Abstract
Context:
Nonadherence to therapeutic plans has been reported among hypertensive patients. Researchers have also shown that adherence to therapeutic plans improves if motivation in the form of social support is provided. There is a dearth of local studies that explore the influence of family support on treatment outcomes of hypertensive patients.
Aims:
The aim of the study was to determine the relationship between BP control and perceived family support in patients with essential hypertension seen at a primary care setting in Western Nigeria.
Settings and Design:
This was a cross-sectional hospital-based study.
Subjects and Methods:
Systematic random sampling technique was used in selecting 360 hypertensive respondents between April and July 2013. Data were collected through a pretested interviewer-administered questionnaire and a standardized tool, Perceived Social Support Family Scale, which measured the respondents’ level of perceived family support.
Statistical Analysis Used:
Statistical Package for Social Sciences (SPSS) version 17.0 was used to analyze data.
Results:
The majority of the respondents were middle-aged (61.1%) and female (59.4%). Blood pressure (BP) was controlled in 46.4% of the respondents. Most of the respondents (79.4%) had “strong” perceived family support. Strong perceived family support (odds ratio [OR] 4.778, 95% confidence interval [CI] =2.569–8.887) and female gender (OR 1.838, 95% CI = 1.177–2.869) were independent predictors of controlled BP.
Conclusions:
The proportion of hypertensive patients with optimal BP control is low in this practice setting. The positive association between BP control and perceived family support emphasizes the need for physicians to reflect on the available family support when managing hypertensive patients.
Keywords: Blood pressure control, essential hypertension, perceived family support
Introduction
Hypertension is the most common noncommunicable disease seen in primary care.[1] It is estimated that nearly 1 billion people are affected by hypertension worldwide, and this figure is predicted to increase to 1.5 billion by the year 2025.[2] In Nigeria, the prevalence of hypertension varied extensively between studies, ranging from a minimum of 12.4% to a maximum of 34.8%.[3] It is a leading cause of global burden of disease with greater population burden in developing than developed countries.[2]
Based on its high prevalence and burden, it is evident that BP control is one of the challenges facing health care providers. Poor adherence to medications and healthy lifestyle has been implicated in the previous studies as a major cause of uncontrolled hypertension.[4,5] Nonadherence still occurs even in a population where antihypertensive medications are given free.[6]
The therapy prescribed by most clinicians will control hypertension only if the patient is motivated.[7] Motivation occurs and improves when the family as a social network around patients with hypertension encourages personal attitudes positively associated with health, such as sharing of information, helping in moments of crisis, and cares with health in general.[8] Can the missing link be support from the family members of this group of patients?
The lack of local study that explores the influence of family supports on BP control made it imperative to carry out this study. This study was aimed at determining the relationship between BP control and perceived family support among patients with essential hypertension.
Subjects and Methods
Study setting
This study was conducted at the Family Medicine Clinic of a Hospital in Abeokuta. Abeokuta is the Capital of Ogun State in South West Nigeria. As of 2005, Abeokuta and the surrounding area had a population of 593,140.[9] The city is known for its traditional style of hand-woven cotton cloth known as “adire” which is dyed with locally produced indigo. The hospital has a tripartite mandate of training and research, service delivery. It also serves as a referral center for primary and secondary public health institutions as well as missionary and private hospitals in Ogun State and neighboring South Western States of Nigeria. The Family Medicine of the Hospital comprises the general outpatient clinic (GOPC), corporate clinic (COOP), and National Health Insurance Scheme Clinic (NHIS) which serve as primary care clinic of the hospital. Family physicians and resident doctors in family medicine are involved in providing care to patients with hypertension at the family medicine clinics.
Study design
This study was a hospital-based, cross-sectional descriptive study conducted on 360 adults aged 18 and above with essential hypertension that attended the GOPC, COOP, and NHIS clinics of the hospital between May and July 2013. The estimated population per year based on the number of adult patients with essential hypertension (cases) that attended the three clinics in 2011 was 2982. The GOPC, NHIS, and COOP clinics had 1502 (50.4%), 836 (28.0%), and 644 (21.6%) attendees, respectively.
Inclusion criteria
Patients aged 18 years and above with essential hypertension
Patients with essential hypertension who had been on outpatient treatment for hypertension in the clinic for at least 1 year.
Exclusion criteria
Patients with secondary hypertension
Patients with major psychiatric illness
Patients with severe illness which make it difficult to follow the study protocol.
Sample size determination
The sample size (n) was calculated using the formula[10] n = z2pq/d2. At 95% confidence interval (CI) and a precision level of 5%, z = 1.96 and d = 0.05. The proportion of hypertensive patients with controlled BP (p) was 39% from the previous study.[11] Therefore, P = 0.39 and q = 1 − 0.39 = 0.61. Then, (n) = 1.962 × 0.39 × 0.61/0.052 = 365.6.
Since the number of patients with essential hypertension (N) that attended the three clinics in 2011 was 2982 (<10,000), the sample size was adjusted by the formula[10] nf = n/(1 + n/N). Thus, nf = 365.6/(1 + 365.6/2982) = 325.7 which is approximately 326.
The minimum sample size was 326. However, 10% of the total sample size was added to the minimum sample size to improve the power of the study. This gave a sample size of 360 respondents.
Sampling technique
Proportionate sampling was predetermined for each clinic (180 for GOPC, 100 for NHIS, and 80 for COOP) representing 50.4%, 28.0%, and 21.6%, respectively of 360 (the sample size). A systematic random sampling technique was utilized to select 360 hypertensive patients from the three clinics. The total number of adult patients with essential hypertension that attended the three clinics in 2011 was 2982. This translated to 960 estimated respondents in 4 months of data collection. The sampling interval “k” was calculated thus; k = N/n where n is the sample size (360), and N is the estimated population size within the study period (960) k = 960/360 = 2.67 ≈ 3. The first person was selected from the first three patients with essential hypertension arriving each clinic by simple random sampling (balloting) once at the outset of the study. Thereafter, every consenting third person was recruited until the required number (180 for GOPC, 100 for NHIS clinic, and 80 for COOP clinic) was achieved.
Data collection tool and process
The eligibility for the study was determined, and consent was taken. Data were collected by the principal investigator and two trained research assistants (resident doctors in the Department of Family Medicine of the hospital) through interview using a pretested questionnaire and a standardized tool for assessment of perceived family support tools (perceived family support scale by Procidano and Heller).[12] The pretesting of the questionnaire was conducted on 25 hypertensive patients who were selected haphazardly from the GOPC of Sacred Heart Hospital, Lantoro, Abeokuta and it lasted for 2 days. The pretesting was done to find out how the questionnaire would interact with the respondents and ensured that there were no ambiguities. The necessary adjustment was made after the pretest.
The pretested questionnaire consisted of three sections: Sociodemographic variables, socioeconomic data, and physical examination. It extracted information regarding patients’ demographic factors, level of education, and monthly earnings.
The subjects’ perceived family support was assessed using the Perceived Social Support Family Scale invented by Procidano and Heller.[12] It is a 20-item validated self-report scale which examines how persons perceive support, information, and response from their family. Respondents answer “yes,” “no,” or “I don’t know” to each item. Each “yes” answer to the questions contained in the perceived family support scale was scored one while other responses were scored 0. Items 3, 4, 16, 19, and 20 were reversed scored (a “no” response is scored as +1). Summated scores were used to arrive at a family support score, and the possible ranges of scores are 0–20. The score was categorized as strong family support (≥11), weak family support (7–10), and no family support (≤6). It has acceptable validity and reliability. Internal consistency of the scale is 0.88 while the short-term test-retest reliability is 0.83.[12] Yoruba version of the original instrument was administered to respondents who did not understand English after it had been translated and back-translated.
BP measurement for each subject was taken in the clinic using an Accoson® mercury sphygmomanometer after subjects had rested for 5 min. Systolic BP and diastolic BP (SBP and DBP) were measured at Korotkoff Phases I and V, respectively.[13] The average of two BPs taken in the sitting position at intervals of 2 min was added to two previous BP readings in the last two visits within the last 6 months from the patients’ record. The average of the three BP readings was used as an indication of the level of control.[14] BP ≥140/90 mmHg in nondiabetic and ≥130/80 mmHg in diabetic were classified as uncontrolled.[7]
Statistical analysis
Data were entered into the Statistical Package for Social Sciences (SPSS) version 17.0 program (SPSS Inc., Chicago, IL). Continuous variables were summarized as mean and standard deviation while categorical variables were summarized as percentages. BP control was the main outcome (dependent) variable while sociodemographic characteristics and perceived family support score were the independent variables. Chi-squared test was used to determine the association between BP control and the various independent variables. The level of significance was set at a P ≤ 0.05 and CI of 95%. Logistic regression analysis was used to identify the independent predictors of BP control. The odds ratios (ORs) and 95% CI (95%) for the predictor variables were then calculated.
Ethical consideration
Ethical approval was obtained from the Ethics Committee of the Hospital. Informed consent was also obtained from the respondents included in the study.
Results
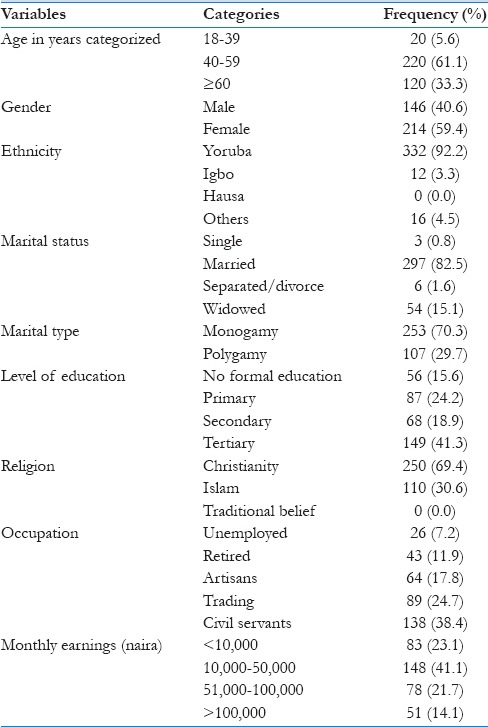
A total of 360 hypertensive subjects were recruited from the three clinics into the study over the 4 months period. The age range of the respondents was 35–84 years. The overall mean age was 55.4 ± 10.5. There were more female (n = 214 [59.4%]) than male (n = 146 [40.6%]) respondents with male: female ratio of 1:1.5. The mean age was comparable between male (55.4 ± 11.3 years) and female respondents (55.5 ± 9.9 years). Most of the respondents were middle-aged (n = 220 [61.1%]). Majority of the respondents (n = 297 [82.5%]) were married [Table 1].
Table 1.
Sociodemographic characteristics of the patients
One hundred and sixty-seven (46.4%) respondents achieved target BP (BP <140/90 mmHg in nondiabetics and BP <130/80 mmHg in diabetics) while this was not achieved in 193 (53.6%) respondents [Figure 1].
Figure 1.
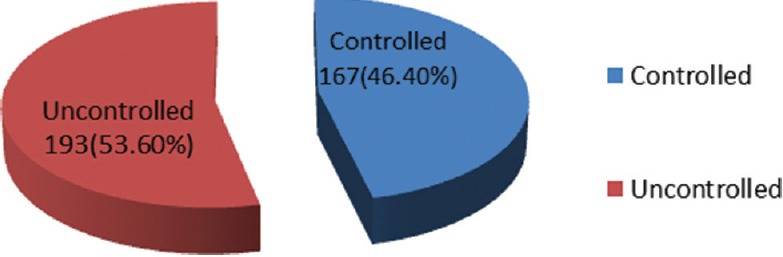
Pattern of blood pressure control among respondents
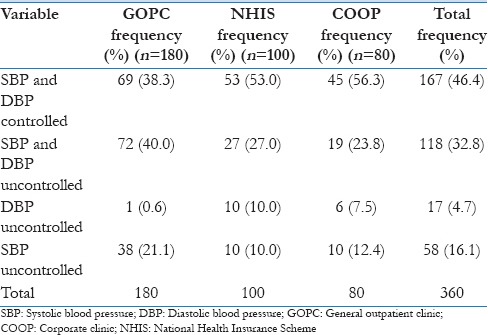
The number of respondents who achieved BP control (SBP and DBP within normal range) in GOPC, NHIS, and COOP clinics was 69 (38.3%), 53 (53.0%), and 45 (56.3%), respectively [Table 2].
Table 2.
Comparison of blood pressure control in the three clinics
Most of the respondents (n = 286 [79.4%]) reported strong perceived family support. The proportions of respondents with weak support and no support were 50 (13.9%) and 24 (6.7%), respectively [Figure 2].
Figure 2.
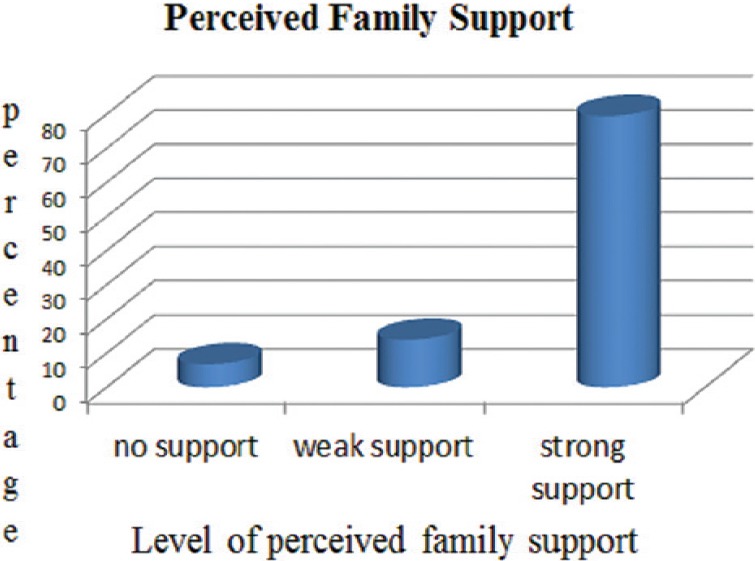
Proportion of respondent in different level of perceived family support
Chi-square analysis showed that BP control was significantly associated with gender (χ2 = 5.332, P = 0.021) and perceived family support (χ2 = 25.736, P = 0.000) [Table 3].
Table 3.
Relationship between blood pressure control and sociodemographic factors/perceived family support of respondents
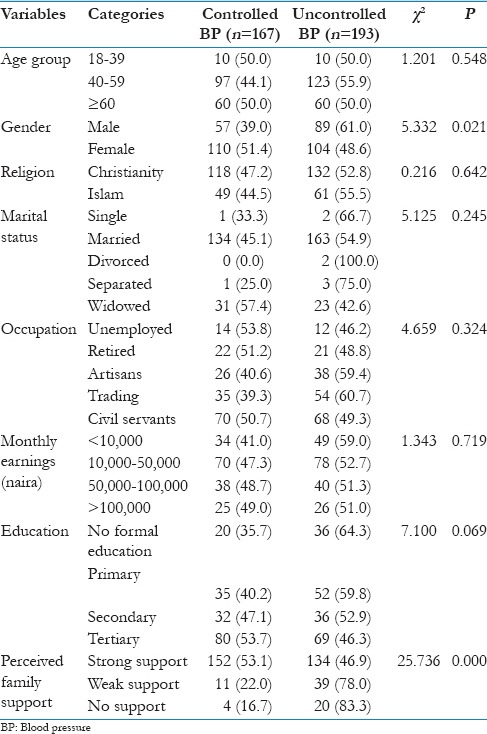
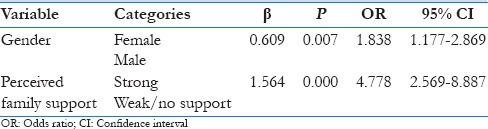
Logistic regression further showed that female respondents were approximately two times more likely to have controlled BP than male respondents (P = 0.007, OR = 1.838, 95% CI = 1.177–2.869). Respondents with strong perceived family support were approximately five times more likely to have controlled BP than respondents without strong perceived family support (P = 0.000, OR = 4.778, 95% CI = 2.569–8.887) [Table 4].
Table 4.
Logistic regression analysis of significant factors associated with blood pressure control
Discussion
The demographic distribution of respondents in this study is characteristic of a middle-aged population (61.1%). This observation is in agreement with findings from most studies on hypertension.[15,16,17] This finding is however not surprising because most chronic medical conditions begin to creep in at the middle-age period. The decline in endogenous estrogen production after age 40 years and consequent atherosclerosis contributes to this occurrence in women.[2]
The female preponderance (59.4%), in this study, is in keeping with the previous reports of more female compared with their male counterparts in most hospital-based studies on hypertension.[16,17] The higher number of hypertensive female participants in the present study may suggest that more females attended the family medicine clinics, rather than an increased prevalence of hypertension in females compared to males. A number of reasons may be liable for this observation. First, in Traditional African Society, males are the major bread winners for their families and lacked the time to get to the hospital for screening or follow-up. Second, women seem to have better health seeking behavior for chronic diseases than men.[18] It is also possible that women are more likely to have their asymptomatic hypertension detected through BP check due to more contact with health care facilities during their reproductive years.
A study in the South West Nigeria however observed a strong male preponderance (74.1%) among hypertensive workers attending the medical center of a research institute.[6] The observed difference perhaps reflects the gender distribution of the workers attending the medical center of this research institute.
The finding of a significant proportion of respondents having a strong perceived family support corroborates the fact that Africans has a naturally rich social support network. The reasons for this can be explained by the extended family system in our environment. It is known that in family-centered societies, people tend to gain major support from family as noted in the previous research works.[19,20] Furthermore, 82.5% of the respondents were married. These marital characteristics are thought to hold significant potential for affecting an individual perception of family support, and therefore be inclined to report better family support perceptions than their unmarried counterparts.[21]
This study still found that less than half of the respondents (46.4%) had controlled BP. Suboptimal BP control seems to be a prevalent finding in most parts of the world, especially in developing countries.[15,22,23] Suboptimal control rates of 36% in Ibadan, South West Nigeria,[6] 24.2% in Portharcourt, South-South Nigeria[16] and 12.4% in Zaria, Northern Nigeria[24] have been reported.
The BP control rate of 46.4% is high when compared with the rates reported in the former local studies. The reason for this could be explained by the study population. All studies mentioned above recruited respondents from the cardiology clinic and the observed difference could be attributed to the fact that patients with complicated hypertension and thus, difficult BP control are likely to be seen in this clinic when compared with primary care clinics. Another possible explanation for the relatively high-control rate, in this study, could be attributed to the fact that patients with secondary hypertension in whom achieving target BP goal could be challenging were excluded from this study.
The BP control rate among patients recruited from GOPC was low (38.3%) when compared with the NHIS clinic (53.0%) and COOP clinic (56.3%). The reasons for this may be due to the highly subsidized drugs that NHIS clinic and some COOP clinic respondents get through health insurance. Furthermore, a hypertensive member of the staff of the hospital who are expected to be health conscious are seen at the corporate clinic. Hypertensive patients with access to health insurance had been shown to have better medication adherence and BP control.[25]
A statististically significant proportion of females compared to males achieved controlled BP (51.4% vs. 39.0%; P = 0.021), and this was confirmed by the multivariate analysis. Female respondents were approximately two times more likely to have their BP controlled than male respondents (OR = 1.838, 95% CI = 1.177–2.869). This agrees with the findings of most studies that investigated the influence of gender on BP control.[6,23,26] The likely explanations for better control in women are multiple. First, the likelihood of having BP checked is higher in women than men due to more contact with health facilities during reproductive years.[18] Second, women accept the diagnosis of hypertension readily even in the absence of symptoms and acknowledge the need to stay healthy to care for their families.[27]
Control of BP was however shown to be better in men compared with women in other reports[28,29] probably because these studies have largely considered older people in whom controlled BP has been shown to be more likely in men compared with women.[29]
This study showed that strong perceived family support was an independent predictor of controlled BP and that respondents with strong perceived family support were approximately five times more likely to have controlled BP than respondents without strong perceived family support (OR = 4.778, 95% CI = 2.569–8.887). A large body of research in developed countries has shown a strong positive association between level of family support and BP control.[7,8,30,31,32] There is a paucity of studies on the relationship between family support and BP control among hypertensive patients in Nigeria and Africa. Studies on family support in Nigeria have focussed on chronic diseases such as diabetes mellitus[21] and depression.[33] Results from these studies[21,33] also indicated a positive relationship between family support and health outcomes.
Possible explanations attributed to the positive relationship between family support and BP control are several. First, the reduced level of family support could lead to the adoption of fewer habits related with a healthy lifestyle.[34] Second, a good social network can attenuate the cardiovascular response in a situation of stress, thereby avoiding the accompanying increase in BP.[35] It has also been reported that those who had support from friends or family members had better compliance with treatment than those who did not.[30,36,37]
A study in Spain however failed to find a positive association between BP control and family support.[38] A number of reasons may be adduced for the observed difference. First, the population in the Spanish study comprised elderly only (60 years and above). Social isolation probably from the death of a partner at this stage of life can limit their receipt of social support, and this can cause an increase in BP. Second, while the former studies used a standardized tool[32] and focus group discussion[8,37] in assessing family support, the Spanish study[38] subjectively assessed the level of support using participants’ frequency of contact with a friend thus reducing its internal and external validity.
Family support is important in the long-term management of hypertension, which requires a life-long change in the lifestyle of the affected person. A strong perceived family support will improve their self-worth and motivation. It is plausible that a motivated hypertensive patient will adhere to therapeutic plans and therefore, achieve better BP control. It is essential that health care providers carry families of patients with hypertension along in their management to improve hypertensive patients’ function and treatment outcome.
The following limitations were considered in this study: The study relied on a questionnaire to elicit individual's perception of family supports. Opinions expressed by the respondents may be different from their actual experience. This might overestimates or underestimates their level of perceived family supports. Second, data from this study cannot address issues of the causal relationship between BP control and perceived family support as a result of the cross-sectional design of the study. Furthermore, some of the patients that were labeled to have primary hypertension might indeed have secondary hypertension. This could be avoided if facilities were readily available for extensive investigations.
Conclusions
It is concluded that the control of blood pressure among hypertensive patients is still sub-optimal in this practice setting, with the lowest control rate across the three clinics recorded at the GOPC. Majority of the respondents had ‘strong’ perceived family support. The independent predictors of controlled blood pressure were strong perceived family support and female gender.
It is recommended that health care providers must be sensitized on the need for aggressive treatment in patients who are likely to have poor blood pressure control. This includes those with poor perceived family support and male clients. More future community-based interventional studies in Nigeria that explore the influence of family support on the control of blood pressure are needed to give more insight into the topic.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We appreciate Mr. Ogunlana of the Department of Physiotherapy of our hospital for his technical support. Special thanks to all our colleagues in the Department of Family Medicine for their contributions during the preparation of this work. We also wish to express our gratitude to the Head of Department of Medical Records of our hospital.
References
- 1.Dennison-Himmelfarb C, Handler J, Lackland DT, LeFevre ML, MacKenzie TD, Ogedegbe O, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: Report from the panel members appointed to the Eighth Joint National Committee (JNC 8) JAMA. 2013;311:507–20. doi: 10.1001/jama.2013.284427. [DOI] [PubMed] [Google Scholar]
- 2.Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J. Global burden of hypertension: Analysis of worldwide data. Lancet. 2005;365:217–23. doi: 10.1016/S0140-6736(05)17741-1. [DOI] [PubMed] [Google Scholar]
- 3.Ekwunife OI, Aguwa CN. A meta-analysis of prevalence rate of hypertension in Nigerian populations. J Public Health Epidemiol. 2011;3:604–7. [Google Scholar]
- 4.Akpa MR, Agomuoh DI, Odia OJ. Drug compliance among hypertensive patients in Port Harcourt, Nigeria. Niger J Med. 2005;14:55–7. doi: 10.4314/njm.v14i1.37136. [DOI] [PubMed] [Google Scholar]
- 5.World Health Organization. Adherence to Long-Term Therapies: Evidence for Action. WHO/MNC/03.01; 2010. Geneva: World Health Organization; 2003. [Google Scholar]
- 6.Salako BL, Ajose FA, Lawani E. Blood pressure control in a population where antihypertensives are given free. East Afr Med J. 2003;80:529–31. doi: 10.4314/eamj.v80i10.8756. [DOI] [PubMed] [Google Scholar]
- 7.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr, et al. The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: The JNC 7 report. JAMA. 2003;289:2560–72. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 8.Costa Rdos S, Nogueira LT. Family support in the control of hypertension. Rev Lat Am Enfermagem. 2008;16:871–6. doi: 10.1590/s0104-11692008000500012. [DOI] [PubMed] [Google Scholar]
- 9.National Population Commission. National Population Census, 2006. National Population Commission. 2006 [Google Scholar]
- 10.Araoye MO, editor. Research Methodology with Statistics for Health and Social Sciences. 1st ed. Ilorin: Nathadex Publishers; 2003. Subject selection: Sample size determination; pp. 117–8. [Google Scholar]
- 11.Alebiosu C, Raimi T, Ayodele O, Bassi P, Salako B, Aina OA, et al. The impact of knowledge, attitude, practice and beliefs of hypertensives on drug compliance. Cardiol Trop. 2003;29:39–42. [Google Scholar]
- 12.Procidano ME, Heller K. Measures of perceived social support from friends and from family: Three validation studies. Am J Community Psychol. 1983;11:1–24. doi: 10.1007/BF00898416. [DOI] [PubMed] [Google Scholar]
- 13.Pickering TG, Hall JE, Appel LJ, Balkner BE, Graves J, Hill MN, et al. Recommendations for blood pressure measurement in humans and experimental animals part 1: Blood pressure measurement in humans. A statement for professionals from the subcommittee of professional and public education of the American heart council on high blood pressure research. Hypertension. 2005;45:142–61. doi: 10.1161/01.HYP.0000150859.47929.8e. [DOI] [PubMed] [Google Scholar]
- 14.Alsairafi M, Alshamali K, Al-rashed A. Effect of physical activity on controlling blood pressure among hypertensive patients from Mishref area of Kuwait. Eur J Gen Med. 2010;7:377–84. [Google Scholar]
- 15.Osman EM, Suleiman I, Elzubair AG. Patients knowledge of hypertension and its control in Eastern Sudan. East Afr Med J. 2007;84:324–8. doi: 10.4314/eamj.v84i7.9587. [DOI] [PubMed] [Google Scholar]
- 16.Akpa MR, Alasia D, Emem-Chioma P. An appraisal of hospital based blood pressure control in Port Harcourt, Nigeria. Niger Health J. 2008;8:27–30. [Google Scholar]
- 17.Amira C, Okubadejo N. Antihypertensive pharmacotherapy in a developing economy: Pattern, acquisition costs and conformity to international guidelines in a tertiary-care setting. J Hum Hypertens. 2006;20:894–7. doi: 10.1038/sj.jhh.1002080. [DOI] [PubMed] [Google Scholar]
- 18.Ong KL, Tso AW, Lam KS, Cheung BM. Gender difference in blood pressure control and cardiovascular risk factors in Americans with diagnosed hypertension. Hypertension. 2008;51:1142–8. doi: 10.1161/HYPERTENSIONAHA.107.105205. [DOI] [PubMed] [Google Scholar]
- 19.Armstrong N. USA: UNC Asheville; 2013. The importance of extended families in the African American community: A qualitative analysis using social learning theory: Proceedings of the National Conference on Undergraduate Research (NCUR), 29-31 March 2012, Weber State University, Ogden, Utah; pp. 1322–7. [Google Scholar]
- 20.Okumagba PO. Family support for the elderly in delta state of Nigeria. Stud Home Community Sci. 2011;5:21–7. [Google Scholar]
- 21.Adetunji A, Ladipo M, Irabor A, Adeleye J. Perceived familysupport and blood glucose control in type 2 diabetes. Diabetes. 2007:18–9. [Google Scholar]
- 22.Bramlage P, Böhm M, Volpe M, Khan BV, Paar WD, Tebbe U, et al. A global perspective on blood pressure treatment and control in a referred cohort of hypertensive patients. J Clin Hypertens (Greenwich) 2010;12:666–77. doi: 10.1111/j.1751-7176.2010.00322.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kayima J, Wanyenze RK, Katamba A, Leontsini E, Nuwaha F. Hypertension awareness, treatment and control in Africa: A systematic review. BMC Cardiovasc Disord. 2013;13:54. doi: 10.1186/1471-2261-13-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Oyati AI, Orogade AA, Danbauchi SS, Azuh PC. Awareness, treatment and control of hypertension among hypertensives in Zaria. J Med Trop. 2011;13:139–44. [Google Scholar]
- 25.Hendriks ME, Wit FW, Akande TM, Kramer B, Osagbemi GK, Tanoviæ Z, et al. Effect of health insurance and facility quality improvement on blood pressure in adults with hypertension in Nigeria: A population-based study. JAMA Intern Med. 2014;174:555–63. doi: 10.1001/jamainternmed.2013.14458. [DOI] [PubMed] [Google Scholar]
- 26.van den Berg N, Meinke-Franze C, Fiss T, Baumeister SE, Hoffmann W. Prevalence and determinants of controlled hypertension in a German population cohort. BMC Public Health. 2013;13:594. doi: 10.1186/1471-2458-13-594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Addo J, Smeeth L, Leon DA. Hypertension in sub-saharan Africa: A systematic review. Hypertension. 2007;50:1012–8. doi: 10.1161/HYPERTENSIONAHA.107.093336. [DOI] [PubMed] [Google Scholar]
- 28.Thoenes M, Neuberger HR, Volpe M, Khan BV, Kirch W, Böhm M. Antihypertensive drug therapy and blood pressure control in men and women: An international perspective. J Hum Hypertens. 2010;24:336–44. doi: 10.1038/jhh.2009.76. [DOI] [PubMed] [Google Scholar]
- 29.Keyhani S, Scobie JV, Hebert PL, McLaughlin MA. Gender disparities in blood pressure control and cardiovascular care in a national sample of ambulatory care visits. Hypertension. 2008;51:1149–55. doi: 10.1161/HYPERTENSIONAHA.107.107342. [DOI] [PubMed] [Google Scholar]
- 30.Osamor PE, Owumi BE. Factors associated with treatment compliance in hypertension in southwest Nigeria. J Health Popul Nutr. 2011;29:619–28. doi: 10.3329/jhpn.v29i6.9899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tobe SW, Kiss A, Szalai JP, Perkins N, Tsigoulis M, Baker B. Impact of job and marital strain on ambulatory blood pressure results from the double exposure study. Am J Hypertens. 2005;18:1046–51. doi: 10.1016/j.amjhyper.2005.03.734. [DOI] [PubMed] [Google Scholar]
- 32.Brittain K, Taylor JY, Wu CY. Family adaptability and cohesion and high blood pressure among urban African American women. J Nurse Pract. 2010;6:786–793. doi: 10.1016/j.nurpra.2010.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Olanrewaju A, Akintunde A, Femi F, Ibrahim B, Olugbenga A. Pattern of depression and family support in a Nigerian family practice population. Internet J Fam Pract. 2008;6:1–10. [Google Scholar]
- 34.Chandola T, Head J, Bartley M. Socio-demographic predictors of quitting smoking: How important are household factors? Addiction. 2004;99:770–7. doi: 10.1111/j.1360-0443.2004.00756.x. [DOI] [PubMed] [Google Scholar]
- 35.Rosland AM. Sharing the Care: The Role of Family in Chronic Illness. Oakland: California Healthcare Foundation; 2009. [Last accessed on 2009 Aug 16]. Available from: http://www.chcf.org/documents/chronicdisease/FamilyInvolvement_Final.pdf . [Google Scholar]
- 36.Fina Lubaki JP, Mabuza L, Malete N, Maduna P, Ndimande JV. Reasons for non compliance among patients with hypertension at Vanga Hospital, Bandundu Province, Democratic Republic of Congo: A qualitative study. Afr J Prim Health Care Fam Med. 2009;1:1–5. [Google Scholar]
- 37.Flynn SJ, Ameling JM, Hill-Briggs F, Wolff JL, Bone LR, Levine DM, et al. Facilitators and barriers to hypertension self-management in urban African Americans: Perspectives of patients and family members. Patient Prefer Adherence. 2013;7:741–9. doi: 10.2147/PPA.S46517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Redondo-Sendino A, Guallar-Castillón P, Banegas JR, Rodríguez-Artalejo F. Relationship between social network and hypertension in older people in Spain. Rev Esp Cardiol. 2005;58:1294–301. [PubMed] [Google Scholar]


