The Editor,
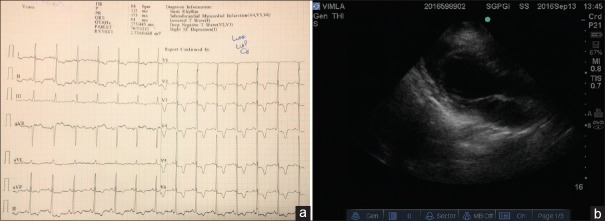
A 64-year-old female diagnosed as a case of transitional cell carcinoma of the ureter. During preanesthetic checkup, we found hypertensive and electrocardiogram (ECG) showed high-voltage QRS complexes with deep T-wave inversion in the chest leads V1-6 and ST segment depression in leads V5-6 [Figure 1a]. ECG and echocardiography, showing apical hypertrophy of left ventricle with Grade-1 diastolic dysfunction without any regional wall motion abnormality, were diagnosed as a case of apical variant of hypertrophic cardiomyopathy (HCM). The gradient across left ventricle was normal without systolic anterior motion of mitral leaflet and no left ventricular outlet obstruction [Figure 1b]. Holter monitoring to rule out any arrhythmia was normal. She was scheduled for laparoscopic radical nephroureterectomy with bladder cuff incision in right lateral kidney position under general anesthesia (GA) with epidural analgesia. She was premeditated with tablet alprazolam 0.25 mg night before surgery. Monitoring was initiated with ECG, noninvasive blood pressure, SpO2 and bispectral index (for depth of anesthesia monitoring). A large bore 16 G IV cannula and FloTrac (FloTrac System, Edward Life Sciences, USA) were used to monitor cardiac output, stroke volume variation, systemic vascular resistance throw 20 G arterial line under local anesthesia.
Figure 1.
(a) Electrocardiogram-12 lead showing high-voltage QRS complexes with deep T-wave inversion in chest leads V1-6 and ST segment depression in leads V5 and V6. (b) Two-dimensional – echo parasternal long axis showing left ventricle apical hypertrophy with no left ventricular outlet obstruction
After preoxygenation, balanced GA was induced with injection fentanyl 100 mcg and etomidate 10 mg. Trachea was intubated with 7.5 number cuffed endotracheal tube. Maintenance was done with 50% oxygen in air and desflurane, fentanyl, and atracurium. A 7F triple lumen central venous line (arrow) was put in left internal jugular vein using ultrasound (Sonosite, USA). Epidural catheter (BD, India) was put at T9 level in left lateral position and injection fentanyl 100 mcg was given before start of surgery. There was one episode of bradycardia without hemodynamic instability; at the time of gas insufflations, may be because of vagal stimulation. Surgeon was asked to hold surgery and heart rate became normal within seconds. Except for this event, she remained hemodynamically stable throughout for 4 h of surgery without any significant blood loss. She was extubated on table and kept in the postoperative Intensive Care Unit for monitoring.
Apical variant of HCM also called as Yamaguchi syndrome is a rare genetic disorder which is present in around 5% cases of HCM in non-Japanese population.[1] Its diagnosis is based on characteristics ECG changes as above.[2] In the ventriculogram, left ventricle appears like an “ace of spades.” This apical variant of HCM can be associated with serious complications such as arrhythmias, embolic events, myocardial infarction (MI), ventricular aneurysm, and sudden cardiac death.[3] Anesthetic management of these patients are similar to case of hypertrophic obstructive cardiomyopathy which includes alleviating sympathetic stimulation which includes avoiding tachycardia, maintaining normal sinus rhythm and euvolemia, and avoiding any increase in cardiac contractility.[4]
If this operation was done as open procedure, the big incision has intense pain and sympathetic stimulation postoperatively may precipitate any unwanted cardiac side effects in this patient. This surgery is usually done laparoscopically under GA at our institute. However, for bladder cuff incision and delivery of excised kidney, a 5–6 cm incision is needed below umbilical. For better pain relief because of this incision postoperatively, epidural analgesia was given.
Preoperatively, it is important to rule out coronary artery disease as most of these patients have ST segment depression with T-wave inversion in ECG leads. She has started on tablet metoprolol 50 mg OD, as beta blockers, which decreases the left ventricular outlet obstruction, and decreases myocardium workload, and decreases chances of perioperative MI.[5] Sinus rhythm is important in these patients as their preload depends on the atrial contraction. We adequately preloaded with crystalloid 30 ml/kg to maintain optimal cardiac output. Intraoperatively, fluid was given based on the values of the stroke volume variation. Vasodilators and agents which increase the cardiac contractility should be avoided.[5] Any episodes of hypotension should be treated preferably with volume replacement than with vasoconstrictors phenylephrine.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Ho AM, Chui PT, Lee AP, Wan S. Apical hypertrophic cardiomyopathy. Anesth Analg. 2015;121:1398–9. doi: 10.1213/ANE.0000000000000867. [DOI] [PubMed] [Google Scholar]
- 2.Zeineh NS, Eles G. Images in clinical medicine. Apical hypertrophic cardiomyopathy. N Engl J Med. 2015;373:e22. doi: 10.1056/NEJMicm1413682. [DOI] [PubMed] [Google Scholar]
- 3.Chan SM, Wu CT, Wong CS, Cherng CH, Lu CH. Apical hypertrophic cardiomyopathy mimicking coronary artery disease with unstable angina. J Med Sci. 2008;28:35–8. [Google Scholar]
- 4.Hensley N, Dietrich J, Nyhan D, Mitter N, Yee MS, Brady M. Hypertrophic cardiomyopathy: A review. Anesth Analg. 2015;120:554–69. doi: 10.1213/ANE.0000000000000538. [DOI] [PubMed] [Google Scholar]
- 5.Ranasinghe I, Yeoh T, Yiannikas J. Negative inotropic agents for the treatment of left ventricular outflow tract obstruction due to sigmoid septum and concentric left ventricular hypertrophy. Heart Lung Circ. 2011;20:579–86. doi: 10.1016/j.hlc.2011.05.002. [DOI] [PubMed] [Google Scholar]