventions had little or no effect.
Conclusions
Compared with interventions promoting healthy eating and physical activity behaviors, breastfeeding was more effective in reducing obesity risk in children aged 1–5 years. When carefully applied, causal inference methods may offer viable alternatives to randomized trials in etiologic and evaluation research.
Keywords: childhood obesity, adiposity, interventions, g-formula, causal inference, breastfeeding
INTRODUCTION
Childhood obesity is a major public health problem affecting millions of young Americans.(1) In the United States, one in three children is obese or overweight.(1) While prevalence rates have begun to stabilize, they continue to be high and are consistently higher among African-Americans and Hispanics.(1) Children who are obese are likely to be obese as adults since excess weight tracks through the life-course, from early childhood to adulthood.(2) This puts children who are obese at higher risk of developing various non-communicable diseases later in life.(3)
When attempting to reduce childhood obesity rates, public health professionals and policy makers need to answer questions such as, “What would be the population impact of a particular health intervention on childhood obesity if every child was exposed to it [e.g. if every child stopped consuming sugar-sweetened beverages (SSB)]?” and “Which interventions or combinations of interventions would yield the greatest long-term impact on childhood obesity?” While a number of prospective observational studies have identified potential protective (e.g. exclusive breastfeeding) and harmful (e.g. SBB consumption) risk factors for childhood obesity, (4) randomized trials (RCTs) have offered limited evidence about the long-term impact of reducing harmful exposures and increasing beneficial exposures either singly or in combination with each other.(5) In addition, results from RCTs are not always generalizable to the population that would be receiving the interventions, partly because of the selective enrollment of participants into the trials.(6) Further, for practical reasons including cost and loss to follow-up, RCTs are rarely able to follow participants for the long term.
One approach to addressing these methodological limitations is to apply causal inference methods to existing observational data to quantify the potential impact of hypothetical interventions under plausible assumptions. This approach has been used by Taubman et al. and Danei et al. in their assessments of the impact of hypothetical interventions aimed at reducing risk factors for coronary heart diseases (7) and diabetes in adult populations,(8) respectively.
Hence, the goal of this study was to illustrate the usefulness of modern causal inference methods for evaluating interventions and providing relevant information for policy decision-making. The specific objective was to quantify the potential impact of various hypothetical and plausible behavioral interventions early in life on adiposity in a multi-ethnic cohort of children aged 1–5 years living in low-income households enrolled in the Special Supplemental Nutrition Program for Women, Infants and Children (WIC) in Los Angeles County.
METHODS
Study population and sources of data
WIC provides food assistance and nutrition education to pregnant and postpartum women and children up to age five living in low-income households in the United States. In Los Angeles County, Public Health Foundation Enterprises WIC, the largest local agency WIC program in the country, maintains an administrative dataset which contains socio-demographic and anthropometric data on every child enrolled in WIC in Los Angeles County since 2003.(9) WIC staff use a standardized protocol to measure height and weight; these measurements have been shown to have high accuracy.(10) In addition, a survey of a random sample of about 5,000 WIC families living in Los Angeles County is conducted every three years to collect behavioral data so as to address the specific needs of communities living in poverty. This WIC survey is conducted in English or Spanish through a computer-assisted telephone interviewing system. Almost half of the eligible WIC participants could not be reached by phone after many attempts (up to 16), giving a response rate of 51%. We linked survey data obtained between April 8 and July 22, 2008 to WIC administrative data to prospectively follow a cohort of 1,054 children aged 1–5 years living in low-income households in Los Angeles County from 2008 to 2010. To ensure that the anthropometric measurements were obtained at a time relevant to the survey period and more specifically at an age when it was developmentally plausible for the child to engage in a specific behavior of interest (e.g. consume fast food or be physically active at the playground), we included in the sample only children who: (i) were at least 12 months old at the time of the first relevant anthropometric measurement, (ii) had three subsequent measurements, and (iii) had a baseline (first) measurement that was taken within six months of the survey. Further excluded from the sample were children with a time interval between measurements of less than three months (n = 1) (eFigure 1 and 2 in the appendix).
The protocol for de-identifying the WIC data for research use was approved by the Ethical and Independent Review Services’ Institutional Review Board. The University of California, Los Angeles (UCLA) Institutional Review Board approved the overall study protocol.
Study variables
Weight-for-height Z score (WHZ)
The outcome variable of interest was child’s weight-for-height Z score (WHZ) calculated from height and weight measurements obtained by trained WIC staff during recertification visits. WHZ is a commonly used indicator for assessing adiposity in growing children as it is independent of height.(11) WHZ was estimated from age- and gender-specific CDC growth reference values.(12) All children in the sample had three WHZ estimates obtained from heights and weights which were mostly measured between 2008 and 2010. The third WHZ (i.e. WHZ3) was the outcome variable of interest while the second WHZ (i.e. WHZ2) was considered an intermediary or mediating variable. We excluded records of children with improbable WHZ (<−4 or >5) (n= 3) as suggested by CDC (eFigure 1 in appendix).
Risk factors and hypothetical interventions
The survey collected data on a number of obesity-related risk factors including duration of exclusive breastfeeding, television watching, fruit and vegetable consumption, playing at the playground every day, SSB consumption, and fast-food consumption (see eTable 1 in appendix for survey questions). Risk factor variables were categorized to avoid sparse data issues and/or to highlight recommended levels. Hypothetical interventions were designed on the basis of these risk factors by asking the question, “What would the population mean WHZ be if every child was exposed to the most beneficial level of a particular risk factor?” In other words, this study aimed to predict the mean WHZ of a population of children exhibiting optimal (recommended or desirable) levels of the behaviors of interest. For example, in the present sample, 23% of the children were exclusively breastfed at the recommended level of six months or more (i.e. at the desirable level), while the remaining 77% were breastfed for lesser amounts of time or not at all (i.e. less desirable levels). This study aimed to predict the population mean WHZ when 100% of the population exclusively breastfeeds for six months or more, that is, the 77% of children who were initially exclusively breastfed less than six months would now be exclusively breastfed for six months or more. The following interventions were similarly evaluated: watching television for no more than one hour/day; eating at least five fruits and vegetables a day; playing at the playground every day; eliminating SSB consumption; and eliminating fast-food consumption. We selected the desired levels of behaviors based on (i) national and international recommendations (e.g. from World Health Organization, American Academy of Pediatrics) regarding optimal child growth, (ii) plausible anticipated risk reduction documented in published literature, and (iii) available response categories used in the survey. A detailed description of the recommendations is available in the appendix (eTable 2).
Covariates
We used a directed acyclic graph(13) to depict the hypothesized data-generating mechanism and causal structure of the processes under study (see appendix eFigure 2). In our first analytic model, we adjusted for child’s baseline WHZ, and sociodemographic variables, namely, age at first relevant measurement, gender, race/ethnicity, birth weight, maternal language preference, maternal education, family size, family monthly income, maternal age and follow-up period (n=799). In Model 2, we further adjusted for maternal Body Mass Index (BMI), a potential confounder of the relationship between certain risk factors such as breastfeeding duration and childhood adiposity.(14) This analysis involved a smaller sample (n= 553) which excluded records with missing or improbable maternal BMI (BMI< 14 or BMI > 48). See eFigure 1 in the appendix for a flow diagram showing sample sizes at various stages of participant inclusion.
Statistical analyses
We used the g-computation algorithm (applied to the parametric g-formula), a generalization of the standardization method for time-varying exposures and confounders,(15) to predict the potential mean WHZ under various hypothetical scenarios. We first fit linear regression models of the outcome WHZ3 and mediator WHZ2 on behavioral risk factors adjusting for the selected covariates. We then used the regression coefficients obtained from these models to predict the potential outcomes and mediators under the different hypothetical interventions. We obtained the marginal mean differences (i.e. intervention impact) by taking the difference between the predicted potential mean WHZ under the various scenarios (in which the exposure distributions were altered so that 100% of the population would be exposed to the desired level of the risk factor) and the WHZ under no intervention (i.e. status quo) (in which the exposure distributions remained the same as in the original sample). Standard errors and 95% confidence intervals were obtained via bootstrapping. These steps are also described in the literature.(7,8) Analyses were conducted in SAS version 9.4 (SAS Institute, Inc., Cary, NC). It was assumed that there was: (i) no uncontrolled confounding after adjusting for the selected covariates, (ii) positivity, (iii) consistency, and (iv) no other source of bias.
We conducted sensitivity analyses to assess the robustness of our findings (1) under different sample restriction scenarios, and (2) when missing values and extreme values of WHZ and maternal BMI were imputed (see appendix eTables 5–9 and eFigures 4–7).
RESULTS
Among the 1,054 children aged 1–5 years who had three measurements, 799 (76%) had complete data on all variables except maternal BMI and were included in the first analytic sample for the main analysis. Due to missing maternal values, analyses including maternal BMI as a covariate were conducted on the reduced analytic sample (n = 553 or 52% of the eligible sample) (appendix eFigure 1). Table 1 shows characteristics of the 799 children included in our main analysis. These children had a mean (SD) age of 23 (7) monthsat baseline; 65% were Hispanic. The median monthly family income was $1,545. Cohort members were followed, on average, for 23 months.
Table 1.
Baseline characteristics of WIC participants in the analytic sample, in 2008 (N = 799)
| Baseline characteristics | Frequency (%) | Mean (SD) |
|---|---|---|
| Child’s age in months | 23 (7) | |
| Follow-up period in months | 23 (3) | |
| Interval between measurements | 11 (2) | |
| Family size | 4 (1) | |
| Child’s gender | ||
| Male | 398 (50) | |
| Female | 401 (50) | |
| Child’s ethnicity | ||
| White | 208 (26) | |
| Black | 24 (3) | |
| Hispanic | 519 (65) | |
| Asians and Others | 48 (6) | |
| Child’s birthweight in kg | 4 (1) | |
| Baseline WHZ | 0.80 (1.15) | |
| Maternal age | 30 (7) | |
| Maternal BMI in kg/m2 (n=553) | 28 (5) | |
| Family monthly income in $ US | 1545 (766) | |
| Family education | ||
| High school or higher | 282 (35) | |
| Less than high school | 517 (65) | |
| Family language preference | ||
| English | 220 (28) | |
| Spanish | 579 (72) |
SD: Standard deviation
At baseline, one in five children was exclusively breastfed for six months or more; one-third watched television one hour or less (0 to 1h) per day; and more than half of the children consumed five or more servings of fruits and vegetables per day. Only 10% played in parks and playgrounds every day; two-thirds reported not consuming SSB; and 15% reported never consuming fast food (eTable 3).
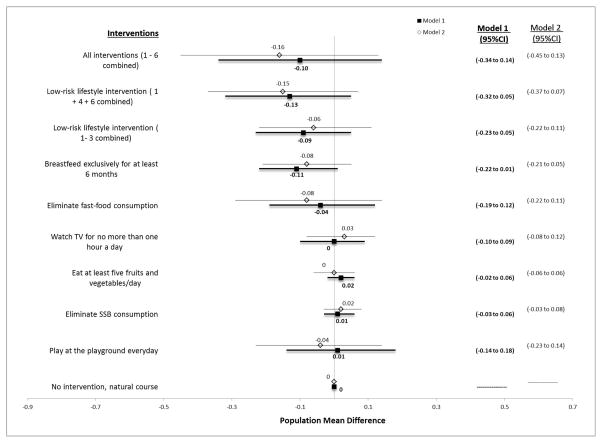
For most interventions considered in this study, we needed to expose more than three quarters of the population in order for the entire population to be exposed to the desirable level of the behavioral factors (e.g. exclusive breastfeeding for six months or longer) (Table 2). The mean WHZ at the end of the follow-up was 0.73 (95%CI 0.65 to 0.81) under no intervention and 0.63 (0.38 to 0.87) when all interventions were imposed (Table 2). The most effective single intervention in this study was exclusive breastfeeding for six months or longer (population mean difference = −0.11, (95% CI −0.22 to 0.01) (Figure). The population mean difference for the other interventions were as follows: watching TV for no more than one hour a day: 0.00 (95% CI −0.10 to 0.09); eating at least five fruits and vegetables a day: 0.02 (95%CI −0.02, 0.06); eliminating SSB consumption: 0.01 (95%CI −0.03 to 0.06) and playing at the playground everyday: 0.01 (95%CI −0.14 to 0.18). Further adjusting for maternal BMI did not change the results in any substantive way (Figure and Table 2). Results from sensitivity analyses showed patterns similar to those reported in the main analyses (eTables 5–9).
Table 2.
Mean WHZ score under hypothetical lifestyle interventions
| Interventions | Mean WHZ at the end of follow-upa (n = 799) | Mean WHZ at the end of follow- upb (n = 553) | Average percent intervened on (%)c |
|---|---|---|---|
| (0) No intervention, natural course | 0.73 (0.65 to 0.81) | 0.71 (0.62 to 0.80) | 0 |
| (1) Breastfeed exclusively for at least 6 months | 0.62 (0.49 to 0.77) | 0.63 (0.48 to 0.78) | 77 |
| (2) Watch TV for no more than one hour a day | 0.72 (0.61 to 0.84) | 0.74 (0.60 to 0.87) | 65 |
| (3) Eat at least five fruits and vegetables/day | 0.75 (0.66 to 0.84) | 0.71 (0.60 to 0.82) | 38 |
| (4) Eliminate SSB consumption | 0.74 (0.65 to 0.83) | 0.73 (0.63 to 0.84) | 35 |
| (5) Play at the playground everyday | 0.74 (0.57 to 0.92) | 0.67 (0.47 to 0.87) | 90 |
| (6) Eliminate fast-food consumption | 0.69 (0.52 to 0.86) | 0.63 (0.40 to 0.87) | 85 |
| (7) Low-risk lifestyle intervention ( 1– 3 combined) | 0.64 (0.48 to 0.79) | 0.65 (0.47 to 0.84) | 94 |
| (8) Low-risk lifestyle intervention ( 1 + 4 + 6 combined) | 0.60 (0.39 to 0.81) | 0.56 (0.32 to 0.81) | 97 |
| (9) All interventions (1 – 6 combined) | 0.63 (0.38 to 0.87) | 0.55 (0.25 to 0.85) | 100 |
Model 1 adjusted for baseline WHZ1, baseline age, gender, race/ethnicity, birthweight, maternal language preference, maternal educational level, maternal age, family size, family monthly income, follow-up time.
Model 2 adjusted for model 1 covariates and maternal BMI
Note that the model for WHZ3 further included interaction terms between race and WHZ2 and between WHZ1 and WHZ2. No interaction was included in the WHZ2 model
Using the first analytic sample (n=799)
Figure.
Forest-plot of the population impacts of hypothetical lifestyle interventions, WIC cohort, 2008–2010
BF, Exclusive breastfeeding duration; TV, television viewing; FV, fruits and vegetable consumption. Model 1 adjusted for baseline WHZ1, baseline age, gender, race/ethnicity, birthweight, maternal language preference, maternal educational level, maternal age, family size, family monthly income, follow-up time and Model 2 adjusted for model 1 covariates and maternal BMI.
DISCUSSION
The purpose of this study was to evaluate the potential impact of hypothetical early behavioral interventions on childhood adiposity in a multi-ethnic and cohort of children aged 1–5 years living in low-income households. Using causal inference methods, we predicted WHZ at the end of follow-up under various hypothetical interventions and contrasted it to the status quo (no intervention) in order to estimate its potential population impact. Our findings suggest that a hypothetical intervention promoting exclusive breastfeeding for six months or longer, alone or in combination with other early behavioral interventions, may reduce a child’s subsequent WHZ. The other early behavioral interventions evaluated singly in this study did not appear to have as much impact on a child’s adiposity trajectory (through age 5 years) as breastfeeding alone did.
Breastfeeding is known to have many benefits. However, its role in obesity prevention is less established.(16,17) Systematic reviews and meta-analyses of observational have concluded that breastfeeding is associated with lower risk of childhood obesity,(14) and our findings are consistent with this conclusion. However, a RCT of a breastfeeding promotion intervention did not find intervention effects on adiposity measures.(18) While this was an impressive effort involving 31 hospitals and clinics and over 15,000 infants, the study took place in Belarus where obesity prevalence is relatively low. Furthermore, the analysis was based on intention-to-treat.
Our findings derived using causal inference methods, support the conclusion that breastfeeding may protect against obesity development in early childhood. Several possible biological mechanisms can explain this protective effect. First, breast milk provides a moderate amount of calories and protein as compared to formula feeding;(19) higher early intakes of protein have been shown to be associated with later adiposity.(20) Second, breast milk is also rich in factors such as leptin, which regulate satiety and subsequent growth and development.(21) Third, it has been suggested that breastfed children may adapt better to new foods compared to formula-fed children.(22)All these mechanisms may also explain why longer duration of breastfeeding, as recommended by the WHO,(23) may help reduce the risk of developing obesity.
In this study, contrary to our expectations, watching television for no more than one hour/day, eating at least five fruits and vegetables a day, playing at the playground every day, eliminating SSB consumption and eliminating fast-food consumption, evaluated singly did not have as much impact on the child’s adiposity trajectory through age 5 as exclusive breastfeeding. This is somewhat surprising as interventions developed to mitigate most of these risk factors have been observed to lower obesity risk among exposed children.(5) One reason why we failed to find an effect could be that our study focused on much younger children than those investigated in most other studies; young children are less likely to engage in vigorous physical activity and eat fast-food than older children. Another reason is that the effects of interventions are more easily detected when there is considerable variation in the behaviors studied. Alternatively, our findings may have merely reflected beneficial effects on growth that could not be detected so early in life. This has also been seen in some RCTs where interventions on parents to promote healthy behavior among children seemed to have little or no effect on childhood obesity risk.(24) Regardless, these behavioral interventions are still warranted for their potential long-term benefits on overall health and well-being.
This study has several limitations. First, we did not have measurements on certain prenatal factors such as smoking during pregnancy and gestational diabetes which are often considered potential confounders of the association between breastfeeding (and other behavioral factors) and childhood obesity.(14,25). Nonetheless, our current covariate adjustment may have minimized this residual confounding since some measured covariates such as maternal education and age are also predictive of these unmeasured factors.(26,27) Second, we did not adjust for the child’s energy intake from solid foods and for parental feeding practices. Third, as can be expected of observational studies, our findings could have been affected by reporting bias and social desirability. However, the magnitude of such bias, if present, would likely be small in this study since a multi-item indirect questioning approach rather than a binary response approach was used to gather relevant information(28) [for example, “How old was the child, the first time (he/she) ate anything besides breast milk?” rather than “Did you breastfeed?”]. Fourth, because eligible participants had to have three consecutive measurements, they were more likely to be younger children since WIC serves children up to only age 5 years. Also, the sample consisted of a high percentage of Spanish-speaking Hispanics who are more likely to stay in WIC longer.(29) Therefore, our results are more generalizable to younger Hispanic children with Spanish-speaking mothers.
The strengths of this study include its longitudinal nature, the relatively large and ethnically diverse sample, the use of causal inference methods, the assessment of multiple behavioral interventions, the use of measured validated heights and weights, the use of WHZ as an adiposity indicator, and various sensitivity analyses. To our knowledge, this is the first attempt to use the parametric g-formula(15) to infer population-level effects of breastfeeding on obesity using individual-level effect estimates. However, it is important to note that while the findings of this study contribute to our collective effort to better understand the role of breastfeeding in obesity development during childhood, they simply provide an estimate of the impact of a breastfeeding intervention in the hypothetical scenario when women exclusively breastfeed for 6 months.
Randomized trials are not always feasible or are difficult to implement, and while they are considered the “gold standard” research design for evaluating community health interventions, they are limited in their applications in real life. This study illustrates the use of the g-computation formula, a more practical and cost effective alternative for examining the controversial role of breastfeeding in reducing childhood obesity risk. Our findings suggest that efforts to promote exclusive breastfeeding in combination with other lifestyle interventions may prove to be an effective strategy for preventing obesity later in life among minority populations and those living in poverty. It is hoped that this study will stimulate further foray into the use of modern causal reasoning and simulation methods for addressing crucial policy questions relevant to obesity and its public health consequences.(30)
Supplementary Material
What is already known about this subject
Childhood obesity is a critical public health problem, which can be addressed through early life prevention.
Modifiable risk factors have been identified.
Randomized trials are often impractical to implement.
What this study adds
Breastfeeding was more effective in reducing obesity risk in children aged 1–5 years compared to the other behavioral interventions evaluated in this study.
Causal inference methods such as the g-formula may offer a viable alternative to randomized trials in evaluation research and policy decision making.
Acknowledgments
Funding/Support: This study was partially supported by 1R01HD072296 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (RAN, MCW, TZN, CMC, SEW, OAA). In addition, RAN received fellowship support from the UCLA Department of Epidemiology and the Burroughs-Wellcome Fund, and AW received a Dissertation Year Fellowship from the University of California, Los Angeles (UCLA). TZN and RAN also benefited from facilities and resources provided by the California Center for Population Research at UCLA (CCPR), which receives core support (R24-HD041022) from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD). CMC was also partially supported by UL1TR000124 from the National Institutes of Health/National Center for Advancing Translational Science. Analysis of WIC data has been supported since 2002 through a Research Partnership with First 5 LA. The funder had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Footnotes
CONFLICT OF INTEREST STATEMENT: The authors declare no conflicts of interest.
Authors’ contributions: RAN contributed to problem definition, conceptualized the analysis plan, conducted the data analysis and wrote the first draft. OAA and MCW led the problem definition, helped conceptualize and supervise the implementation of the analysis plan, reviewed and revised the manuscript. AW and TZN helped with data management and analysis and reviewed and revised the manuscript. CMC and SEW participated in the study design and reviewed and revised the manuscript. SEW directed the design and implementation of the survey. All authors provided critical input and insights into the development and writing of the article and approved the final manuscript as submitted
References
- 1.Ogden CL, Carroll MD, Kit BK, et al. JAMA. Vol. 311. American Medical Association; 2014. Prevalence of childhood and adult obesity in the United States, 2011–2012; pp. 806–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Singh AS, Mulder C, Twisk JWR, et al. Tracking of childhood overweight into adulthood: a systematic review of the literature. Obes Rev. 2008;9:474–88. doi: 10.1111/j.1467-789X.2008.00475.x. [DOI] [PubMed] [Google Scholar]
- 3.Freedman DS, Dietz WH, Srinivasan SR, et al. The relation of overweight to cardiovascular risk factors among children and adolescents: the Bogalusa Heart Study. Pediatrics. 1999;103:1175–1182. doi: 10.1542/peds.103.6.1175. [DOI] [PubMed] [Google Scholar]
- 4.Silveira JAC, Colugnati FAB, Poblacion AP, et al. The role of exclusive breastfeeding and sugar-sweetened beverage consumption on preschool children’s weight gain. Pediatr Obes. 2015;10:91–7. doi: 10.1111/ijpo.236. [DOI] [PubMed] [Google Scholar]
- 5.Doak CM, Visscher TLS, Renders CM, et al. The prevention of overweight and obesity in children and adolescents: a review of interventions and programmes. Obes Rev. 2006;7:111–36. doi: 10.1111/j.1467-789X.2006.00234.x. [DOI] [PubMed] [Google Scholar]
- 6.Murthy VH, Krumholz HM, Gross CP. Participation in cancer clinical trials: race, sex-, and age-based disparities. JAMA. 2004;291:2720–6. doi: 10.1001/jama.291.22.2720. [DOI] [PubMed] [Google Scholar]
- 7.Taubman SL, Robins JM, Mittleman MA, et al. Intervening on risk factors for coronary heart disease: an application of the parametric g-formula. Int J Epidemiol. 2009;38:1599–1611. doi: 10.1093/ije/dyp192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Danaei G, Pan A, Hu FB, et al. Hypothetical midlife interventions in women and risk of type 2 diabetes. Epidemiology. 2013;24:122–8. doi: 10.1097/EDE.0b013e318276c98a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Public Health Foundation Project WIC. Data Mining Project. 2002 http://www.phfewic.org/projects/DataMining.aspx.
- 10.Crespi CM, Alfonso VH, Whaley SE, et al. Validity of child anthropometric measurements in the Special Supplemental Nutrition Program for Women, Infants, and Children. Pediatr Res. 2012;71:286–92. doi: 10.1038/pr.2011.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jones A, Charakida M, Falaschetti E, et al. Adipose and height growth through childhood and blood pressure status in a large prospective cohort study. Hypertension. 2012;59:919–25. doi: 10.1161/HYPERTENSIONAHA.111.187716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kuczmarski RJ, Ogden CL, Guo SS, et al. 2000 CDC Growth Charts for the United States: methods and development. Vital Health Stat. 2002;11:1–190. [PubMed] [Google Scholar]
- 13.Greenland S, Pearl J, Robins JM. Causal diagrams for epidemiologic research. Epidemiology. 1999;10:37–48. [PubMed] [Google Scholar]
- 14.Yan J, Liu L, Zhu Y, et al. The association between breastfeeding and childhood obesity: a meta-analysis. BMC Public Health. 2014;14:1267. doi: 10.1186/1471-2458-14-1267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Robins JM, Hernan MA. Estimation of the causal effects of time-varying exposures. In: Verbeke G, Davidian M, Fitzmaurice G, et al., editors. Longitidun. Boca Raton, FL: Chapman and Hall/CRC; 2009. [Google Scholar]
- 16.Casazza K, Fontaine KR, Astrup A, et al. Myths, Presumptions, and Facts about Obesity. N Engl J Med. 2013;368:446–454. doi: 10.1056/NEJMsa1208051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hancox RJ, Stewart AW, Braithwaite I, et al. Association between breastfeeding and body mass index at age 6–7 years in an international survey. Pediatr Obes. 2015;10:283–7. doi: 10.1111/ijpo.266. [DOI] [PubMed] [Google Scholar]
- 18.Kramer MS, Matush L, Vanilovich I, et al. Effects of prolonged and exclusive breastfeeding on child height, weight, adiposity, and blood pressure at age 6.5 y: evidence from a large randomized trial. Am J Clin Nutr. 2007;86:1717–1721. doi: 10.1093/ajcn/86.5.1717. [DOI] [PubMed] [Google Scholar]
- 19.Hernell O. Human milk vs. cow’s milk and the evolution of infant formulas. Nestle Nutr Workshop Ser Pediatr Program. 2011;67:17–28. doi: 10.1159/000325572. [DOI] [PubMed] [Google Scholar]
- 20.Rolland-Cachera MF, Deheeger M, Akrout M, et al. Influence of macronutrients on adiposity development: a follow up study of nutrition and growth from 10 months to 8 years of age. Int J Obes Relat Metab Disord. 1995;19:573–8. [PubMed] [Google Scholar]
- 21.Casabiell X, Piñeiro V, Tomé MA, et al. J Clin Endocrinol Metab. Endocrine Society; 2013. Presence of Leptin in Colostrum and/or Breast Milk from Lactating Mothers: A Potential Role in the Regulation of Neonatal Food Intake. [DOI] [PubMed] [Google Scholar]
- 22.Birch LL, Fisher JO. Development of eating behaviors among children and adolescents. Pediatrics. 1998;101:539–549. [PubMed] [Google Scholar]
- 23.World Health Organization. The optimal duration of exclusive breastfeeding. 2001. Global strategy for infant and young child feeding; pp. 1–5. [Google Scholar]
- 24.Nyberg G, Sundblom E, Norman Å, et al. Effectiveness of a universal parental support programme to promote healthy dietary habits and physical activity and to prevent overweight and obesity in 6-year-old children: the Healthy School Start Study, a cluster-randomised controlled trial. PLoS One. 2015;10:e0116876. doi: 10.1371/journal.pone.0116876. Public Library of Science. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shearrer GE, Whaley SE, Miller SJ, et al. Association of gestational diabetes and breastfeeding on obesity prevalence in predominately Hispanic low-income youth. Pediatr Obes. 2015;10:165–71. doi: 10.1111/ijpo.247. [DOI] [PubMed] [Google Scholar]
- 26.Ergin I, Hassoy H, Tanik FA, et al. Maternal age, education level and migration: socioeconomic determinants for smoking during pregnancy in a field study from Turkey. BMC Public Health. 2010;10:325. doi: 10.1186/1471-2458-10-325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Makgoba M, Savvidou MD, Steer PJ. An analysis of the interrelationship between maternal age, body mass index and racial origin in the development of gestational diabetes mellitus. BJOG. 2012;119:276–82. doi: 10.1111/j.1471-0528.2011.03156.x. [DOI] [PubMed] [Google Scholar]
- 28.Sanzone LA, Lee JY, Divaris K, et al. A cross sectional study examining social desirability bias in caregiver reporting of children’s oral health behaviors. BMC Oral Health. 2013;13:24. doi: 10.1186/1472-6831-13-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chaparro MP, Whaley SE, Crespi CM, et al. Influences of the neighbourhood food environment on adiposity of low-income preschool-aged children in Los Angeles County: a longitudinal study. J Epidemiol Community Health. 2014;68:1027–1033. doi: 10.1136/jech-2014-204034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nianogo RA, Arah OA. Agent-based modeling of noncommunicable diseases: a systematic review. Am J Public Health. 2015;105:e20–31. doi: 10.2105/AJPH.2014.302426. American Public Health Association. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.