Abstract
Background:
Data on the prehospital interventions received by critically ill children at arrival to Paediatric Emergency Services (PES) is limited in developing countries. This study aims to describe the pre-hospital care scenario, transport and their impact on outcome in non-traumatic, acutely ill children presenting in PES with agonal breathing.
Methods:
Prospective observational study done on children aged below 15 years arriving in PES with agonal breathing due to non-trauma related causes.
Results:
Out of 75 children studied, 69% were infants. The duration of illness among 65% of them (75) was less than 3 days. Majority of them (81%) had received treatment prior to arrival. Government sector physicians (72%), half of them (51%) being pediatricians were the major treating doctors. 37% of the children had arrived to the Emergency in an ambulance. Cardiopulmonary Resuscitation (CPR) was given to 27% on arrival in PES. Other interventions included fluid boluses to correct shock (92%) and inotrope infusion (56%). Sepsis (24%) and pneumonia (24%) were the most common diagnoses. Out of 75, 57 (76%) children who were stabilized and shifted to PICU and among them 27 (47%) survived to discharge. Normal blood pressure (p=0.0410) and non-requirement of CPR (0.0047) and inotropic infusion (0.0459) in PES were associated with a higher chance of survival.
Conclusion:
36% (27/75) of children who arrived to our PES with agonal breathing survived to hospital discharge. Survival was significantly better among those who did not need CPR.
Keywords: Agonal breathing, children, intubation, pediatric emergency service, resuscitation
Introduction
Most cardiac arrests in infants and children result from progressive respiratory failure, shock, or both. Cardiac arrests occurring without warning are less common among children.[1] Life-threatening conditions leading to cardiorespiratory failure and arrest among children are more likely to commence outside the hospital. Hence, interventions to provide adequate oxygenation and correction of shock may have to be instituted in the prehospital setting to save life.[1] The provision of an effective prehospital emergency medical service (EMS) is an important element in reducing childhood mortality.[2] It has been shown to improve outcomes among adult trauma victims.[3]
In countries with established pediatric EMS, the health-care personnel are trained for interventions such as bag-valve-mask ventilation, intravenous/intraosseous access placement, and provision of life-saving medications, endotracheal intubation, and defibrillation if needed.[4,5,6] In developing countries, due to the varied topography, financial constraints and lack of appropriate health infrastructure assistance by a time-sensitive emergency medical service (EMS) are often not provided to critically ill children.
Ambulance services run by government, police, fire brigades, hospitals, and private agencies are increasingly available, but there is little coordination among them. These ambulances are often just about transport vehicles equipped with only a bed and an oxygen supply, manned by personnel staff with minimal or no medical training. Due to lack of any categorization of hospitals, sick children are often taken to the nearest facility, to treat that particular emergency. A nation led agency to coordinate various components of a prehospital care system and mechanisms for accreditation of services and professionals are the need of the hour.
In our setting, it was not uncommon for critically ill children to be brought to the pediatric emergency service (PES) with agonal breathing. Data on prehospital care in children with impending cardiorespiratory arrest from rural/semi-urban areas in transitional countries are limited. This study attempted to look into the prehospital care settings, clinical profile, transport, and treatment required on arrival along with the final outcome of the sick nontraumatic children presenting in PES in agonal breathing.
Methods
This prospective observational cohort study was conducted in PES of a large tertiary care center in South India over a 1-year period from June 2010 to May 2011. The PES has 21 beds, 8 of which are dedicated for resuscitation and admitting around 25,000 children below 15 years annually including newborns. Children with trauma are attended to in the Adult Accident and Emergency Department as per the hospital's policy.
All children arriving in PES are received and triaged by the triage nurse. If any of the airway, breathing, circulation components were unstable, stabilization was carried out according to the guidelines given by the pediatric advanced life support (PALS) course including cardiopulmonary resuscitation (CPR). Isotonic fluid boluses and inotropic infusions were given to correct shock. After stabilization, patients are shifted to the Pediatric Intensive Care Unit (PICU) for further management.
All the children who were included in the study were closely followed up in PES, PICU, and the pediatric wards until the time of their discharge from the hospital. The information related to demography, prehospital interventions, clinical profile, emergency room interventions, and outcomes was carefully documented in a pro forma for final analysis.
Parent's consent was obtained to use the data for analysis, and the study was carried out under the supervision of the Ethics Board.
The instruments used were as follows:
Questionnaire
Referral letters
Telephonic interview
Hospital records.
The outcomes that came about in these children were death in the PES/PICU, discharge home at parental request against medical advice, or survival to hospital discharge.
The details from the pro forma were entered into a Microsoft Excel® sheet and analyzed using the Statistical Package for the Social Sciences (IBM, New York, United States). Demographic variables were described using mean, standard deviation, and proportions as appropriate. Risk factors and final outcome were evaluated by Chi-square test to calculate P values.
Results
Children attended
Seventy-five children who arrived with agonal breathing were recruited for the study. Their demography and the clinical characteristics are shown in Table 1. Among them, 69% of them were infants, one-third being <2 months of age. The mean age was 24.67 ± 40.34 months. A greater proportion of the patients (60%) were boys. The duration of illness was ≤3 days in 65%, 4–7 days in 23%, and >7 days in 12% of the children. Only 19% came directly to the PES; 81% of them had received medical treatment prior to arrival.
Table 1.
Demography, clinical profile, prehospital care, and transport of children (n=75)
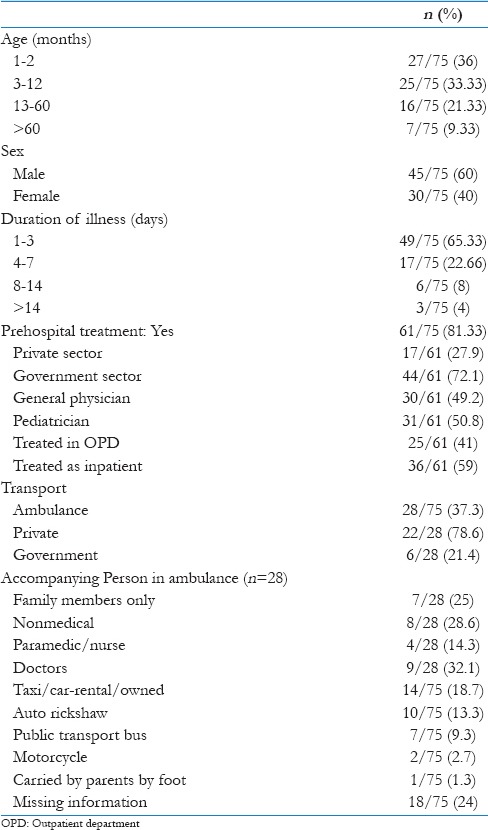
Government sector doctors were the major contributors (72%) for treating our sick children prior to their arrival to our PES. Among them, 51% were pediatricians and 49% were nonspecialist medical doctors. Thirty-six (59%) had been hospitalized prior to their arrival to our PES.
Information related to the details of transport was available in 57 (76%) children. While 28 (37%) children availed ambulance facility (private [22, 79%] and government [6, 21%]), a significant proportion came by taxi/car (14 [19%]), auto-rickshaws (10 [13%]), public bus (7 [9%]), and even two-wheelers (2 [3%]). One child was carried by the parents to the PES by foot. Among the 28 children who were transported by ambulance, a medical doctor had accompanied the patient in 9 (32%), paramedic/nurse in 4 (14%), and nonmedical personnel without basic life support (BLS) training in 8 (29%) children. The remaining 7 (25%) were transported accompanied only by members of their family.
The vital signs on arrival, the emergency room interventions, and critical events during stabilization of the children are shown in Table 2. All the 75 children who arrived with agonal breaths were intubated in PES and 20 (27%) received CPR. In 25 (33%) children, there was no recordable blood pressure. It was low for age in 41 (55%) and normal for age in 9 (12%) children. For stabilization, 69 (92%) children were given fluid resuscitation and 42 (56%) were commenced on inotropic infusion in the PES.
Table 2.
Vitals and initial treatment of sick children at arrival to pediatric emergency service (n=75)
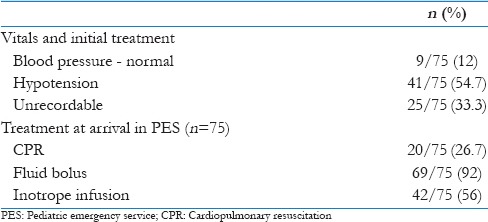
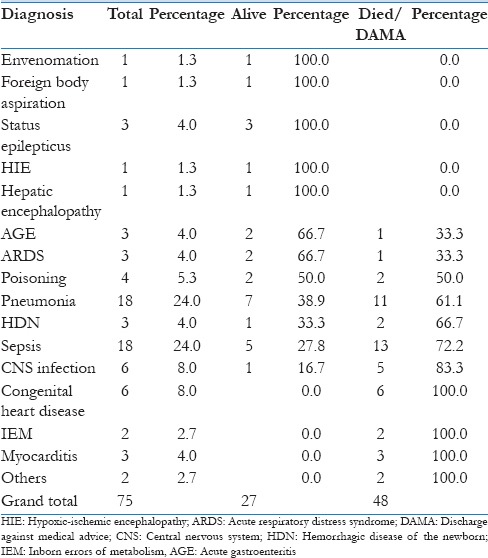
Table 3 shows the final diagnoses made in the group. Sepsis (18, 24%) and pneumonia (18, 24%) were the most common diagnoses, followed by central nervous system (CNS) infection (6, 8%), congenital heart disease (6, 8%), and poisoning (4, 5%) in that order. Other diagnoses were neonatal hypoxic ischemic encephalopathy (1, 1.3%), acute gastroenteritis (3, 4%), acute lung injury 3 (4%), inborn errors of metabolism (2, 3%), myocarditis (3, 4%), envenomation (1, 1.3%), and foreign body aspiration (1, 1.3%). There were 3 (4%) children with late hemorrhagic disease of the newborn (HDN) due to Vitamin K deficiency which continues to be seen in our geographic area and had all presented with intracranial bleed.
Table 3.
Final diagnosis and outcome (n=75)
Outcomes
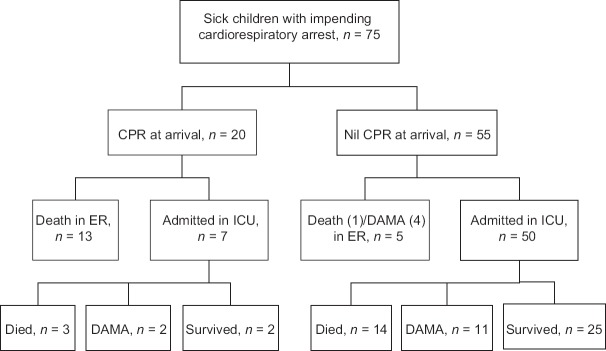
Twenty received CPR in PES of which 2 (10%) survived to discharge from hospital, whereas from among the remaining 55 children who did not require CPR at arrival in PES, 25 (45%) survived to hospital discharge, P = 0.0047 [Figures 1, 2 and Table 4].
Figure 1.
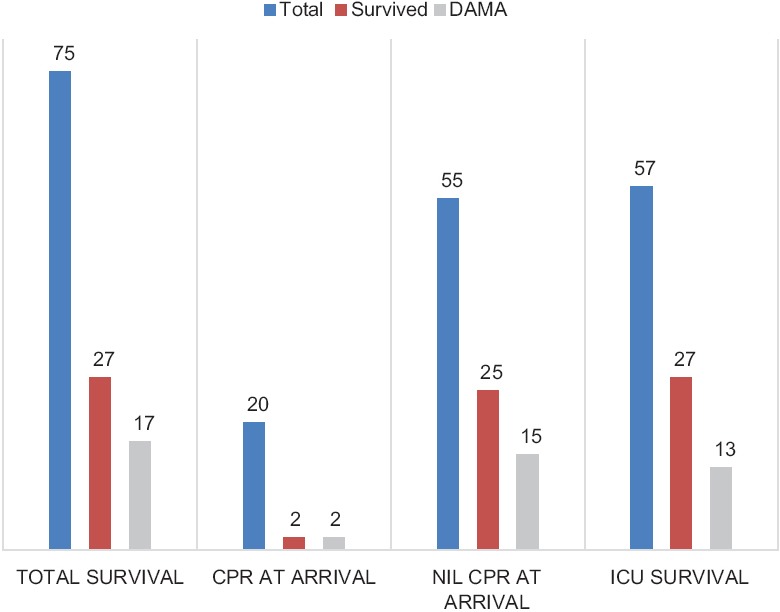
Survival among the children arriving at the pediatric emergency service with agonal breathing
Figure 2.
Outcome of 75 children arriving at the pediatric emergency service with agonal breathing
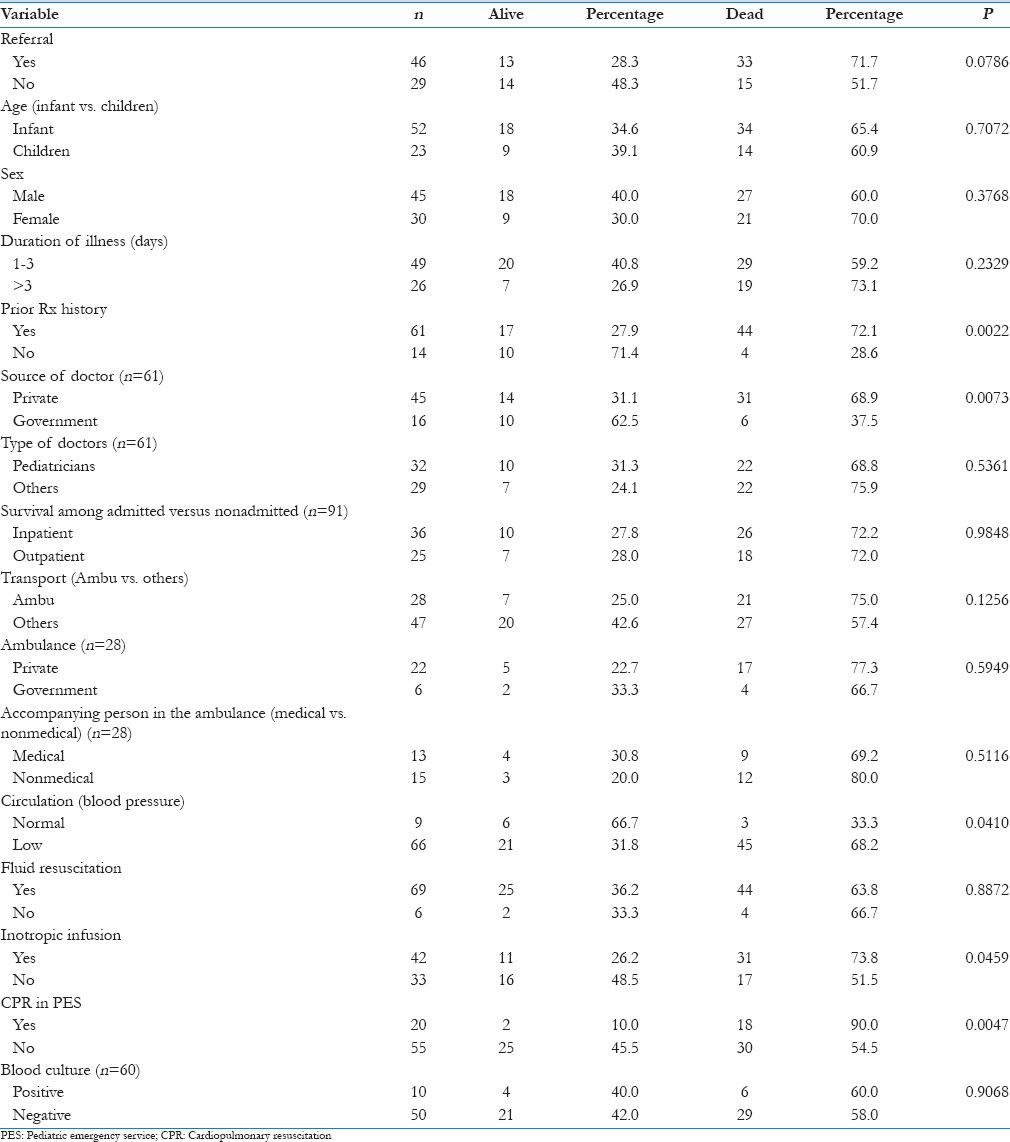
Table 4.
Association of various factors with survival to hospital discharge (n=75)
The final outcome of the 75 children in relation to their diagnoses is shown in Table 3. Survival in patients with acute gastroenteritis and acute respiratory distress syndrome was 67% whereas among those with poisoning 50% survived. Of the 18 children with pneumonia, 7 (39%) survived. Survival was low among children with late HDN (25%), sepsis (24%), CNS infection (17%), and congenital heart disease (8%). Survival among the single child each with envenomation, foreign body aspiration, hepatic encephalopathy, and newborn with birth asphyxia and the three children with status epilepticus was 100%.
Table 4 shows the outcome in relation to the variables of demography, clinical features, prehospital care, transport, and treatment in PES. It shows that the survival was significantly higher among those children who had normal blood pressure at arrival (P = 0.041) and who did not require treatment with inotropic infusion (P = 0.045) or CPR (P = 0.004) in PES. Prior treatment, history adversely affected the survival (P = 0.002) but not the type of doctor (P = 0.536). Treatment as inpatients or outpatients also did not affect the outcome (P = 0.984).
Discussion
Our data provide insight into the accessibility of health care facilities for families of sick children from rural/semi-urban parts of Southern India. Agonal breathing is the respiratory pattern prior to terminal apnea and an abnormal brainstem reflex.[7] It is easy to recognize and usually results in terminal apnea unless resuscitated. However, elective intubation and immediate transfer of patients are not a common practice among primary health-care providers.
Large portions (69%) of the study population were infants. The duration of illness was below 72 h in 65% of these children giving their families little time to think and prepare access toward medical care.
Despite the difficulties, 81% of the children received treatment prior to presenting in the PES, 51% from pediatricians and 59% had been in patients. One-third had been transported by ambulance, accompanied by doctors (32%) or paramedics/nurses (14%). None of these factors affected the outcome of these children favorably. This reflects that outcomes cannot be different unless an organized and trained emergency medical system is available at the secondary hospital level to provide time-appropriate care and safely transfer the critically ill child to a higher center for continued care.
As was expected, sepsis (24%) and pneumonia (24%), the important causes of infant mortality, were the most common underlying conditions that showed low survival (28% and 39%, respectively). Among the remaining disease conditions, acute gastroenteritis (AGE) had a survival of 67%. According to the United Nations Children's Fund, the infant mortality rate (IMR) decreased from 44 deaths for every 1000 live births in 2011 to 42 deaths for every 1000 live in 2013 in India. One of the important causes for this plateauing in the IMR is lack of a robust prehospital care in rural and semi-urban areas.[8]
Survival to hospital discharge following prehospital cardiac arrest in children is low, with the reported percentages of 2–9%.[9,10,11,12,13] Even those children who arrive at the hospital pulseless or apneic have poor outcome.[14,15,16] When encountered with children who arrive in the hospital with agonal breathing, emergency and intensive care physicians are often at a dilemma whether to resuscitate or not as the outcome of these children is uncertain. Our experience has shown that 36% of the 75 children who arrived agonal breathing had survived to discharge from hospital. Clearly, the decision to “not to treat” should be taken cautiously in the emergency room setting even within the constraints of resource limitations after carefully considering various factors that might not be known immediately on arrival.
The only factor that favored survival was normal blood pressure at arrival (P = 0.041). Other factors that significantly favored survival to hospital discharge were not requiring chest compression, normal blood pressure, not requiring inotropic infusion at arrival. These highlight the importance of simple, timely interventions such as provision of oxygen and correction of shock for improving outcomes from a critical condition.
This study was limited to only medical emergencies as the unit did not receive children with trauma, and being a tertiary care center, the results of this study may not be applicable to remote environments or even to rural health system.
Our study highlights the need for early provision of oxygenation, fluid resuscitation, and monitoring without which even the best care will only be a futile exercise. Although pediatric emergencies may not be common occurrence in primary-care setting, numerous studies have shown that a significant number of children present to primary-care physicians (PCPs) office with variety of urgent or emergency problems.[17] PCPs play a vital role in the recognition of emergencies, providing life support, and supervised transport to a center with emergency and intensive care services and to educate families about prevention.[18] As PCPs have a critical role to advocate high-quality care to their first contact, consequences of being unprepared are serious.[19] Various studies have shown that PCPs trained with BLS, PALS, likely to use resuscitation equipment in their office practice and their training will improve the chance of survival of sick children, especially the chance of survival among the children who experience cardiac arrest.[20] Our study underscores the need for such training for health-care professionals so that acutely ill children arriving in the ER in a pulseless or apneic state which is obviously associated with a poor outcome can be prevented.
Further research exploring the feasibility and safety of endotracheal intubation by the referring center/doctor before transferring as against transfer with bag and mask ventilation on patient outcomes are required.
Conclusion
A significant proportion of the children who arrived with agonal breaths to our PES survived to hospital discharge. Survival was significantly better if children reached the PES before cardiac arrest. As sepsis and pneumonia were the most common diagnoses encountered in our study, giving the first dose of antibiotic might be an appropriate intervention prior to transferring the sick children to a higher center. Sick children should be transported by ambulance trained medical/paramedical personnel, along with provisions to monitor oxygen saturation and vital signs during their transport to a higher center.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We are grateful to Dr. Selvaraj, Senior Consultant, in the Department of Biostatistics for helping us in analyzing the statistical data.
References
- 1.Advanced Life Support Group. Pre Hospital Pediatric Life Support. London: BMJ Publishing Group; 1999. pp. 4–5. 8, 21-3. [Google Scholar]
- 2.Jewkes F. Prehospital emergency care for children. Arch Dis Child. 2001;84:103–5. doi: 10.1136/adc.84.2.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Seid T, Ramaiah R, Grabinsky A. Pre-hospital care of pediatric patients with trauma. Int J Crit Illn Inj Sci. 2012;2:114–20. doi: 10.4103/2229-5151.100887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Stiell IG, Wells GA, Field BJ, Spaite DW, De Maio VJ, Ward R, et al. Improved out-of-hospital cardiac arrest survival through the inexpensive optimization of an existing defibrillation program: OPALS study phase II. Ontario prehospital advanced life support. JAMA. 1999;281:1175–81. doi: 10.1001/jama.281.13.1175. [DOI] [PubMed] [Google Scholar]
- 5.Stiell IG, Wells GA, Field B, Spaite DW, Nesbitt LP, De Maio VJ, et al. Advanced cardiac life support in out-of-hospital cardiac arrest. N Engl J Med. 2004;351:647–56. doi: 10.1056/NEJMoa040325. [DOI] [PubMed] [Google Scholar]
- 6.Gausche M, Lewis RJ, Stratton SJ, Haynes BE, Gunter CS, Goodrich SM, et al. Effect of out-of-hospital pediatric endotracheal intubation on survival and neurological outcome: A controlled clinical trial. JAMA. 2000;283:783–90. doi: 10.1001/jama.283.6.783. [DOI] [PubMed] [Google Scholar]
- 7.Perkin RM, Resnik DB. The agony of agonal respiration: Is the last gasp necessary? J Med Ethics. 2002;28:164–9. doi: 10.1136/jme.28.3.164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Moore B, Sapien R Committee on Pediatric Emergency Medicine. The role of the pediatrician in rural emergency medical services for children. Pediatrics. 2012;130:978–82. doi: 10.1542/peds.2012-2547. [DOI] [PubMed] [Google Scholar]
- 9.Young KD, Gausche-Hill M, McClung CD, Lewis RJ. A prospective, population-based study of the epidemiology and outcome of out-of-hospital pediatric cardiopulmonary arrest. Pediatrics. 2004;114:157–64. doi: 10.1542/peds.114.1.157. [DOI] [PubMed] [Google Scholar]
- 10.Atkins DL, Everson-Stewart S, Sears GK, Daya M, Osmond MH, Warden CR, et al. Epidemiology and outcomes from out-of-hospital cardiac arrest in children: The resuscitation outcomes consortium epistry-cardiac arrest. Circulation. 2009;119:1484–91. doi: 10.1161/CIRCULATIONAHA.108.802678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gerein RB, Osmond MH, Stiell IG, Nesbitt LP, Burns S OPALS Study Group. What are the etiology and epidemiology of out-of-hospital pediatric cardiopulmonary arrest in Ontario, Canada? Acad Emerg Med. 2006;13:653–8. doi: 10.1197/j.aem.2005.12.025. [DOI] [PubMed] [Google Scholar]
- 12.Kuisma M, Suominen P, Korpela R. Paediatric out-of-hospital cardiac arrests – Epidemiology and outcome. Resuscitation. 1995;30:141–50. doi: 10.1016/0300-9572(95)00888-z. [DOI] [PubMed] [Google Scholar]
- 13.Pitetti R, Glustein JZ, Bhende MS. Prehospital care and outcome of pediatric out-of-hospital cardiac arrest. Prehosp Emerg Care. 2002;6:283–90. doi: 10.1080/10903120290938300. [DOI] [PubMed] [Google Scholar]
- 14.O’Rourke PP. Outcome of children who are apneic and pulseless in the emergency room. Crit Care Med. 1986;14:466–8. [PubMed] [Google Scholar]
- 15.Schindler MB, Bohn D, Cox PN, McCrindle BW, Jarvis A, Edmonds J, et al. Outcome of out-of-hospital cardiac or respiratory arrest in children. N Engl J Med. 1996;335:1473–9. doi: 10.1056/NEJM199611143352001. [DOI] [PubMed] [Google Scholar]
- 16.Sirbaugh PE, Pepe PE, Shook JE, Kimball KT, Goldman MJ, Ward MA, et al. A prospective, population-based study of the demographics, epidemiology, management, and outcome of out-of-hospital pediatric cardiopulmonary arrest. Ann Emerg Med. 1999;33:174–84. doi: 10.1016/s0196-0644(99)70391-4. [DOI] [PubMed] [Google Scholar]
- 17.Schuman AJ. Be prepared: Equipping your office for medical emergencies. Contemp Pediatr. 1996;13:27–43. [Google Scholar]
- 18.Frush K American Academy of Pediatrics Committee on Pediatric Emergency Medicine. Preparation for emergencies in the offices of pediatricians and pediatric primary care providers. Pediatrics. 2007;120:200–12. doi: 10.1542/peds.2007-1109. [DOI] [PubMed] [Google Scholar]
- 19.Singer J, Ludwig S, editors. American Academy of Pediatrics, Committee on Pediatric Emergency Medicine. Your office as an emergency care site. Emergency Medical Services for Children: The Role of the Primary Care Provider. Elk Grove Village, IL: American Academy of Pediatrics; 1992. pp. 31–44. [Google Scholar]
- 20.Knapp JF, Pyles LA. American Academy of Pediatrics Committee on Pediatric Emergency Medicine. Role of pediatricians in advocating life support training courses for parents and the public. Pediatrics. 2004;114:1676. doi: 10.1542/peds.2004-2020. [DOI] [PubMed] [Google Scholar]