Abstract
Background:
There has been a constant emphasis on developing management strategies to improve the outcome of high-risk cardiac patients undergoing surgical revascularization. The performance of coronary artery bypass surgery on an off-pump coronary artery bypass (OPCAB) avoids the risks associated with extra-corporeal circulation. The preliminary results of goal-directed therapy (GDT) for hemodynamic management of high-risk cardiac surgical patients are encouraging. The present study was conducted to study the outcome benefits with the combined use of GDT with OPCAB as compared to the conventional hemodynamic management.
Material and Method:
Patients with the European System for Cardiac Operative Risk Evaluation ≥3 scheduled for OPCAB were randomly divided into two groups; the control and GDT groups. The GDT group included the monitoring and optimization of advanced parameters, including cardiac index (CI), systemic vascular resistance index, oxygen delivery index, stroke volume variation; continuous central venous oxygen saturation (ScVO2), global end-diastolic volume, and extravascular lung water (EVLW), using FloTrac™, PreSep™, and EV-1000® monitoring panels, in addition to the conventional hemodynamic management in the control group. The hemodynamic parameters were continuously monitored for 48 h in Intensive Care Unit (ICU) and corrected according to GDT protocol. A total of 163 patients consented for the study.
Result:
Seventy-five patients were assigned to the GDT group and 88 patients were in the control group. In view of 9 exclusions from the GDT group and 12 exclusions from control group, 66 patients in the GDT group and 76 patients in control group completed the study.
Conclusion:
The length of stay in hospital (LOS-H) (7.42 ± 1.48 vs. 5.61 ± 1.11 days, P < 0.001) and ICU stay (4.2 ± 0.82 vs. 2.53 ± 0.56 days, P < 0.001) were significantly lower in the GDT group as compared to control group. The duration of inotropes (3.24 ± 0.73 vs. 2.89 ± 0.68 h, P = 0.005) was also significantly lower in the GDT group. The two groups did not differ in duration of ventilated hours, mortality, and other complications. The parameters such as ScVO2, CI, and EVLW had a strong negative and positive correlation with the LOS-H with r values of − 0.331, −0.319, and 0.798, respectively. The study elucidates the role of a goal-directed hemodynamic optimization for improved outcome in high-risk cardiac patients undergoing OPCAB.
Keywords: Cardiac index, extravascular lung water, goal directed therapy, off pump CABG
Introduction
Coronary artery disease is a common cause of death in the world. The extensive disease in few patients cannot be managed by medical treatment. Surgical revascularization has yielded promising results in such condition. The standard procedure is coronary artery bypass surgery with the use of cardiopulmonary bypass (CPB) under cardioplegic arrest. The use of CPB has its own risk factors such as systemic inflammatory response, coagulation disorders, and multiple organ dysfunction. The development of epicardial stabilization devices such as Octopus has facilitated coronary artery bypass grafting (CABG) without the use of CPB, also known as off-pump coronary artery bypass grafting (OPCAB). This technique decreases the incidence of postoperative neurological complications and the need for transfusion relative to conventional coronary bypass.[1] The technique has allowed to be used in patients with compromised left ventricular function. These patients get benefited from the avoidance of CPB. Therefore, nowadays, an increase in the number of OPCAB procedures has been observed. But still, a considerable number of patients develop problems in perioperative period, which include prolonged duration of mechanical ventilator support, Intensive Care Unit (ICU) admission, and hospital stay of patients. This entails increased burden on the health-care resources.
Goal-directed therapy (GDT) is a term used to describe the use of cardiac output (CO) or similar parameters to guide intravenous fluid and inotropic therapy. It involves goal-directed manipulation of cardiac preload, afterload, and contractility to achieve a balance between systemic oxygen demand and delivery. There are some studies documenting the positive role of GDT in decreasing morbidity and mortality in cardiac surgical patients.[2,3]
We have used GDT in moderate-to-high risk patients with the European System for Cardiac Operative Risk Evaluation (EuroSCORE) ≥3 undergoing CABG with the use of CPB and found beneficial result of GDT in these patients.[4] We now assume that using GDT during perioperative period in patients with OPCAB will also help us to maintain cardiovascular parameters within normal limits which in turn decrease postoperative complications in perioperative period and decrease the total duration of mechanical ventilation, ICU, and hospital stay. There are limited studies in patients for OPCAB in literature using GDT.[5] However, they involve a small number of patients from a single center. Here, we have done this study to find efficacy of the GDT in patients undergoing OPCAB in two cardiac surgical centers.
Aims and objectives
The aim and objective of this study was to compare outcome in terms of total duration of mechanical ventilation and inotropic support, ICU, and hospital stay required in patients managed with the GDT as compared to the conventional hemodynamic management in patients undergoing OPCAB.
And also, it aimed to study the correlation of advanced hemodynamic parameters with the length of stay in hospital.
Study design
It is a randomized, prospective, and multicenter study. This study was done in All India Institute of Medical Sciences, New Delhi, and Medanta, The Medicity, Gurgaon.
Inclusion criteria
Patients
Adult patients of both sexes and age more than 18 years with elective coronary artery bypass waiting list with EuroSCORE ≥3 were enrolled in this study.
Exclusion criteria
Patients having cardiac arrhythmia, emergency or redo surgery, severe renal impairment, familial hypercoagulability (lupus anticoagulant, protein C deficiency), and thromboembolic disease (pulmonary embolism, spontaneous arterial embolism) were excluded from the study. Contraindication to central venous cannulation and patients on intra-aortic balloon pump (IABP) were also excluded from the study.
Materials and Methods
This study was done in two cardiac centers in Delhi and NCR Region. The patients were randomly divided into two groups, namely control group and gold-directed group by a sealed envelope technique. All patients received intramuscular premedication of morphine 0.1 mg/kg and promethazine 0.5 mg/kg, 30 min before operation. Standard techniques of induction and maintenance of anesthesia using midazolam, fentanyl, and sleep dose of thiopentone were followed in these patients. Rocuronium 1 mg/kg was used for intubation. All the patients were ventilated with 50% oxygen in air using 1 minimum alveolar concentration sevoflurane and respiratory rate adjusted to maintain end-tidal CO2 (EtCO2) 35–45 mmHg. In control group, patients were continuously monitored by electrocardiogram, pulse oximetry, EtCO2, invasive arterial blood pressure, nasopharyngeal temperature, and urine output. Any derangement in parameters was corrected at the earliest with standard techniques. Blood glucose level was maintained in between 80 and 180 mg/dL with the use of plain insulin actrapid, if required.
In GDT group, additional PreSep™ oximetry catheter was inserted through the right internal jugular vein. One FloTrac device (Edwards Lifesciences, Irvine, CA, USA) was attached to arterial line. We used a special device known as EV-1000 clinical platform (Edwards Lifesciences) for monitoring hemodynamic parameters, such as global end-diastolic volume (GEDV) and extravascular lung water (EVLW). Pressure transducers, FloTrac sensor, and PreSep™ oximetry catheters were used to transfer these signals from patients to its data box. An algorithm embedded in its data box processes signals and provides stroke volume (SV), CO, cardiac index (CI), systemic vascular resistance (SVR), SV variation (SVV), oxygen delivery index (DO2 I), and central venous oxygen saturation (ScVO2) [Figure 1]. We assumed that continuous monitoring would enable us to assess the various abnormal physiological parameters of patients and we could manage them at the earliest in patients who are undergoing OPCAB.
Figure 1.
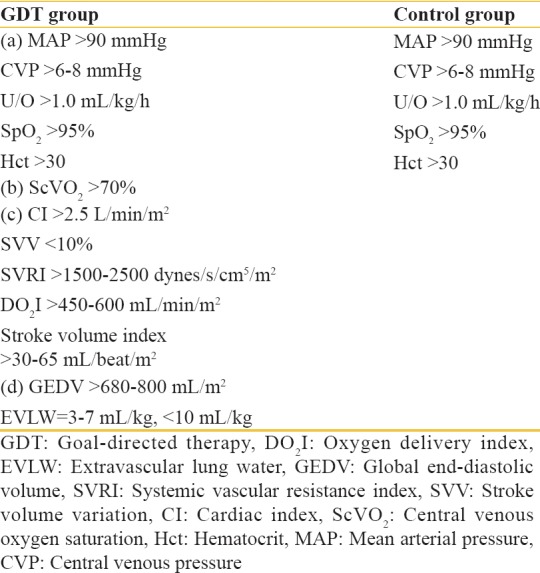
The hemodynamic goals of management in the goal-directed therapy and control groups
After surgery, all the patients were shifted to the ICU on full mechanical ventilation support and ventilated for 4 h. After this period, patients were weaned from ventilator support. Once they met the criteria of extubation, the endotracheal tube was removed from trachea. The decision was based on the normalization of arterial blood gas (ABG) analysis of pH 7.35–7.45, PaO2 >100 mmHg (with FiO2 of <50%), and lactate <2 mmol/L. Standard protocol for weaning was followed for extubation of trachea. Thereafter, patients were monitored for the next 48 h, and any derangement was corrected at the earliest.
All patients received maintenance fluid ringer lactate 1 mL/kg/h. Hematocrit was maintained at more than 30%, and packed red blood cell (PRBC) was given if required. Central venous pressure (CVP) was maintained at 6–8 mmHg. If it is less, fluid bolus of 100 mL crystalloid or colloid was given to the patients. It was repeated, if required, to bring CVP within the prescribed range. The mean arterial pressure (MAP) was adjusted >90 mmHg, with fluid boluses (initially) and use of inotrope infusion of dobutamine starting from 5 μg/kg/min, epinephrine with starting dose of 0.05 μg/kg/min or support, and vasodilator infusion of nitroglycerin of 0.5 μg/kg/min. The dose of inotrope infusion was escalated if required. ABG was done at 4 hourly intervals.
In addition, the following interventions were done to manage patients in GDT group. An increase in SVV more than 10% was managed by giving fluid boluses, which was repeated in frequent intervals to maintain it <10%. With low hematocrit and ScVO2 reading of <70%, transfusion of PRBC was given to keep hematocrit more than 30%. With persistent low ScVO2 along with low CI, we started inotropic support of dobutamine starting from 5 μg/kg/min or epinephrine with starting dose of 0.05 μg/kg/min. This inotropic support was increased if required and titrated to maintain CI within 2.0–4.5 L/min/m2. Inotropic agents and vasodilators were adjusted to maintain the parameters such as EVLW <7 mL/kg and GEDV within the target values.
These hemodynamic parameters were continuously monitored for 48 h in the ICU and corrected according to protocol. Each patient was followed up for 1 month or until death.
The endpoints
The endpoints were duration of mechanical ventilation and inotropic support, length of ICU stay and hospital stay.
Statistical analysis
The quantitative variables in both groups are expressed as mean ± standard deviation and compared using unpaired t-test/Mann–Whitney test between groups and paired t-test within groups at various follow-ups. The qualitative variables are expressed as frequencies/percentages and compared using Chi-square test. Pearson's correlation coefficient was used to identify correlations between quantitative variables. P < 0.05 was considered statistically significant. Statistical Package for Social Sciences (SPSS, IBM Corporation, USA) version 16.0 was used for statistical analysis.
Results
The study was done in two cardiac surgical centers. Ethical committee approval for the study was obtained from the respective Institutional Committee. A total of 163 patients had given consent for the study. About 88 patients were assigned in control group and 75 patients were assigned in GDT group. Four patients in control group and three patients in GDT group developed hemodynamic disturbances during surgery, for which either IABP was inserted or surgeon decided to complete operation using CPB. They were excluded from the study. Eight patients in control group and six patients in GDT group developed arrhythmias in perioperative period, the most common being atrial fibrillation or frequent ventricular premature contractions. The reading from FloTrac-based monitoring was not reliable during arrhythmia. We have used this device in GDT group. These were also excluded from the study. Totally 76 participants in control group and 66 patients in GDT group completed the study for analysis [Figure 2].
Figure 2.
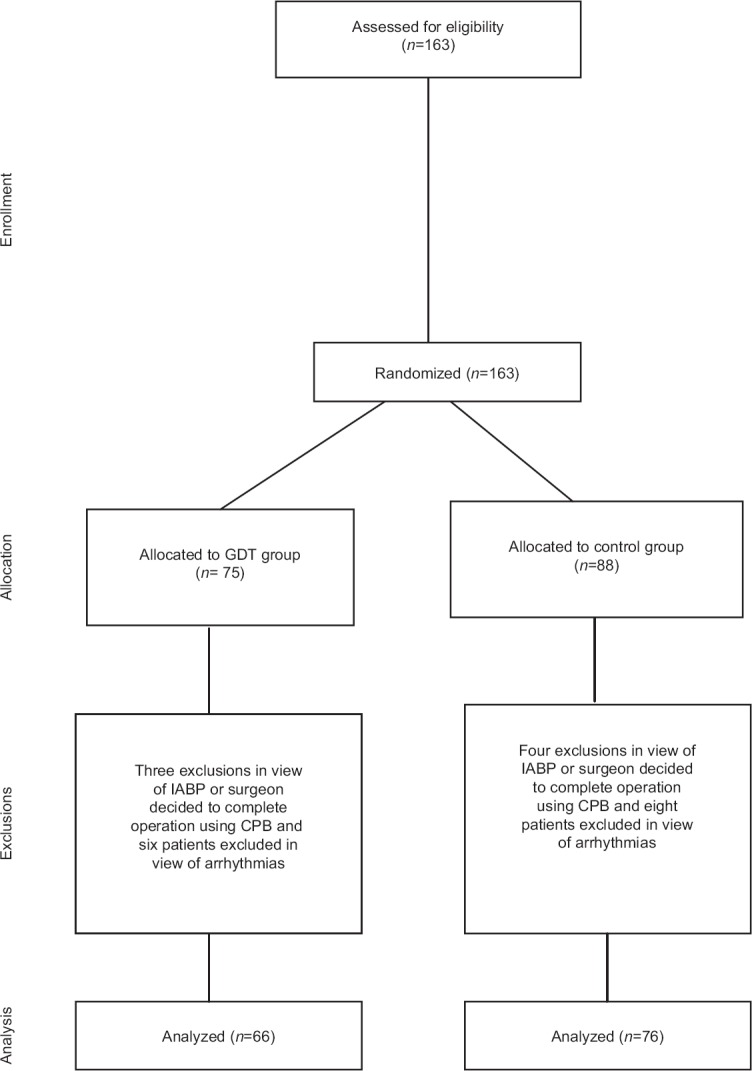
The study and analytical design (indications for converting into cardiopulmonary bypass – persistence of the following for >15 min despite aggressive therapy: cardiac index <1.5 L/min/m2, SvO2 <60%, mean arterial pressure <50 mmHg, ST-segment elevation >2 mV, large new wall motion abnormalities or collapse of left ventricle function assessed by transesophageal echocardiography, and sustained malignant arrhythmias, depending on the available monitoring in the individual group)
The two groups were comparable with respect to the demographic characteristics [Table 1] and the baseline risk factors. Heart rate, MAP, and CVP at various time intervals were comparable between the groups [Table 2]. ScVO2, CI, SVV, SVR index, stroke volume index (SVI), DO2 I, GEDV, and EVLW were maintained within the physiological values in the GDT group.
Table 1.
Demographic characteristics in the two groups
| Parameter | Control group (n=76) | GDT group (n=66) | P |
|---|---|---|---|
| Age (years) | 61.26±5.45* | 61.27±5.47* | 0.992 |
| Male: female | 62:14 | 55:11 | 0.784 |
| Height (cm) | 161.39±5.27* | 159.71±5.86* | 0.074 |
| Weight (kg) | 73.50±14.35* | 72.67±8.49* | 0.705 |
| EuroSCORE | 4.13±0.79* | 4.02±0.83* | 0.394 |
| Number of grafts | 3.63±0.65* | 3.48±0.73* | 0.207 |
*Standard deviation, P<0.05 is considered statistically significant. EuroSCORE: European System for Cardiac Operative Risk Evaluation, GDT: Goal-directed therapy
Table 2.
Heart rate, mean arterial pressure, and central venous pressure in the two groups
| Parameter | Time | Control group (n=76) | GDT group (n=66) | P |
|---|---|---|---|---|
| Heart rate | T1 | 68.07±6.61* | 68.61±5.47* | 0.600 |
| T2 | 92.17±6.89* | 92.53±7.21 | 0.762 | |
| T3 | 100.58±7.6* | 98.80±7.52* | 0.165 | |
| T4 | 101.13±5.67* | 99.14±7.7* | 0.078 | |
| T5 | 101.99±5.38* | 100.55±7.58* | 0.189 | |
| T6 | 101.53±6.62* | 99.86±6.83* | 0.144 | |
| MAP | T1 | 89.01±6.96* | 89.14±6.15* | 0.912 |
| T2 | 94.43±4.31* | 93.85±5.36* | 0.472 | |
| T3 | 93.96±11.85* | 94.33±5.65* | 0.816 | |
| T4 | 93.33±5.33* | 93.65±4.88* | 0.709 | |
| T5 | 94.82±5.05* | 94.44±5.4* | 0.669 | |
| T6 | 93.03±5.16* | 94.08±5.5* | 0.243 | |
| CVP | T1 | 6.21±0.48* | 6.24±0.43* | 0.746 |
| T2 | 6.65±0.89* | 6.53±0.84* | 0.389 | |
| T3 | 6.55±1.07* | 6.30±0.57* | 0.087 | |
| T4 | 6.70±0.7* | 6.91±0.93* | 0.133 | |
| T5 | 6.82±0.86* | 7.09±0.98* | 0.081 | |
| T6 | 6.83±1.00* | 6.99±1.14* | 0.398 |
*Standard deviation, P<0.05 is considered statistically significant. T1 (baseline), T2 (sternal closure), T3 (0), T4 (12), T5 (24), T6 (48) hours in ICU. ICU: Intensive Care Unit, GDT: Goal-directed therapy, MAP: Mean arterial pressure, CVP: Central venous pressure
There was a statistically significant difference in the number of times the inotropic agents were changed for hemodynamic optimization (2.04 ± 0.58 vs. 3.11 ± 0.61*, P < 0.001) in the control and GDT groups, respectively [Table 3]. The duration of inotropic support (2.89 ± 0.68 days vs. 3.24 ± 0.73 days, P = 0.005), length of hospital stay (5.61 ± 1.11 days vs. 7.42 ± 1.48 days, P < 0.001) and ICU stay (2.53 ± 0.56 days vs. 4.20 ± 0.82 days, P < 0.001) were significantly less in the GDT group, compared to those in the control group [Table 3]. The duration of ventilator support was less in the GDT group, though not significant as compared to the control group. Four patients in GDT group and six patients in the control group had renal dysfunction, which improved by administering diuretics. There were six mortalities in the goal directed group and twelve mortalities in the control group during the study period. The causes ranged from malignant arrhythmias to refractory hemodynamic instability.
Table 3.
Comparison of the outcomes between the control and the goal-directed therapy groups
| Parameter | Control group | GDT group | P |
|---|---|---|---|
| Number of times inotropes adjusted | 2.04±0.58* | 3.11±0.61* | <0.001 |
| Duration of ventilation (h) | 16.36±3.84* | 15.85±1.98* | 0.336 |
| Duration of inotrope usage (days) | 3.24±0.73* | 2.89±0.68* | 0.005 |
| Length of ICU stay (days) | 4.20±0.82* | 2.53±0.56* | <0.001 |
| Length of hospital stay (days) | 7.42±1.48* | 5.61±1.11* | <0.001 |
| Mortality (%) | 12 (15.79%) | 6 (9.09%) | 0.116 |
| Renal failure (%) | 6 (7.89) | 4 (6.06) | 0.335 |
*Standard deviation, P<0.05 is considered statistically significant. ICU: Intensive Care Unit, GDT: Goal-directed therapy
The correlation analysis of the advanced hemodynamic parameters with the length of hospital stay revealed a strong negative correlation of ScVO2 and CI and a strong positive correlation of EVLW with the length of hospital stay with r values of − 0.331, −0.319, and 0.798 respectively [Figure 3]. The optimization of the hemodynamic parameters is associated with a reduced hospital stay.
Figure 3.
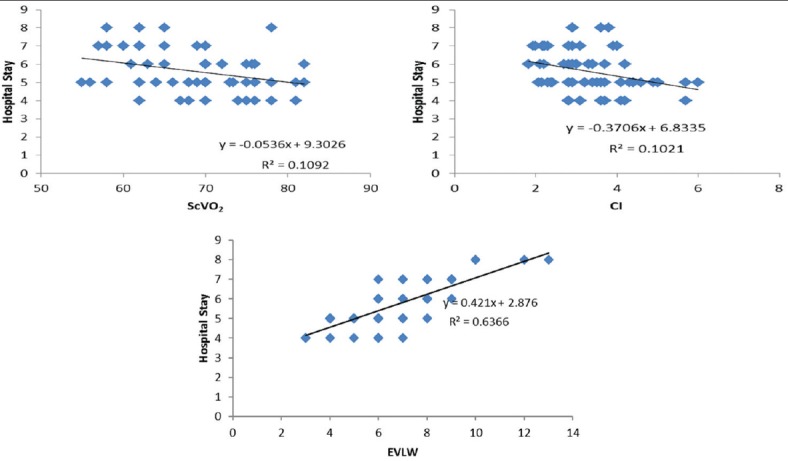
The correlation plots of central venous oxygen saturation (%), cardiac index (L/min/m2), and extravascular lung water (mL/kg) with the length of hospital stay (days). The length of hospital stay reduces with optimization of the advanced hemodynamic parameters (the strength of negative correlation: extravascular lung water >> central venous oxygen saturation >> cardiac index)
Discussion
Considering the patterns of the hemodynamic perturbations in an OPCAB procedure, it becomes imperative to adopt a robust strategy that aims at optimizing myocardial oxygen demand–supply balance. This can be effected by maintaining a low myocardial oxygen consumption and by preserving coronary artery perfusion pressure with infusion of vasopressors, inotropes, and optimization of preload and afterload.[5] Goal-directed manipulation of cardiac preload, afterload, and contractility can help achieve a balance between systemic oxygen demand and delivery in cardiac surgical patients. The study was conducted to analyze the outcome benefits with the combined use of GDT with OPCAB as compared to the conventional hemodynamic management.
Mixed venous oxygen saturation is ideally measured by estimating the oxygen content of the pulmonary artery through pulmonary artery catheter (PAC). PreSep™ central venous oximetry catheter can be used to continuously monitor the ScVO2 (though not similar to SvO2, correlates well with SvO2).[6,7] In cardiac surgery, GDT was commenced by a noninvasive method such as esophageal Doppler instead of the PAC to measure the CO.[8,9,10] Unlike the FloTrac™, Doppler probe is not readily tolerated by conscious patients, restricting its use in patients who are ventilated, and the PAC is invasive with its own set of complications. Studies by Manecke and Auger, McGee et al., and Chakravarthy et al., have validated the Vigileo system,[11,12,13] with a good agreement between CO values obtained by the FloTrac arterial pressure waveform analysis and intermittent bolus thermodilution techniques.[14]
EVLW defines the amount of fluid accumulated in the interstitial and alveolar spaces. Increased EVLW is associated with a poor outcome since it impairs gas exchange and impairs the lung compliance. Transpulmonary thermodilution provides a reliable measurement of EVLW. EV-1000®, (Edwards Lifesciences, Irvine, CA, USA) uses the Stewart–Hamilton principle to calculate the EVLW and GEDV.[15] Therapeutic algorithms including EVLW have yielded clinical benefits in high-risk cardiac surgical patients.[16]
Rivers et al. provided GDT to patients in the early stage of sepsis and septic shock and found a significant reduction in hospital stay and mortality.[17] They concluded that this benefit results from the early identification of patients at a high risk for cardiovascular collapse and early therapeutic intervention to restore a balance between oxygen delivery and demands. Smetkin et al. studied forty patients; twenty each in control and GDT groups for patients undergoing OPCAB. They monitored pulse contour analysis CO (PiCCO device) and ScvO2 and regulated their interventions by the use of fluid, blood, and inotropes. They described that GDT facilitates early detection and correction of hemodynamic changes and influences the strategy for fluid that can improve the course of postoperative period after CABG on beating heart, with a decrease in ICU and hospital duration.[18]
McKendry et al. studied a total of 179 patients, 90 in control and 89 in GDT for cardiac patients undergoing CABG and valve surgery. They used esophageal Doppler to study SVI in goal-directed group and manipulated fluids, inotropes, and nitrates according to SVI, and concluded that this technique is beneficial.[8] Gordon and Russell described substantial efficacy in reducing morbidity and mortality of high-risk surgical patients when GDT is started at an early stage. However, once organ failure is established, this benefit is lost.[19]
Pearse et al. applied GDT in postoperative period in patients after major surgery and found that it reduces complication rate and hospital length of stay.[20] A meta-analysis done by Aya et al. suggested that goal-directed hemodynamic therapy reduces postoperative complications and hospital stay after cardiac surgery.[21] We also observed a significant reduction in hospital and ICU stay with the use of GDT in our study. We also discovered that the optimization of advanced hemodynamic parameters, such as ScVO2, CI, and EVLW, is associated with a reduced length of hospital stay.
The GDT during perioperative period in patients with OPCAB helped us to detect abnormal hemodynamic parameters at the earliest, which facilitated early correction. It enabled us to maintain cardiovascular parameters within normal limits. It improved early discharge of patients from the ICU and hospital with decreased inotropic requirements.
Conclusion
GDT is associated with a decrease in the total duration of hospital and ICU stay and decreased duration of inotropic support in patients undergoing an OPCAB procedure. More multicenter trials should be performed to validate the finding to a wider population.
Interest
We have used EV-1000® clinical platform in GDT group. It is provided by Edwards Lifesciences for the study purpose. FloTrac™ and PreSep™ oximetry catheter were provided by ICMR, New Delhi.
Limitations
This study has certain limitations. GDT group involves the use of an extra monitor. The interventions performed in this group cannot be blinded. Fluid resuscitation can be subjective in managing the case clinically.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Morgan and Mikhail's. Clinical Anesthesiology. 5th ed. Ch. 22. New York: Lange; 2013. pp. 468–9. [Google Scholar]
- 2.Shoemaker WC, Appel PL, Kram HB, Waxman K, Lee TS. Prospective trial of supranormal values of survivors as therapeutic goals in high-risk surgical patients. Chest. 1988;94:1176–86. doi: 10.1378/chest.94.6.1176. [DOI] [PubMed] [Google Scholar]
- 3.Wilson J, Woods I, Fawcett J, Whall R, Dibb W, Morris C, et al. Reducing the risk of major elective surgery: Randomised controlled trial of preoperative optimisation of oxygen delivery. BMJ. 1999;318:1099–103. doi: 10.1136/bmj.318.7191.1099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kapoor PM, Magoon R, Rawat R, Mehta Y. Perioperative utility of goal-directed therapy in high-risk cardiac patients undergoing coronary artery bypass grafting: “A clinical outcome and biomarker-based study”. Ann Card Anaesth. 2016;19:638–82. doi: 10.4103/0971-9784.191552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Do QB, Goyer C, Chavanon O, Couture P, Denault A, Cartier R. Hemodynamic changes during off-pump CABG surgery. Eur J Cardiothorac Surg. 2002;21:385–90. doi: 10.1016/s1010-7940(02)00009-x. [DOI] [PubMed] [Google Scholar]
- 6.Goldman RH, Klughaupt M, Metcalf T, Spivack AP, Harrison DC. Measurement of central venous oxygen saturation in patients with myocardial infarction. Circulation. 1968;38:941–6. doi: 10.1161/01.cir.38.5.941. [DOI] [PubMed] [Google Scholar]
- 7.Lee J, Wright F, Barber R, Stanley L. Central venous oxygen saturation in shock: A study in man. Anesthesiology. 1972;36:472–8. doi: 10.1097/00000542-197205000-00012. [DOI] [PubMed] [Google Scholar]
- 8.McKendry M, McGloin H, Saberi D, Caudwell L, Brady AR, Singer M. Randomised controlled trial assessing the impact of a nurse delivered, flow monitored protocol for optimisation of circulatory status after cardiac surgery. BMJ. 2004;329:258. doi: 10.1136/bmj.38156.767118.7C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wakeling HG, McFall MR, Jenkins CS, Woods WG, Miles WF, Barclay GR, et al. Intraoperative oesophageal Doppler guided fluid management shortens postoperative hospital stay after major bowel surgery. Br J Anaesth. 2005;95:634–42. doi: 10.1093/bja/aei223. [DOI] [PubMed] [Google Scholar]
- 10.Gan TJ, Soppitt A, Maroof M, el-Moalem H, Robertson KM, Moretti E, et al. Goal-directed intraoperative fluid administration reduces length of hospital stay after major surgery. Anesthesiology. 2002;97:820–6. doi: 10.1097/00000542-200210000-00012. [DOI] [PubMed] [Google Scholar]
- 11.Manecke GR, Jr, Auger WR. Cardiac output determination from the arterial pressure wave: Clinical testing of a novel algorithm that does not require calibration. J Cardiothorac Vasc Anesth. 2007;21:3–7. doi: 10.1053/j.jvca.2006.08.004. [DOI] [PubMed] [Google Scholar]
- 12.McGee WT, Horswell JL, Calderon J, Janvier G, Van Severen T, Van den Berghe G, et al. Validation of a continuous, arterial pressure-based cardiac output measurement: A multicenter, prospective clinical trial. Crit Care. 2007;11:R105. doi: 10.1186/cc6125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chakravarthy M, Patil TA, Jayaprakash K, Kalligudd P, Prabhakumar D, Jawali V. Comparison of simultaneous estimation of cardiac output by four techniques in patients undergoing off-pump coronary artery bypass surgery: A prospective observational study. Ann Card Anaesth. 2007;10:121–6. doi: 10.4103/0971-9784.37937. [DOI] [PubMed] [Google Scholar]
- 14.Mehta Y, Chand RK, Sawhney R, Bhise M, Singh A, Trehan N. Cardiac output monitoring: Comparison of a new arterial pressure waveform analysis to the bolus thermodilution technique in patients undergoing off-pump coronary artery bypass surgery. J Cardiothorac Vasc Anesth. 2008;22:394–9. doi: 10.1053/j.jvca.2008.02.015. [DOI] [PubMed] [Google Scholar]
- 15.Kiefer N, Hofer CK, Marx G, Geisen M, Giraud R, Siegenthaler N, et al. Clinical validation of a new thermodilution system for the assessment of cardiac output and volumetric parameters. Crit Care. 2012;16:R98. doi: 10.1186/cc11366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Goepfert MS, Reuter DA, Akyol D, Lamm P, Kilger E, Goetz AE. Goal-directed fluid management reduces vasopressor and catecholamine use in cardiac surgery patients. Intensive Care Med. 2007;33:96–103. doi: 10.1007/s00134-006-0404-2. [DOI] [PubMed] [Google Scholar]
- 17.Rivers EP, Coba V, Whitmill M. Early goal-directed therapy in severe sepsis and septic shock: A contemporary review of the literature. Curr Opin Anaesthesiol. 2008;21:128–40. doi: 10.1097/ACO.0b013e3282f4db7a. [DOI] [PubMed] [Google Scholar]
- 18.Smetkin AA, Kirov MY, Kuzkov VV, Lenkin AI, Eremeev AV, Slastilin VY, et al. Single transpulmonary thermodilution and continuous monitoring of central venous oxygen saturation during off-pump coronary surgery. Acta Anaesthesiol Scand. 2009;53:505–14. doi: 10.1111/j.1399-6576.2008.01855.x. [DOI] [PubMed] [Google Scholar]
- 19.Gordon AC, Russell JA. Goal directed therapy: How long can we wait? Crit Care. 2005;9:647–8. doi: 10.1186/cc3951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pearse R, Dawson D, Fawcett J, Rhodes A, Grounds RM, Bennett ED. Early goal-directed therapy after major surgery reduces complications and duration of hospital stay. A randomised, controlled trial [ISRCTN38797445] Crit Care. 2005;9:R687–93. doi: 10.1186/cc3887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Aya HD, Cecconi M, Hamilton M, Rhodes A. Goal-directed therapy in cardiac surgery: A systematic review and meta-analysis. Br J Anaesth. 2013;110:510–7. doi: 10.1093/bja/aet020. [DOI] [PubMed] [Google Scholar]


