Abstract
Marijuana smoke can cause thermal injury, and since legalization and increased use of marijuana in our society, differentiating, diagnosing, and managing this condition have become mandatory. A case of a 28-year-old male with Quincke's disease secondary to marijuana inhalation is presented.
Keywords: Isolated uvular angioedema, marijuana, Quincke's disease
Introduction
Quincke's disease, or isolated uvular angioedema, was first described in 1882 and has since been a relatively rare form of angioedema of the upper airway.[1] Although it is typically caused by an immediate Type I hypersensitivity reaction, uvular edema can also be caused by trauma, thermal injury, and infections.[2] Smoking marijuana is the most common and efficient way of using Cannabis and has grown in popularity over the years. With the recent legalization of marijuana in several states of America, the healthcare practitioner must become aware of the potential complications of this drug. Typical complications include xerostomia, leukoedema, and an increased incidence of Candida albicans.[3] Quincke's diseases, however, is a relatively rare, life-threatening complication seen with marijuana use and is characterized by localized swelling of the deeper layers of the skin and fatty tissues beneath the skin. The pathophysiology, differential diagnosis, and treatment of this disease will be discussed.
Case Report
A 28-year-old male presented to emergency department with difficulty swallowing with associated shortness of breath for 1 day. He reported no recent history of trauma and denied swelling of the face, pruritus, fever, or any sick contact. His past medical history was significant for atypical hemolytic uremic syndrome, malignant hypertension, and end-stage renal disease on hemodialysis. The patient also denied any history of illicit drug abuse.
Physical examination revealed temperature of 36.1°C, heart rate of 65 beats/min, respiratory rate of 12 with oxygen saturation of 99% on room air. Upon examination of the oral cavity, it was noted that the uvula was edematous but without any lesion [Figure 1]. The visualized pharynx and dentition were within normal limits, and the patient had no pain with palpation of his trachea. The remainder of the physical examination was normal.
Figure 1.
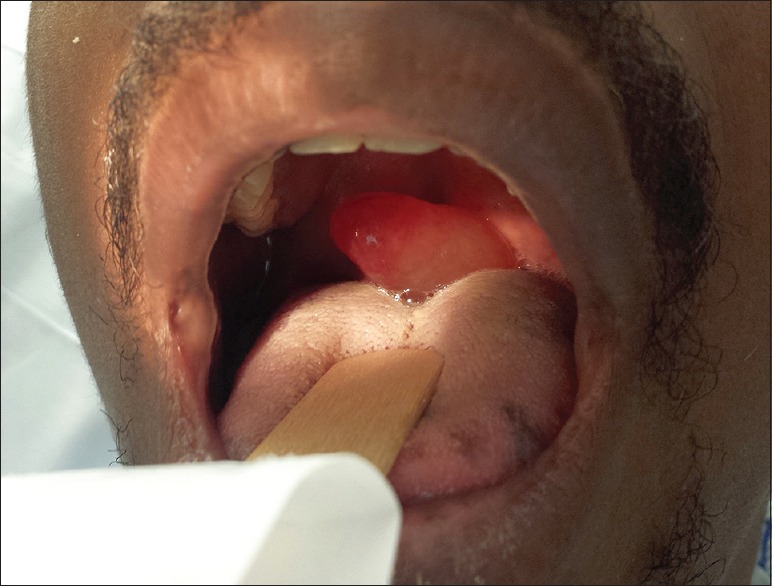
Photograph demonstrating uvular edema
Soft-tissue radiograph of the neck was obtained and showed swollen uvula [Figure 2]. A complete blood count revealed white blood cell count of 4.7 (4.5–11), hemoglobin 12.4 (14–18), hematocrit 38 (40–54), and platelets 210 (140–440). A basic metabolic profile revealed sodium of 132 (136–145), potassium 5.2 (3.5–5.1), chloride 100 (98–107), CO2 24 (22–29), blood urea nitrogen 32 (9–21), creatinine 4.9 (0.7–1.3), glomerular filtration rate 14, and glucose 82 (70–105). Both flu A and B were also negative.
Figure 2.
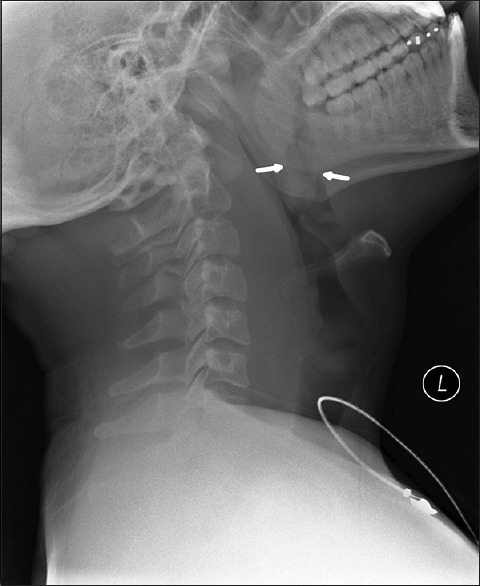
Lateral radiograph of the neck demonstrating a swollen uvula
The patient was treated with intravenous (IV) steroids, diphenhydramine and admitted to the intensive care unit for further airway monitoring. While on the floor, the patient subsequently admitted to using marijuana just prior to the onset of symptoms and was diagnosed with cannabinoid-induced Quincke's disease.
Discussion
Quincke's disease, or isolated uvular angioedema, was first described in 1882 and has since been a relatively rare form of angioedema of the upper airway.[1] Due to the rarity of this illness, the clinician should develop a detailed differential diagnosis for a patient with acute onset of difficulty swallowing with associated with shortness of breath. Within this differential epiglottitis, retropharyngeal abscess and peritonsillar abscess should all be considered.
Epiglottitis is a rare, life-threatening disease caused by inflammation of the epiglottis that can occur at any age. Common clinical manifestations of epiglottitis include acute high fever, severe sore throat, and difficulty swallowing with the sitting up and leaning forward position and drooling. The most common organism is Haemophilus influenzae Type B (HIB).[4] The “thumb sign” is the standard finding on lateral radiograph of the neck. Our patient presented with the absence of fever, sore throat, and drooling supported by no thumb sign on the neck radiograph excluding this diagnosis.
Retropharyngeal abscess is an infection in one of the deep spaces of the neck and can pose an immediate life-threatening emergency. It is a rare finding in adults and reported as a result of local trauma, such as foreign body ingestion or instrumental procedures. Aerobic, anaerobic, and Gram-negative organisms can cause abscesses in this space. Clinical symptoms are variable and nonspecific. Computed tomography (CT) is used for the diagnosis.[5] Our patient did not report any trauma or recent procedure; hence, retropharyngeal abscess was excluded.
Peritonsillar abscess is the most common deep infection of the head and neck in adults and is typically caused by both aerobic and anaerobic bacterial infections. The clinical presentation includes fever, throat pain, and trismus. Ultrasonography and CT scanning are used for diagnosis.[6] Our patient did not present with signs of infection and no trismus was found on examination; therefore, peritonsillar abscess was excluded.
Once the diagnosis of Quincke's disease is suspected, management is based on the etiology with clues collected during the history and physical examination. Although it is typically caused by an immediate Type I hypersensitivity reaction, uvular edema can also be caused by trauma, thermal injury, and infections.[2]
Suggested laboratory workup is blood and surface cultures of pharynx and uvula, latex agglutination studies for HIB and Streptococcus pneumoniae antigens in blood and urine, lateral neck films, and toxicology on urine and blood must be done[7] Fever is highly suggestive of infectious etiology. Group A beta-hemolytic Streptococcus, HIB, and S. pneumoniae are the most common causative organisms. Immediate IV antibiotic is to be started for an infectious isolated uvular angioedema after laboratory workup collected. For patient with posttraumatic or inhalant uvulitis, steroids must be administered. Epinephrine and diphenhydramine should be added in allergic reaction induced isolated uvular angioedema. The premise for uvular edema following marijuana smoking is that marijuana burns at a higher temperature than tobacco and can be more irritating to the mucous membranes.
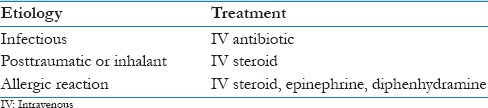
Treatment is aimed at maintaining a patent airway in conjunction with antihistamines, glucocorticoids, and epinephrine if needed. Rapid access to proper equipment and personnel for intubation or tracheostomy is necessary.[7] Table 1 summarizes the suggested treatments for the most common etiologies-induced Quincke's disease.
Table 1.
Most common etiologies and suggested treatment for Quincke's disease
Conclusion
Marijuana is commonly used in our society and although most of its side effects are known, Quincke's disease, or isolated uvular angioedema, is a relatively uncommon presentation which can compromise airway and potentially be life-threatening. The premise for uvular edema following marijuana smoking is that marijuana burns at a higher temperature than tobacco and can be more irritating to the mucous membranes. Treatment is aimed at maintaining a patent airway in conjunction with antihistamines, glucocorticoids, and epinephrine if needed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Quincke H. Acute localized edema of the skin. Monatschr Prakt Dermatol. 1882;1:129–31. [Google Scholar]
- 2.Huang CJ. Isolated uvular angioedema in a teenage boy. Internet J Emerg Med. 2006:3. [Google Scholar]
- 3.Versteeg PA, Slot DE, van der Velden U, van der Weijden GA. Effect of cannabis usage on the oral environment: A review. Int J Dent Hyg. 2008;6:315–20. doi: 10.1111/j.1601-5037.2008.00301.x. [DOI] [PubMed] [Google Scholar]
- 4.Abdallah C. Acute epiglottitis: Trends, diagnosis and management. Saudi J Anaesth. 2012;6:279–81. doi: 10.4103/1658-354X.101222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Harkani A, Hassani R, Ziad T, Aderdour L, Nouri H, Rochdi Y, et al. Retropharyngeal abscess in adults: Five case reports and review of the literature. ScientificWorldJournal. 2011;11:1623–9. doi: 10.1100/2011/915163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Steyer TE. Peritonsillar abscess: Diagnosis and treatment. Am Fam Physician. 2002;65:93–6. [PubMed] [Google Scholar]
- 7.Guarisco JL, Cheney ML, LeJeune FE, Jr, Reed HT. Isolated uvulitis secondary to marijuana use. Laryngoscope. 1988;98:1309–12. doi: 10.1288/00005537-198812000-00006. [DOI] [PubMed] [Google Scholar]


